Abstract
Objective
Very few studies have addressed the relationship between number of peritoneal dialysis (PD) patients treated at a clinic (PD clinic size) and clinical outcomes. In a national prospective cohort study of incident PD patients (n=236, from 26 clinics), we examined whether being treated at a larger PD clinic [≥50 PD patients (n=3 clinics) vs. <50 PD patients (n=23 clinics)] was associated with better patient outcomes, including fewer switches to hemodialysis, fewer cardiovascular events, lower cardiovascular mortality, and lower all-cause mortality.
Methods
Multivariable Cox models were used to assess relative hazards (RHs) for modality switches, cardiovascular events, cardiovascular deaths, and all-cause deaths by PD clinic size. All models were adjusted for demographics, comorbidities, laboratory values, and clinic years in operation.
Results
Being treated at a clinic with ≥50 patients was associated with fewer switches to hemodialysis (RH=0.13, 95% CI, 0.06-0.31) and fewer cardiovascular events (RH=0.62, 95% CI, 0.06-0.98). No associations of PD clinic size with cardiovascular or all-cause mortality were seen.
Conclusion
PD patients that are treated at clinics with greater numbers of PD patients may have better outcomes in terms of technique failure and cardiovascular morbidity. PD clinic size may act as a proxy of greater PD experience, more focus on the modality, and better PD practices at the clinic, resulting in better outcomes.
Keywords: peritoneal dialysis, clinic size, technique failure, cardiovascular morbidity, mortality
Introduction
Dialysis clinics that offer peritoneal dialysis (PD) vary widely in the number of PD patients they treat: some clinics may have only a few patients at a time, while others may be entirely devoted to PD and have dozens of PD patients. The number of PD patients treated, or PD clinic size, may act as a proxy for the clinic's PD experience and investment in the modality. Clinics with larger PD clinic size may devote more time and staff to establishment and maintenance of good PD practices; conversely, staff may be overwhelmed by a large patient load and be less able to give patients individual attention. Whether PD patients treated at clinics with a larger PD clinic size have better or worse outcomes has not been well-studied.
One possible adverse outcome for PD patients is technique failure, in which the patient starts on PD and must switch to hemodialysis. Although some patients may switch due to personal choice, often the reasons are related to infection, catheter issues, inadequate dialysis, or psychosocial issues (1). Approximately 20-25% of PD patients switch modality to hemodialysis in the first year, and by 4 years the rate is approximately 50% (1;2). A recent study of administrative data on four large cohorts of U.S. adult PD patients showed that greater number of PD patients treated at a center was a powerful predictor of greater technique survival (1), and a study in the Netherlands also showed that larger clinics had fewer technique failures (3).
Other patient outcomes may also be affected by PD clinic size, including morbidity and mortality. A Canadian study showed that a greater cumulative number of PD patients treated at a clinic was associated with decreased mortality among the patients treated at such clinics (4). The authors postulated that this association was due to the clinics with more experience (reflected by the cumulative number of patients) adopting better PD practices or choosing more appropriate patients for PD, or both. For these same reasons, cardiovascular events and mortality could also be decreased among patients at clinics with large PD clinic size.
Few studies have examined the relationship between PD clinic size and outcomes in incident patients well-characterized with regard to not only demographics but also comorbid disease status and other clinical and laboratory characteristics. In a national prospective cohort study of incident PD patients, we examined whether being treated at a larger PD clinic was associated with better patient outcomes, including fewer switches to hemodialysis, fewer cardiovascular events, lower cardiovascular mortality, and lower all-cause mortality.
Materials and Methods
Study Design
Our cohort for this cross-sectional study consisted of 236 incident PD patients from the ESRD Quality (EQUAL) Study who were treated at 26 free-standing outpatient dialysis clinics in 13 states throughout the United States. All PD modalities (continuous ambulatory PD, continuous cycling PD, and intermittent cycling PD) were combined as a single category. The EQUAL cohort was assembled from the Choices for Healthy Outcomes in Caring for End-Stage Renal Disease (CHOICE) study (5), which enrolled 1041 incident dialysis patients (767 hemodialysis, 274 PD) at 81 dialysis clinics in 19 states between October 1995 and June 1998. The CHOICE study was based upon a collaborative relationship between Johns Hopkins University and Dialysis Clinic, Inc. (DCI), New Haven CAPD, and St. Raphael's Hospital. To be eligible, patients had to be older than 18 years of age and speak either English or Spanish. Median time from dialysis initiation to enrollment was 45 days, with 98% enrolling within 4 months of initial dialysis. Informed consent was obtained from each patient. Institutional review boards for the Johns Hopkins University School of Medicine and clinical centers approved the study protocol.
Data Collection
Independent Variable
As part of the EQUAL Study, a questionnaire was administered to medical directors or head nurses at the 81 participating clinics in October 1998. The questionnaire collected information regarding customary practice for several processes of care (6-8). For this study, our independent variable was derived from questionnaire items related to PD processes of care, and only those responses from clinics with PD patients enrolled in CHOICE (n=30) were examined. PD clinic size was derived from the item “How many peritoneal dialysis patients were dialyzed at your clinic in October 1998?” with possible responses of “None,” “Less than 25 patients,” 25-50 patients,” “51-100 patients,” “101-200 patients,” and “More than 200 patients.” Of the 30 clinics that enrolled PD patients, 26 (87%) responded to this item, representing 236 of the 274 total PD patients. The distribution of patients according to clinic response was: none, 1%; <25, 17%; 25-50, 26%; 51-100, 9%; 101-200, 48%; and >200, 0%. Due to small numbers of patients in the individual categories, we collapsed responses into two categories (50 or fewer patients vs. more than 50 patients) for all analyses. We chose the 50-patient size cutoff this gave a fairly even distribution of patients, and we planned to do patient-level outcomes analyses.
Outcome Ascertainment
Our outcome variables included modality switch (to hemodialysis), cardiovascular events, cardiovascular mortality, and all-cause mortality. Modality switches were defined as switches to hemodialysis that lasted more than 30 days, as described previously (2).
Non-fatal cardiovascular events were assigned by the following algorithm: (i) adjudicated records (from medical chart review) were considered the primary source of information for a non-fatal cardiovascular event, regardless of whether it was a procedure or non-procedure event; (ii) in the absence of an adjudicated record, any USRDS billing data record or report from DCI confirmed a procedure event; (iii) for non-procedure events without an adjudicated record, the algorithm for assigning cardiovascular events was: (a) any USRDS or HCFA billing data record allowed assignment of the cardiovascular event; (b) a clinic record, when supported by a corresponding comorbidity record, allowed assignment of the event; and (c) subsequent cardiovascular events in the same broad category within 30 days of discharge from a prior hospitalization for an assigned cardiovascular event were not assigned as separate events. Cardiovascular events included myocardial infarction, cerebrovascular accident, and the following ASCVD-related procedures: abdominal aortic aneurysm, percutaneous transluminal coronary angioplasty, coronary artery bypass graft, carotid endarterectomy, peripheral bypass of the lower extremity, and amputations (excluding digit amputations).
For fatal cardiovascular events, cardiovascular cause of death was assigned according to the following hierarchy: (i) the immediate cause of death from the adjudicated record, if cardiovascular-related; (ii) the underlying cause of death from the adjudicated record, if cardiovascular-related; and (iii) the first listed cardiovascular-related cause in the National Death Index (NDI) record, excluding contributing causes; otherwise death was considered non-cardiovascular. The first cardiovascular event (fatal or non-fatal) during the study period was considered as an incident cardiovascular event; fatal cardiovascular causes of death were considered cardiovascular mortality. All-cause mortality information was ascertained from NDI records, clinic report, medical records, and Centers for Medicare & Medicaid Services (CMS; death notification forms and Social Security records). Follow-up for cardiovascular events and mortality continued until death, transplantation, or the last follow-up date of December 31, 2004.
Other Variables
Data on patients' demographics (age, sex, and race) and socioeconomic status (education, employment, and marital status) were collected from a baseline self-report questionnaire. Presence and severity of comorbid conditions were assessed at baseline using the Index of Coexistent Disease (ICED), whose composite integer score ranges from 0-3 (with 3 as the highest severity level) (9;10). Presence of individual conditions, including diabetes, was determined from the same medical record review process through which ICED was determined. Late referral was defined as a time between first nephrologist evaluation and start of dialysis of less than 4 months, as described previously (11). Laboratory values and height and weight [used to calculate body mass index (BMI)] were obtained from patients' records and from the CMS Medical Evidence report (CMS Form 2728). Clinic years in operation were obtained along with the independent variable from the facility questionnaire, as described above.
Statistical Methods
We first compared patient characteristics by dichotomized measures of processes of care, using Pearson's χ2 tests for categorical variables and two-sided t tests for continuous variables. Kaplan-Meier estimates were calculated for time to modality switch, first cardiovascular event, cardiovascular mortality, and all-cause mortality; multivariable Cox models were used to obtain relative hazards of the outcomes by PD clinic size. Due to concerns about possible bias in the >50 patient group (representing only 3 clinics), we also performed sensitivity analyses, in which outcomes were examined using a 25-patient cutoff. This cutoff gave an even distribution of clinics rather than patients.
Variables were chosen as covariates for the adjusted models if they were confounders (i.e., significantly associated with both the PD clinic size and patient outcomes) or previously shown to be associated with patient outcomes. All analyses were performed using STATA v. 9.1 (College Station, Texas).
Results
Patient Characteristics by Peritoneal Dialysis Clinic Size
Table 1 shows the total number of dialysis clinics and enrolled PD patients represented in our cohort for each possible categorical response regarding PD clinic size on the facility survey sent to CHOICE clinics. Compared to 112 PD patients treated at clinics reporting fewer than 50 PD patients, 124 PD patients treated at clinics with more than 50 PD patients were older, had fewer comorbidities, had higher BMI, and were more likely to have been referred late to a nephrologist (Table 2). Additionally, these patients were also seen at clinics that had been operating longer, had more frequent physician visits, and had shorter initial PD training.
Table 1.
Numbers of dialysis clinics and PD patients enrolled in CHOICE for each possible reported PD clinic size (total number of PD patients reported at clinic)
| Total number of PD patients reported at clinic | Number of clinics | Number of PD patients enrolled in CHOICE* |
|---|---|---|
| None | 4 | 9 |
| <25 | 9 | 41 |
| 25-50 | 10 | 62 |
| 51-100 | 1 | 19 |
| 101-200 | 2 | 105 |
| >200 | 0 | 0 |
| Total | 26 | 236 |
Patient enrollment in CHOICE occurred over a nearly 3-year period, from October 1995 to June 1998; our cross-sectional facility survey was distributed in October 1998. Thus, the numbers of patients being treated with PD in the clinic may have differed between time of patient enrollment and the facility survey, from which we obtained PD clinic size. Additionally, although clinics reported PD clinic size as the total number of PD patients treated at their clinic, not all treated patients were enrolled in the CHOICE study.
Table 2.
Baseline patient and facility characteristics by whether patients were treated at facilities reporting larger (>50 PD patients) or smaller (≤50 PD patients) size
| PD clinic size |
||
|---|---|---|
| Characteristic | ≤50 PD patients | >50 PD patients |
| No. (%) of patients | 112 (47.5%) | 124 (52.5%) |
| No. (%)of clinics | 23 (88.5%) | 3 (11.5%) |
| Patient Characteristics: | ||
| Demographic | ||
| Mean age (SD), years | 51.5 (13.9)* | 56.3 (15.6)* |
| Sex (% male) | 54.5 | 58.1 |
| Race (% white) | 75.0 | 75.8 |
| Education (% HS graduate) | 81.7 | 85.0 |
| Employment (% employed) | 23.2 | 29.0 |
| Marital status (% married) | 61.3 | 70.6 |
| Clinical | ||
| ICED (% score of 3) | 26.8* | 21.0* |
| Mean BMI (SD) | 25.8 (5.6)* | 27.5 (6.1)* |
| Diabetes mellitus (% diabetic) | 58.0 | 48.4 |
| Late referral (% <4 months to dialysis) | 14.0* | 26.7* |
| Laboratory | ||
| Mean albumin (SD), g/dl | 3.56 (0.38) | 3.63 (0.46) |
| Mean creatinine (SD), mg/dl | 7.44 (2.75) | 7.20 (2.65) |
| Mean hemoglobin (SD), g/dl | 11.2 (1.5) | 11.3 (1.4) |
| Facility Characteristics: | ||
| Mean years (SD) in operation | 16.5 (6.3)* | 18.3 (2.9)* |
| Frequency of physician visit (% monthly) | 92.4* | 100.0* |
| Length of PD training (% ≤1 week) | 75.2** | 100.0** |
BMI: body mass index; IQR: interquartile range.
P < 0.05;
P<0.001, by t test (continuous variables) or χ2 or Fisher's exact test (categorical variables).
Association of Peritoneal Dialysis Clinic Size with Modality Switch to Hemodialysis
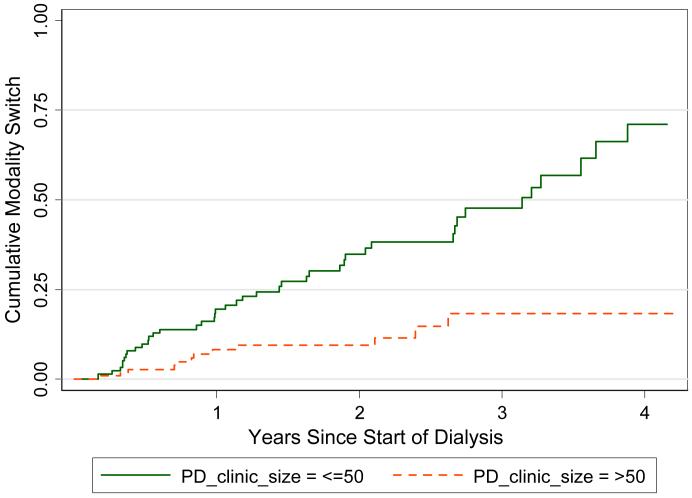
Fig. 1 shows that the cumulative incidence of modality switches from PD to hemodialysis was much less in the clinics with more than 50 PD patients. This association held up to adjustment for demographics, clinical characteristics, laboratory values, and clinic years in operation (Table 3), with the risk of switching to HD being 74-86% less in those patients treated at clinics with more than 50 patients overall.
Fig. 1.
Kaplan-Meier curve of cumulative modality switch to HD by PD clinic size. P<0.001 by log-rank test.
Table 3.
Association of PD clinic size (>50 vs. ≤50 PD patients) with clinical outcomes
| Outcome | Crude Rate | Model | |||
|---|---|---|---|---|---|
| Unadjusted | +Demographics | +Clinical | +Laboratory | ||
| Switching Modality toHD | % switching | Relative Hazard (95% CI) | |||
| ≤50 PD patients | 37.5% | 1.00 (ref.) | 1.00 (ref.) | 1.00 (ref.) | 1.00 (ref.) |
| >50 PD patients | 9.7% | 0.26 (0.14-0.50)* | 0.25 (0.13-0.48)* | 0.20 (0.10-0.42)* | 0.13 (0.06-0.31)* |
| Cardiovascular Events | Incidence per pt-yr | Relative Hazard (95% CI) | |||
| ≤50 PD patients | 0.22 | 1.00 (ref.) | 1.00 (ref.) | 1.00 (ref.) | 1.00 (ref.) |
| >50 PD patients | 0.12 | 0.54 (0.35-0.84)* | 0.45 (0.29-0.70)* | 0.57 (0.35-0.93)* | 0.61 (0.38-0.98)* |
| Cardiovascular Mortality | Incidence per pt-yr | Relative Hazard (95% CI) | |||
| ≤50 PD patients | 0.09 | 1.00 (ref.) | 1.00 (ref.) | 1.00 (ref.) | 1.00 (ref.) |
| >50 PD patients | 0.05 | 0.69 (0.33-1.44) | 0.63 (0.30-1.34) | 1.03 (0.45-2.34) | 1.05 (0.46-2.40) |
| All-cause mortality | Incidence per pt-yr | Relative Hazard (95% CI) | |||
| ≤50 PD patients | 0.18 | 1.00 (ref.) | 1.00 (ref.) | 1.00 (ref.) | 1.00 (ref.) |
| >50 PD patients | 0.15 | 0.91 (0.57-1.46) | 0.78 (0.48-1.26) | 1.31 (0.76-2.24) | 1.35 (0.78-2.35) |
Demographics: age, sex, and race; clinical: ICED score, diabetic status, and BMI; laboratory: albumin and creatinine.
P < 0.05.
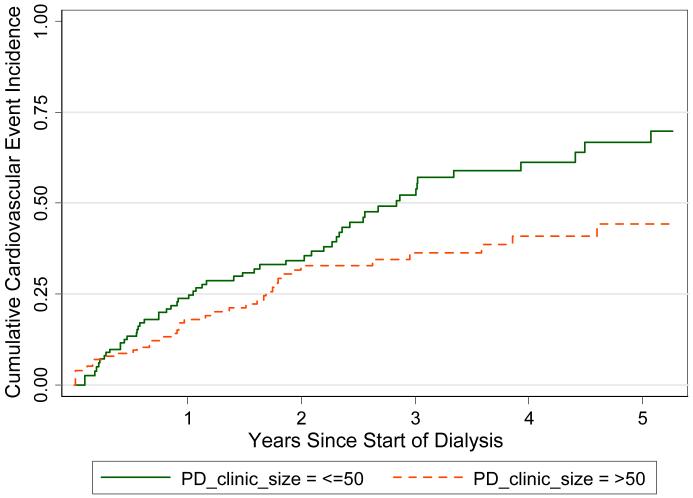
Association of Peritoneal Dialysis Clinic Size with Cardiovascular Events, Cardiovascular Mortality, and All-Cause Mortality
Cumulative cardiovascular event incidence was less in the larger clinics (Fig. 2). This 38-55% lower risk of cardiovascular event incidence in patients treated at larger clinics was independent of adjustment for demographics, clinical characteristics, laboratory values, and clinic years in operation (Table 3). Although the relative hazard for cardiovascular mortality indicated that incidence was lower in the larger clinics, these associations were not statistically significant and disappeared after adjustment for comorbidity (Table 3). Finally, no associations of PD clinic size and all-cause mortality were seen in this study (Table 3).
Fig. 2.
Kaplan-Meier curve of cumulative cardiovascular event incidence by PD clinic size. P=0.007 by log-rank test.
Sensitivity Analyses
Using a clinic size cutoff of 25 rather than 50 patients (giving an equal number of clinics in each group), we found that the results were generally quite similar to those using the original cutoff. Those in the larger (≥25 patients) PD clinics were less likely to switch modality (adjusted RH=0.23, 95% CI, 0.12-0.43; P<0.001) and less likely to have a CVD event (adjusted RH=0.55, 95% CI, 0.33-0.92; P=0.023). As with the 50-patient cutoff, clinic size using a 25-patient cutoff was not associated with either cardiovascular or all-cause mortality.
Discussion
In this national prospective cohort study, we found that PD patients who were treated at clinics with greater numbers of PD patients were at lower risk of switching to hemodialysis and cardiovascular events. The associations of decreased switching to hemodialysis and cardiovascular events with larger PD clinic size were consistent, regardless of adjustments for demographics, comorbidities, body size, albumin, creatinine, and clinic years in operation; the results were also robust to a change in clinic size cutoff. No association of PD clinic size with cardiovascular mortality or all-cause mortality was seen.
Our results showing that patients treated at clinics with greater numbers of PD patients were far less likely to switch to hemodialysis over the course of the study are consistent with previous reports showing decreased technique failure with large PD clinic size (3;4). Greater numbers of PD patients at a clinic reflect a greater investment in the PD modality, in terms of both staff and time dedicated to training and patient care. Such an investment could result in better overall PD practices, more individual time spent with PD patients, and more efficient training of PD patients, in turn resulting in fewer complications (or better management of complications) that lead to modality switching. The staff at these large clinics may also have strong incentive to encourage patients to stay with PD for as long as possible. Additionally, clinical staff caring for a larger number of PD patients have probably logged more PD experience than those caring for fewer PD patients and may be more adept at recruiting the best candidates for this modality, and such candidates would have fewer reasons to switch to hemodialysis.
The occurrence of cardiovascular events was also decreased in patients treated at clinics with greater numbers of PD patients. Greater staffing and better training at clinics that have more PD patients may lead to more opportunities for cardiovascular disease prevention through dietary or medication adherence. Such clinics could also have better, more established, referral systems—including pre-transplant evaluation and comprehensive cardiovascular workups—and better management, including improved fluid volume management (12); these improvements could prevent some cardiovascular events. Another possibility is that these larger, more established clinics recruit fewer patients with severe cardiovascular disease, although, since we adjusted for presence and severity of comorbid conditions, this would likely not completely explain the association we found.
Finally, we saw no association of PD clinic size with cardiovascular mortality after adjustment for comorbidity, although there was a non-significant trend toward decreased risk without this adjustment. The leading cause of mortality in dialysis patients is cardiovascular disease, and it may be that the inflammatory processes and hypertension that go along with dialysis cannot be sufficiently controlled to prevent cardiovascular death, even if intermediate events can be reduced. We also found that all-cause mortality was not decreased in patients treated at clinics with greater numbers of PD patients, although one Canadian study did find such an association with cumulative numbers of PD patients treated (4). It may be that differences between Canada and the United States account for this difference (13), or it may be that cumulative number of patients treated is a better marker of PD experience than a cross-sectional determination of number of patients treated in PD clinics.
Some limitations of this study deserve mention. First, measure of PD clinic size was taken cross-sectionally at the start of the study. PD practice may have changed over time. Additionally, clinic size does not necessarily completely reflect clinic experience, since we did not have information on staff experience, which may be greater in some of the smaller clinics. Second, we had no information on the characteristics of the PD trainers, and it has been recommended that trained, experienced nurses provide PD training whenever possible to improve outcomes (14). Third, the number of clinics being examined is small and imbalanced in terms of size (3 larger clinics versus 23 smaller clinics); although we performed sensitivity analyses with balanced numbers of clinics and showed similar results, the possibility of bias cannot be discounted. Finally, the observational design of the study does not allow for causal inference, and, despite measurement of and adjustment for many patient and clinic characteristics, there is always the possibility of residual confounding due to unmeasured patient or clinic factors.
In summary, patients treated at clinics that have more experience in caring for PD patients, which may be reflected by having greater numbers of PD patients, may have better outcomes in terms of switching to hemodialysis and cardiovascular morbidity. PD clinic size may act as a proxy of not only greater PD experience but also more focus on the modality and more incentives to improve PD practices at the clinic.
Acknowledgments
We thank Beth Piraino, MD, for her expert advice in preparing this manuscript. We also thank the patients, staff, and medical directors of the participating clinics at DCI and New Haven CAPD who contributed to the study.
Grant support: This work was supported by grant no. RO1 DK 59616 from the National Institute of Diabetes and Digestive and Kidney Diseases, Bethesda, MD, grant no. R01-HS-08365 from the Agency for Health Care Research and Quality, Rockville, Maryland, and grant no. R01 HL 62985 from the National Heart Lung and Blood Institute, Bethesda, MD. Dr. Powe is supported by grant K24DK02643.
References
- (1).Mujais S, Story K. Peritoneal dialysis in the US: Evaluation of outcomes in contemporary cohorts. Kidney Int Suppl. 2006;103:S21–6. doi: 10.1038/sj.ki.5001912. [DOI] [PubMed] [Google Scholar]
- (2).Jaar BG, Coresh J, Plantinga LC, Fink NE, Klag MJ, Levey AS, et al. Comparing the risk for death with peritoneal dialysis and hemodialysis in a national cohort of patients with chronic kidney disease. Ann Intern Med. 2005;143:174–83. doi: 10.7326/0003-4819-143-3-200508020-00003. [DOI] [PubMed] [Google Scholar]
- (3).Huisman RM, Nieuwenhuizen MG, Th de Charro F. Patient-related and centre-related factors influencing technique survival of peritoneal dialysis in The Netherlands. Nephrol Dial Transplant. 2002;17:1655–60. doi: 10.1093/ndt/17.9.1655. [DOI] [PubMed] [Google Scholar]
- (4).Schaubel DE, Blake PG, Fenton SS. Effect of renal center characteristics on mortality and technique failure on peritoneal dialysis. Kidney Int. 2001;60:1517–24. doi: 10.1046/j.1523-1755.2001.00969.x. [DOI] [PubMed] [Google Scholar]
- (5).Powe NR, Klag MJ, Sadler JH, Anderson GF, Bass EB, Briggs WA, et al. Choices for healthy outcomes in caring for end stage renal disease. Semin Dial. 1996;9:9–11. [Google Scholar]
- (6).Plantinga LC, Fink NE, Sadler JH, Levey AS, Levin NW, Rubin HR, et al. Frequency of patient-physician contact and patient outcomes in hemodialysis care. J Am Soc Nephrol. 2004;15:210–8. doi: 10.1097/01.asn.0000106101.48237.9d. [DOI] [PubMed] [Google Scholar]
- (7).Plantinga LC, Fink NE, Jaar BG, Sadler JH, Coresh J, Klag MJ, et al. Frequency of sit-down patient care rounds, attainment of clinical performance targets, hospitalization, and mortality in hemodialysis patients. J Am Soc Nephrol. 2004;15:3144–53. doi: 10.1097/01.ASN.0000146424.91128.2A. [DOI] [PubMed] [Google Scholar]
- (8).Plantinga LC, Pham HH, Fink NE, Rubin HR, Jaar BG, Powe NR. Use of dialysis educators beyond nurses and physicians and outcomes in patients with kidney failure. Adv Chronic Kidney Dis. 2005;12:424–32. doi: 10.1053/j.ackd.2005.07.006. [DOI] [PubMed] [Google Scholar]
- (9).Athienites NV, Miskulin DC, Fernandez G, Bunnapradist S, Simon G, Landa M, et al. Comorbidity assessment in hemodialysis and peritoneal dialysis using the index of coexistent disease. Semin Dial. 2000;3:320–6. doi: 10.1046/j.1525-139x.2000.00095.x. [DOI] [PubMed] [Google Scholar]
- (10).Miskulin DC, Meyer KB, Athienites NV, Martin AA, Terrin N, Marsh JV, et al. Comorbidity and other factors associated with modality selection in incident dialysis patients: the CHOICE Study. Choices for Healthy Outcomes in Caring for End-Stage Renal Disease. Am J Kidney Dis. 2002;39:324–36. doi: 10.1053/ajkd.2002.30552. [DOI] [PubMed] [Google Scholar]
- (11).Kinchen KS, Sadler J, Fink N, Brookmeyer R, Klag MJ, Levey AS, et al. The timing of specialist evaluation in chronic kidney disease and mortality. Ann Intern Med. 2002;137:479–86. doi: 10.7326/0003-4819-137-6-200209170-00007. [DOI] [PubMed] [Google Scholar]
- (12).Yang X, Fang W, Bargman JM, Oreopoulos DG. High peritoneal permeability is not associated with higher mortality or technique failure in patients on automated peritoneal dialysis. Perit Dial Int. 2008;28:82–92. [PubMed] [Google Scholar]
- (13).Churchill DN, Thorpe KE, Vonesh EF, Keshaviah PR. Lower probability of patient survival with continuous peritoneal dialysis in the United States compared with Canada. Canada-USA (CANUSA) Peritoneal Dialysis Study Group. J Am Soc Nephrol. 1997;8:965–71. doi: 10.1681/ASN.V86965. [DOI] [PubMed] [Google Scholar]
- (14).Bernardini J, Price V, Figueiredo A. Peritoneal dialysis patient training, 2006. Perit Dial Int. 2006;26:625–32. [PubMed] [Google Scholar]