Abstract
OBJECTIVES
To determine whether elderly people who meet national guidelines have higher physical function (PF) scores than those who do not and the effect on functional trajectory when physical activity (PA) levels change from above to below this threshold, or vice versa.
DESIGN
Pooled data.
SETTING
Two 6-month randomized controlled trials aimed at increasing PA in adults.
PARTICIPANTS
Adults aged 65 to 94 (N 5 357).
INTERVENTION
PA counseling over the telephone and through mailed materials.
MEASUREMENTS
Self-reported PA dichotomized at 150 minutes/week and PF using the Medical Outcomes Study 36-item Short Form Questionnaire PF subscale.
RESULTS
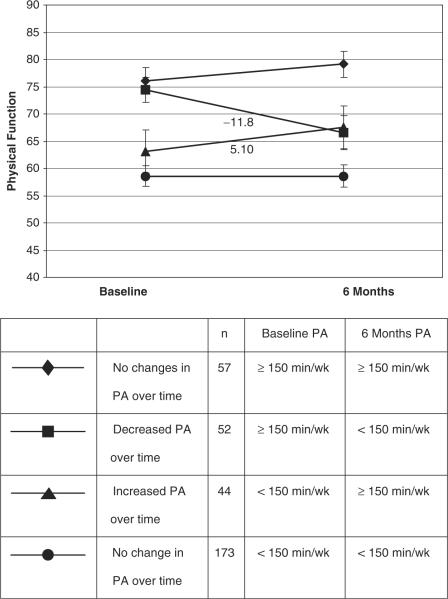
At baseline, individuals reporting 150 minutes or more of moderate PA/week had mean PF scores that were 20.3 points higher than those who did not (Po<.001). Change in PA minutes from above threshold to below threshold or from below threshold to above threshold from baseline to 6 months resulted in an average change in PF of 11.18 (P<.001) and +5.10 (P =.05), respectively.
CONCLUSION
These findings suggest that PA is an important predictor of functional status. Older sedentary adults can improve PF by meeting recommended PA levels. Conversely, dropping below recommended PA levels has a deleterious effect on PF. Given the importance of PF in maintenance of independence and quality of life in older adults, adherence to recommended PA guidelines should be endorsed.
Keywords: exercise, aging, physical function, meta-analysis, evidence-based guidelines, clinical trials
In 1996, in one of the first government recognitions of the potential health benefit of physical activity (PA), the Surgeon General (SG) endorsed guidelines for practice.1 The report represented a consensus statement aimed at facilitating a public health recommendation for PA that would be acceptable to the majority of Americans in lieu of previous recommendations that emphasized vigorous exercise. The primary message was simple and directed at all ages—to accumulate 30 minutes or more of moderate PA on 5 or more days of the week. Although the SG report was detailed and addressed known PA benefits for different segments of the population or for specific medical conditions, no distinction was made relative to a recommendation for older adults. The report indicated that more research was needed to determine the types of PA necessary to preserve strength and physical function (PF) in this population.1
The ensuing decade produced a large amount of PA research directed at the older adult.2-8 An abundance of evidence indicated that PA was consistently associated with better fitness parameters and related health outcomes,9,10 but few studies have specifically examined the effect of the PA threshold endorsed by the SG (150 min/week) on PF. The relationship between the SG-endorsed PA guidelines and PF was examined cross-sectionally in a sample of healthy older adults and prospectively in a sample of postmenopausal women undergoing a walking intervention, and a significant association was found between PA and PF.11,12
Leisure time activity counseling to Improve Fitness In Elders (Project LIFE) and Leading the Way in Exercise and Diet (Project LEAD), two PA intervention trials that targeted older adults and used self-reported PF as a primary outcome, were recently completed,.13-15 Using data pooled from these two studies, the following two research questions were examined: Do individuals who meet the SG guidelines have higher PF scores than those who do not? Does changing from above to below thresholds, or vice versa, affect functional trajectory?
METHODS
Two clinical trials that tested a PA intervention in older adults were combined for this study. The respective institutional review boards reviewed and approved each study annually, and the studies have been described in detail elsewhere, although brief descriptions are provided below.13-15
Project LIFE was a 6-month feasibility trial designed to determine whether PA health counselors could interface successfully with primary care providers to enhance delivery of PA counseling in elderly people with multiple chronic diseases. Patients aged 70 and older who were being followed in geriatric and primary care clinics were screened and recruited for this study. Patients were free of terminal diagnoses, unstable angina pectoris or recent myocardial infarction, stroke with moderate to severe aphasia, or active substance abuse. Patients already engaged in regular PA also were excluded based on their affirmative response to one question that asked about moderate physical activity for 30 minutes or more on 5 or more days per week. Of 1,385 medical record reviewed, 914 patients met initial eligibility criteria. Of these, 639 were contacted over the telephone after receiving a recruitment package, and 276 gave initial oral consent. From this group, 179 patients reported for an in-person baseline assessment on the day of a clinical appointment. Written consent was obtained, and patients were randomly assigned to receive intensive telephone PA counseling (n = 88) twice a week for 3 months and then monthly for 3 months, health education counseling (n = 43) twice a week for 3 months and then monthly for 3 months on general health topics, or usual care (n = 44) with no additional contact.
Project LEAD was a 6-month intervention development study that promoted a healthy diet (low in total and saturated fat, low in cholesterol, high in fruit and vegetable consumption, and rich in calcium and iron) and increased PA in older adults with a recent diagnosis of early-stage breast or prostate cancer using a home-based approach of mailed materials and telephone counseling. The primary endpoint was change in self-reported PF. In this study, patients with breast and prostate cancer aged 65 and older and within 18 months of diagnosis were identified and recruited from hospital registries within North Carolina. Permission to contact patients was obtained from oncology-care physicians, and recruitment packages, which included consent forms and screening surveys, were mailed to potential study participants (n = 2,037). The survey assessed conditions that would preclude unsupervised exercise such as uncontrolled heart failure, recent myocardial infarction, pulmonary disease requiring oxygen use, use of a mobility aid other than a cane, plans to have hip or knee replacement, kidney failure, or chronic warfarin use. Additional exclusion criteria included progressive malignant disease or additional primary tumors and inability to participate fully in telephone or mailed material interventions (i.e., severe hearing or speaking impairments, lack of English competency, or mental incompetence). For study inclusion, participants had to self-report two or more deficits on the Medical Outcomes Study 36-item Short-Form Questionnaire (SF-36) PF subscale,16 less than 90 min/wk of vigorous exercise (~ equivalent to 150 minutes of moderate PA), and poor diet quality.
Of 688 participants consenting to participate, 182 met full study criteria and were randomly assigned to an experimental arm (n = 89) consisting of receipt of a specially directed workbook and twice-monthly telephone counseling on improving diet (first 3 months) and level of PA (second 3 months) or a health education arm (n = 93) consisting of receipt of a workbook and twice -monthly telephone counseling for 6 months on general health promotion topics.
Measures
Although each study used a single-item question during the screening process to exclude individuals engaged in regular moderate or vigorous activity at levels consistent with the SG guidelines, the baseline and 6-month follow-up surveys included a more-thorough assessment (the Community Health Activities Model Program for Seniors (CHAMPS)), which is well validated and sensitive to change.17 No exclusions were made at the time of the baseline interview if participants reported PA over the threshold established for the screening instrument. Frequency and total time spent per week on a list of activities was assessed. Total time per week per activity was placed into categories ranging from not at all, less than 1 h/week and upwards in 1.5-hour increments up to more than 9 h/week. Because the CHAMPS does not assess minutes as a continuous variable, minutes of activities were estimated by multiplying the midpoint of each category of hours per week by 60. Items coded as moderate- or higher-intensity PA were used in this study. Minutes of PA were dichotomized at 150 min/week.
Self-reported PF was assessed using the SF-36 PF subscale.18 The PF subscale is a self-report of functional status that has been well validated, has good psychometric properties that are subscale specific, and is sensitive to change.16 The scale was scored on a range of 0 to 100, with higher scores indicating better functional status. Comorbidity was assessed from a checklist of 35 medical conditions adapted from the Older Americans Resources and Services survey in which the participant is asked “Do you have any of the following illnesses at the present time?” Positive responses are summed to create a total number of diseases.19 Other than demographic and descriptive variables, there were no other outcomes in common between these two studies.
Statistical Analysis
Data from the two studies were pooled (N = 357 at baseline). Baseline characteristics are reported as means and standard deviations or percentages. Baseline comparisons of PA and PF were controlled for baseline age, race, sex, and study. Analyses pertaining to change scores included only individuals who completed each trial and had data for the outcomes of interest (n = 326). Analyses evaluating the effects of baseline PA level and change in PA level from baseline to 6 months were performed separately for each study, controlling for baseline PF, age, race, sex, and comorbidity. The overall, across-study effect for PA and change in PA were then obtained using standard meta-analytical techniques by calculating a weighted average of the individual study effects.20
RESULTS
The characteristics of the study sample (N = 357) are provided in Table 1. Study participants ranged from age 65 to 94 and were predominantly male (70.6%) because one of the studies was based at the Department of Veterans Affairs. Participants were largely overweight, with 78.9% in Project LIFE and 70.9% in Project LEAD reporting a body mass index of 25 or greater. Sixty-eight percent of individuals reported less than 150 min/week of moderate PA. Although participants reported an average of 162 minutes of moderate- or higher-intensity PA per week from the CHAMPS assessment at baseline, a large proportion of this PA came from a small number of individuals who reported high amounts of heavy household activities and gardening. In both studies, the top two reported physical activities were heavy gardening and heavy housework. Only 15% performed what would be considered structured exercise (walking, hiking, jogging, cycling, use of exercise machines, strength training) for more than 150 min/week. The average baseline PF score was 63.2 (scale scores range from 0 to 100 with higher scores indicating better function), which approximates the 60th percentile of age-based norms for men and women aged 75 and older.16
Table 1.
Baseline Characteristics of Study Participants (N = 357)
| Characteristic | Life (N = 175) | Lead (N = 182) | Combined (N = 357) |
|---|---|---|---|
| Age, mean ± SD | 78.3 ± 5.2 | 71.7 ± 5.0 | 74.9 ± 6.1 |
| Minority race, % | 25.1 | 17.6 | 21.3 |
| Male, % | 99.4 | 42.9 | 70.6 |
| Number of diseases, mean ± SD | 5.2 ± 2.6 | 3.6 ± 2.1 | 4.4 ± 2.5 |
| Body mass index, mean ± SD | 27.9 ± 4.6 | 27.6 ± 5.2 | 27.7 ± 4.9 |
| Physical function, mean ± SD | 58.8 ± 26.6 | 68.3 ± 21.0 | 63.6 ± 24.4 |
| Physical activity < 150 min/week, % | 63.4 | 72.5 | 68.1 |
SD = standard deviation.
Association Between PA and PF
PF was significantly different in individuals reporting more than or less than 150 min/week of moderate PA. Individuals reporting 150 min/week or more of PA had a mean PF score of 74.5, which was approximately 15.9 ± 2.6 points higher than those reporting lower amounts of PA (PF = 58.6, P<.001), controlling for age, race, sex, and study.
Effect of Change or No Change in Exercise Minutes Threshold on Functional Trajectory
Table 2 provides the results of the stratified and combined analyses employed in this study and includes control for baseline PF, age, race, and sex. Baseline PA was not a statistically significant predictor of PF at 6 months in either of the individual trials, but the combined weighted effect was significant (P =.02) and indicated an average difference in 6-month score of 6.08 between each baseline PA stratum (≥ 150 min/week and <150 min/week). Change in PA between baseline and 6 months occurred in two directions. For individuals decreasing from 150 min/week or more of PA at baseline to less than 150 min/week of PA at 6 months, the combined weighted average effect indicated a significant decline in PF of 11.8 points (P<.001). A decline of this magnitude, given the average raw baseline score of 62.8, has been associated with greater 4-year mortality risk.21
Table 2.
Effect of Change in Physical Activity (PA) Level on Physical Function (PF)
| Life |
Lead |
Combined* |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| Variable | β | SE | P-Value | β | SE | P-Value | Average Weighted Effect | Average Weighted SE | P-Value |
| Baseline PA | 6.5 | 3.40 | .06 | 5.61 | 3.71 | .13 | 6.09 | 2.51 | .02 |
| Decrease in PA | -15.2 | 5.1 | .003 | -8.89 | 4.72 | .03 | -11.80 | 3.46 | <.001 |
| Increase in PA | 2.08 | 3.33 | .55 | 10.25 | 4.36 | .03 | 5.10 | 2.64 | .05 |
| No change in PA | Reference | Reference | Reference | Reference | Reference | Reference | Reference | Reference | Reference |
| Baseline PF | 0.85 | 0.05 | <.001 | 0.69 | 0.06 | <.001 | |||
| Age | -0.18 | 0.24 | .44 | -0.56 | 0.26 | .03 | |||
| Race | -2.99 | 2.82 | .29 | -2.52 | 3.25 | .44 | |||
| Sex | 11.0 | 15.6 | .48 | 2.92 | 2.57 | .26 | |||
| Number of diseases | -0.39 | 0.53 | .47 | -1.13 | 0.62 | .07 | |||
Note: To facilitate a clinical interpretation of the effect sizes, the betas for change in physical activity level, either decrease or increase, can be added or subtracted to the average weighted baseline PF score of 63.2; range of scale is 0 to 100, with higher scores indicating better function.
Includes control for age, race, sex, baseline PF, and number of diseases.
SE = standard error.
In contrast, for individuals increasing from less than 150 min/week of PA at baseline to 150 min/week or more of PA at 6 months, the combined weighted average effect indicated an increase in PF of 5.1 points (P =.05). A change of this magnitude, although moderate, given the average raw baseline score of 58.6, would be comparable with gains observed after laparoscopic surgery for inguinal hernia or treatment of asthma with flucticasone.22
To simplify the graphical presentation of these data, the pooled values were used to illustrate the functional trajectories over time for the entire study sample (Figure 1). Four groups are depicted using raw mean scores and standard errors: individuals reporting 150 min/week or more of PA at baseline and 6 months (n = 57), individuals reporting 150 min/week or more of PA at baseline who dropped below 150 min/week of PA at 6 months (n = 52), individuals reporting less than 150 min/week of PA at baseline who increased to 150 min/week or more of PA at 6 months (n = 44), and individuals reporting less than 150 min/week of PA at baseline and 6 months (n = 173). Although the predictive models fixed “no change in PA status” as the reference group, the trajectories in Figure 1 indicate that individuals who maintained PA levels throughout the study period maintained their functional level.
Figure 1.
Physical function over time based on reported physical activity over time. Baseline and 6-month data points are the raw means ± standard errors of pooled data. The numeric estimates of change written on the slopes are weighted average estimates from the meta-analysis and should be interpreted as such. PA 5 physical activity.
DISCUSSION
The overlap in PA and PF outcomes of these two studies presented a unique opportunity to examine the effect of the SG-endorsed PA guidelines on PF. The recommended 150 minutes of moderate PA per week or more is well integrated into clinical practice,23 yet there is a paucity of data pertaining to the direct functional effect of these guidelines on older adults. Maintenance of PF is considered a hallmark of successful aging.24 One limitation in assessing global PF as an outcome relative to PA is that it potentially requires a large sample size. Estimates of projected sample sizes needed to obtain clinically meaningful changes in a variety of outcomes following a PA intervention have been previously published.13 Estimates projected for global PF measures required the largest sample size (N = 261 per group in a two-armed trial). A sample size of this magnitude is frequently beyond the reach of most PA interventionists. By pooling two modest-sized intervention trials, which used identical measures of PA and PF, it was possible to obtain a large enough sample and enhance generalizability to address the research questions relative to the association between PA and PF and whether change in PA affects the functional trajectory.
This study confirms that PA is an important contributor to PF, given the strong cross-sectional and longitudinal association between PA and PF. This study is unique in assessing PA relative to the specific threshold set by the national recommendations. For the first time, to the authors' knowledge, clinicians will be better able to characterize functional differences between individuals meeting or failing to meet PA guidelines. The 16-point difference in PF observed in this study is substantial. Of subjects exceeding PA guidelines, the baseline PA score of 74 was at approximately the 70th percentile of PF for mean and women aged 75 and older.16 A reduction of 16 points in PF would be comparable with the combined comorbidity burden of arthritis and congestive heart failure.22 Therefore, these findings are clinically meaningful.
A cross-sectional view is limited in that one cannot determine whether individuals with low PF had conditions that inhibited their ability to be physically active. Therefore, the second research objective, using longitudinal trajectories of PF, allowed the independent effect of the PA threshold on functional status to be examined. As a group, individuals who changed PA level also experienced a change in functional status. This is of particular interest to inactive individuals with poor functional status. Individuals who, independent of functional status, were able to increase their PA level improved 5.1 points in PF from an average baseline score of 63.4. As was noted earlier, a change in PF of this magnitude is clinically meaningful and would be comparable with medical interventions such as treatment for asthma with fluticasone versus placebo and treatment of sleep apnea with continuous positive airway pressure.22 The changes noted in the current study are comparable, in trajectory but not magnitude, with changes observed in a study of older patients with severe chronic obstructive pulmonary disease (baseline PF = 30) whose PF score increased 9 points after a pulmonary rehabilitation program.25 The difference in magnitude of change makes sense, given that the interventions were of home-based PA in contrast to a medically supervised structured exercise program. Two other studies have examined PA relative to global PF (physical disability) and found a protective effect of PA on incident disability, but in these studies, the rates of PA were not specific to the threshold levels purported by the SG guidelines.26,27 These studies, in addition to the current one, are highly relevant, because they suggest that exercise initiated in later life is highly beneficial.
Conversely, a reduction in PA level is associated with a clinically meaningful reduction in PF. Unfortunately it was not possible to determine the causes of the decreases in PA levels (whether reductions were due to sudden illness, injury, caregiving needs, or lack of interest). Nonetheless, a reduction in PA level was associated with a clinically meaningful loss in PF at a level that is associated with a greater inability to work because of health problems, the onset of a disease such as congestive heart failure, or the combined functional burden of diabetes mellitus and hypertension.22
The functional trajectory of individuals who maintained PA, although not surprising, is equally important in confirming that PF is preserved with maintenance of PA. An earlier study examined functional trajectories in a group of older women who sustained PA, sustained inactivity, or were irregularly active over several years and found lower rates of reported difficulty with activities of daily living in the women who were consistently active.11 Other studies confirming this finding have used tests of physical performance such as gait speed and walking ability to determine PF.11,12 This article is a contribution to the field, because the literature pertaining to PA and global PF is so sparse. A review article of exercise intervention outcomes found that 97% of outcomes reported were fitness impairment outcomes (e.g., improved strength, aerobic capacity, flexibility), and although 87% of studies reported functional outcomes, most of these were based on physical performance tests such as walking or stair climbing. A global indicator of health-related PF was rarely assessed.3
Although this pooled analysis offers valuable findings, there are limitations that must be borne in mind in generalizing these data. One limitation is that the measures, although validated, are based on self-report. Although self-report of PF is considered to be a reliable indicator of functional status, self-report of PA is more prone to misclassification. Both studies had a single-item screening question designed to exclude individuals engaging in regular exercise. The screening items targeted structured exercise and not general physical activities. In contrast, the PA outcomes in this study were derived from the moredetailed CHAMPS questionnaire, which assesses all types of PA. Although 68% of the sample reported less than 150 min/week of PA, the average number of reported minutes of PA was 162. This suggests that the single-item screening question was not sensitive enough to capture nonexercise PA that typically count toward the assessment of total daily PA, especially with regard to gardening and household activities, or that some individuals may have overreported their PA. Thus these data should be interpreted conservatively. Also, consideration should be given to potential sex differences in that this sample consisted predominantly of men and the findings may be less applicable to women.
In conclusion, this study is an initial step in quantifying the relationship between evidence-based guidelines for PA and PF in older adults. The guidelines endorsed by the SG were based upon an exhaustive review of the evidence. The current study confirms the validity of the SG recommendation and adds insight to the utility of the recommendation for older adults. Newly released PA recommendations for older adults advocate strength training and flexibility exercises in addition to the recommendation to perform moderate PA for 30 minutes on 5 or more days of the week.23 Although adoption of these guidelines will strengthen the association between PA and PF, prospective trials assessing the effect of these guidelines on functional status are warranted.
ACKNOWLEDGMENTS
We dedicate this manuscript to the memory of our esteemed and beloved colleague, Elizabeth “Jody” Clipp. Words cannot describe her contribution to our lives.
Conflict of Interest: The editor in chief has reviewed the conflict of interest checklist provided by the authors and has determined that the authors have no financial or any other kind of personal conflicts with this manuscript. Supported by research grants E2788-RA from the Department of Veterans Affairs Rehabilitation Research and Development and P60-AG11268, P30-AGO28716, and R01-CA106919 from the National Institutes of Health.
Footnotes
Sponsor's role: Limited to approval and funding of the research.
REFERENCES
- 1.U.S. Department of Health and Human Services . Physical Activity and Health: A Report of the Surgeon General. U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion; Atlanta, GA: 1996. [Google Scholar]
- 2.U.S. Department of Health and Human Services . Physical Activity and Older Americans, 2001. Agency for Healthcare Research and Quality, Centers for Disease Control, U.S. Department of Health and Human Services; 2002. [Google Scholar]
- 3.Keysor JJ, Jette AM. Have we oversold the benefit of late-life exercise? J Gerontol A Biol Sci Med Sci. 2001;56A:M412–M423. doi: 10.1093/gerona/56.7.m412. [DOI] [PubMed] [Google Scholar]
- 4.van der Bij AK, Laurant MGH, Wesing M. Effectiveness of physical activity interventions for older adults. Am J Prev Med. 2001;22:120–133. doi: 10.1016/s0749-3797(01)00413-5. [DOI] [PubMed] [Google Scholar]
- 5.Cress ME, Buchner DM, Prohaska T, et al. Physical activity programs and behavior counseling in older adult populations. Med Sci Sports Exerc. 2004;36:1997–2003. doi: 10.1249/01.mss.0000145451.08166.97. [DOI] [PubMed] [Google Scholar]
- 6.Cress ME, Buchner DM, Prohaska T, et al. Best practices for physical activity programs and behavior counseling in older adult populations. J Aging Phys Act. 2005;13:61–74. doi: 10.1123/japa.13.1.61. [DOI] [PubMed] [Google Scholar]
- 7.King AC, Rejeski WJ, Buchner DM. Physical activity interventions targeting older adults. A critical review and recommendations. Am J Prev Med. 1998;15:316–333. doi: 10.1016/s0749-3797(98)00085-3. [DOI] [PubMed] [Google Scholar]
- 8.Latham NK, Bennett DA, Stretton CM, et al. Systemaic review of progressive resistance strength training in older adults. J Gerontol A Biol Sci Med Sci. 2004;59A:48–61. doi: 10.1093/gerona/59.1.m48. [DOI] [PubMed] [Google Scholar]
- 9.Larson EB, Wang L, Bowen JD, et al. Exercise is associated with reduced risk for incident dementia among persons 65 years of age and older. Ann Intern Med. 2006;144:73–81. doi: 10.7326/0003-4819-144-2-200601170-00004. [see comment][summary for patients in Ann Intern Med 2006;144:I20; PMID: 16418403] [DOI] [PubMed] [Google Scholar]
- 10.Brown DW, Brown DR, Heath GW, et al. Associations between physical activity dose and health-related quality of life. Med Sci Sports Exerc. 2004;36:890–896. doi: 10.1249/01.mss.0000126778.77049.76. [DOI] [PubMed] [Google Scholar]
- 11.Brach JS, FitzGerald S, Newman AB, et al. Physical activity and functional status in community-dwelling older women: A 14-year prospective study. Arch Intern Med. 2003;163:2565–2571. doi: 10.1001/archinte.163.21.2565. [DOI] [PubMed] [Google Scholar]
- 12.Brach JS, Simonsick EM, Kritchevsky S, et al. The association between physical function and lifestyle activity and exercise in the health, aging and body composition study. J Am Geriatr Soc. 2004;52:502–509. doi: 10.1111/j.1532-5415.2004.52154.x. [DOI] [PubMed] [Google Scholar]
- 13.Morey MC, Ekelund CC, Pearson MP, et al. Project LIFE: A partnership to increase physical activity in elders with multiple chronic illnesses. J Aging Phys Act. 2006;14:324–343. doi: 10.1123/japa.14.3.324. [DOI] [PubMed] [Google Scholar]
- 14.Demark-Wahnefried W, Morey MC, Clipp EC, et al. Leading the way in exercise and diet (Project LEAD): Intervening to improve function among older breast and prostate cancer survivors. Control Clin Trials. 2003;24:206–223. doi: 10.1016/s0197-2456(02)00266-0. [DOI] [PubMed] [Google Scholar]
- 15.Demark-Wahnfried W, Clipp EC, Morey MC, et al. Lifestyle intervention development study to improve physical function in older adults with cancer: Outcomes from Project LEAD. J Clin Oncol. 2006;24:3465–3473. doi: 10.1200/JCO.2006.05.7224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ware JE, Jr., Snow K, Kosinski M, et al. SF-36® Health Survey: Manual and Interpretation Guide. Quality Metric Incorporated; Lincoln, RI: 2000. [Google Scholar]
- 17.Stewart AL, Mills KM, King AC, et al. CHAMPS physical activity questionnaire for older adults: Outcomes for interventions. Med Sci Sports Exerc. 2001;33:1126–1141. doi: 10.1097/00005768-200107000-00010. [DOI] [PubMed] [Google Scholar]
- 18.Ware JE, Sherbourne CD. The MOS 36-Item Short-Form Health Survey (SF-36) Med Care. 1992;30:473–483. [PubMed] [Google Scholar]
- 19.Fillenbaum GG. OARS Multidimensional Functional Assessment Questionnaire. In: Maddox G, editor. The Encyclopedia of Aging. Springer; New York: 1987. [Google Scholar]
- 20.Hedges LV, Olkin I. Statistical Methods for Meta Analyses. Academic Press; Orlando: 1895. [Google Scholar]
- 21.Ware JE, Bayliss MS, Rogers WH, et al. Differences in 4-year health outcomes for elderly and poor, chronically ill patients treated in HMO and fee-for-service systems. JAMA. 1996;276:1039–1047. [PubMed] [Google Scholar]
- 22.Alonso J, Ferrer M, Gandek B, et al. Health-related quality of life associated with chronic conditions in eight countries: Results from the International Quality of Life Assessment (IQOLA) Project. Qual Life Res. 2004;13:283–298. doi: 10.1023/b:qure.0000018472.46236.05. [DOI] [PubMed] [Google Scholar]
- 23.Nelson ME, Rejeski WJ, Blair SN, et al. Physical activity and public health in older adults: Recommendation from the American College of Sports Medicine and the American Heart Association. Circulation. 2007;116:1094–1105. doi: 10.1161/CIRCULATIONAHA.107.185650. [DOI] [PubMed] [Google Scholar]
- 24.Rowe JW, Kahn RL. Successful Aging. Pantheon Books; New York: 1998. Productivity in Old Age; pp. 167–180. [Google Scholar]
- 25.Boueri FM, Bucher-Bartelson BL, Glenn KA, et al. Quality of life measured with a generic instrument (Short Form-36) improves following pulmonary rehabilitation in patients with COPD. Chest. 2001;119:77–84. doi: 10.1378/chest.119.1.77. [DOI] [PubMed] [Google Scholar]
- 26.Boyle PA, Buchman AS, Wilson RS, et al. Physical activity is associated with incident disability in community-based older persons. J Am Geriatr Soc. 2007;55:195–201. doi: 10.1111/j.1532-5415.2007.01038.x. [DOI] [PubMed] [Google Scholar]
- 27.Berk DR, Hubert HB, Fries JF. Associations of changes in exercise level with subsequent disability among seniors: A 16-year longitudinal study. J Gerontol A-Biol Sci Med Sci. 2006;61A:97–102. doi: 10.1093/gerona/61.1.97. [DOI] [PubMed] [Google Scholar]