Summary
Neurovascular development requires communication between two developing organs, the neuroepithelium and embryonic blood vessels. We investigated the role of VEGF-A signaling in the embryonic crosstalk required for ingression of angiogenic vessel sprouts into the developing neural tube. As the neural tube develops, blood vessels enter at specific points medially and ventrally from the surrounding perineural vascular plexus. Localized ectopic expression of heparin-binding VEGF165 or VEGF189 from the developing avian neural tube resulted in supernumerary blood vessel ingression points and disrupted vessel patterning. By contrast, localized ectopic neural expression of non-heparin-binding VEGF121 did not produce supernumerary blood vessel ingression points, although the vessels that entered the neural tube became dysmorphogenic. Localized loss of endogenous VEGF-A signaling in the developing neural tube via ectopic expression of the VEGF inhibitor sFlt-1 locally blocked blood vessel ingression. The VEGF pathway manipulations were temporally controlled and did not dramatically affect neural tube maturation and dorsal-ventral patterning. Thus, neural-derived VEGF-A has a direct role in the spatially localized molecular crosstalk that is required for neurovascular development and vessel patterning in the developing neural tube.
Keywords: Vessel patterning, Vessel ingression, Neurovascular crosstalk, VEGF signaling, VEGF isoforms, Soluble Flt-1
INTRODUCTION
A properly patterned network of blood vessels is crucial to embryonic development, as this network supplies nutrients and oxygen to developing organ systems within the embryo. Embryonic blood vessels pattern reproducibly in both space and time, indicating that molecular cues emanating from other embryonic organs shape the vasculature and are also highly regulated (for reviews, see Hogan and Bautch, 2004; Coultas et al., 2005). Although it is known that the developing vasculature responds to spatial cues from other embryonic structures to produce a functional vessel network, relatively little is known about how this crosstalk is established and regulated.
The central nervous system (CNS) is initially devoid of blood vessels and blood vessel precursors, so communication between the developing CNS and the developing vasculature outside the CNS is essential for proper development of the brain and spinal cord. The brain and neural tube recruit blood vessels by inducing the proliferation, migration and differentiation of angioblasts and endothelial cells from the adjacent presomitic mesoderm and the lateral plate mesoderm (Pardanaud and Dieterlen-Lievre, 1993; Wilting et al., 1995; Klessinger and Christ, 1996; Kurz et al., 1996; Pardanaud et al., 1996; Ambler et al., 2001; Hogan et al., 2004). A ring of vessels, known as the peri-neural vascular plexus (PNVP), initially forms around the CNS. Subsequently, vessels invade the neural tissue through angiogenic sprouting, and in avian neural tubes single angioblast migration into the dorsal neural tube also contributes to neural vascularization (Kurz et al., 1996). Thus, a vessel network is established within the developing CNS to support further growth and development. As blood vessels enter the neural tube, they migrate along radial glia to move inwards from the lateral surface (Virgintino et al., 1998). In some areas of the CNS, the pattern of blood vessel ingression is highly stereotypical, as originally described by Feeney and Watterson (Feeney and Watterson, 1946), suggesting that neural-derived spatial cues regulate the patterning of ingressing vessels. Although there is recent evidence that endothelial cells may respond to intrinsic transcription factor programs to pattern in the telencephalon (Vasudevan et al., 2008), this paradigm is unlikely to be operative in the neural tube where internal vessels arise from nearby surface vessels.
Several signaling pathways are involved in embryonic vascular patterning, including VEGF-A (VEGF), Notch, ephrin and semaphorins (for reviews, see Hogan and Bautch, 2004; Carmeliet and Tessier-Lavigne, 2005; Eichmann et al., 2005). Target tissues produce ligands that interact with receptors expressed on angioblasts or endothelial cells, and these interactions impart attractive or repulsive cues that pattern blood vessels. This paradigm, however, is difficult to demonstrate in the developing nervous system, because most of the relevant signaling pathways have roles in both the neural and vascular compartments (for reviews, see Carmeliet and Tessier-Lavigne, 2005; Lambrechts and Carmeliet, 2006). For example, genetic manipulation of components of the VEGF-A (VEGF) signaling pathway indicates a positive role for the pathway in neurovascular crosstalk, but the exact role of VEGF signaling in vascular versus nervous tissue is unclear. Global deletion of VEGF-A or its major signaling receptor Flk-1 (VEGFR-2) is embryonic lethal early in development (Shalaby et al., 1995; Carmeliet et al., 1996; Ferrara et al., 1996), precluding analysis of neurovascular interactions. Reduction of VEGF signaling from the developing CNS can be achieved by conditional deletion of VEGF-A using a nestin-Cre deletor strain. This produces a reduced density of blood vessel branching with moderate reduction of VEGF-A signal, while a more profound reduction leads to neuronal apoptosis and lethality (Haigh et al., 2003; Raab et al., 2004). Genetic deletion of a VEGF-A co-receptor, neuropilin 1 (NRP1), results in appropriate vessel ingression but reduced lateral branching in the sub-ventricular zone (Gerhardt et al., 2004), whereas endothelial-specific deletion of NRP1 results in large unbranched vessels in the brain, indicating a role for NRP1 in vessel branching and morphogenesis after ingression (Gu et al., 2003).
VEGF-A RNA is alternatively spliced to yield several major isoforms, and different isoforms have differential affinity for the extracellular matrix. VEGF165 and VEGF189 interact moderately or strongly with the matrix via heparin-binding domains, whereas VEGF121 does not have heparin-binding properties and is more diffusible (Park et al., 1993). Analysis of mice that express individual VEGF-A isoforms shows that vessel morphogenesis is affected by these perturbations (Ruhrberg et al., 2002; Stalmans et al., 2002). VEGF120/120 embryos have larger diameter vessels that branch less often than normal, whereas VEGF188/188 embryos have smaller diameter vessels that branch more often than normal. However, embryos expressing single VEGF-A isoforms supported vessel ingression into the CNS.
We have previously shown that endothelial cells of presomitic mesoderm origin make a significant contribution to the PNVP (Ambler et al., 2001), and that VEGF signaling is important in this process (Ambler et al., 2003; Hogan et al., 2004). Ectopically grafted neural tubes recruited a PNVP, and an explant model was used to show that neural tube derived VEGF-A is required for formation of a vascular plexus from presomitic mesoderm. Here, we address the role of VEGF-A signaling in the next step of neurovascular communication: the ingression of blood vessels into the developing neural tube. We show that locally mis-expressed heparin-binding VEGF-A isoforms induce ectopic ingression of blood vessels into the neural tube, and that local blockade of endogenous VEGF-A prevents vessel ingression in a spatially restricted manner. These perturbations are temporally controlled and do not dramatically affect the patterning of the neuronal populations of the developing neural tube, indicating that direct communication between neural tissue and developing vessels via VEGF-A signaling is crucial to proper and patterned blood vessel ingression into the neural tube.
MATERIALS AND METHODS
Expression vectors
The human VEGF121, VEGF165 and VEGF189 cDNAs (gift of J. Abraham) (Tischer et al., 1991) were inserted into the pCAGGS-IRES2-nucEGFP (pCIG) vector (Megason and McMahon, 2002) (gift of L. Pevny and A. McMahon) between the PstI and SmaI sites (VEGF121 and VEGF165) or the EcoRI and PstI sites (VEGF189) to make the VEGF expression vectors pCIG-VEGF121, pCIG-VEGF165 and pCIG-VEGF189. Mouse soluble Flt1 cDNA (Kappas et al., 2008) was inserted into the EcoRI site of the pCIG vector, generating pCIG-sFlt-1.
In ovo quail electroporation
Hamburger and Hamilton stage 16-18 (HH 16-18) Japanese quail embryos (Coturnix japonica, Ozark Egg Company, Stover, MO) were electroporated in ovo as described previously (Itasaki et al., 1999), with modifications. Briefly, the pCIG control vector (0.5 μg/μl), VEGF121, VEGF165, VEGF189 (0.2 μg/μl), or sFlt-1 (0.5 μg/μl) DNA was suspended in DMEM-F12 media (GIBCO, Grand Island, NY) containing 1× penicillin/streptomycin and 50 ng/ml Fast Green (Sigma, St Louis, MO). Approximately 1 nl was injected, to fill the posterior lumen of the neural tube. Electroporation was with three pulses (50 milliseconds each) of 20 mV using a BTX ECM830 Square Electroporator (Harvard Apparatus, Holliston, MA) equipped with 3 mm gold-tipped, L-shaped BTX genetrode electrodes (Genetronics) that flanked the neural tube. Eggshells were taped and embryos developed an additional 48 hours at 37°C before dissection into cold PBS. Embryos were viewed under an Olympus IX-50 epifluorescence microscope (Opelco, Sterling, VA) to visualize DNA incorporation via GFP expression.
Immunofluorescence and analysis of ingression patterns
At stage HH 25-26, embryos were dissected from the yolk and fixed for 1-2 hours in 4% PFA (paraformaldehyde)/PBS at 4°C, rinsed in cold PBS, then washed for 1 hour in PBS on ice. Embryos were incubated in 30% sucrose/PBS overnight at 4°C, then embedded in OCT media (TissueTEK, Sakura Finetek, Torrance, CA), and 12 μm sections through the upper-limb level (thoracic neural tube just posterior to the heart) were cut with a cryostat (Microm HM505E, Germany). Frozen sections were washed in PBS, briefly blocked in antibody staining solution containing: 1× PBS, 0.1% Triton X-100 (Sigma), 1% heat-inactivated goat serum (GIBCO), then incubated in antibody staining solution and primary antibody overnight at 4°C. Monoclonal mouse antibodies to Pax7, Pax6 and MNR2 were used at a concentration of 1:50 [obtained from the Developmental Studies Hybridoma Bank (DSHB) developed under the auspices of the NICHD and maintained by The University of Iowa Department of Biological Sciences, Iowa City, IA 52242]. QH1 (DSHB), transitin (DSHB) and anti-β-Tubulin type III (Tuj1, Covance, Emeryville, CA) were used at a concentration of 1:500. Sections were rinsed twice in antibody staining solution, then incubated with anti-mouse IgG conjugated Cy3 (Sigma) for 2 hours at room temperature at a concentration of 1:250. Mounted sections were visualized with an Olympus IX-50 epifluorescence microscope and images were acquired with an Olympus DP71 digital camera (Center Valley, PA).
Ingression patterns were analyzed quantitatively as follows. A 1 mm region of quail neural tube, starting at the upper limb, was sectioned. Cryostat sections (12 μm) were taken at intervals of approximately 72 μm and stained with QH1. Vessel ingression points were scored when a clear vascular connection from the PNVP into the neural tube was noted. Angle measurements of ingressing angiogenic sprouts were calculated for each image by drawing a center line through the lumen of the neural tube from the floor plate to the roof plate and locating the center point of this line. To determine the location of angiogenic sprouts, we plotted the angle of ingression from the initiation point of each sprout to the center, then down to the ventral-most point. Angles were then measured using Metamorph software. The ventral-most point along the center line is labeled 0°, whereas the dorsal-most point is 180° (Fig. 2A). Angles were binned into each 10° of arc. In each group, five embryos were analyzed and the total number of ingression points in each 10° of arc plotted on a graph.
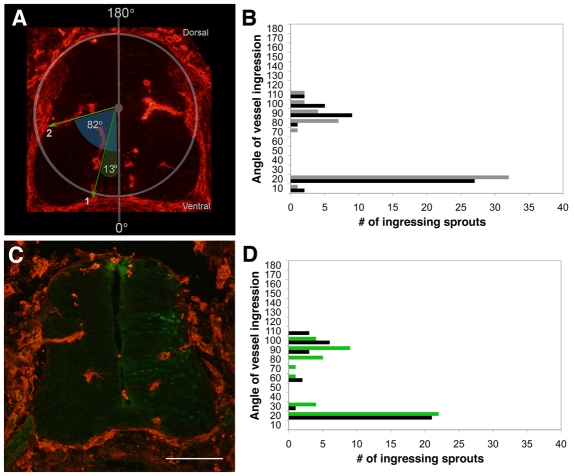
Fig. 2.
Quantitative analysis of angiogenic sprouting into the developing neural tube reveals stereotypical ingression points. Unperturbed quail embryos and embryos whose neural tubes were electroporated with eGFP control DNA at HH stage 16-18 were serially sectioned at stage HH 25-26 through the upper limb. Every sixth 12 μm section was stained for QH1 (red). Fourteen images were analyzed for each embryo as described in the Materials and methods. (A) Unperturbed quail embryo section stained with QH1 to illustrate blood vessel analysis strategy. (B) Total number of angiogenic sprouts within the left (gray) and right (black) neural tube halves of five unperturbed embryos. There were concentrations of ingression points between 0-20° (ventral ingression points) and 70-110° (medial ingression points). (C) Representative image of a quail neural tube electroporated with eGFP DNA (electroporated side to the right). (D) Total number of ingressing angiogenic sprouts within the neural tubes of five control embryos electroporated with eGFP DNA (green); untransfected control contralateral neural tube side (black). Scale bar: 100 μm.
In situ hybridization
cDNAs were generated from quail genomic DNA obtained from whole embryos (HH 23). Published quail VEGF (qVEGF) primer sequences were used to amplify fragments of qVEGF166 cDNA (Flamme et al., 1995). The fragment was gel-extracted and ligated into the pCR-Blunt II-TOPO vector (Invitrogen, Carlsbad, CA). Quail VEGF166 antisense probe was amplified using the SP6 promoter according to manufacturer's instructions (Roche, Indianapolis, IN). In situ hybridization was performed as described (Colbert et al., 1995), with minor modifications, on 20 μm transverse sections cut with a cryostat.
RNA analysis
Neural tubes electroporated on day 3 were harvested on day 5, and three to five neural tubes/construct were pooled. Total RNA was isolated using Trizol (Invitrogen) and cDNA was generated as described (Kappas et al., 2008). Equivalent amounts of cDNA were amplified using human VEGF-A (hVEGF-A) primers that spanned the alternative splice region, and PCR products were visualized by agarose gel electrophoresis and normalized to GFP. The primers used were: forward hVEGF-A, 5′-CTGCTGTCTTGGGTGCATTGG-3′; reverse hVEGF-A, 5′-TCACCGCCTCGGCTTGTC-3′; eGFP forward, 5′-CCTACGGCGTGCAGTGCTTCAGC-3′; eGFP reverse, 5′-CGGCGAGCTGCACGCTGCGTCCTC-3′.
RESULTS
Blood vessel patterning around and within the quail neural tube
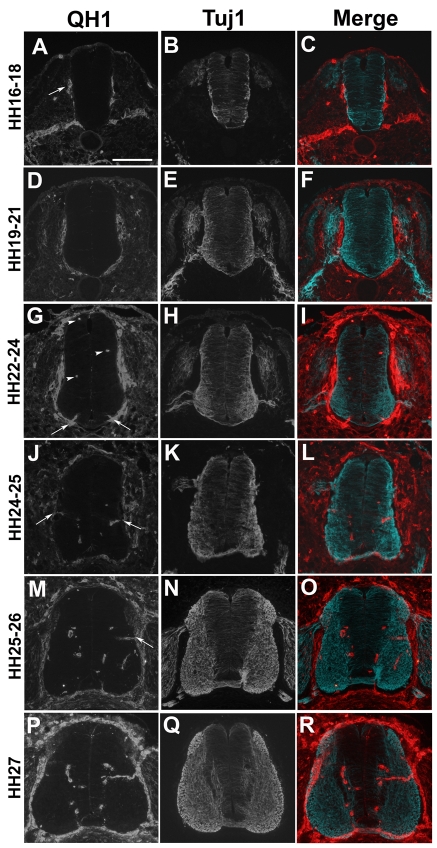
Feeney and Watterson described stereotypical vessel ingression into the embryonic chick neural tube at the cervical level from days 4-16 of development using dye injection (Feeney and Watterson, 1946). Our studies focused on the thoracic level of the quail neural tube between days 3-5 of development. To establish a developmental time frame for major blood vessel patterning events in this area of the neural tube, we performed a time-course analysis of blood vessel patterning in transverse sections at stages HH 16-27, using QH1 immunostaining to visualize both patent vessels and non-patent sprouts (Hamburger and Hamilton, 1951; Pardanaud et al., 1987) (Fig. 1A,D,G,J,M,P). Similar to initial neurovascular patterning events in mouse (Hogan et al., 2004), the perineural vascular plexus (PNVP) begins to form first along the mid-levels of the lateral (pial) surface of the neural tube (Fig. 1A, arrow). As development proceeds, the PNVP becomes progressively more complete (Fig. 1D,G). Dorsal angioblast migration (Fig. 1G, arrowheads) and ventral sprouting (Fig. 1G, arrows) were first observed at stage HH 22-24, and medial angiogenic sprouting was first observed at stage HH 24-25 (Fig. 1J,M, arrows). Angiogenic sprouting from the PNVP never occurred dorsal to the entry site for the DRG (dorsal root ganglia), and vessels were never seen sprouting into the floor plate. These results are consistent with an earlier description of developmental vessel ingression in the cervical region of the quail embryo (Kurz et al., 1996) and with the work of Feeney and Watterson (Feeney and Watterson, 1946), given that events occur earlier in more anterior regions of the CNS.
Fig. 1.
Formation of the PNVP and vessel ingression coordinate with neural differentiation in the quail neural tube. HH stage 16-27 Japanese quail embryos were sectioned in the transverse plane at the thoracic level and stained with either QH1 (red, A,D,G,J,M,P) to label blood vessels or Tuj1 (β tubulin III, blue, B,E,H,K,N,Q) to label differentiated neurons. Merged images (C,F,I,L,O,R) represent two super-imposed, adjacent 12 μm sections at the upper limb level. (A-C) At stage HH 16-18, initiation of PNVP formation correlated with the start of neuronal differentiation and migration of Tuj1-positive neurons to the pial surface of the neural tube. (D-F) At stage HH 19-21, the PNVP continued to develop around the ventral neural tube, whereas motoneurons extended axonal projections from the motor horn, and DRG axons innervated the neural tube at the dorsal root entry zone. (G-I) By stage HH 22-24, PNVP formation was complete. Single QH1-positive angioblasts were noted dorsally and medially (arrowheads), and ventral angiogenic sprouts were seen (arrows) adjacent to the floor plate. (J-L) At stage HH 24-25, angiogenic sprouts from the PNVP formed mediolaterally (arrows) along the dorsal-ventral axis of the neural tube (this vessel ingression site was maintained at later stages, see M and P). (M-O) At stage HH 25-26, both ventral and medial (arrow) vessel ingression sites were noted, along with continued differentiation of Tuj1-positive neurons. (P-R) By stage HH 27, the amount of Tuj1-positive neurons increased, while the vessel ingression pattern established at earlier stages was maintained. Scale bar: 100 μm.
β-Tubulin III was visualized by staining with the TuJ1 antibody on adjacent sections to follow neural development. During early development the neural tube exists primarily as a proliferating pool of neural progenitor cells that maintain connections with both the luminal and pial surfaces of the neural tube. As these cells undergo programmed differentiation, they lose contact with the luminal surface of the neural tube and migrate laterally to the pial surface, where they begin to express β-tubulin III (Fig. 1B,E,H,K,N,Q). At these stages, the Tuj1-positive cells are primarily neurons (Nakai and Fujita, 1994). Angiogenic sprouts ingressed into the Tuj1-positive area, but only in specific medial and ventral regions (compare Fig. 1G-R). Once in the neural tube, angiogenic sprouts avoided the Tuj1-negative medial area that contained proliferative progenitor cells, as described for the hindbrain (Gerhardt et al., 2004). These data suggest that the developing neural tube may influence blood vessel ingression.
Blood vessel ingression into the neural tube is highly stereotypical
To determine the spatial patterning of ingressing blood vessels in the developing neural tube, a region of the quail embryo at the upper limb level (thoracic) was serially sectioned in the transverse plane, stained for QH1 and analyzed as described in the Materials and methods (n=5 embryos). Control analyses showed that the ingression points of angiogenic sprouts within the quail neural tube were highly stereotypical (Fig. 2A,B). Approximately 33% of blood vessels ingressed into the neural tube between 70 and 110 degrees, whereas the remaining 66% of vessels ingressed between 10 and 20 degrees. To determine whether electroporation and/or expression of GFP affected the spatial pattern of vessel ingression, quail neural tubes were electroporated with a vector that only expressed eGFP (Fig. 2C,D). At the time of electroporation (HH stage 16-18, day 3), the DNA enters the cells that line the lumen of the neural tube. The neural cells that acquire DNA are primarily neuroepithelial and radial glia progenitor cells whose descendents form neurons and glial cells such as astrocytes and oligodendrocytes (Leber and Sanes, 1995; Gotz and Huttner, 2005). At this time, no blood vessel sprouts have entered the neural tube, so they are not electroporation targets. Analysis of these embryos at HH stage 25-26 (day 5) showed that the pattern of vessel ingression was similar to that of unperturbed controls, on both the side of the neural tube that expressed eGFP and the contralateral side that received current but no DNA. Thus, these technical manipulations did not affect the spatial pattern of vessel sprouting ingression into the developing neural tube. As in ovo electroporation at these developmental stages ultimately delivered DNA to the medial vessel ingression area of the neural tube more efficiently than to the ventral ingression area, medial blood vessel ingression into the neural tube was further analyzed.
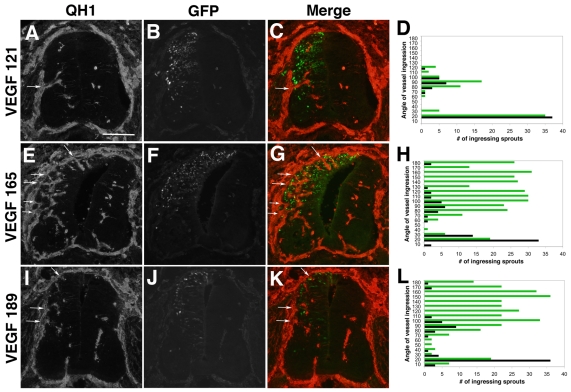
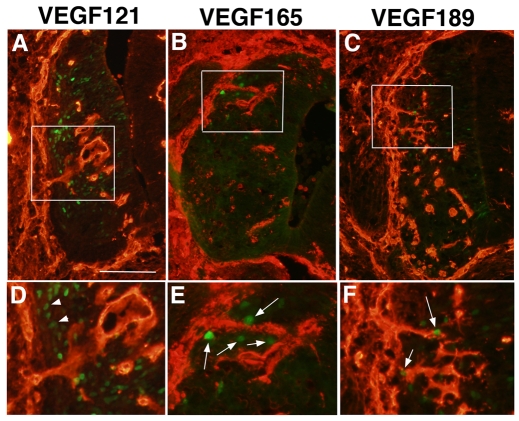
Localized mis-expression of matrix-binding VEGF isoforms alters the neural tube blood vessel ingression pattern
We hypothesized that VEGF-A expressed by the developing neural tube was involved in the ingression of angiogenic sprouts into the tube. We confirmed that VEGF-A was expressed in the quail neural tube at the stages analyzed (see Fig. S1 in the supplementary material), consistent with previous reports (Aitkenhead et al., 1998; Nanka et al., 2006). The pattern of VEGF-A RNA expression did not correlate with specific ingression points. Rather, it was fairly uniform throughout the developing neural tube, with a modest concentration of signal in the floor plate, roof plate and motoneuron area, which are sites blocked to blood vessel ingression (see Fig. S1 in the supplementary material). To analyze the role of individual VEGF isoforms in blood vessel ingression into the developing neural tube, we electroporated DNAs that expressed VEGF121, VEGF165 or VEGF189 from the ubiquitous chicken β-actin promoter into stage HH 16-18 quail neural tubes. The DNAs also expressed eGFP from an IRES sequence, so GFP-positive cells corresponded to cells that expressed the VEGF isoforms. The amount of DNA and the electroporation conditions were titrated to achieve moderate and localized expression of the reporter GFP and VEGF isoform cDNAs, so that the phenotypes could be analyzed in a spatial context. Analysis of human VEGF mRNA in electroporated neural tubes by semi-quantitative RT-PCR indicated that equivalent amounts of each transgene were expressed relative to the GFP signal (see Fig. S2 in the supplementary material). Expression of VEGF121 did not alter the vessel ingression pattern (Fig. 3A-D, n=5 embryos). The pattern was indistinguishable from that seen on the contralateral non-electroporated side and in the controls, although medial ingression points were scored more frequently on the VEGF121-expressing side of the neural tube (Fig. 3D). In some cases, the vessels that ingressed into neural tubes expressing VEGF121 had an increased diameter (data not shown, Fig. 4A and Fig. 5A). By contrast, expression of similar levels of the heparin-binding VEGF-A isoforms VEGF165 or VEGF189 induced ectopic vessel ingression points along the PNVP (Fig. 3E-L, n=5 embryos for each group). Analysis of the ingression points in relation to the cells expressing VEGF165 or VEGF189 showed that ectopic ingression points were localized to areas of the neural tube that contained cells expressing the heparin-binding VEGF isoform (Fig. 4B,C,E,F). By contrast, neural tubes with cells that ectopically expressed VEGF121 showed blood vessel ingression only in the medial region, despite the presence of VEGF121-expressing cells along the dorsoventral axis of the neural tube (Fig. 4A,D).
Fig. 3.
Ectopic expression of heparin-binding VEGF isoforms induces supernumerary vessel ingression points into the developing neural tube. Quail neural tubes were electroporated with hVEGF121-GFP, hVEGF165-GFP or hVEGF189-GFP DNAs (green, panels B, F, J) on day 3 (HH 16-18) and harvested 48 hours later (HH 25-26). Transverse sections were stained with QH1 antibody (red, panels A,E,I) to visualize vessels, and five embryos from each group were analyzed as described (panels D,H,L; green lines, total ingression points for ectopic VEGF-expressing sides of neural tubes at each 10° of arc; black lines, total ingression points for contralateral control sides of the neural tubes at each 10° of arc). C, G and K are a merge of red (QH1) and green (eGFP) channels. (A-C) Quail neural tubes electroporated with hVEGF121 DNA displayed a grossly normal distribution of angiogenic ingression points along the dorsoventral axis of the ectopic VEGF-expressing side of the neural tube (arrows in A,C). (D) The quantitative analysis showed no change in the distribution of ingression points for sprouts between the control (black) and VEGF121-expressing (green) sides of the neural tube, and a slight increase in the frequency of ingression points in the medial region of the VEGF-expressing side of the neural tubes (n=5 embryos). (E-G) Quail neural tubes electroporated with hVEGF165 DNA had ectopic dorsal sprouts (arrows in E,G). (H) The quantitative analysis showed increased distribution and frequency of vessel ingression points in the dorsal region of the hVEGF165-expressing side of the neural tube (green), where ectopic expression is localized (n=5 embryos). (I-K) Quail neural tubes electroporated with hVEGF189 DNA had ectopic dorsal sprouts (arrows in I,K). (L) The quantitative analysis showed increased distribution and frequency of vessel ingression points in the dorsal region of the hVEGF189-expressing side of the neural tube, where ectopic expression is localized (n=5 embryos). Scale bar: 100 μm.
Fig. 4.
Localized ectopic expression of heparin-binding VEGF-A isoforms in the developing neural tube correlates with supernumerary vessel ingression points. Neural tubes processed for QH1 (red) and eGFP (green, reporter for ectopic VEGF-A isoform expression) were examined for the relationship between vessel ingression points and ectopic VEGF-A isoform expression. (A-C) Lower power views to show location of normal (A) or supernumerary (B,C) vessel sprout ingressions on the dorsoventral axis of the neural tube. (D-F) Higher magnification of the boxed areas in A-C. Several eGFP-positive cells that ectopically express heparin-binding hVEGF165 or hVEGF189 are close to the supernumerary vessel sprouts (arrows in E,F), whereas numerous eGFP-positive cells that ectopically express hVEGF121 (arrowheads in D) do not induce supernumerary vessel ingression points. Scale bar: 100 μm in A-C; 50 μm in D-F.
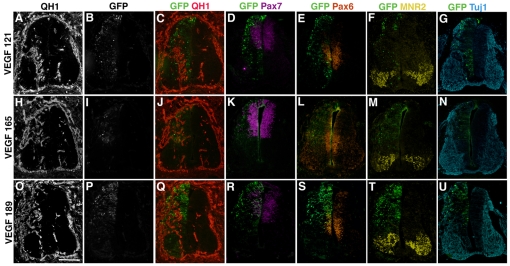
Fig. 5.
Neural patterning is not perturbed in neural tubes that ectopically express VEGF-A isoforms. (A-U) Quail neural tubes were electroporated with (A-G) hVEGF121, (H-N) hVEGF165 and (O-U) hVEGF189 on day 3 (HH 16-18), and harvested 48 hours later (HH 25-26). Neural tubes were sectioned and adjacent sections were stained with antibodies to: QH1 (red, A,H,O,C,J,Q) to visualize vessels; Pax7 (purple, D,K,R) to visualize dorsal neural precursors; Pax6 (orange, E,L,S) to visualize medial neural precursors; MNR2 (yellow, F,M,T) to visualize ventral motoneuron precursors; and Tuj1 (blue, G,N,U) to visualize differentiated neurons. (B,I,P) eGFP expression (green) illustrates the neural tube side expressing ectopic VEGF-A isoforms (left) versus the control contralateral side (right); (C-G,J-N,Q-U) merges of marker and eGFP channels for each section. Scale bar: 100 μm.
We next analyzed several regional markers of neural tube patterning to determine whether ectopic VEGF-A isoform expression affected neural tube development (Fig. 5). Pax7 is expressed in population of dorsal neural progenitors, Pax6 is expressed in a group of medial neural progenitors and MNR2 is a marker for motoneuron progenitors, which are localized to the ventral-most region of the developing neural tube. The localized, moderate expression levels of the VEGF isoforms over 48 hours did not significantly affect the expression patterns of these markers (Fig. 5D-F,K-M,R-T). Thus, VEGF isoforms that interact with the matrix induce ectopic blood vessel sprouting from the PNVP into the developing neural tube and perturb vascular patterning, without significantly affecting neural tube development on the dorsoventral axis.
Because blood vessels migrate along radial glia once they enter the neural tube, we asked whether electroporated neural tubes had perturbed patterning of the radial glia. Staining with the radial glia marker transitin showed that expression of moderate levels of any of the VEGF isoforms did not significantly alter the staining pattern (see Fig. S3 in the supplementary material). Moreover, the radial glia staining pattern on both the electroporated and control sides of the neural tube suggested that radial glia do not selectively associate with ingression points. Instead, the staining indicated that radial glial processes are spaced relatively evenly along the dorsal-ventral axis of the lateral edge of the neural tube (see Fig. S3 in the supplementary material).
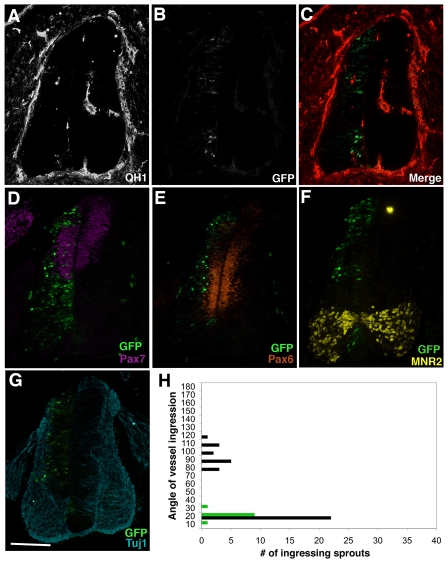
Loss of VEGF signaling from the neural tube blocks vessel ingression
To assess the effect of loss-of-function of the VEGF signaling pathway, we electroporated a soluble Flt-1 (sFlt-1)-expressing cDNA into the developing neural tube. sFlt-1 is a natural splice form of the Flt-1 receptor that can bind and sequester VEGF-A, thus preventing binding of VEGF-A to Flk-1 and downstream signaling (Kendall and Thomas, 1993). In contrast to the supernumerary blood vessel ingressions seen with VEGF isoform over-expression, localized ectopic expression of sFlt-1 led to a complete blockade of vessel ingression in areas of sFlt-1 expression (Fig. 6, n=5 embryos). Relative to the contralateral control side of the neural tube, the sFlt-1-expressing side showed no ingression points in the medial area where sFlt-1 cDNA was expressed, and reduced ingression even in the ventral area of the developing neural tube (Fig. 6A-C,H). Expression of the VEGF-A blocking peptide over a 48-hour period did not significantly affect the dorsoventral patterning of the neural tube (Fig. 6D-G). These findings indicate that endogenous VEGF-A expressed by cells of the developing neural tube is required for the stereotypical ingression of angiogenic blood vessels into the medial and ventral regions.
Fig. 6.
VEGF signaling from the neural tube is required for blood vessel ingression. Quail neural tubes were electroporated with sFlt1-GFP and analyzed as previously described. (A-C) No medial vessel ingression and little ventral vessel ingression was seen in areas of the neural tube that were eGFP positive. (D-G) Neural patterning is not detectably perturbed on the electroporated side of the neural tube (left) based on Pax7 (D, purple), Pax6 (E, orange), MNR2 (F, yellow) and Tuj1 (G, blue) expression patterns. (H) Quantitative analysis of five electroporated neural tubes showed no medial and few ventral vessel ingression points in areas of localized sFlt1 expression (green), compared with the control contralateral side (black) (n=5 embryos). Scale bar: 100 μm.
DISCUSSION
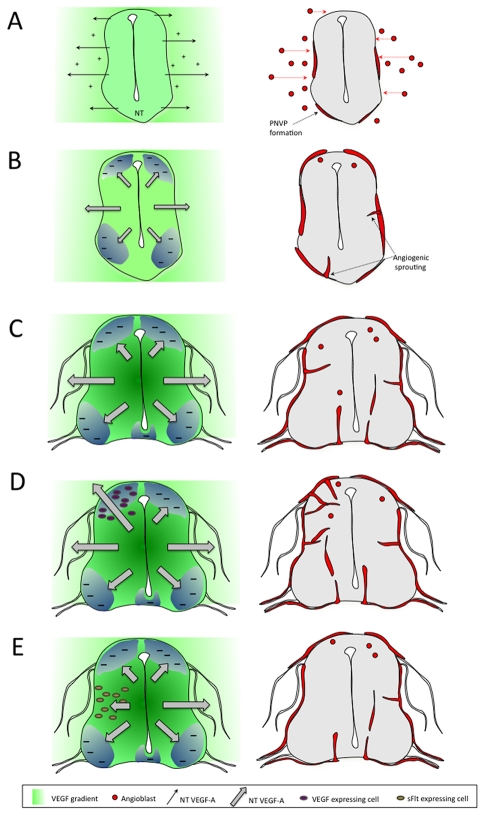
Our results show that VEGF-A signaling is crucial to the communication between the developing neural tube and the developing vascular system. Moreover, here we highlight the precise choreography between neural VEGF-A expression and blood vessel patterning, and we show that a very reproducible pattern of blood vessel ingression depends on proper spatial regulation of VEGF signaling from the neural compartment. The essential aspects of our model are shown in Fig. 7. We have previously shown that neural-tube derived VEGF-A was required for formation of the PNVP that surrounds the developing neural tube (Ambler et al., 2003; Hogan et al., 2004) (Fig. 7A). By manipulating ectopic expression of VEGF-A isoforms or the sFlt-1 inhibitor in time and space, we now reveal a second requirement for neural-derived VEGF-A in blood vessel ingression into the developing neural tube (Fig. 7B-E). This ingression requires VEGF-A at the ingression sites, as local loss via sFlt expression prevents ingression (Fig. 7E). However, VEGF-A localization does not explain why vessels only ingress at specific points along the dorsoventral axis. We hypothesize that stereotypical vessel ingression into the neural tube also uses negative patterning cues (Fig. 7B-E), and this is discussed further below.
Fig. 7.
Model of blood vessel ingression into the developing neural tube. The model covers events of neurovascular patterning between stages HH 16 and HH 26 in the avian embryo, and also shows the VEGF-A perturbations analyzed in this study. (A) At early stages (HH 16-18), VEGF-A isoforms (121, 165, 189) expressed by the developing neural tube set up a gradient that leads to angioblast migration from the lateral plate and presomitic mesoderm to form the PNVP. At this stage, blood vessel ingression does not occur because of insufficient levels of neural tube-derived VEGF-A. (B) At later stages (HH 22-25), increased levels of VEGF165 and VEGF189 are required for blood vessel ingression, but negative patterning cues that are co-expressed prevent ingression except at specific medial and ventral points. (C) By stage HH 26 there are obvious stereotypical blood vessel ingression points medially and ventrally, whereas angioblasts migrate in dorsally. (D) Neural tubes electroporated with VEGF165 or VEGF 189 show ectopic ingression in normally avascular dorsal areas on the electroporated side. (E) Neural tubes electroporated with sFlt-1 do not have ingression at the normal medial site on the electroporated side. For each set of panels, the left side demonstrates the signals and the right side demonstrates the vessel patterning outcome. Symbols are described in the key below the figure.
Why is it important that blood vessels sprout into the developing neural tube at specific places? One possibility is that ingressing vessels must coordinate with neural development and maturation to prevent mis-routing of neural connections and disruption of fasciculation of the axon tracts. For example, the motoneurons form in the ventral part of the neural tube, and their axons subsequently migrate out of the neural tube ventro-laterally to enervate their targets (for a review, see Price and Briscoe, 2004). As axons leave the neural tube they form bundles, and perturbation of either their fasciculation or egression compromises their ability to migrate and properly connect to their targets. Thus, extensive vessel ingression at points of motoneuron egression may compromise the function of the nervous system. Stereotypical ingression patterns of vessels into the neural tube may also be important for efficient functioning of the vascular system. Once angiogenic sprouts enter the neural tube at the medial ingression point, they migrate forward until they reach the sub-ventricular zone that separates differentiated neurons from neural progenitors cells. When they reach this border, they branch and migrate in both the dorsal-ventral and rostral-caudal axes. The rostral-caudal migration leads to interconnections within the neural tube and eventual blood flow (Feeney and Watterson, 1946; Nakao et al., 1988). These interconnections are probably made more efficiently and sooner if the vessels are at the same level on the dorsal-ventral axis, which is accomplished by having a defined medial ingression point.
We used a naturally produced inhibitor of VEGF-A signaling, sFlt-1, to downregulate endogenous VEGF signaling. We and others have shown that this spliced isoform of the sFlt-1 receptor complexes with VEGF-A and competitively inhibits binding to Flk-1 (VEGFR-2) (Kendall and Thomas, 1993; Roberts et al., 2004; Kappas et al., 2008). Because we were able to direct modest expression of sFlt-1 to localized areas within the neural tube for a specific time period, neural degeneration was minimized and neural development and dorsal-ventral patterning was not significantly affected. However, even this modest blockade of VEGF-A signaling was sufficient to block normal vessel ingression dramatically in areas of sFlt-1 expression, revealing an absolute requirement for VEGF-A signaling for proper blood vessel ingression into the developing neural tube. Our preliminary results show that, just as the supernumerary sprouts ingressed locally in conjunction with ectopic VEGF-A expression, the block to ingression produced by sFlt-1 expression was also localized and did not extend significantly beyond areas of sFlt-1 expression (J.M.J. and V.L.B., unpublished). The localized nature of the blockade indicates that sFlt-1 is also a local morphogenetic mediator, as suggested by its ability to bind heparin and thus the surrounding matrix (Park and Lee, 1999).
Localized ectopic expression of the three major VEGF-A isoforms revealed that, although all isoforms perturbed neural tube angiogenesis, VEGF165 and VEGF189 but not VEGF121 were able to induce supernumerary sprouts at locations along the periphery that normally did not allow for sprout ingression. There are two major differences between these VEGF isoforms. VEGF165 and 189 bind heparin and thus can interact with the matrix, whereas VEGF121 does not bind heparin. VEGF165 and presumably VEGF189 can use NRP1 as a co-receptor to enhance signaling through the Flk-1 (VEGFR-2) receptor, whereas VEGF121 binds NRP1 but does not use it as a co-receptor for signaling through VEGFR-2 (Soker et al., 1998; Pan et al., 2007). Deletion of NRP1 affects vascular development (Kawasaki et al., 1999; Gu et al., 2003; Gerhardt et al., 2004). However, ingression of vessels into the CNS is not compromised; the vessel defects in NRP1 mutant neural tubes result from mis-patterning in lateral branching and vessel size increases, indicating that neural tube vessel ingression is not NRP1 dependent (Gu et al., 2003; Gerhardt et al., 2004). Our preliminary results show that co-electroporation of VEGF165 and a soluble form of NRP1 that is predicted to act as a dominant-negative block to NRP1/Flk-1 interactions does not block ectopic ingression of vascular sprouts (J.M.J. and V.L.B., unpublished). Taken together, these findings suggest that NRP1 interactions are not crucial to blood vessel ingression into the neural tube, and that the heparin-binding properties of VEGF165 and 189 confer on these isoforms the ability to induce ectopic ingression points.
The hypothesis that VEGF isoform interactions with the local matrix within the neural tube are crucial to proper vessel ingression is also supported by our finding that ectopic sprouting ingression is localized to areas of the neural tube that contain cells expressing either VEGF165 or VEGF189. When broad areas expressed heparin-binding VEGF ectopically, there were numerous sprouts in these areas. However, even when only a few cells expressed heparin-binding VEGF DNA, supernumerary sprouts correlated with their placement. This finding strongly indicates that heparin-binding VEGF-A is normally deposited near the cells of origin in the neural tube, and this spatial arrangement of VEGF-A contributes to the stereotypical ingression pattern. It also shows that endothelial cells outside the neural tube can sense sources of VEGF-A within the neural tube, over multiple cell diameters, and can overcome normal restraints to ingression if the positive signal is strong enough. Although it is formally possible that VEGF-A signaling could travel over space via a relay system from a localized ligand source, existing data suggest that the gradient hypothesis of VEGF-A signaling is responsible for our findings. This model proposes that a gradient of VEGF-A protein emanating from a source provides a haptotactic slope that directs the migration of angiogenic sprouts. Support for this model was provided by Ruhrberg and colleagues, who showed that VEGF-A protein is concentrated at the midline of the developing hindbrain and decreases in lateral areas (Ruhrberg et al., 2002). The use of a VEGF-A gradient for blood vessel ingression into the developing neural tube is also consistent with our finding that ectopic expression of VEGF121 is not capable of inducing supernumerary vessel ingression points, although once in the neural tube vessels exposed to ectopic VEGF121 become dysmorphogenic. However, mice that express only VEGF120 still exhibit ingression of angiogenic vessels into the developing neural tube (Ruhrberg et al., 2002), although ingression is delayed and ingression points are less dense than in controls (J.M.J. and V.L.B., unpublished). This finding contrasts with our results showing that ectopic expression of VEGF121 does not result in supernumerary vessel ingression into the neural tube. One explanation of this paradox is that in the absence of normal VEGF-A isoforms, VEGF120 forms a `soluble' gradient from its source that can provide instructional information for endothelial sprout migration, although with less efficiency than a gradient formed by heparin-binding VEGF-A isoforms. However, when VEGF121 is overexpressed in the context of a normal gradient it cannot contribute significantly to the positional information conveyed by that gradient.
A model of patterned vessel ingression into the neural tube that only considers VEGF-A, however, is obviously not sufficient to explain the stereotypical pattern we observed. VEGF-A RNA expression is not localized to areas of ingression, but is broadly expressed, with no observable differences along the dorsal-ventral axis at stages when blood vessels ingress at specific medial locations. Moreover, staining for the heparan sulfate proteoglycans that bind VEGF165 and VEGF189 showed uniform expression along the lateral edge of the neural tube, suggesting that VEGF protein is not preferentially localized to ingression points via matrix binding (J.M.J. and V.L.B., unpublished). We thus conclude that VEGF-A is necessary but not sufficient to pattern the angiogenic blood vessels that enter the developing neural tube. Although it is formally possible that the endothelial cells at the ingression points are uniquely able to respond to the VEGF-A signal due to cell-autonomous differences between them and neighboring endothelial cells, our data do not support such a model, as all PNVP endothelial cells seem capable of responding to ectopic expression of heparin-binding VEGF-A. Likewise, a model whereby egression of motor neurons and/or ingression of DRG neurons physically blocks blood vessel ingression does not account for the extensive areas of the floor plate, ventral neural tube, and dorsal neural tube that do not support ingression of the adjacent PNVP vessels. Our data best support a model in which the positive signals emanating from the neural tube are balanced by negative spatial cues that are also produced by the neural tube and prevent ingression both dorsally and ventrally (Fig. 7B-E). Several signaling pathways are candidates to coordinate with VEGF signaling to pattern vessel ingression into the neural tube, based on the expression of the ligands and their ability to negatively influence vessel migration (see review by Eichmann et al., 2005). Among these are the semaphorins that signal through plexins, the slits that signal through robo receptors and netrins that signal through UNC and DCC receptors. Thus, VEGF-A signaling is predicted to provide a positive spatial cue that, when balanced by a negative spatial cue, is neutralized. However, this balance can be tipped in favor of VEGF-A and vessel ingression by ectopic expression of VEGF-A. In our model endothelial cells are capable of a sophisticated reading of incoming cues, and of integrating these cues to produce a behavior that leads to proper neurovascular communication. Moreover, pathologies such as the CCMs (cerebral cavernous malformations) disrupt a unique communication between the neural and vascular compartment (for reviews, see McCarty, 2005; Lok et al., 2007) that begins at the earliest stages of development.
Supplementary material
Supplementary material for this article is available at http://dev.biologists.org/cgi/content/full/136/5/833/DC1
Supplementary Material
We thank Yongquin Wu and the UNC Neurobiology Core for performing the in situ hybridizations, Andy McMahon and Larysa Pevny for the pCIG expression vector, Judith Abraham for the VEGF isoform cDNAs, and Eva Anton for the use of his cryostat. We thank Larysa Pevny and Anthony LaMantia for critical comments on the manuscript, and Daniel Meechan and members of the Bautch laboratory for discussions. This work was supported by grants from the NIH (HL43174 and HL86564) to V.L.B., by T32 (HL69768) NIH Pre-doctoral training grant (J.M.J.) and by a UNC Summer Undergraduate Research Fellowship (S.U.R.F.) to C.G. Deposited in PMC for release after 12 months.
References
- Aitkenhead, M., Christ, B., Eichmann, A., Feucht, M., Wilson, D. J. and Wilting, J. (1998). Paracrine and autocrine regulation of vascular endothelial growth factor during tissue differentiation in the quail. Dev. Dyn. 212, 1-13. [DOI] [PubMed] [Google Scholar]
- Ambler, C. A., Nowicki, J. L., Burke, A. C. and Bautch, V. L. (2001). Assembly of trunk and limb blood vessels involves extensive migration and vasculogenesis of somite-derived angioblasts. Dev. Biol. 234, 352-364. [DOI] [PubMed] [Google Scholar]
- Ambler, C. A., Schmunk, G. A. and Bautch, V. L. (2003). Stem cell-derived endothelial cells/progenitors migrate and pattern in the embryo using the VEGF signaling pathway. Dev. Biol. 257, 205-219. [DOI] [PubMed] [Google Scholar]
- Carmeliet, P. and Tessier-Lavigne, M. (2005). Common mechanisms of nerve and blood vessel wiring. Nature 436, 193-200. [DOI] [PubMed] [Google Scholar]
- Carmeliet, P., Ferreira, V., Breier, G., Pollefeyt, S., Kieckens, L., Gertsenstein, M., Fahrig, M., Vandenhoeck, A., Harpal, K., Eberhardt, C. et al. (1996). Abnormal blood vessel development and lethality in embryos lacking a single VEGF allele. Nature 380, 435-439. [DOI] [PubMed] [Google Scholar]
- Colbert, M. C., Rubin, W. W., Linney, E. and LaMantia, A. S. (1995). Retinoid signaling and the generation of regional and cellular diversity in the embryonic mouse spinal cord. Dev. Dyn. 204, 1-12. [DOI] [PubMed] [Google Scholar]
- Coultas, L., Chawengsaksophak, K. and Rossant, J. (2005). Endothelial cells and VEGF in vascular development. Nature 438, 937-945. [DOI] [PubMed] [Google Scholar]
- Eichmann, A., Makinen, T. and Alitalo, K. (2005). Neural guidance molecules regulate vascular remodeling and vessel navigation. Genes Dev. 19, 1013-1021. [DOI] [PubMed] [Google Scholar]
- Feeney, J. and Watterson, R. (1946). The development of the vascular pattern within the walls of the central nervous system of the chick embryo. J. Morphol. 78, 231-304. [DOI] [PubMed] [Google Scholar]
- Ferrara, N., Carver-Moore, K., Chen, H., Dowd, M., Lu, L., O'Shea, K. S., Powell-Braxton, L., Hillan, K. J. and Moore, M. W. (1996). Heterozygous embryonic lethality induced by targeted inactivation of the VEGF gene. Nature 380, 439-442. [DOI] [PubMed] [Google Scholar]
- Flamme, I., von Reutern, M., Drexler, H. C. A., Syed-Ali, S. and Risau, W. (1995). Overexpression of vascular endothelial growth factor in the avian embryo induces hypervascularization and increased vascular permeability without alterations of embryonic pattern formation. Dev. Biol. 171, 399-414. [DOI] [PubMed] [Google Scholar]
- Gerhardt, H., Ruhrberg, C., Abramsson, A., Fujisawa, H., Shima, D. and Betsholtz, C. (2004). Neuropilin-1 is required for endothelial tip cell guidance in the developing central nervous system. Dev. Dyn. 231, 503-509. [DOI] [PubMed] [Google Scholar]
- Gotz, M. and Huttner, W. (2005). The cell biology of neurogenesis. Nat. Rev. Mol. Cell Biol. 6, 777-788. [DOI] [PubMed] [Google Scholar]
- Gu, C., Rodriguez, E. R., Reimert, D. V., Shu, T., Fritzsch, B., Richards, L. J., Kolodkin, A. L. and Ginty, D. D. (2003). Neuropilin-1 conveys semaphorin and VEGF signaling during neural and cardiovascular development. Dev. Cell 5, 45-57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haigh, J. J., Morelli, P. I., Gerhardt, H., Haigh, K., Tsien, J., Damert, A., Miquerol, L., Muhlner, U., Klein, R., Ferrara, N. et al. (2003). Cortical and retinal defects caused by dosage-dependent reductions in VEGF-A paracrine signaling. Dev. Biol. 262, 225-241. [DOI] [PubMed] [Google Scholar]
- Hamburger, V. and Hamilton, H. L. (1951). A series of normal stages in the development of the chick embryo. J. Morphol. 88, 49-92. [PubMed] [Google Scholar]
- Hogan, K. A. and Bautch, V. L. (2004). Blood vessel patterning at the embryonic midline. Curr. Top. Dev. Biol. 62, 55-85. [DOI] [PubMed] [Google Scholar]
- Hogan, K. A., Ambler, C. A., Chapman, D. L. and Bautch, V. L. (2004). The neural tube patterns vessels developmentally using the VEGF signaling pathway. Development 131, 1503-1513. [DOI] [PubMed] [Google Scholar]
- Itasaki, N., Bel-Vialar, S. and Krumlauf, R. (1999). `Shocking' developments in chick embryology: electroporation and in ovo gene expression. Nat. Cell Biol. 1, E203-E207. [DOI] [PubMed] [Google Scholar]
- Kappas, N. C., Zeng, G., Chappell, J. C., Kearney, J. B., Hazarika, S., Kallianos, K. G., Patterson, C., Annex, B. H. and Bautch, V. L. (2008). The VEGF receptor Flt-1 spatially modulates Flk-1 signaling and blood vessel branching. J. Cell Biol. 181, 847-858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kawasaki, T., Kitsukawa, T., Bekku, Y., Matsuda, Y., Sanbo, M., Yagi, T. and Fujisawa, H. (1999). A requirement for neuropilin-1 in embryonic blood vessel formation. Development 126, 4895-4902. [DOI] [PubMed] [Google Scholar]
- Kendall, R. L. and Thomas, K. A. (1993). Inhibition of vascular endothelial cell growth factor activity by an endogenously encoded soluble receptor. Proc. Natl. Acad. Sci. USA 90, 10705-10709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klessinger, S. and Christ, B. (1996). Axial structures control laterality in the distribution pattern of endothelial cells. Anat. Embryol. 193, 319-330. [DOI] [PubMed] [Google Scholar]
- Kurz, H., Gartner, T., Eggli, P. S. and Christ, B. (1996). First blood vessels in the avian neural tube are formed by a combination of dorsal angioblast immigration and ventral sprouting of endothelial cells. Dev. Biol. 173, 133-147. [DOI] [PubMed] [Google Scholar]
- Lambrechts, D. and Carmeliet, P. (2006). VEGF at the neurovascular interface: therapeutic implications for motor neuron disease. Biochim. Biophys. Acta 1762, 1109-1121. [DOI] [PubMed] [Google Scholar]
- Leber, S. and Sanes, J. (1995). Migratory paths of neurons and glia in the embryonic chick spinal cord. J. Neurosci. 15, 1236-1248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lok, J., Gupta, P., Guo, S., Kim, W. J., Whalen, M. J., van Leyen, K. and Lo, E. H. (2007). Cell-cell signaling in the neurovascular unit. Neurochem. Res. 32, 2032-2045. [DOI] [PubMed] [Google Scholar]
- McCarty, J. H. (2005). Cell biology of the neurovascular unit: implications for drug delivery across the blood-brain barrier. Assay Drug Dev. Technol. 3, 89-95. [DOI] [PubMed] [Google Scholar]
- Megason, S. G. and McMahon, A. P. (2002). A mitogen gradient of dorsal midline Wnts organizes growth in the CNS. Development 129, 2087-2098. [DOI] [PubMed] [Google Scholar]
- Nakai, J. and Fujita, S. (1994). Early events in the histo- and cytogenesis of the vertebrate CNS. Int. J. Dev. Biol. 38, 175-183. [PubMed] [Google Scholar]
- Nakao, T., Ishizawa, A. and Ogawa, R. (1988). Observations of vascularization in the spinal cord of mouse embryos, with special reference to development of boundary membranes and perivascular spaces. Anat. Rec. 221, 663-677. [DOI] [PubMed] [Google Scholar]
- Nanka, O., Valasek, P., Dvorakova, M. and Grim, M. (2006). Experimental hypoxia and embryonic angiogenesis. Dev. Dyn. 235, 723-733. [DOI] [PubMed] [Google Scholar]
- Pan, Q., Chathery, Y., Wu, Y., Rathore, N., Tong, R. K., Peale, F., Bagri, A., Tessier-Lavigne, M., Koch, A. W. and Watts, R. J. (2007). Neuropilin-1 binds to VEGF121 and regulates endothelial cell migration and sprouting. J. Biol. Chem. 282, 24049-24056. [DOI] [PubMed] [Google Scholar]
- Pardanaud, L., Altmann, C., Kitos, P., Dieterlen-Lievre, F. and Buck, C. A. (1987). Vasculogenesis in the early quail blastodisc as studied with a monoclonal antibody recognizing endothelial cells. Development 100, 339-349. [DOI] [PubMed] [Google Scholar]
- Pardanaud, L. and Dieterlen-Lievre, F. (1993). Emergence of endothelial and hemopoietic cells in the avian embryo. Anat. Embryol. 187, 107-114. [DOI] [PubMed] [Google Scholar]
- Pardanaud, L., Luton, D., Prigent, M., Bourcheix, L.-M., Catala, M. and Dieterlen-Lievre, F. (1996). Two distinct endothelial lineages in ontogeny, one of them related to hemopoiesis. Development 122, 1363-1371. [DOI] [PubMed] [Google Scholar]
- Park, J. E., Keller, G. A. and Ferrara, N. (1993). The vascular endothelial growth factor (VEGF) isoforms: differential deposition into the subepithelial extracellular matrix and bioactivity of extracellular matrix-bound VEGF. Mol. Biol. Cell 4, 1317-1326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park, M. and Lee, S. (1999). The fourth immunoglobulin-like loop in the extracellular domain of FLT-1, a VEGF receptor, includes a major heparin-binding site. Biochem. Biophys. Res. Commun. 264, 730-734. [DOI] [PubMed] [Google Scholar]
- Price, S. R. and Briscoe, J. (2004). The generation and diversification of spinal motor neurons: signals and responses. Mech. Dev. 121, 1103-1115. [DOI] [PubMed] [Google Scholar]
- Raab, S., Beck, H., Gaumann, A., Yuce, A., Gerber, H. P., Plate, K., Hammes, H. P., Ferrara, N. and Breier, G. (2004). Impaired brain angiogenesis and neuronal apoptosis induced by conditional homozygous inactivation of vascular endothelial growth factor. Thromb. Haemost. 91, 595-605. [DOI] [PubMed] [Google Scholar]
- Roberts, D. M., Kearney, J. B., Johnson, J. H., Rosenberg, M. P., Kumar, R. and Bautch, V. L. (2004). The vascular endothelial growth factor (VEGF) receptor Flt-1 (VEGFR-1) modulates Flk-1 (VEGFR-2) signaling during blood vessel formation. Am. J. Pathol. 164, 1531-1535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ruhrberg, C., Gerhardt, H., Golding, M., Watson, R., Ioannidou, S., Fujisawa, H., Betsholtz, C. and Shima, D. T. (2002). Spatially restricted patterning cues provided by heparin-binding VEGF-A control blood vessel branching morphogenesis. Genes Dev. 16, 2684-2698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shalaby, F., Rossant, J., Yamaguchi, T. P., Gertsenstein, M., Wu, X.-F., Breitman, M. L. and Schuh, A. C. (1995). Failure of blood-island formation and vasculogenesis in Flk-1 deficient mice. Nature 376, 62-66. [DOI] [PubMed] [Google Scholar]
- Soker, S., Takashima, S., Miao, H. Q., Heufeld, G. and Klagsbrun, M. (1998). Neuropilin-1 is expressed by endothelial and tumor cells as an isoform-specific receptor for vascular endothelial growth factor. Cell 92, 735-745. [DOI] [PubMed] [Google Scholar]
- Stalmans, I., Ng, Y.-S., Rohan, R., Fruttiger, M., Bouche, A., Yuce, A., Fujisawa, H., Hermans, B., Shani, M., Jansen, S. et al. (2002). Arteriolar and venular patterning in retinas of mice selectively expressing VEGF isoforms. J. Clin. Invest. 109, 327-336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tischer, E., Mitchell, R., Hartman, T., Silva, M., Gospodarowicz, D., Fiddes, J. C. and Abraham, J. A. (1991). The human gene for vascular endothelial growth factor. Multiple protein forms are encoded through alternative exon splicing. J. Biol. Chem. 266, 11947-11954. [PubMed] [Google Scholar]
- Vasudevan, A., Long, J., Crandell, J., Rubenstein, J. and Bhide, P. (2008). Compartment-specific transcription factors orchestrate angiogenesis gradients in the embryonic brain. Nat. Neurosci. 11, 429-431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Virgintino, D., Maiorano, E., Errede, M., Vimercati, A., Greco, P., Selvaggi, L., Roncali, L. and Bertossi, M. (1998). Astroglia-microvessel relationship in the developing human telencephalon. Int. J. Dev. Biol. 42, 1165-1168. [PubMed] [Google Scholar]
- Wilting, J., Brand-Saberi, B., Huang, R., Zhi, Q., Kontges, G., Ordahl, C. P. and Christ, B. (1995). Angiogenic potential of the avian somite. Dev. Dyn. 202, 165-171. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.