Abstract
The Illness Management and Recovery (IMR) program was developed based on a comprehensive review of research on teaching illness self-management strategies to clients with schizophrenia and other severe mental illnesses and “packaged” in a resource kit to facilitate dissemination. Despite growing dissemination of this program, it has not yet been empirically validated. This article describes the development and theoretical underpinnings of the IMR program and presents pilot data from the United States and Australia (N = 24, 88% schizophrenia or schizoaffective) on the effects of individual-based and group-based treatment over the 9-month program and over a 3-month follow-up. High satisfaction was reported by participants. Strong improvements over treatment and at follow-up were found in clients' self-reported effectiveness in coping with symptoms and clinicians' reports of global functioning and moderate improvements in knowledge about mental illness, distress related to symptoms, hope, and goal orientation. These findings support the feasibility and promise of the IMR program and point to the need for controlled research to rigorously evaluate its effects.
Keywords: illness self-management, recovery, schizophrenia, evidence-based practices, psychosocial treatment, psychiatric rehabilitation
The past decade has witnessed an unparalleled focus on quality improvement in services for schizophrenia and other severe mental illnesses. Much of this focus has been stimulated by the identification of standards for care for schizophrenia based on research evidence,1 coupled with the finding that these practices were rarely provided.2–4 The President's New Freedom Commission5 drew attention to the disparity between research and practice and called for a transformation of the mental health system to one that provides access to high-quality treatment based on the best scientific evidence and embraces clients and their families as partners in treatment. In addition, the report echoed the growing consensus that treatment should focus on not just managing symptoms but on recovery, which was defined as helping people with mental illness “live, work, learn, and participate fully in their communities.”
Traditional medical definitions of recovery focus on remission of symptoms and return to prior functioning. Although medical recovery from schizophrenia occurs,6–11 alternative definitions have emerged that are more personal in nature and emphasize a blend of subjective aspects with improved functioning.12–16 These personal conceptualizations evoke several common themes, including hope, social connection, personal responsibility, meaningful life activities, a positive identity, full life beyond the illness, and personal growth.14,16–20
Recovery or living successfully with any chronic health condition requires individuals to learn how to manage their illness in collaboration with treatment providers.21 In the broader health field, evidence supports the value of teaching illness self-management for improving chronic medical conditions such as diabetes, arthritis, and asthma.22 In addition, collaborative management of chronic illness, which involves the patient and doctor working together to identify problems, set goals, incorporate self-management strategies, and monitor progress over time,23 leads to higher levels of trust and satisfaction, reduced emotional burden, and improved biomedical markers such as blood pressure and blood sugar control (eg, hemoglobin A1Cs).24 However, the vast majority of people with schizophrenia still need help managing their illness, collaborating with treatment providers, and pursuing their recovery goals.
Relapses of psychotic symptoms are common and have a disruptive effect on the quality of clients' lives and their capacity for independence.25–27 Although new antipsychotics continue to be developed, persistent psychotic symptoms plague 25%–50% of clients with schizophrenia,28–32 and these symptoms are associated with a host of negative outcomes, including depression and demoralization,33–36 impaired social functioning,37,38 and low employment.39,40 Over 85% of persons with schizophrenia are unemployed,41 despite the fact that most want to work42–45 and are capable of working in competitive jobs.46 Furthermore, although most clients live in the community, many lead lonely, isolated lives, without social or recreational outlets or personal purpose.47–50
In addition, there is a lack of active collaboration between people with schizophrenia and their treatment providers. Treatment plans often fail to address clients' goals, and clinicians assume that they need to be protected from stress and live in protected settings,47 despite evidence to the contrary.50 Pharmacological treatment is often provided with little explanation or choice,51 thereby compromising adherence52 and increasing risk of relapse. There is a need for interventions that teach clients how to manage their schizophrenia collaboratively with treatment providers, in order to help them improve their lives.
Illness Management and Recovery Program
The Illness Management and Recovery (IMR) program was developed in order to help clients with schizophrenia or major mood disorders learn how to manage their illnesses more effectively in the context of pursuing their personal goals.53 The impetus for developing IMR initially arose at a Robert Wood Johnson Foundation Consensus conference of National Institute of Mental Health staff, services researchers, advocates, and the schizophrenia Patient Outcomes Research Team1,2 in Baltimore in 1997, where it was suggested that the various psychosocial interventions for helping people manage their symptoms and prevent relapses needed to be consolidated into a single standardized program for study and dissemination. To meet this need, the IMR program was developed as part of the National Implementing Evidence-Based Practices (EBPs) Project54–56 between 2000 and 2002 and packaged as an “implementation resource kit” designed to foster its dissemination (eg, manual and handouts, information brochures, introductory and training videos, fidelity scale, outcome measures). All of the EBP resource kits were developed by 2 coleaders and a committee of stakeholders, including researchers, clinicians, consumers, family members, and program leaders. Susan Gingerich and Kim Mueser were the coleaders for the IMR resource kit.
The IMR program was developed based on a review of controlled research on teaching illness self-management strategies to clients with severe mental illness.57 Five empirically supported strategies were identified in this review and incorporated into the program, including psychoeducation about mental illness and its treatment, cognitive-behavioral approaches to medication adherence (eg, incorporating cues for taking medication into daily routines), developing a relapse prevention plan, strengthening social support by social skills training, and coping skills training for the management of persistent symptoms. In order to motivate clients to learn how to better manage their illness and to help them move forward in their lives, IMR begins with an exploration of the meaning of recovery to the client and setting personal recovery goals to work toward in the program.
The five empirically supported illness self-management strategies are incorporated into the IMR program, which is organized into 9 curriculum topic areas. These topics are taught using a combination of educational, motivational, and cognitive-behavioral teaching strategies, with weekly individual or group sessions requiring approximately 9 months to complete. Homework assignments are developed collaboratively with the client. In addition, with clients' consent, significant others (eg, family, friends) are encouraged to be involved in helping clients learn self-management strategies and pursue their personal goals. All the materials for the IMR program (except the videos, available by writing Substance Abuse and Mental Health Services Administration [SAMHSA]) are available free from the SAMHSA Web site: http://www.mentalhealth.samhsa.gov/cmhs/communitysupport/toolkits. An outline of the curriculum taught in IMR is provided in table 1.
Table 1.
Overview of Topics for Illness Management and Recovery (IMR) Modules
| Module | Topic | Goals | Number of Sessions |
|---|---|---|---|
| 1 | Recovery strategies | • Engage clients in group | 4 |
| • Increase awareness of recovery | |||
| • Set personal recovery goals | |||
| • Develop plans for achieving goals | |||
| 2 | Practical facts about schizophrenia | • Identify symptoms associated with schizophrenia | 4 |
| • Dispel myths about schizophrenia | |||
| • Address stigma | |||
| • Help clients become aware of people with schizophrenia who lead productive lives | |||
| 3 | Stress-vulnerability model and treatment strategies | • Explain that stress and biological vulnerability cause symptoms of schizophrenia | 3 |
| • Discuss strategies for reducing stress and biological vulnerability | |||
| • Inform clients about treatment options | |||
| 4 | Building social support | • Discuss how building social support can facilitate recovery | 7 |
| • Teach strategies for increasing support, such as finding places to meet people, conversation skills, and getting closer to people | |||
| 5 | Using medications effectively | • Teach clients about benefits and side effects of medications | 4 |
| • Increase skills for discussing medication issues with physician | |||
| • Help clients weigh pros and cons of taking medications | |||
| • Teach behavioral tailoring to facilitate medication adherence | |||
| 6 | Reducing relapses | • Teach clients that relapses are predictable and preventable | 4 |
| • Develop an individual relapse prevention plan | |||
| 7 | Coping with stress | • Inform clients they can reduce stress and improve their ability to cope with it effectively | 5 |
| • Identify and practice strategies to prevent and to cope with stress | |||
| 8 | Coping with problems and persistent symptoms | • Teach problem-solving model | 6 |
| • Help clients identify common problems and symptoms that cause distress | |||
| • Practice coping strategies for persistent symptoms | |||
| 9 | Getting your needs met in the mental health system | • Review different mental health services | 3 |
| • Identify insurance benefits clients are entitled to | |||
| • Help clients identify strategies to advocate for self in mental health system |
Note: Since the completion of this study, a 10th IMR module has been developed for Drug and Alcohol Use that is usually taught between the fifth and sixth modules. This module provides information on the effects of substance use on mental illness, reasons for using the pros and cons of continued use vs sobriety, and (for motivated clients) developing a personal sobriety plan. The handout for this module and clinical guidelines for teaching it can be obtained from Dr Mueser.
Theoretical Underpinnings of IMR
The IMR program integrates specific empirically supported strategies for teaching illness self-management into a cohesive treatment package based on 2 theoretical models: the transtheoretical model and the stress-vulnerability model. The transtheoretical model proposes that motivation to change develops over a series of stages (precontemplation, contemplation, preparation, action, maintenance) and that facilitating change requires stage-specific interventions.58,59 At the earliest stages, people are not committed to change and intervention focuses on instilling motivation. In the IMR program, motivational interviewing60,61 is used at the beginning and throughout the program to help clients develop their own vision of recovery, to identify and pursue their personal goals based on that vision, and to explore how improved illness management can help them achieve these goals.
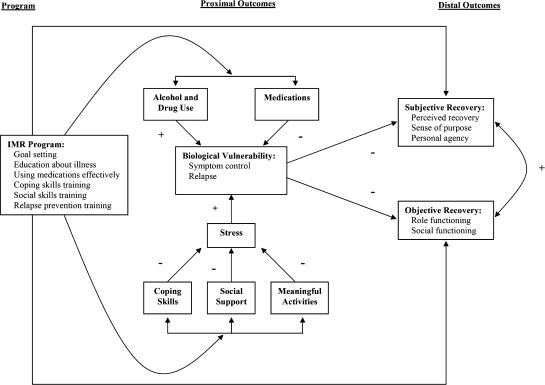
The stress-vulnerability model62,63 posits that the course and outcome of schizophrenia is determined by the dynamic interplay of biological vulnerability, stress, and coping. IMR is aimed at interrupting the cycle of stress and vulnerability that leads to relapse and poor functioning (see figure 1). In IMR, the proximal goal is to teach clients the fundamentals of illness self-management based on the stress-vulnerability model (ie, adherence to medications, reduced substance use, increased social support, increased coping, involvement in meaningful activities) in order to improve illness outcomes such as symptoms, relapses, and hospitalizations. Then, through the combination of pursuing personal goals and improved illness self-management, the distal goal of IMR is to help clients make progress toward recovery, including objective (eg, community functioning, social relationships, work) and subjective (eg, sense of purpose, hope, confidence) dimensions.
Fig. 1.
Conceptual Framework for the Illness Management and Recovery program.
Need for Research on the IMR Program
The standardization of the IMR program, the free and easy access to the resource kit, and its broadly accepted status as an “EBP” have led to its rapid adoption throughout the United States since it became available in 2003. For example, approximately 1700 IMR resource kits have been distributed by SAMHSA (N. Brown, personal communication, February 2006), and an unknown number more downloaded from SAMHSA's Web site. Furthermore, the IMR program has become the focus of federal grants aimed at dissemination, developing reimbursement policies to support its implementation, or adapting it for special populations (C. Boyle and M. P. Salyers, unpublished data, 2006, SM56140:10/03–09/06; J. M. J. Martinez, unpublished data, 2006; E. G. Riera, unpublished data, 2006, R34MH074786:10/05–09/08; M. P. Salyers, unpublished data, 2006, H133G030106:10/03–09/06; G. C. Souther, unpublished data, 2006, 11-P-92508/1:10/04–19/07; T. White, unpublished data, 2006).
Despite the growing popularity of the IMR program, it has not yet been critically evaluated. Furthermore, although IMR incorporates specific empirically supported strategies for teaching illness self-management, its emphasis on developing and pursuing personal recovery goals is unique. Research is needed to determine whether the IMR program in fact improves the management of severe mental illness and longer term functional outcomes such as community adjustment and quality of social relationships. The present report provides pilot data on the effects of the IMR program, implemented in a number of different formats (individual and group) in several different settings.
Methods
The study took place at 3 different centers, 2 in North Carolina (NC) and 1 in Australia, and employed either individual or group formats.
Study Sites and Participants
In NC, individual IMR was provided at the Schizophrenia Treatment and Evaluation Program at the University of NC at Chapel Hill (N = 13) and group IMR was conducted at the Wake County Human Services in Raleigh, NC (N = 9). Inclusion criteria were ages 18–65 and State of NC designation of severe mental illness (Axis I disorder and impaired social, vocational, or self-care functioning). There were no exclusion criteria.
In Australia, group IMR was implemented at the Newcastle Community Mental Health Service (N = 10). Inclusion criteria were ages 18–65 and a diagnosis of schizophrenia or schizoaffective disorder.
All participants were assessed at baseline, posttreatment, and 3-month follow-up.
IMR Program Implementation: All Sites
IMR was introduced to clients at all sites with an orientation videotape, which describes the program and features clients telling their recovery stories. Each IMR module includes an educational handout that summarizes the main points of the topic and worksheets to enhance learning. Clinicians used a variety of techniques to optimize learning and retention, such as interactive teaching and checking for understanding during each session. Sessions were held weekly over approximately 9 months and comprised 9 modules taught sequentially. Each module lasted approximately 2–4 weeks but varied depending on clients' abilities and preferences.
Individual and group IMR sessions followed a standardized structure53:
Informal socializing. The clinician and clients used this time to build rapport and discuss any additional issues that needed to be covered at the end of the session.
Review content from previous sessions. Material was reviewed from the previous session in order to assess clients' understanding and retention of information and skills.
Review home assignment from previous session. Completion of home assignments was reviewed, successful efforts by clients or outcomes were reinforced, and any difficulties encountered were collaboratively problem solved by the clinician and clients.
Follow up on goals. Clients' progress toward their personal goals was assessed, obstacles were identified and problem solved together, and success was followed up by determining and planning the next steps or setting new goals.
Set agenda for current session. An agenda was collaboratively set for the remainder of the session.
Teach new material and practice new strategies. Material in the handouts for the IMR program was reviewed and taught using a combination of educational, motivational, and cognitive-behavioral strategies, tailored to each consumer's reading ability, interests, previous knowledge, and goals.
Collaboratively formulate home assignment for the next week. Clinicians and clients agreed on a home assignment to review and practice material taught in the session or to make steps toward clients' personal goals, anticipated any obstacles that might prevent completion of the assignment, and problem solved ways to overcome those obstacles.
Summarize progress made in current session. Material covered in session was reviewed and feedback obtained from the clients.
Individual IMR—United States
The individual IMR therapists included 2 clinical psychologists, a clinical psychology graduate student, and 2 psychiatry residents. All the therapists received weekly individual supervision from one of the authors (Dr Penn). Sessions lasted approximately 1 hour.
Group IMR—United States
The IMR group was coled by a clinical psychologist (Dr Penn), a psychiatrist, and a licensed social worker, and sessions lasted about an hour. The group leader role was rotated, with the 2 other mental health professionals serving as coleaders and facilitators. In addition to clients in the group having home assignments, similar assignments were also developed for the group leaders in order to improve group cohesion and provide role models. The IMR material was reviewed using PowerPoint in half the sessions, depending on the availability of the liquid-crystal display (LCD) projector, giving the group a classroom feel. In the other sessions, the material was reviewed on paper.
Group IMR—Australia
All clinicians (N = 25) working at the Newcastle Mental Health Service attended a 2-day IMR training program. Even though clinicians were trained in the IMR program and introduced to the concepts of evidence-based toolkits, most were skeptical and remained unenthusiastic regarding the introduction of the program. However, clinicians involved in delivering the IMR groups were drawn from staff who were committed to the program's implementation. The initial group was led by a clinical nurse consultant and cofacilitated by a senior social worker. The second group was led by a senior social worker and cofacilitated by a registered nurse.
The Australian IMR groups were conducted using comparable methods to those employed in the United States. There were some differences in session duration; in Australia, each session consisted of two 45-minute meetings with a 30-minute break in between. The IMR modules were converted to PowerPoint to assist in the group-based delivery of the program. The visual impact of the modules combined with pictures was useful for clients who responded better to visual rather than auditory learning. The use of PowerPoint and LCD projector in the group context not only provided an excellent medium to deliver the program but also afforded the opportunity for group facilitators to model completion of worksheets while the electronic image was being projected onto a whiteboard. The clients responded very positively to these changes and stated that they felt like they were attending a class rather than a “group.”
The original modules received from the United States were reformatted using larger font sizes and line spacing, specific language changes were made as needed, and the module on “Getting Your Needs Met in the Mental Health System” was changed to incorporate the services specific to the Australian context. Each module was printed on colored paper, with a different color for each module. This increased the visual appeal of the modules and assisted less literate participants within the groups. Additionally, the group developed home assignment cards that were small enough to fit in a wallet or purse to help improve follow-through.
Regular supervision sessions ensured faithful adherence to the group structure and core IMR strategies described in the IMR toolkit and outlined previously.
Measures
Self-report measures were given to clients to assess several domains of illness management and recovery.
Illness Management
The Brief Symptom Inventory (BSI)64 is a 53-item scale used to evaluate psychiatric symptoms with an global composite score (global severity index [GSI]), which was developed based on the longer Symptom Checklist-90, Revised (SCL-90).65 Each item is measured using a 5-point distress scale that ranges from 0 (not at all) to 4 (extremely). The SCL-90 and BSI were designed to measure symptom distress related to 9 different subscales, with coefficient α values for the subscales on the BSI ranging from .63 to .89 in clients with either depression or schizophrenia,66 indicating good internal reliability. Factor analyses of the SCL-90 and BSI suggest they measure a single factor related to distress.66,67 Convergent validity of the BSI in schizophrenia68 is supported by significant associations with quality of well-being69 and self-reported health and mental health functioning on the Medical Outcomes Study 36-item Short Form Health Survey.70
The Coping Skills Scale was adapted from a coping measure developed by Mueser et al.71 Coping strategies and their perceived efficacy were elicited in a semistructured interview for up to 15 distressing symptoms. There are no psychometric data on this scale from prior studies. For the present study, coefficient α was .74 for ratings of coping effectiveness, indicating good internal reliability; convergent validity was supported by a Pearson correlation of .66 between number of distressing symptoms and BSI GSI score.
The IMR Scale72 taps all the critical self-management domains targeted in the IMR program and uses 5-point behaviorally anchored scales. In this pilot study, we used a shortened version of the Client IMR Scale with 11 items that included progress toward goals, knowledge about mental illness, involvement with significant others and self-help, time in structured roles, impairment in functioning, symptom distress and coping, relapse prevention and hospitalizations. Prior research on the Client IMR Scale indicates satisfactory internal reliability (coefficient α = .70), test-retest reliability over 2 weeks (r = .82), and convergent validity with the Recovery Assessment Scale (RAS)73 and the Colorado Symptom Inventory74 (r values = .38 and .54, respectively). The Knowledge Questionnaire is a 42-item multiple-choice and true/false test designed for the IMR program to assess knowledge of mental illness. Psychometric data on this scale are not available from prior research; for the present study, coefficient α was .59, indicating moderate internal reliability.
Recovery
The RAS73 is a 41-item scale used to assess perceptions of recovery from severe mental illness with a 5-point Likert scale. The RAS includes 5 factors: personal confidence and hope (eg, “Fear doesn't stop me from living the way I want to”), willingness to ask for help (eg, “I ask for help when I need it”), goal and success oriented (eg, “I have goals in my life that I want to reach”), positive reliance on others (eg, “I have people I can count on”), and not dominated by symptoms (eg, “My symptoms interfere less and less with my life”). Prior research on the RAS indicates high internal reliability (coefficient α = .93), test-retest reliability over 2 weeks (r = .88), and convergent validity with the Rosenberg Self-Esteem Scale,75 the Empowerment Scale,76 the Social Support Questionnaire,77 the subjective component of the Quality of Life Interview,78 and the Brief Psychiatric Rating Scale79 (r values = .55, −.71, .48, .62, and −.44, respectively).80
The Multidimensional Scale of Perceived Social Support (MSPSS)81 is a self-report inventory that measures perceived social support from family, friends, and a significant other. The MSPSS consists of 12 items that assess the degree of satisfaction with social support. Prior research on the MSPSS indicates high internal reliability (coefficient α values = .91 and .94 for schizophrenia and major mood disorders, respectively) and moderate convergent validity with the Network Orientation Scale82 (r = .31). The original MSPSS used a 7-point Likert scale that ranges from 1 (very strongly disagree) to 7 (very strongly agree); however, due to a word-processing error in this study, a 4-point scale was used. The items were then summed as an overall measure of social support. The Global Assessment of Functioning (GAF) scale83 was used as a measure of psychological, social, and occupational functioning with ratings ranging from 1 to 100. The GAF has well-established reliability, even for minimally trained raters, and abundant evidence supports its validity.84,85 Lastly, each participant was asked to complete a 6-item satisfaction survey. Each item had 3 choices (not helpful, helpful, or very helpful).
Data Analytic Plan
All analyses were performed using SPSS. Participants who completed at least baseline and posttreatment assessments were included in the final analysis. We compared the dropouts with the participants who completed the study using t test and χ2 analyses. We also compared the US and Australian clients on all demographic and clinical measures to determine if there were any differences between the groups.
To compare the IMR treatment effects over time on measures of symptoms, recovery, and functioning, linear mixed-effects regression models were computed with unstructured and first-order autoregressive covariance matrixes using the MIXED procedure. Time and treatment group were used as fixed effects, and random intercepts were allowed for each participant. After conducting a global F test, pairwise comparisons of adjusted means between all time points were conducted using 2-tailed Tukey tests for each measure. Effect size estimates were calculated by using Cohen's d statistic for paired t tests from baseline to follow-up, and missing data was replaced using the Last Observation Carried Forward method. To assess satisfaction with IMR treatment, frequencies from the satisfaction survey were reported.
Results
Of the 12 individuals who were recruited into the US individual IMR treatment program, 10 completed the treatment and 2 dropped out. The length of treatment ranged from 3.23 to 9.23 months with a mean of 6.59 (SD = 1.96) months. The mean length of time between the posttreatment and follow-up assessment was 3.77 (SD = 0.98) months. In the US IMR group, 9 individuals were recruited into the study and 8 completed at least half the sessions and were included in this pilot study. Six participants completed the entire protocol, one left the group after the first month, one left midtreatment to return to school, and one stopped attending after 6 months. The dropouts were compared with the participants who completed the treatment on demographic characteristics and the baseline measures, and no differences were found. The IMR group lasted for 9.46 months, and the mean length of time between the posttreatment and follow-up assessment was 5.31 (SD = 0.42) months.
In Australia, 10 individuals were recruited into 2 IMR groups with 6 out of 10 participants completing the entire program over the 2 groups. Retention rates in the first Australian IMR group were low. Four out of 5 clients dropped out; 1 client left the group after 2 sessions, another client chose to leave the group after 5 sessions, and 2 moved away from the area after completing 6 and 11 sessions, respectively. One participant completed the program in 8.54 months, and the length of time between the posttreatment and follow-up assessments was 3.46 months.
Retention rate for the second Australian IMR group was significantly better with 5 out of 5 clients completing the entire program. This group lasted for 9.92 months, and the length of time between posttreatment and follow-up assessment was 3 months. Possible reasons for the improved retention are considered in the “Discussion” section.
The US and Australian participants did not significantly differ on any demographic or functioning variables, including age, education, race, diagnosis, gender, or GAF, and thus, the sites were combined for all further analysis.
Table 2 shows the demographic and clinical characteristics of the combined sample. The majority of the sample was Caucasian, male, and never married. Most participants had a diagnosis of either schizophrenia or schizoaffective disorder.
Table 2.
Demographics Total Australian/US Sample (N = 24)
| Mean (count) | SD (%) | |
|---|---|---|
| Age | 39.12 | 11.20 |
| Education (N = 20) | 14.70 | 3.11 |
| Gender | ||
| Male | 15 | 63 |
| Female | 9 | 37 |
| Ethnicity | ||
| Caucasian | 16 | 89 |
| Black | 2 | 11 |
| Marital situation | ||
| Never married | 20 | 83 |
| Married | 3 | 13 |
| Divorced | 1 | 4 |
| Primary diagnosis | ||
| Schizophrenia | 10 | 42 |
| Schizoaffective disorder | 11 | 46 |
| Bipolar disorder | 2 | 8 |
| Delusional disorder | 1 | 4 |
| Treatment | ||
| Individual IMR | 10 | 42 |
| Group IMR | 14 | 58 |
Note: IMR, Illness Management and Recovery.
After IMR treatment, participants showed improvements in illness management and recovery domains (see table 3). Clients reported significant decreases in symptom severity from baseline to follow-up. Additionally, clients reported some improvements in effective coping strategies for their symptoms as measured by the Coping Skills Scale from baseline to posttreatment but not at follow-up. Illness self-management was enhanced as shown by increases in IMR Scale scores from baseline to posttest. Participants also improved in their knowledge of mental illness at posttreatment and follow-up.
Table 3.
IMR Pilot Study Assessment Measures
| Baseline (N = 24)
|
Posttreatment (N = 24)
|
Follow-up (N = 17)
|
|||||||
|---|---|---|---|---|---|---|---|---|---|
| M | SD | M | SD | M | SD | F (df) | P | d | |
| Illness management | |||||||||
| BSI GSIa | 1.03 | 0.17 | 0.92 | 0.15 | 0.77 | 0.14 | 4.37 (2, 22) | .03 | .50 |
| Coping—total symptomsb | 6.05 | 1.07 | 4.62 | 0.95 | 5.87 | 1.18 | 2.28 (2, 14) | .14 | .38 |
| Coping effectivec | 3.05 | 0.28 | 3.55 | 0.27 | 3.25 | 0.21 | 3.79 (2, 22) | .04 | .84 |
| Client IMR—shortened/sumc,d | 36.97 | 2.29 | 45.82 | 2.18 | 42.08 | 2.62 | 10.82 (2, 16) | .00 | .83 |
| Knowledge of illnessd,e | 91.52 | 1.38 | 95.32 | 0.86 | 94.66 | 1.34 | 6.63 (2, 23) | .01 | .63 |
| Social support | 45.82 | 1.96 | 47.65 | 1.64 | 46.90 | 1.88 | 0.44 (2, 20) | .65 | .18 |
| Recovery | |||||||||
| Recovery meand,e | 3.81 | 0.10 | 3.98 | 0.10 | 4.04 | 0.11 | 4.76 (2, 41) | .01 | .64 |
| RAS—hoped,e | 32.75 | 1.14 | 34.27 | 1.14 | 34.96 | 1.19 | 3.66 (2, 40) | .04 | .55 |
| RAS—willingness ask help | 12.11 | 0.32 | 12.91 | 0.32 | 12.73 | 0.36 | 2.71 (2, 40) | .08 | .30 |
| RAS—goal orientedd,e | 18.75 | 0.84 | 20.17 | 0.84 | 20.94 | 0.91 | 3.28 (2, 39) | .05 | .48 |
| RAS—rely on others | 16.90 | 0.41 | 16.53 | 0.41 | 17.03 | 0.44 | 1.24 (2, 41) | .30 | .02 |
| RAS—not dominated symptomd,e | 9.95 | 0.54 | 11.24 | 0.54 | 11.48 | 0.60 | 3.48 (2, 41) | .04 | .60 |
| GAFd,e | 53.71 | 2.43 | 61.45 | 3.05 | 59.99 | 3.43 | 10.91 (2, 18) | .00 | .80 |
Note: IMR, Illness Management and Recovery; BSI, Brief Symptom Inventory; GSI, global severity index, GAF, Global Assessment of Functioning.
Baseline > follow-up (P < .05).
N = 16.
N = 15.
Baseline < posttest (P < .05).
Baseline < follow-up (P < .05).
Recovery attitudes also showed a pattern of improvement at posttreatment. Scores on the RAS suggested that participants had more hope about recovery and felt less dominated by their symptoms. These improvements were maintained through follow-up. GAF scores improved significantly from baseline to posttest and were sustained over follow-up. Perceived social support did not change over time.
Additional analyses were conducted to evaluate differences between clients in the individual and group IMR formats over time. Only one significant difference emerged: individual participants had higher scores across all 3 time points on the relying on others subscale of the RAS than the group participants (individual M = 17.63, SD = 0.51; group M = 16.01, SD = 0.47; F1,23 = 5.43, P = .03).
Results from the satisfaction survey are summarized in table 4 and indicated that most participants found the intervention to be helpful, respectful, and useful.
Table 4.
Participant Feedback From Illness Management and Recovery Satisfaction Survey (N = 22)
| Not Helpful/Respectful/ Useful N (%) | Helpful/Respectful/ Useful N (%) | Very Helpful/Respectful/Useful N (%) | |
|---|---|---|---|
| Covers sufficient material | 1 (4) | 21 (96) | 0 |
| Materials are understandablea | 1 (5) | 10 (48) | 10 (48) |
| Useful | 0 | 13 (59) | 9 (41) |
| Respectful | 0 | 9 (41) | 13 (59) |
| Helps better manage symptoms | 0 | 15 (68) | 7 (32) |
| Helps recovery | 0 | 14 (64) | 8 (36) |
N = 21.
Discussion
The pilot data on the implementation of the IMR program supports both its feasibility and its acceptability. The rates of program retention, defined as participation in more than half of the IMR sessions, were high for both group and individual IMR at the NC sites, with 19 out of 22 (86%) clients “treatment takers.” Retention rates were low in the first group conducted at the Australia site (20%) but high in the second group (100%). Possible reasons for the high dropout rate in the first Australian IMR group may be related to the Australian services' initial low readiness to embrace EBPs in the toolkit form at the time of recruitment for the this group. Higher retention of participants in the second Australian group may have been due to a combination of factors, including improved support from case managers for clients' attendance at the groups, increased acceptance of the IMR program by clinicians, and referral of clients to IMR who were more stable in terms of symptoms and living situation.
Clients who participated in IMR expressed high satisfaction, with all reporting that the program was useful, respectful, helpful for managing their symptoms, and helped them make progress toward their goals. All but one client found the program covered sufficient breadth of information and that the materials were understandable. While dropouts were probably less satisfied with the program, these findings suggest that most found the materials and approach helpful to managing their illness and making progress toward personally meaningful goals.
Changes from baseline to posttreatment and follow-up indicated significant effects across most measures, with no interactions between treatment modality (individual vs group) and change over time. The largest effect sizes were for clients' ratings of their coping effectiveness (d = .84), the Client IMR Scale (d = .83), and GAF score (d = .80). These findings are in line with the primary aims of the IMR program. Skills for coping with persistent symptoms are systematically taught, and clients reported better coping self-efficacy for these symptoms. This is consistent with studies showing that the number of coping strategies clients report using to manage symptoms is correlated with their coping efficacy71,86,87 and with research on the effects of teaching coping strategies for persistent symptoms.88 The IMR Scale was developed in order to tap the specific dimensions of illness self-management targeted in the IMR program (eg, progress toward goals, support in managing one's illness, use of medication adherence strategies, involvement in structured activities, having a relapse prevention plan), and thus, improvements in it are in line with the aims of the program. Of greatest significance was the finding that participation in IMR was associated with improvements in functioning on the GAF. These findings are also consistent with the main goal of the IMR program, which is to help clients articulate personally meaningful goals and to learn how to manage their illness in the service of making progress toward these goals.
Moderate effect sizes were also found for several other outcomes. Consistent with improvement in coping self-efficacy, clients also reported modest improvements in distress related to their symptoms on the BSI (d = .5). Furthermore, in line with the aim of the IMR program of providing clients with information about mental illness and its treatment in order to facilitate informed decision making, significant improvements were found in knowledge of the illness (d = .63). Finally, clients who participated in the IMR program showed significant improvements in hope (d = .55) and goal orientation (d = .48) on the RAS. The importance of hope to recovery has been emphasized by many people with mental illness.19,27,89 The increased orientation toward goals on the RAS may be related to the focus of IMR on helping clients articulate and make progress toward personal goals and on removing illness-related obstacles to achieving them.
The effect sizes were small and nonsignificant for improvements in social support and help from others. Willingness to ask for help on the RAS showed a modest improvement (d = .30), while satisfaction with social support showed a small but nonsignificant improvement (d = .18) and reliance on others on the RAS showed no change at all (d = .02). The relative lack of change in support has several possible interpretations and implications. First, improvements in the quality of social relationships and social support may simply take longer to accrue. For example, skills training programs usually report changes in social functioning in schizophrenia over 1–2 years.90,91 Thus, improved illness self-management, including skills for developing closer relationships with others, could lead to gradual improvements in social support over the longer term. Second, the relatively small amount of time devoted in the IMR program to improving social support (1 out of 9 modules) may be insufficient to make an impact on social relationships. Social skills training has the best track record for improving social functioning in schizophrenia,92 with programs usually involving a minimum of 3–6 months of concerted skills training, considerably more than is provided in IMR.
Third, it is possible that more could be done in the IMR program to help clients collaborate actively with significant others in learning how to manage their psychiatric illness. Although collaboration with significant others is identified as a core feature of IMR,53 anecdotal reports indicate that such collaboration occurs in only a minority of clients who participate in the program. Because social contact with others and social support are established predictors of the course of schizophrenia93–95 and family psychoeducation reduces relapses and rehospitalizations,96 developing additional strategies in the IMR program to foster collaboration with significant others is an important priority.
One possible strategy is to formally incorporate into training programs for IMR clinicians skills for collaborating with families (and other significant persons). Another strategy would be to offer a regular multifamily psychoeducational group (eg, monthly), with topics based on the IMR curriculum, for participants in the IMR program and their significant others. This group could provide an opportunity to review the fundamentals of illness management with concerned others in a context where clients could get support and help in pursuing their personal recovery goals.
In summary, these pilot data support the feasibility of implementing the IMR program for clients with schizophrenia receiving services at typical community mental health center settings and suggest that participation in the program is associated with benefits in illness management, progress toward recovery, and improved functioning. These findings suggest that controlled research is the next step toward evaluating the effects of the IMR program. Such research might be undertaken with several considerations in mind. First, assessments should focus on both traditional domains of illness management, such as symptoms and rehospitalizations, and outcomes related to both the subjective and objective aspects of recovery, such as community functioning, social relationships, personal empowerment, and sense of purpose. Qualitative assessments of the experience of recovery would be an additional welcome feature that could illuminate the process of growing “beyond the catastrophic effects of mental illness.”12 Second, as the IMR program is aimed at helping clients develop skills for managing their illness and pursuing personal goals, follow-up assessments are needed to determine whether gains continue to accrue after the program has ended, such as 9–12 months later. Third, given that one of the main goals of IMR is to reduce relapses and associated acute care services, attention to the effects of the program on reducing the costs associated with such services would be of interest.
Several limitations of this study should be noted. Although experienced clinicians provided IMR services to the individuals and groups in these settings, the IMR program was new to these clinicians, and the data reported here are from those early treatment experiences. With more practice and experience with the IMR model, it is plausible that clinicians would become more effective and would improve treatment retention and outcomes. The sample was predominantly Caucasian, indicating that work is needed on more racially-ethnically diverse populations. In addition, ratings of clients' functioning were not obtained by blinded interviews, but rather by clinicians who were familiar with the clients, and may have been biased in their ratings of improvement. These limitations notwithstanding, the present study provides a basis for cautious optimism that the marriage between focusing on recovery and learning to manage one's psychiatric illness may be a fruitful approach to empowering clients to take control over their illness and achieving personally important goals.
References
- 1.Lehman, AF and Steinwachs, DM. Translating research into practice: the schizophrenia Patient Outcomes Research Team (PORT) treatment recommendations. Schizophr Bull 1998. ;241–10. [DOI] [PubMed] [Google Scholar]
- 2.Lehman, AF and Steinwachs, DM. Patterns of usual care for schizophrenia: initial results from the schizophrenia Patient Outcomes Research Team (PORT) client survey. Schizophr Bull 1998. ;2411–20. [DOI] [PubMed] [Google Scholar]
- 3.National Institute of Mental Health. Bridging Science and Service: A Report by the National Advisory Mental Health Council's Clinical Treatment and Services Research Workgroup 1999. Rockville, Md: Author.
- 4.US Surgeon General. Surgeon General's Report on Mental Health 2000. Washington, DC: US Government Printing Office.
- 5.President's New Freedom Commission on Mental Health. Achieving the Promise: Transforming Mental Health Care in America. Final Report 2003. Rockville, Md: Substance Abuse and Mental Health Services Administration DHHS Publication SMA-03-3832.
- 6.Ciompi, L. The natural history of schizophrenia in the long term. Br J Psychiatry 1980. ;136413–420. [DOI] [PubMed] [Google Scholar]
- 7.Harding, CM, Brooks, GW, Ashikaga, T, Strauss, JS, Breier, A. The Vermont longitudinal study of persons with severe mental illness: I. Methodology, study sample and overall status 32 years later. Am J Psychiatry 1987. ;144718–726. [DOI] [PubMed] [Google Scholar]
- 8.Harding, CM, Brooks, GW, Ashikaga, T, Strauss, JS, Breier, A. The Vermont longitudinal study of persons with severe mental illness: II. Long-term outcome of subjects who retrospectively met DSM-III criteria for schizophrenia. Am J Psychiatry 1987. ;144727–735. [DOI] [PubMed] [Google Scholar]
- 9.DeSisto, MJ, Harding, CM, McCormick, RV, Ashikaga, T, Brooks, GW. The Maine and Vermont three-decade studies of serious mental illness. Br J Psychiatry 1995. ;167331–342. [DOI] [PubMed] [Google Scholar]
- 10.Ohaeri, JU. Long-term outcome of treated schizophrenia in a Nigerian cohort. Retrospective analysis of 7-year follow-ups. J Nerv Ment Dis 1993. ;181514–516. [DOI] [PubMed] [Google Scholar]
- 11.Tsuang, M and Winokur, G. The Iowa 500: field work in a 35-year follow-up of depression, mania and schizophrenia. Can Psychiatr Assoc J 1975. ;20359–365. [DOI] [PubMed] [Google Scholar]
- 12.Anthony, WA. Recovery from mental illness: the guiding vision of the mental health service system in the 1990s. Psychosoc Rehabil J 1993. ;1611–23. [Google Scholar]
- 13.Deegan, PE. Recovery: the lived experience of rehabilitation. Psychosoc Rehabil J 1988. ;1111–19. [Google Scholar]
- 14.Mead, S and Copeland, ME. What recovery means to us: consumers' perspectives. Community Ment Health J 2000. ;36315–328. [DOI] [PubMed] [Google Scholar]
- 15.Noordsy, DL, Torrey, WC, Mueser, KT, Mead, S, O'Keefe, CO, Fox, L. Recovery from severe mental illness: an interpersonal and functional outcome definition. Int Rev Psychiatry 2002. ;14318–326. [Google Scholar]
- 16.Ridgway, PAE. The Recovery Papers 2000. Lawrence, KS: University of Kansas School of Social Welfare Vol ;1.
- 17.Beale, V and Lambric, T. The Recovery Concept: Implementation in the Mental Health System: A Report by the Community Support Program Advisory Committee 1995. Columbus, Ohio: Department of Mental Health, Office of Consumer Services.
- 18.Frese, FJ and Davis, WW. The consumer-survivor movement, recovery, and consumer professionals. Prof Psychol Res Pract 1997. ;28243–245. [Google Scholar]
- 19.Davidson, L. Living Outside Mental Illness: Qualitative Studies of Recovery in Schizophrenia 2003. New York: New York University Press.
- 20.Roe, D and Chopra, M. Beyond coping with mental illness: toward personal growth. Am J Orthopsychiatry 2003. ;73334–344. [DOI] [PubMed] [Google Scholar]
- 21.Holman, H and Lorig, K. Patients as partners in managing chronic disease: partnership is a prerequisite for effective and efficient health care [comment]. BMJ 2000. ;320526–527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Newman, S, Steed, L, Mulligan, K. Self-management interventions for chronic illness. Lancet 2004. ;3641523–1537. [DOI] [PubMed] [Google Scholar]
- 23.Von Korff, M, Gruman, J, Schaefer, J, Curry, SJ, Wagner, EH. Collaborative management of chronic illness. Ann Intern Med 1997. ;1271097–1102. [DOI] [PubMed] [Google Scholar]
- 24.Stewart, M, Brown, JB, Donner, A, McWhinney, IR, Oates, J, Weston, WW. The impact of patient-centered care on patient outcomes. J Fam Pract 2000. ;49796–804. [PubMed] [Google Scholar]
- 25.Carpinello, SE, Knight, E, Jatulis, LL. A Study of the Meaning of Self-Help, Self-Help Group Processes, and Outcomes. Third Annual Meeting of the National Association of State Mental Health Program Directors (NASMHPD) 1992. Alexandria, VA: NASMHPD Research Institute Inc.
- 26.Chien, CF, Steinwachs, DM, Lehman, AF, Fahey, M, Skinner, EA. Provider continuity and outcomes of care for persons with schizophrenia. Ment Health Serv Res 2000. ;2201–211. [Google Scholar]
- 27.Ralph, RO. Recovery. Psychiatr Rehabil Skills 2000. ;4480–517. [Google Scholar]
- 28.Curson, DA, Patel, M, Liddle, PF, Barnes, TRE. Psychiatric morbidity of a long stay hospital population with chronic schizophrenia and implications for future community care. BMJ 1988. ;297819–822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kane, JM. Treatment resistant schizophrenic patients. J Clin Psychiatry 1996. ;57suppl 935–40. [PubMed] [Google Scholar]
- 30.Kane, JM and Marder, SR. Psychopharmacologic treatment of schizophrenia. Schizophr Bull 1993. ;19287–302. [DOI] [PubMed] [Google Scholar]
- 31.Harrow, M and Silverstein, ML. Psychotic symptoms in schizophrenia after the acute phase. Schizophr Bull 1977. ;3608–616. [DOI] [PubMed] [Google Scholar]
- 32.Lindenmayer, J-P. Treatment refractory schizophrenia. Psychiatr Q 2000. ;71373–384. [DOI] [PubMed] [Google Scholar]
- 33.Birchwood, M, Mason, R, MacMillian, F, Healy, J. Depression, demoralization and control over psychotic illness: a comparison and non-depressed patients with a chronic psychosis. Psychol Med 1993. ;23387–395. [DOI] [PubMed] [Google Scholar]
- 34.Garety, P, Kuipers, E, Fowler, D, Chamberlain, F, Dunn, G. Cognitive behavior therapy for drug resistant psychosis. Br J Med Psychol 1994. ;67259–271. [DOI] [PubMed] [Google Scholar]
- 35.Johnson, DAW. Studies of depression in schizophrenia. Br J Psychiatry 1981. ;13989–101. [DOI] [PubMed] [Google Scholar]
- 36.Mueser, KT, Douglas, MS, Bellack, AS, Morrison, RL. Assessment of enduring deficit and negative symptom subtypes in schizophrenia. Schizophr Bull 1991. ;17565–582. [DOI] [PubMed] [Google Scholar]
- 37.Angell, B and Test, MA. The relationship of clinical factors and environmental opportunities to social functioning in young adults with schizophrenia. Schizophr Bull 2002. ;28259–271. [DOI] [PubMed] [Google Scholar]
- 38.Norman, RM, Malla, AK, Cortese, L, et al. Symptoms and cognition as predictors of community functioning: a prospective analysis. Am J Psychiatry 1999. ;156400–405. [DOI] [PubMed] [Google Scholar]
- 39.McGurk, SR and Mueser, KT. Cognitive functioning, symptoms, and work in supported employment: a review and heuristic model. Schizophr Res 2004. ;70147–174. [DOI] [PubMed] [Google Scholar]
- 40.Racenstein, JM, Harrow, M, Reed, R, Martin, E, Herbener, E, Penn, DL. The relationship between positive symptoms and instrumental work functioning in schizophrenia: a 10-year follow-up study. Schizophr Res 2002. ;5695–103. [DOI] [PubMed] [Google Scholar]
- 41.Marwaha, S and Johnson, S. Schizophrenia and employment: a review. Soc Psychiatry Psychiatr Epidemiol 2004. ;39337–349. [DOI] [PubMed] [Google Scholar]
- 42.McQuilken, M, Zahniser, JH, Novak, J, Starks, RD, Olmos, A, Bond, GR. The work project survey: consumer perspectives on work. J Vocat Rehabil 2003. ;1859–68. [Google Scholar]
- 43.Mueser, KT, Salyers, MP, Mueser, PR. A prospective analysis of work in schizophrenia. Schizophr Bull 2001. ;27281–296. [DOI] [PubMed] [Google Scholar]
- 44.Rogers, ES, Anthony, WA, Toole, J, Brown, MA. Vocational outcomes following psychosocial rehabilitation: a longitudinal study of three programs. J Vocat Rehabil 1991. ;121–29. [Google Scholar]
- 45.Rogers, ES, Walsh, D, Masotta, L, Danley, K. Massachusetts Survey of Client Preferences for Community Support Services (Final Report) 1991. Boston, Mass: Center for Psychiatric Rehabilitation.
- 46.Bond, GR, Becker, DR, Drake, RE, et al. Implementing supported employment as an evidence-based practice. Psychiatr Serv 2001. ;52313–322. [DOI] [PubMed] [Google Scholar]
- 47.Carling, PJ. Return to Community: Building Support Systems for People With Psychiatric Disabilities 1995. New York, NY: Guilford Publications.
- 48.Geller, JL. The last half-century of psychiatric services as reflected in Psychiatric Services. Psychiatr Serv 2000. ;5141–67. [DOI] [PubMed] [Google Scholar]
- 49.McGrew, JH, Wright, E, Pescosolido, B. Closing of a state hospital: an overview and framework for a case study. J Behav Health Serv Res 1999. ;26236–245. [DOI] [PubMed] [Google Scholar]
- 50.Wong, YI and Solomon, PL. Community integration of persons with psychiatric disabilities in supportive independent housing: a conceptual model and methodological considerations. Ment Health Serv Res 2002. ;413–28. [DOI] [PubMed] [Google Scholar]
- 51.Mann, SB. Talking through medication issues: one family's experience. Schizophr Bull 1999. ;25407–409. [DOI] [PubMed] [Google Scholar]
- 52.Day, JC, Bentall, RP, Roberts, C, et al. Attitudes toward antipsychotic medication: the impact of clinical variables and relationships with health professionals. Arch Gen Psychiatry 2005. ;62717–724. [DOI] [PubMed] [Google Scholar]
- 53.Gingerich, S and Mueser, KT. Illness management and recovery. In Drake, RE, Merrens, MR, Lynde, DW (Eds.). Evidence-Based Mental Health Practice: A Textbook 2005. New York, NY: Norton pp. 395–424.
- 54.Drake, RE, Goldman, HH, Leff, HS, et al. Implementing evidence-based practices in routine mental health service settings. Psychiatr Serv 2001. ;52179–182. [DOI] [PubMed] [Google Scholar]
- 55.Mueser, KT, Torrey, WC, Lynde, D, Singer, P, Drake, RE. Implementing evidence-based practices for people with severe mental illness. Behav Modif 2003. ;27387–411. [DOI] [PubMed] [Google Scholar]
- 56.Torrey, WC, Lynde, DW, Gorman, P. Promoting the implementation of practices that are supported by research: the national implementing evidence-based practice project. Child Adolesc Psychiatr Clin N Am 2005. ;14297–306. [DOI] [PubMed] [Google Scholar]
- 57.Mueser, KT, Corrigan, PW, Hilton, D, et al. Illness management and recovery for severe mental illness: a review of the research. Psychiatr Serv 2002. ;531272–1284. [DOI] [PubMed] [Google Scholar]
- 58.Prochaska, JO and DiClemente, CC. The Transtheoretical Approach: Crossing the Traditional Boundaries of Therapy 1984. Homewood, Ill: Dow-Jones/Irwin.
- 59.Prochaska, JO. Systems of Psychotherapy: A Transtheoretical Analysis 1984. Homewood, Ill: Dorsey.
- 60.Corrigan, PW, McCracken, SG, Holmes, EP. Motivational interviews as goal assessment for persons with psychiatric disability. Community Ment Health J 2001. ;37113–122. [DOI] [PubMed] [Google Scholar]
- 61.In Miller, WR and Rollnick, S (Eds.). Motivational Interviewing: Preparing People for Change 2002. New York, NY: Guilford Press.
- 62.Liberman, RP, Mueser, KT, Wallace, CJ, Jacobs, HE, Eckman, T, Massel, HK. Training skills in the psychiatrically disabled: learning coping and competence. Schizophr Bull 1986. ;12631–647. [DOI] [PubMed] [Google Scholar]
- 63.Zubin, J and Spring, B. Vulnerability: a new view of schizophrenia. J Abnorm Psychol 1977. ;86103–126. [DOI] [PubMed] [Google Scholar]
- 64.Derogatis, LR. Brief Symptom Inventory (BSI): Administration, Scoring, and Procedures Manual 3rd ed. 1993. Minneapolis, Minn: National Computer Systems.
- 65.Derogatis, LR. SCL-90-R (rev.) 1977. Baltimore, Md: Johns Hopkins University School of Medicine.
- 66.Coelho, VLD, Strauss, ME, Jenkins, JH. Expression of symptomatic distress by Puerto Rican and Euro-American patients with depression and schizophrenia. J Nerv Ment Dis 1998. ;186477–483. [DOI] [PubMed] [Google Scholar]
- 67.Cyr, JJ, McKenna-Foley, JM, Peacock, E. Factor structure of the SCL-90-R: is there one? J Pers Assess 1985. ;49571–578. [DOI] [PubMed] [Google Scholar]
- 68.Wetherell, JL, Palmer, BW, Thorp, SR, Patterson, TL, Golshan, S, Jeste, DV. Anxiety symptoms and quality of life in middle-aged and older outpatients with schizophrenia and schizoaffective disorder. J Clin Psychiatry 2003. ;641476–1482. [DOI] [PubMed] [Google Scholar]
- 69.Kaplan, RM and Anderson, JP. An integrated approach to quality of life assessment: the general health policy model. In Spilker, B (Ed.). Quality of Life in Clinical Studies 1990. New York, NY: Raven Press pp. 131–149.
- 70.Ware, J and Sherbourne, C. The MOS 36-item short-form health survey (SF-36). Med Care 1992. ;30473–481. [PubMed] [Google Scholar]
- 71.Mueser, KT, Valentiner, DP, Agresta, J. Coping with negative symptoms of schizophrenia: patient and family perspectives. Schizophr Bull 1997. ;23329–339. [DOI] [PubMed] [Google Scholar]
- 72.Mueser, KT and Gingerich, S. Illness Management and Recovery (IMR) Scales. In Campbell-Orde, T, Chamberlin, J, Carpenter, J, Leff, HS (Eds.). Measuring the Promise: A Compendium of Recovery Measures 2005. Cambridge, Mass: Evaluation Center at Human Services Research Institute Vol ;2 pp. 124–132. [Google Scholar]
- 73.Corrigan, PW, Salzer, M, Ralph, R, Sangster, Y, Keck, L. Examining the factor structure of the Recovery Assessment Scale. Schizophr Bull 2004. ;301035–1041. [DOI] [PubMed] [Google Scholar]
- 74.Shern, D, Lee, B, Coen, A. The Colorado Symptom Inventory: A Self-Report Measure for Psychiatric Symptoms 1996. Tampa, Fla: Louis de la Parte Mental Health Institute.
- 75.Rosenberg, M. Conceiving the Self 1979. New York, NY: Basic Books.
- 76.Rogers, ES, Chamberlin, J, Ellison, ML, Crean, T. A consumer-constructed scale to measure empowerment among users of mental health services. Psychiatr Serv 1997. ;481042–1047. [DOI] [PubMed] [Google Scholar]
- 77.Sarason, IG, Levine, HM, Basham, RB, Sarason, BR. Assessing social support: the Social Support Questionnaire. J Pers Soc Psychol 1983. ;44127–139. [Google Scholar]
- 78.Lehman, A, Kernan, E, Postrado, L. Toolkit for Evaluating Quality of Life for Persons With Severe Mental Illness 1995. Baltimore, Md: The Evaluation Center at HSRI.
- 79.Lukoff, D, Nuechterlein, KH, Ventura, J. Manual for the expanded Brief Psychiatric Rating Scale (BPRS). Schizophr Bull 1986. ;12594–602. [Google Scholar]
- 80.Schmook, GD, Vollendorf, WD, Gervain, M. Recovery Assessment Scale (RAS). In Campbell-Orde, T, Chamberlin, J, Carpenter, J, Leff, HS (Eds.). Measuring the Promise: A Compendium of Recovery Measures 2005. Cambridge, Mass: Evaluation Center at Human Services Research Institute Vol ;2 pp. 60–64. [Google Scholar]
- 81.Zimet, GD, Powell, SS, Farley, GK, Werkman, S, Berkoff, KA. Psychometric characteristics of the Multidimensional Scale of Perceived Social Support. J Pers Assess 1990. ;55610–617. [DOI] [PubMed] [Google Scholar]
- 82.Vaux, A, Burda, P, Steward, D. Orientation toward utilization of support resources. J Community Psychol 1986. ;14159–170. [Google Scholar]
- 83.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (DSM-IV) 1994. Washington, DC: Author.
- 84.Jones, SH, Thornicroft, G, Coffey, M, Dunn, G. A brief mental health outcome scale-reliability and validity of the Global Assessment of Functioning (GAF). Br J Psychiatry 1995. ;166654–659. [DOI] [PubMed] [Google Scholar]
- 85.Söderberg, P, Tungström, S, Armelius, BA. Special section on the GAF: reliability of Global Assessment of Functioning ratings made by clinical psychiatric staff. Psychiatr Serv 2005. ;56434–438. [DOI] [PubMed] [Google Scholar]
- 86.Falloon, IRH and Talbot, RE. Persistent auditory hallucinations: coping mechanisms and implications for management. Psychol Med 1981. ;11329–339. [DOI] [PubMed] [Google Scholar]
- 87.Wahass, S and Kent, G. Coping with auditory hallucinations: a cross-cultural comparison between western (British) and non-western (Saudi Arabian) patients. J Nerv Ment Dis 1997. ;185664–668. [DOI] [PubMed] [Google Scholar]
- 88.Tarrier, N, Beckett, R, Harwood, S, Baker, A, Yusupoff, L, Ugarteburu, I. A trial of two cognitive behavioural methods of treating drug-resistant residual psychotic symptoms in schizophrenic patients: I. Outcome. Br J Psychiatry 1993. ;162524–532. [DOI] [PubMed] [Google Scholar]
- 89.Deegan P. Recovery and the conspiracy of hope. Sixth Annual Mental Health Conference of Australia and New Zealand; September 1996; Brisbane, Australia.
- 90.Glynn, SM, Marder, SR, Liberman, RP, et al. Supplementing clinic-based skills training with manual-based community support sessions: effects on social adjustment of patients with schizophrenia. Am J Psychiatry 2002. ;159829–837. [DOI] [PubMed] [Google Scholar]
- 91.Marder, SR, Wirshing, WC, Mintz, J, et al. Two-year outcome for social skills training and group psychotherapy for outpatients with schizophrenia. Am J Psychiatry 1996. ;1531585–1592. [DOI] [PubMed] [Google Scholar]
- 92.Bellack, AS. Skills training for people with severe mental illness. Psychiatr Rehabil J 2004. ;27375–391. [DOI] [PubMed] [Google Scholar]
- 93.Bebbington, P and Kuipers, L. Life events and social factors. In Kavanagh, DJ (Ed.). Schizophrenia: An Overview and Practical Handbook 1992. London, England: Chapman & H all pp. 126–144.
- 94.Erickson, DH, Beiser, M, Iacono, WG, Fleming, JAE, Lin, T. The role of social relationships in the course of first-episode schizophrenia and affective psychosis. Am J Psychiatry 1989. ;1461456–1461. [DOI] [PubMed] [Google Scholar]
- 95.Strauss, JS and Carpenter, WT. Prediction of outcome in schizophrenia III. Five-year outcome and its predictors. Arch Gen Psychiatry 1977. ;34159–163. [DOI] [PubMed] [Google Scholar]
- 96.Pitschel-Walz, G, Leucht, S, Bäuml, J, Kissling, W, Engel, RR. The effect of family interventions on relapse and rehospitalization in schizophrenia: a meta-analysis. Schizophr Bull 2001. ;2773–92. [DOI] [PubMed] [Google Scholar]