Abstract
A patent ductus arteriosus (PDA) alters pulmonary mechanics and regional blood flow in the preterm infant. Its significance with respect to brain injury and brain development are unclear. We evaluated the effects of surgical ductal ligation on the preterm baboon brain. Baboons were delivered at 125 days of gestation (dg, term ~185dg) and ventilated for 14 days (n=12). The PDA was ligated 6 days after delivery (n=7) or left untreated (n=5). Animals were euthanized at 139dg and brains compared histologically with gestational control fetuses (n=7) at 140dg. Brain and body weights were reduced (p<0.05) in both groups of ventilated preterm animals, however, the brain to body weight ratio was increased (p<0.01) in ligated but not unligated newborns compared to gestational controls. No overt lesions were observed in either premature newborn group. Astrocyte density in the neocortex and hippocampus were greatest in the unligated newborns (p<0.01). Myelination and oligodendrocytes were reduced (p<0.05) in both premature newborn groups. The brain growth and development index was reduced and the damage index was increased in prematurely delivered baboons. Surgical ligation of the PDA does not increase the incidence of brain injury and may be beneficial if the PDA is contributing to persistent pulmonary and hemodynamic instability.
Keywords: non-human primate, prematurity, cerebral injury, positive pressure ventilation, brain development
Hemodynamic symptoms from a patent ductus arteriosus (PDA) are present in 55-70% of infants delivered below 1000g or prior to 28 weeks of gestation with the PDA resulting in increased pulmonary blood flow and redistribution of flow to other organs (1). However, the impact of the PDA on the brain remains uncertain. Current therapy for PDA includes medical therapy with indomethacin or ibuprofen and/or surgical ligation. There has been considerable debate about the benefits and risks of surgical ligation for PDA on subsequent neurodevelopmental outcome. Surgery in the neonatal period is associated with a systemic inflammatory response; in addition the use of sedative and/or anesthetic drugs may adversely impact the immature brain (2). An increased incidence of neurosensory impairment has been observed among infants who underwent ductal ligation (3). On the other hand in a single centre study where infants received prophylactic Indocin and no infant was exposed to patency of the ductus arteriosus for more than 5-7 days, ductal ligation was not associated with abnormal neurodevelopmental outcome (4). No experimental studies have been done to try to answer the impact of ligating a PDA on the developing brain.
The premature baboon, delivered at 125 days of gestation (dg; term ~ 185d), has a similar neonatal course to the premature human delivered between 26-27 weeks of gestation: they both develop respiratory distress and fail to close their PDA after birth (5). In addition, despite antenatal glucocorticoids, surfactant treatment, total parenteral nutrition, low tidal volume ventilation, and low supplemental oxygen administration during the first 2 weeks after delivery, premature baboons develop a similar pattern of both lung and brain injury as premature human infants (6-8). We hypothesize that surgical ligation of the ductus arteriosus will not increase the risk of delayed brain growth or injury in the premature baboon. In the present study, our aim was to compare the neuropathological consequences of premature birth with or without ductal ligation on the growth and development of the brain.
METHODS
All animal studies were performed at the Southwest Foundation for Biomedical Research in San Antonio, TX. All animal husbandry, animal handling, and procedures were reviewed and approved to conform to American Association for Accreditation of Laboratory Animal Care (AAALAC) guidelines.
Delivery and Instrumentation
Pregnant baboon dams (Papio papio) with timed gestations underwent elective hysterotomy under general anesthesia. Study animals were delivered at 125±2 (dg). The dams did not receive antenatal glucocorticoids. At birth, animals were weighed, sedated, intubated and treated with 4ml/kg surfactant (Survanta, courtesy Ross Laboratories, Columbus, OH) prior to the initiation of ventilatory support.
Ventilatory Management
Newborn baboons were mechanically ventilated for 14d as described previously (9). A complete description of the details of the surgical procedures and animal care (including ventilator management, target goals for PaO2, PaCO2, tidal volume, and nutritional, fluid, transfusion, antibiotic and blood pressure management) has been previously described (9). Animals were randomized before delivery to either undergo surgical ductal ligation on day 6 of life (ligated, n=7), or receive no intervention (unligated, n=5). Animals in the unligated group did not receive anesthesia or sham surgery since our intention was to mimic the clinical care of human newborns. None of the unligated animals closed their ductus spontaneously. Fetal gestational control animals (n=7) were delivered at 140dg and euthanized immediately with sodium pentobarbitone.
Physiological data
PaO2, PaCO2, pH, FiO2, systolic, diastolic and mean arterial blood pressure (BP), and heart rate were monitored continuously throughout the experimental period. Oxygenation Index (OI=mean airway pressure (cmH2O) × iO2 × 100/PaO2) and Ventilation Index (VI=peak inspiratory pressure × ventilator rate × PaCO2/1000) were also calculated. We also examined the relationship between a newborn baboon's physiological instability and measurements of brain growth and injury (see below). To do this we calculated the “interval flux” of physiological variables as a surrogate measure of the physiological instability. We first determined the maximum and minimum values of each variable during a time interval (6 hourly time periods for the first 48 hours and daily periods thereafter), the interval flux was the difference between these values during the specified time period. For each animal we then: 1) identified the maximum flux; and 2) calculated the mean of the interval fluxes over the entire experimental time period. Other findings relating to the clinical course, cardiovascular performance, and proinflammatory cytokines of the two newborn groups have been published elsewhere (9).
Histological Analysis
Brains were weighed, immersed in 10% buffered formalin and sectioned into 5mm coronal blocks (10-12 blocks per animal) (6). Blocks from the right hemisphere of each brain were processed to paraffin and 10 (8μm) sections collected from the rostral surface. A section from each block was stained with hematoxylin and eosin (H&E) and assessed for gross morphologic changes, including the presence of hemorrhages, lesions or infarcts, neuronal death, axonal injury, gliosis and perivascular cuffing. Masson's trichrome was used to assess for collagen deposition; Van Gieson's stain for elastic fibers, reticulin for reticulated fibers; Perls stain to visualize hemosiderin deposition.
Immunohistochemistry for rabbit anti cow-glial fibrillary acid protein (GFAP, 1:500, Sigma, St Louis, MO, USA) was used to identify astrocytes; rabbit anti-ionized calcium-binding adapter molecule 1 (Iba1, 1:100, Wako Chemicals, Osaka, Japan) to identify microglia/macrophages; mouse anti-human Ki67 clone MIB-1 (1:100; DakoCytomation, Glostrup, Denmark) to identify proliferating cells; and mouse anti-chicken myelin basic protein (MBP, 1:100; Chemicon, USA) to assess the extent of myelination, as previously described (6).
All analyses were performed on all brains in the study. Qualitative and quantitative measurements were made on coded slides blinded to the observer.
Qualitative analysis
Sections were scored for hemorrhages (present-1; absent-0) or overt injury such as infarcts, cystic white matter lesions or neuronal death. Iba1-immunoreactive (IR) sections were assessed for the presence of reactive microglial/macrophage cells in the grey and white matter.
Quantitative analysis
All quantitative measurements were made for sections from each block using an image analysis system (Image Pro v4.1, Media Cybernetics, Maryland, USA). Measurements of cell numbers were expressed as cells/mm2; all values were calculated as mean of means for each group.
Volumetric measurements
Cross-sectional areas of regions in the right forebrain were assessed in H&E-stained sections using a digitizing tablet (Sigma Scan Pro 4, Media Cybernetics, California, USA); volumes of the white matter, neocortex, deep grey matter (basal ganglia, thalamus and hippocampus) and ventricles were then estimated using the Cavalieri principle (10).
Area of subventricular zone (SVZ)
The area of the SVZ was assessed (×30) at 3 levels in the parietal/temporal region in H&E-stained sections. The high density of cells in this region of the SVZ compared to the adjacent striatum and white matter allowed for clear delineation of the region (11).
Surface folding index
The surface folding index (SFI), which gives an estimation of the expansion of the surface area relative to volume, was determined (6).
Percentage of white matter occupied by blood vessels
Point counting (12) was used to determine the density of blood vessel profiles in deep and subcortical white matter (×660) as an indicator of changes such as vasodilation or vasculogenesis. Assessment was performed in GFAP-IR sections as blood vessel profiles are clearly delineated (13).
Areal density of astrocytes
GFAP-IR cells were counted (×660) in randomly selected areas (0.02mm2) in each of the deep and subcortical white matter regions; the cerebral neocortex (three sites in blocks from frontal/temporal, parietal/temporal and occipital lobes in layers 5 and 6); the hippocampus (stratum radiatum in the CA1 region).
Areal density of oligodendrocytes
MBP-IR oligodendrocytes were counted (×300) in two randomly selected areas (0.42mm2) in both the deep and subcortical white matter from the parietal/temporal lobe.
Ki67-IR cell density in the SVZ and in the subgranular zone (SGZ) in the hippocampus
To assess cell proliferation, counts were made of Ki67-IR cells in lengths of the SVZ in the anteromedial striatal neuroepithelium and subventricular zone by 2 observers. Three regions (0.02mm2) were randomly sampled 40μm from the ependymal surface (×660) in two sections for each animal (6 measurements/animal). Counts were also made in 3 randomly selected regions (0.02mm2) in the SGZ of the dentate gyrus (3 measurements/animal; ×660).
Apoptotic cell counts
Apoptotic figures (14) were counted in stratum radiatum in CA1 region in the hippocampus and in layers 5 and 6 of the neocortex in 5 sites (0.09mm2) in 2 sections per animal and expressed as apoptotic figures/mm2.
Semi-Quantitative analysis
Myelination
In gestational control brains myelination as evidenced by (MBP-IR) was most advanced in the internal capsule with fibers extending into the subcortical white matter towards the subplate region; this was given a score of 3. The extent of myelination in the prematurely delivered groups was scored against this standard in the parietal/temporal region (0-no myelination; 1-a few myelinated fibers; 2-bundles of myelinated fibers; 3-similar extent of myelination to controls).
Perivascular cuffing in the subcortical white matter
The extent of perivascular cuffing was scored as: 0-not observed; 1-occasionally observed; 2-moderate degree; 3-considerable number of vessels with cuffing.
GFAP-IR radial glial fibers
Sections from the frontal/temporal, parietal/temporal and occipital regions were scored for the presence of GFAP-IR radial glial fibers on a scale of 0-3 (0-not observed; 1-occasionally observed; 2-moderate degree; 3-considerable number of fibers observed).
Growth and Development and Brain Damage Indices
Growth and development and brain damage indices were constructed as previously described (15). We acknowledge that in constructing both of the above indices we have given equal weighting to all variables. At this stage of gestation it is difficult to predict which variables of development might be the most relevant predictors of long lasting deficits.
Statistical Analysis
Linear regression analysis was carried out to determine if there was a correlation between: a) physiological variables (maximum and mean fluxes for pH, PaO2, PaCO2, FiO2, OI, VI and blood pressure and mean Qp/Qs and cardiac output) and brain growth and development or brain damage indices; b) physiological variables and quantitative variables (volumetric measurements, oligodendrocyte and astrocyte densities); c) volumetric measurements (white matter volume) and brain growth and development indices; and d) volumetric measurements (white matter volume) and quantitative variables (oligodendrocytes and astrocyte densities); a probability of p<0.05 was considered to be significant.
The statistical significance of differences between prematurely-delivered and control groups were tested using a one-way ANOVA with post-hoc analysis (Tukey's test) for histological variables. T-tests were used to compare between ligated and unligated groups for comparison of maximum and mean flux results and one-way ANOVAs were used for comparison of all other physiological variables; a probability of p<0.05 was considered to be significant. Results are expressed as mean ± SEM (weights and areas) and mean of means ± SEM (histological variables).
RESULTS
Prematurely Delivered Newborn Group Characteristics and Physiology
There were no differences between the 2 newborn groups (unligated and ligated) in any of the measured physiological variables (PaO2, PaCO2, pH, FiO2, Qp/Qs, VI, OI, diastolic, systolic and mean BP) (Table 1) nor in birth weight (unligated, 394±20g vs ligated, 376±16g), sex (M/F: unligated, 3/2 vs ligated, 5/2) or gestational age (unligated, 131.2±0.2 days vs ligated, 131.0±0.0 days) prior to the time of planned ductal ligation (day 6); all newborns had a patent ductus on day 6. During the post-ligation period (days 7-14), unligated animals continued to have a moderate left-to-right PDA shunt. The diastolic systemic blood pressure was lower, and VI and Qp/Qs were higher in unligated compared to ligated animals (p<0.05; Table 1). Ligated animals had a reduced OI following ligation on day 6 (p<0.03), no other differences were observed between the pre- and post-ligation period for ligated animals. There were no differences between the two groups in base deficit, serum bicarbonate or need for dopamine/dobutamine administration during the 14d treatment course (9). The maximum fluxes in pH (unligated, 0.37±0.3 vs ligated, 0.26±0.03), PaO2 (unligated, 81.6±5.4mmHg vs ligated, 60.3±8.3mmHg) and PaCO2 (unligated, 58.4±6.8mmHg vs ligated, 32.9±3.4mmHg) and the mean flux in PaCO2 (unligated, 17.4±1.8mmHg vs ligated, 13.7±1.6mmHg) and FiO2 (unligated, 0.09±0.01% vs ligated, 0.06±0.01%) were higher in unligated compared to ligated animals over the 14d study period (p<0.05).
Table 1.
Physiological data
| Pre-ligation period (days 1-6) | Post-ligation period (days 7-14) | |||
|---|---|---|---|---|
| ligated | unligated | ligated | unligated | |
| Qp/Qs | 1.60±0.10 | 1.80±0.24 | 1.01 ±0.01 | 2.27±0.12** |
| Oxygenation Index | 6.00±0.14 | 6.21±0.16 | 3.74±0.14† | 5.53±0.18 |
| Ventilation Index | 41.56±1.90 | 43.53±1.6 | 28.62±0.70 | 48.57±1.90* |
| Diastolic BP (mmHg) | 28.82±0.50 | 28.10±0.70 | 32.32±0.42 | 26.19±0.50* |
| Mean BP (mm Hg) | 35.30±0.50 | 37.10±0.80 | 42.04±0.45 | 39.13±0.48 |
p<0.03
p<0.007 vs ligated (days 7-14)
p<0.03 vs ligated (days 1-6).
ANOVA for repeated measures, Day 7-14, Values are mean ± sem.
BP, blood pressure
Brain Growth and Development (Table 2)
Table 2.
Body and brain weights and cerebral volumetric measurements
| Parameter | Control (n=7) | Unligated (n=5) | Ligated (n=7) |
|---|---|---|---|
| Body weight at necropsy (g) | 543.0±14.4 | 343.8±4.1† | 339.3±18.7† |
| Total brain weight (after fixation; g) | 60.0±1.6 | 39.8±0.9† | 45.0±2.6† |
| Brain/body weight, ratio | 0.11±0.01 | 0.12±0.01 | 0.13±0.01** |
| Volume of right forebrain (mm3) | 20,177±777 | 14,606±802† | 15,360±490† |
| White matter Volume (mm3) | 9,136±300 | 6,426±313† | 6,962±300† |
| Neocortical Volume (mm3) | 8,858±425 | 6,559±668* | 6,744±218* |
| Deep grey matter (basal ganglia, thalamus, hippocampal) Volume (mm3) | 2,037±193 | 1,441±104* | 1,442±55* |
| White matter/Total Volume (%) | 45.5±0.9 | 45.5±0.8 | 45.3±0.7 |
| Neocortex/Total Volume (%) | 43.9±0.7 | 43.5±0.6 | 43.9±0.7 |
| Deep grey matter/Total volume (%) | 10.1±0.7 | 10.5±0.8 | 9.4±0.4 |
| White matter/Neocortex, ratio | 1.04±0.04 | 1.02±0.09 | 1.03±0.03 |
| Surface Folding Index (SFI) | 43.9±2.2 | 37.4±1.1* | 39.9±0.9 |
p<0.05 vs control
p<0.01 vs control
p<0.001 vs control.
Values are mean ± SEM. All volume measurements were made on the right hemisphere only
Brain and body weights
Weights were reduced in both groups of prematurely delivered newborns, at the time of necropsy, compared to age-matched gestational controls (p<0.001). The brain to body weight ratio was higher in ligated newborns compared to gestational control animals (p<0.01), indicative of some brain sparing in this group.
Volumetric Measurements
The total volume of the forebrain (right; p<0.001), as well as the white matter (p<0.001), neocortical (p<0.05) and deep grey matter (p<0.05) volumes, were reduced in both premature newborn groups compared to gestational controls. There was no difference (p>0.05) between the groups in the ratios of white matter, neocortical or deep grey matter volumes to the total forebrain volume or in the ratio of white matter/neocortex. The area of the SVZ (gestational control, 1.97±0.18mm2; unligated, 1.59±0.08mm2; ligated, 2.26±0.19mm2) and the area of the SVZ expressed as a percentage of the total cross-sectional area (gestational control, 0.45±0.06%; unligated, 0.47±0.06%; ligated, 0.6±0.05%) were not different (p>0.05) between groups. There was no difference between ligated and unligated groups in any of the variables listed in Table 2.
Surface Folding Index
Compared to gestational controls, the overall SFI of the forebrain was reduced in unligated newborns (p<0.05).
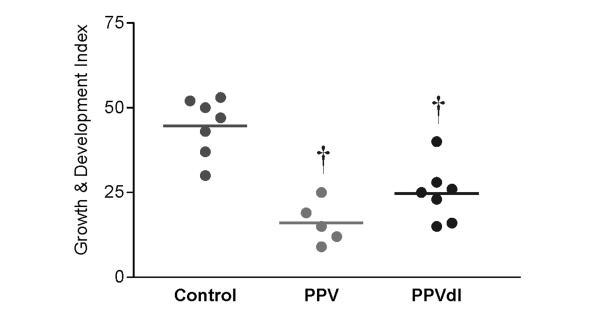
Growth and Development Index
The index was decreased (p<0.001) for both unligated (16.0±2.8) and ligated newborns (24.7±3.2) animals compared to gestational controls (44.6±2.5); there was no difference (p>0.05) between unligated and ligated animals (Figure 1).
Figure 1.
The growth and development index scores were decreased (†, p<0.001) in both unligated and ligated groups compared to gestational controls but there was no difference between prematurely delivered groups.
Brain Injury
Qualitative Assessment
There was no evidence of infarction or intraventricular or parenchymal hemorrhages in any animal. In one ligated animal, meningeal cell proliferation was evident in the sub-arachnoid space; this was associated with a proliferation of small capillaries with a hyalinised subendothelial matrix. Extravasated intact red cells were seen adjacent to this region; the presence of fresh red cells with no adjacent cellular reaction is difficult to interpret.
Ramified (resting) Iba1-IR microglia/macrophages were observed throughout the grey and white matter; activated Iba1-IR cells were observed infrequently and the incidence was similar in both newborn groups compared to gestational controls.
Quantitative Assessment (Table 3)
Table 3.
Brain damage index
| Parameter | Control (n=7) | Unligated (n=5) | Ligated (n=7) |
|---|---|---|---|
| Astrocytes in deep WM (cells/mm2) | 402±23 | 453±22 | 484±30 |
| Astrocytes in subcortical WM (cells/mm2) | 378±28 | 407±22 | 430±29 |
| Astrocytes in neocortex (cells/mm2) | 131±26 | 243±31*,‡ | 126±13 |
| Astrocytes in hippocampus (cells/mm2) | 241±14 | 558±36†,§ | 375±19** |
| MBP-IR oligodendrocytes in the deep WM (cells/mm2) | 106±11 | 48±6** | 52+13* |
| MBP-IR oligodendrocytes in the subcortical WM (cells/mm2) | 42±7 | 12±5* | 20±4* |
| Extent of Myelination | 2.4±0.2 | 1.5±0.2** | 1.5±0.3** |
| GFAP-IR radial glial fibres | 1.4±0.2 | 2.2±0.3 | 1.9±0.3 |
| Perivascular Cuffing | 0.4±0.3 | 0.6±0.4 | 1.4±0.5 |
| Brain damage index | 49.9±5.9 | 109.8±7.6† | 99.1±9.5† |
p<0.05 vs control
p<0.01 vs control
p<0.001 vs control
p<0.05 vs
p<0.01 vs Ligated.
Values are mean ± SEM. WM, white matter.
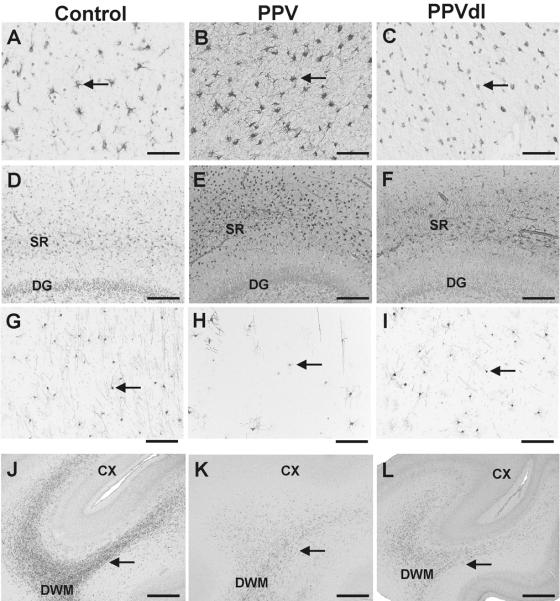
Areal density of astrocytes
There was no difference between groups (p>0.05) in either the deep or subcortical white matter. In the cerebral neocortex, there was an increase (p<0.05) in the overall density in unligated (Figure 2B) compared to ligated (Figure 2C) and gestational control animals (Figure 2A). On a regional basis (data not shown) there was an increase in astrocytes in the frontal/temporal (p<0.05) and the occipital (p<0.05) regions in unligated compared to ligated and control animals. The density within the stratum radiatum of the hippocampus was increased in both unligated (p<0.001; Figure 2E) and ligated (p<0.01; Figure 2F) animals compared to controls (Figure 2D) and in unligated compared to ligated animals (p<0.01).
Figure 2.
A-C: GFAP-IR in the neocortex; Astrocyte density was increased in unligated (B) compared to ligated (C) and control animals (A). D-F: GFAP-IR in the hippocampus; Astrocyte density within the stratum radiatum of the hippocampus was increased in unligated (E, p<0.001) and ligated (F, p<0.05) compared to control animals (D) and in unligated animals (p<0.01) compared to ligated animals; arrows indicating astrocytes. G-L: There was a reduction (p<0.05) in the density of myelin basic protein-immunoreactive (MBP-IR) oligodendrocytes in unligated (H, K) and ligated (I, L) animals compared to controls (G, J); arrows indicate MBP-IR oligodendrocytes. A-C=70μm; D-I=1.7mm; J-L=160μm.
Areal density of oligodendrocytes:
The overall density in both the deep and subcortical white matter in the parietal/temporal lobe was reduced (p<0.05) in unligated (Figure 2H, K) and ligated (Figure 2I, L) animals compared to gestational controls (Figure 2G, J). There was no difference between prematurely delivered animals in either region (p=0.5).
Percentage of white matter occupied by blood vessels:
There was no difference between groups (p>0.05) in either the subcortical (gestational control, 1.4±0.2%; unligated, 1.7±0.3%; ligated, 2.0±0.3%) or deep white matter (gestational control, 1.2±0.1%; unligated, 1.8±0.2%; ligated, 1.9±0.5%) regions indicating that neither regimen resulted in vasculogenesis or vasodilatation at least as seen at postmortem.
Ki67-IR cell counts:
There was no difference (p>0.05) in the number of cells in the SVZ (gestational control, 329±97cells/mm2; unligated, 655±87cells/mm2; ligated, 457±68cells/mm2) or in the SGZ of the dentate gyrus of the hippocampus (gestational control, 207±52cells/mm2; unligated, 180±39cells/mm2; ligated, 144±25cells/mm2) between groups.
Apoptotic cell counts in the hippocampus and cerebral neocortex
There was no difference (p>0.05) between any of the groups in either the dentate region of the hippocampus (gestational control, 1.6±0.7cells/mm2; unligated, 3.0±1.2cells/mm2; ligated, 1.9±0.5cells/mm2) or the neocortex (gestational control, 2.0±0.2cells/mm2; unligated, 1.8±0.9 cells/mm2; ligated, 1.4±0.5cells/mm2).
Semi-Quantitative Assessment (Table 3)
Myelination
In gestational control brains MBP-IR axons were present in the thalamus and posterior limb of the internal capsule; there was also some staining in the alveus of the hippocampus and white matter of the pre- and post-central gyri. Scoring revealed a reduction (p<0.01) in the extent of myelination in both unligated and ligated animals compared to controls.
Radial Glia
Intensely GFAP-IR radial glial fibers were present at the ventricular surface projecting into the deep white matter in all control animals. There was no difference (p>0.05) in the occurrence of GFAP-IR radial glial between the newborn groups.
Perivascular cuffing
There was no difference (p>0.05) between groups in the incidence of cuffing in the deep white matter.
Brain Damage Index
The variables comprising the brain damage index are contained in Table 3. There was an increase in the brain damage index for both unligated (p<0.001) and ligated (p<0.001) animals compared to controls. However, there was no difference (p=0.4) between unligated and ligated newborns.
Correlations between brain growth, brain injury and physiological variables Indices vs Structural variables
Across all of the animals there were positive correlations between the following: the growth and development index and white matter volume (r2=0.78; p<0.0001); the SFI and brain weight (r2=0.23; p<0.004); the SFI and white matter volume (r2=0.44; p<0.002); white matter volume and the areal density of MBP-IR oligodendrocytes in the deep (r2=0.38; p<0.005) and subcortical white matter (r2=0.23; p<0.04). These correlations confirm the expected increase in SFI, white matter volume, and oligodendrocyte development with increasing brain weight.
There were negative correlations between the following: brain weight and the brain damage index (r2=0.50; p<0.0008); white matter volume and the brain damage index (r2=0.75; p<0.0001); the areal density of MBP-IR oligodendrocytes in the deep white matter and the brain damage index (r2=0.27; p<0.02); white matter volume and the areal density of astrocytes in the deep (r2=0.23; p<0.04), and subcortical white matter (r2=0.22; p<0.04). These correlations indicate that: 1) as brain weight, white matter volume and oligodendrocyte density decrease the brain damage index increases; 2) as astrocyte density increases, the volume of white matter decreases.
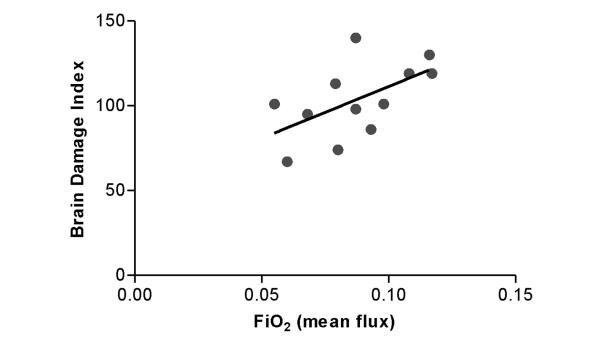
Physiological vs structural variables
There were no significant correlations between physiological variables and indices of growth and development. On the other hand, there were significant correlations between the fluxes in FiO2 and PaCO2 and the extent of injury. There were positive correlations between the brain damage index and the mean (r2=0.33; p<0.05; Figure 3) and maximum fluxes (r2=0.50; p<0.01) in FiO2; the areal density of neocortical astrocytes and the maximum flux in PaCO2 (r2=0.41; p<0.03). There were negative correlations between: the areal density of MBP-IR oligodendrocytes in the deep white matter and the maximum flux in FiO2 (r2=0.50; p<0.01). There was no correlation between both average Qp/Qs or cardiac output and any histological variable.
Figure 3.
Regression analysis included both groups of prematurely delivered animals (unligated and ligated). A positive correlation was observed between the mean flux in FiO2 and the brain damage index score (r2=0.33; p<0.05).
DISCUSSION
This study confirms our previous reports (15, 16) that premature delivery and critical illness are associated with significant neuropathological alterations in the brains of newborn baboons; importantly these changes occur in the absence of chorioamnionitis.
Growth and development
The brain growth and development index was lower in both groups of newborn animals compared with gestational controls confirming our previous observations that brain growth is slowed in this model of premature birth (15, 16). There was no difference between the ligated and unligated animals in any of our measurements of brain volume (the small number of animals used in our study may have limited the interpretation of some of the results). However, we did find that eliminating a persistent, moderate size PDA shunt might have some protective effect on brain growth. We base this on the findings that: 1) there was a small but significant increase in the brain to body weight ratio in ligated compared to gestational control animals; and 2) the surface folding index (a measure of gyrification) was reduced in unligated animals with a persistent PDA but not in ligated animals. Gyrification is thought to reflect the development of cerebral and subcortical connectivity (17).
Brain injury
Our study demonstrates alterations in cerebral white and grey matter in both groups of newborn animals. The reduction in oligodendrocyte cell numbers could have resulted from their marked susceptibility to oxidative and/or nitrosative stress at this developmental stage (18, 19). The concomitant reduction in myelination might be related either to a direct effect on oligodendrocytes or to a reduction in axon numbers and/or a reduction in axonal diameter and hence to thinner myelin sheaths.
There was a greater increase in the density of astrocytes in the neocortex and hippocampus in unligated compared to ligated animals. While this was not reflected in a significant difference in the overall brain damage index between prematurely delivered groups the mean score was lower in the unligated group. It is possible that a difference was not found due to the composite construction of the score and to the small sample size (Type II error).
Despite attempts to maintain respiratory stability, hypoxic episodes occur in the baboon newborns as they do in the preterm human newborn. In general, the animals that had better ventilatory control and required less manipulation of FiO2 (lower fluxes), had lower brain indices. Although ductal ligation does not always produce a significant improvement in clinical status (9, 20), in the present study, both pulmonary status (as evidenced by VI) and blood pressure control improved after ligation. It is possible that these factors combined to improve cerebral blood flow and oxygen delivery to the brain resulting in less gliosis and a tendency for better brain growth in the ligated animals. Reactive astrocytes produce IGF-1 (21) and FGF (22) to support neuronal survival and to assist in repair mechanisms but they also produce cytokines and reactive oxygen species which could exacerbate injury via oxidative and inflammatory pathways (23). There was no overt indication of inflammation as evidenced by an increase in activated microglia in the brain, although it is possible that the peak of such a response will have occurred prior to the end of the experiment.
Our findings in the premature baboon help to explain the apparent differences between previous clinical studies that examined the relationship between PDA, surgical ligation and neurodevelopmental outcome (3, 4). Chorne et al. reported that when ligation was performed, after a brief exposure to a symptomatic PDA, there was no relationship between ligation and neurodevelopmental abnormality (4). On the other hand, Kabra et al. observed that when infants were ligated after allowing the symptomatic PDA to persist for varying lengths of time, the risk for neurosensory impairment was increased (3). Human preterm infants will almost uniformly receive indomethacin prior to surgical ligation. Indomethacin exposure might be an important variable and should be acknowledged when considering the translation of these study findings to human infants. Our study was designed to examine the specific effects of ductus ligation on brain development and injury.
We conclude from our study that closing the PDA, even by ligation, does not necessarily lead to brain injury; it may even be of some benefit to the brain if the PDA is contributing to persistent pulmonary and hemodynamic instability. Similar conclusions have also been made regarding other organ systems (24).
Acknowledgements
We are grateful to Dr. Coalson, Ms Winter and the personnel at the BPD Resource Centre, San Antonio, Texas, to Drs. Folkerth and Kinney, Department of Pathology, Children's Hospital, Boston, USA for neuropathological advice and to Ms Amy Shields, University of Melbourne for histological assistance.
Financial Support: Supported in part by NIH Grants R01 HL074942; HL3399; HL056061, HL52636 BPD Resource centre and P51RR13986 baboon facility support.
Abbreviations
- GFAP
glial fibrillary acidic protein
- IR
immunoreactivity
- MBP
myelin basic protein
- PDA
patent ductus arteriosus
- SFI
surface-folding index
- SGZ
subgranular zone
- SVZ
subventricular zone
REFERENCES
- 1.Clyman RI. Mechanisms regulating the ductus arteriosus. Biol Neonate. 2006;89:330–335. doi: 10.1159/000092870. [DOI] [PubMed] [Google Scholar]
- 2.Doyle LW. Outcome at 5 years of age of children 23 to 27 weeks' gestation: refining the prognosis. Pediatrics. 2001;108:134–141. doi: 10.1542/peds.108.1.134. [DOI] [PubMed] [Google Scholar]
- 3.Kabra NS, Schmidt B, Roberts RS, Doyle LW, Papile L, Fanaroff A. Trial of Indomethacin Prophylaxis in Preterms Investigators 2007 Neurosensory impairment after surgical closure of patent ductus arteriosus in extremely low birth weight infants: results from the Trial of Indomethacin Prophylaxis in Preterms. J Pediatr. 150:229–234. 234 e1. doi: 10.1016/j.jpeds.2006.11.039. [DOI] [PubMed] [Google Scholar]
- 4.Chorne N, Leonard C, Piecuch R, Clyman RI. Patent ductus arteriosus and its treatment as risk factors for neonatal and neurodevelopmental morbidity. Pediatrics. 2007;119:1165–1174. doi: 10.1542/peds.2006-3124. [DOI] [PubMed] [Google Scholar]
- 5.Clyman RI, Chan CY, Mauray F, Chen YQ, Cox W, Seidner SR, Lord EM, Weiss H, Waleh N, Evans SM, Koch CJ. Permanent anatomic closure of the ductus arteriosus in newborn baboons: the roles of postnatal constriction, hypoxia, and gestation. Pediatr Res. 1999;45:19–29. doi: 10.1203/00006450-199901000-00005. [DOI] [PubMed] [Google Scholar]
- 6.Dieni S, Inder T, Yoder B, Briscoe T, Camm E, Egan G, Denton D, Rees S. The pattern of cerebral injury in a primate model of preterm birth and neonatal intensive care. J Neuropathol Exp Neurol. 2004;63:1297–1309. doi: 10.1093/jnen/63.12.1297. [DOI] [PubMed] [Google Scholar]
- 7.Coalson JJ, Winter VT, Siler-Khodr T, Yoder BA. Neonatal chronic lung disease in extremely immature baboons. Am J Respir Crit Care Med. 1999;160:1333–1346. doi: 10.1164/ajrccm.160.4.9810071. [DOI] [PubMed] [Google Scholar]
- 8.Yoder BA, Siler-Khodr T, Winter VT, Coalson JJ. High-frequency oscillatory ventilation: effects on lung function, mechanics, and airway cytokines in the immature baboon model for neonatal chronic lung disease. Am J Respir Crit Care Med. 2000;162:1867–1876. doi: 10.1164/ajrccm.162.5.9912145. [DOI] [PubMed] [Google Scholar]
- 9.McCurnin DC, Yoder BA, Coalson J, Grubb P, Kerecman J, Kupferschmid J, Breuer C, Siler-Khodr T, Shaul PW, Clyman R. Effect of ductus ligation on cardiopulmonary function in premature baboons. Am J Respir Crit Care Med. 2005;172:1569–1574. doi: 10.1164/rccm.200502-230OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gundersen HJ, Jensen EB. The efficiency of systematic sampling in stereology and its prediction. J Microsc. 1987;147:229–263. doi: 10.1111/j.1365-2818.1987.tb02837.x. [DOI] [PubMed] [Google Scholar]
- 11.Ong J, Plane JM, Parent JM, Silverstein FS. Hypoxic-ischemic injury stimulates subventricular zone proliferation and neurogenesis in the neonatal rat. Pediatr Res. 2005;58:600–606. doi: 10.1203/01.PDR.0000179381.86809.02. [DOI] [PubMed] [Google Scholar]
- 12.Rees S, Stringer M, Just Y, Hooper SB, Harding R. The vulnerability of the fetal sheep brain to hypoxemia at mid-gestation. Brain Res Dev Brain Res. 1997;103:103–118. doi: 10.1016/s0165-3806(97)81787-7. [DOI] [PubMed] [Google Scholar]
- 13.Loeliger M, Watson CS, Reynolds JD, Penning DH, Harding R, Bocking AD, Rees SM. Extracellular glutamate levels and neuropathology in cerebral white matter following repeated umbilical cord occlusion in the near term fetal sheep. Neuroscience. 2003;116:705–714. doi: 10.1016/s0306-4522(02)00756-x. [DOI] [PubMed] [Google Scholar]
- 14.Wyllie AH, Kerr JF, Currie AR. Cell death: the significance of apoptosis. Int Rev Cytol. 1980;68:251–306. doi: 10.1016/s0074-7696(08)62312-8. [DOI] [PubMed] [Google Scholar]
- 15.Loeliger M, Inder T, Cain S, Ramesh RC, Camm E, Thomson MA, Coalson J, Rees SM. Cerebral outcomes in a preterm baboon model of early versus delayed nasal continuous positive airway pressure. Pediatrics. 2006;118:1640–1653. doi: 10.1542/peds.2006-0653. [DOI] [PubMed] [Google Scholar]
- 16.Rees SM, Camm EJ, Loeliger M, Cain S, Dieni S, McCurnin D, Shaul PW, Yoder B, McLean C, Inder TE. Inhaled nitric oxide: effects on cerebral growth and injury in a baboon model of premature delivery. Pediatr Res. 2007;61:552–558. doi: 10.1203/pdr.0b013e318045be20. [DOI] [PubMed] [Google Scholar]
- 17.Van Essen DC. A tension-based theory of morphogenesis and compact wiring in the central nervous system. Nature. 1997;385:313–318. doi: 10.1038/385313a0. [DOI] [PubMed] [Google Scholar]
- 18.Haynes RL, Folkerth RD, Keefe RJ, Sung I, Swzeda LI, Rosenberg PA, Volpe JJ, Kinney HC. Nitrosative and oxidative injury to premyelinating oligodendrocytes in periventricular leukomalacia. J Neuropathol Exp Neurol. 2003;62:441–450. doi: 10.1093/jnen/62.5.441. [DOI] [PubMed] [Google Scholar]
- 19.Back SA, Han BH, Luo NL, Chricton CA, Xanthoudakis S, Tam J, Arvin KL, Holtzman DM. Selective vulnerability of late oligodendrocyte progenitors to hypoxia-ischemia. J Neurosci. 2002;22:455–463. doi: 10.1523/JNEUROSCI.22-02-00455.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Moin F, Kennedy KA, Moya FR. Risk factors predicting vasopressor use after patent ductus arteriosus ligation. Am J Perinatol. 2003;20:313–320. doi: 10.1055/s-2003-42693. [DOI] [PubMed] [Google Scholar]
- 21.Gluckman P, Klempt N, Guan J, Mallard C, Sirimanne E, Dragunow M, Klempt M, Singh K, Williams C, Nikolics K. A role for IGF-1 in the rescue of CNS neurons following hypoxic-ischemic injury. Biochem Biophys Res Commun. 1992;182:593–599. doi: 10.1016/0006-291x(92)91774-k. [DOI] [PubMed] [Google Scholar]
- 22.Takami K, Iwane M, Kiyota Y, Miyamoto M, Tsukuda R, Shiosaka S. Increase of basic fibroblast growth factor immunoreactivity and its mRNA level in rat brain following transient forebrain ischemia. Exp Brain Res. 1992;90:1–10. doi: 10.1007/BF00229250. [DOI] [PubMed] [Google Scholar]
- 23.Ganat Y, Soni S, Chacon M, Schwartz ML, Vaccarino FM. Chronic hypoxia up-regulates fibroblast growth factor ligands in the perinatal brain and induces fibroblast growth factor-responsive radial glial cells in the sub-ependymal zone. Neuroscience. 2002;112:977–991. doi: 10.1016/s0306-4522(02)00060-x. [DOI] [PubMed] [Google Scholar]
- 24.Jaillard S, Larrue B, Rakza T, Magnenant E, Warembourg H, Storme L. Consequences of delayed surgical closure of patent ductus arteriosus in very premature infants. Ann Thorac Surg. 2006;81:231–234. doi: 10.1016/j.athoracsur.2005.03.141. [DOI] [PubMed] [Google Scholar]