Abstract
Background: Proximal humeral migration is commonly seen in rotator-cuff-deficient shoulders. The specific effects of the size of the rotator cuff tear and of pain on glenohumeral kinematics have been poorly defined. The purpose of this study was to examine the influences of cuff tear size and pain, separately, on humeral migration in a series of patients with symptomatic and asymptomatic rotator cuff tears.
Methods: Ninety-eight asymptomatic and sixty-two symptomatic shoulders were identified from a cohort of patients with unilateral shoulder pain related to rotator cuff disease. All shoulders underwent ultrasonographic evaluation of the rotator cuff and standardized radiographic evaluation. Humeral migration was measured by three observers using software-enhanced radiographic analysis.
Results: There was no significant difference in rotator cuff tear size between the asymptomatic and symptomatic shoulders, although more tears involved the infraspinatus in the symptomatic group (p = 0.01). Proximal humeral migration was greater in the shoulders with a symptomatic tear than it was in those with an asymptomatic tear (p = 0.03). Tears that involved the infraspinatus resulted in more migration than did isolated supraspinatus tears in both the symptomatic (p = 0.01) and the asymptomatic shoulders (p = 0.03). When the symptomatic tears of ≥175 mm2 were analyzed separately, the size of the tear was found to correlate strongly with humeral migration (p = 0.01). However, when the symptomatic tears that were <175 mm2 were analyzed, neither tear size nor pain was found to have a significant relationship with migration. When the analysis was limited to full-thickness symptomatic tears of ≥175 mm2, both pain (p = 0.002) and tear area (p = 0.0002) were found to have a significant effect on migration. Multivariate analysis showed that tear size (p = 0.01) was the strongest predictor of migration in symptomatic shoulders.
Conclusions: Proximal humeral migration correlates with rotator cuff tear size. Tears extending into the infraspinatus tendon are associated with greater humeral migration than is seen with isolated supraspinatus tears. Humeral migration resulting from symptomatic rotator cuff tears is greater than that resulting from asymptomatic tears. Additionally, there is a critical size for tendon tears resulting in humeral migration in painful shoulders. Although both pain and tear size influence glenohumeral kinematics in symptomatic shoulders, only tear size is an independent predictor of humeral migration.
Level of Evidence: Prognostic Level II. See Instructions to Authors for a complete description of levels of evidence.
Proximal humeral migration has been observed both clinically and experimentally in rotator-cuff-deficient shoulders1-7. Proximal humeral migration is clinically important as it implies disruption of normal glenohumeral kinematics and is often a sign of advanced rotator cuff disease7-10. Characteristics of a rotator cuff tear such as a larger size and the presence of fatty changes within the muscle11-15, which have been linked to a poorer prognosis following surgical repair, have been associated with radiographic evidence of proximal humeral migration4,14. Despite the important clinical implications of a radiographic finding of proximal humeral migration, our understanding of the nature of this condition remains incomplete. Specifically, the separate effects of the size and location of the rotator cuff tendon tear and the influence of pain on proximal humeral migration have not been clearly defined.
Clinical studies to date have focused on proximal humeral migration in patients with a symptomatic rotator cuff tear2,4,8. In that population, it is likely that both pain and rotator cuff dysfunction contribute to abnormal glenohumeral kinematics. There is evidence that pain alone can affect normal glenohumeral kinematics in shoulders with a structurally intact rotator cuff16, but as far as we know the effect of pain on glenohumeral biomechanics has not been separated from the effect of rotator cuff tear size in cuff-deficient shoulders. Defining the relative contributions of pain and rotator cuff tear size on glenohumeral kinematics is fundamental to our understanding of the treatment of symptomatic rotator cuff tears. Alterations in glenohumeral kinematics may explain the transition of an asymptomatic rotator cuff tear to a symptomatic tear. Additionally, if pain is found to influence proximal humeral migration independent of rotator cuff tear size, more studies of the effect of pain-relieving modalities such as corticosteroid injections and physical therapy on glenohumeral kinematics would be warranted.
Little is known about humeral head migration in relation to asymptomatic rotator cuff tears. Consideration of proximal migration as it relates to a broader spectrum of rotator cuff tears, including both asymptomatic and symptomatic lesions, may provide further insight into the factors that contribute to this phenomenon. Comparison of glenohumeral kinematics between symptomatic and asymptomatic shoulders would allow more careful determination of the relative effects of pain and rotator cuff tear size on kinematics. By controlling for the effects of pain, the relationship of rotator cuff tear size and location with glenohumeral kinematics can be better defined.
The purpose of this study was to examine the influences of rotator cuff tear size and pain on proximal humeral migration in rotator-cuff-deficient shoulders. We hypothesized that (1) the degree of proximal humeral migration would correlate with the size of the rotator cuff tendon tear and (2) there would be more proximal humeral migration with symptomatic tears than with asymptomatic tears.
Materials and Methods
The records from an ongoing prospective, longitudinal study regarding asymptomatic rotator cuff tears were reviewed. Subjects who had undergone standardized radiographic and ultrasound examinations of both shoulders for the evaluation of unilateral shoulder pain were identified. The level of pain was reported on a visual analog scale ranging from 0 to 10 and was recorded as the average daily pain for each shoulder. Asymptomatic shoulders were defined as having a reported visual analog pain score of ≤3 and symptomatic shoulders, as a visual analog pain score of >3 for at least six weeks. This level of pain was used to distinguish between the groups because our clinical experience demonstrated that patients seeking medical evaluation for a painful shoulder generally report a visual analog pain score of ≥5. Additional criteria to define symptomatic tears included any of the following: a pain level considered greater than normally experienced as a part of daily living, pain that required the use of medications such as narcotics or nonsteroidal anti-inflammatory medications, and pain that prompted a visit to a physician.
To be included in the study, a patient had to (1) have undergone bilateral ultrasound and radiographic evaluations because of unilateral shoulder pain and (2) have available complete sonographic and clinical data for both shoulders, including the presence or absence of a rotator cuff tear and the morphology of the rotator cuff tear, and a recorded visual analog pain score at the time of examination. The exclusion criteria were (1) bilateral shoulder symptoms, (2) previous surgery on either shoulder, (3) inflammatory arthropathy, (4) glenohumeral osteoarthritis, (5) previous shoulder trauma, (6) non-standardized radiographs, and (7) a full-thickness tear of the subscapularis tendon on ultrasound examination.
Our institutional review board approved the review of the medical records. One hundred and seventeen patients (234 eligible shoulders) met the inclusion criteria. Forty-four shoulders were excluded because of non-standardized radiographic analysis. At the initiation of the prospective longitudinal study of asymptomatic rotator cuff disease, the study protocol dictated that radiographs be made for only the asymptomatic shoulder, and not the symptomatic shoulder. Later the protocol was changed to include standardized radiographs of the symptomatic side as well. Ten shoulders were excluded because of poor anatomic detail of the radiographs (a failure to adequately define the glenoid margins); four, because of previous surgery; six, because of radiographic evidence of osteoarthritis; and two, because they had a full-thickness subscapularis tear. Eight asymptomatic shoulders were not included in the analysis as the radiographs of these shoulders were made after the study time period. Complete imaging and clinical data were available for ninety-eight asymptomatic and sixty-two symptomatic shoulders of the eligible 117 subjects. All study data, including the results of the shoulder ultrasonography and radiographs, were collected prior to the initiation of treatment of the painful shoulder.
Ultrasonography
The ultrasonographic examinations were performed by one of two musculoskeletal radiologists with extensive experience in the use of high-resolution ultrasonography for evaluation of pathological conditions of the shoulder. Ultrasonography has been validated at our institution as an accurate means with which to evaluate the rotator cuff17-19. All study subjects underwent standardized bilateral shoulder examinations as previously described17. The ultrasound examinations were performed in real time with the use of a Siemens scanner (Munich, Germany) and a variable high-frequency linear array transducer (5 to 10 MHz). Views included sagittal and coronal images of the rotator cuff muscles and tendons facilitated by positioning of the shoulder. The dimensions, location, and amount of retraction of the rotator cuff tendon tear were carefully quantified in millimeters. Tear width describes the anterior-to-posterior dimension and tear length, the medial-to-lateral dimension. The tear area was calculated by multiplying the tear width by the tear length.
Radiographic Analysis
Three radiology technicians were specifically selected and trained to standardize the quality of the radiographs. According to the study protocol, bilateral modified scapular plane anteroposterior radiographs were made for all patients. The radiographs were made with the shoulder in neutral rotation and 30° of active scapular plane elevation to elicit muscular activity within the rotator cuff and the deltoid. An angled grid was placed behind the subjects to precisely control the elevation angle of the shoulder. In addition, the arm was held in neutral rotation (the forearm parallel to the floor) and the humerus was horizontally adducted from the coronal plane approximately 30° to an angle in line with the body of the scapula. The distances between the shoulder and the cassette and between the shoulder and the x-ray beam were kept constant to avoid magnification errors. A premeasured, radiopaque marker was placed on all cassettes to further standardize magnification.
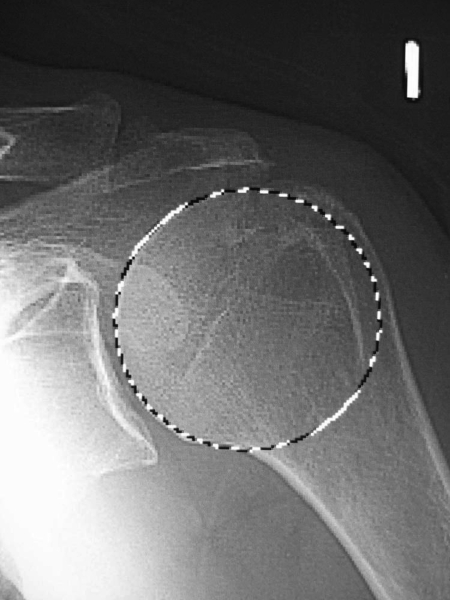
Three independent observers blinded to the clinical and ultrasound data measured proximal humeral migration on all radiographs with a software-enhanced modification of the technique described by Poppen and Walker20, and the mean of these measurements was used for analysis. Scion Image software (Scion, Frederick, Maryland) was used to measure proximal humeral migration in reference to the glenoid with use of a previously described technique7. The geometric center of the humeral head was found with a “best-fit” circle positioned over the humeral articular surface (Fig. 1-A). The superior and inferior rims of the glenoid articular surface were then marked and connected to determine the glenoid line (Fig. 1-B). The glenoid center was calculated from this demarcated line with use of the software. The length of the radiopaque marker on the radiograph was measured and was compared with the known length of the marker to control for subtle variations in magnification. The software then determined proximal humeral migration by calculating the position of the humeral head center in relation to the glenoid center. The measurements made by each of the observers were analyzed to determine interobserver reliability.
Fig. 1-A.
The geometric center of the humeral head was found with a “best-fit” circle positioned over the humeral articular surface.
Fig. 1-B.
To determine the geometric center of the glenoid, the superior and inferior rims of the glenoid articular surface were marked and connected to determine the glenoid line. The glenoid center was then calculated from this demarcated line with use of computer software.
Statistical Analysis
Unpaired t tests were used for between-group comparisons of continuous measures with a normal distribution. When data distributions were non-normal, unpaired t tests were performed on log-transformed data. Chi-square tests were used for between-group comparisons of categorical variables except when sample sizes were small and the Fisher exact test was used instead. Pearson correlations (r) and scatterplots were used to assess the bivariate association between continuous measures. Multivariate linear regression analysis was performed to examine the influence of pain on the association between tear size and migration, with pain and tear size used as the independent variables and migration used as the dependent variable. An alpha level of 0.05 was chosen to represent significance.
When we analyzed the transformed data for symptomatic shoulders we observed an inflection point in the distribution of the data. The association between the tear size and proximal humeral migration changed at this inflection point. Thus, the association between tear size and migration on the symptomatic side is expressed separately for cases above and below this threshold. Intraclass correlation coefficients with associated 95% confidence intervals were used to assess interrater reliability of the proximal migration measurements.
Source of Funding
The funding source used for this study was an R01 grant (AR051026-01A1) from the National Institutes of Health.
Results
Ultrasound examination showed that, of the ninety-eight asymptomatic shoulders, twenty-four had an intact rotator cuff, twenty-nine had a partial-thickness rotator cuff tear, and forty-five had a full-thickness tear. Of the sixty-two symptomatic shoulders, three were noted on ultrasound to have an intact rotator cuff, nine had a partial-thickness rotator cuff tear, and fifty had a full-thickness tear (Table I). The average age was 61.7 years for the patients in whom the asymptomatic shoulder had no rotator cuff tear and 61.2 years for those in whom it had a rotator cuff tear. The average age of the patients in whom the symptomatic shoulder had a rotator cuff tear was 60.6 years.
TABLE I.
Summary of Variables According to Side (Symptomatic or Asymptomatic) and Tear Category (N = 160)
| Asymptomatic Side (N = 98)
|
Symptomatic Side (N = 62)
|
|||||
|---|---|---|---|---|---|---|
| Variable | No Tear (N = 24) | Partial-Thickness Tear (N = 29) | Full-Thickness Tear (N = 45) | No Tear (N = 3) | Partial-Thickness Tear (N = 9) | Full-Thickness Tear (N = 50) |
| Age*(yr) | 61.7 ± 8.6 | 58.6 ± 10 | 62.9 ± 9.4 | 55.3 ± 4.6 | 58.4 ± 8.6 | 61.0 ± 9.3 |
| Sex† | ||||||
| Male | 13 (54%) | 14 (48%) | 27 (60%) | 0 | 4 (44%) | 28 (56%) |
| Female | 11 (46%) | 15 (52%) | 18 (40%) | 3 (100%) | 5 (56%) | 22 (44%) |
| Migration*(mm) | −0.68 ± 1.3 | −0.30 ± 1.1 | −0.27 ± 1.4 | −0.85 ± 0.05 | 0.22 ± 1.3 | 0.27 ± 1.6 |
| Tear length*(mm) | Not applic. | 6.96 ± 2.5 | 15.2 ± 10 | Not applic. | 6.28 ± 2.1 | 16.5 ± 13 |
| Tear width*(mm) | Not applic. | 9.34 ± 3.2 | 13.1 ± 8.1 | Not applic. | 9.78 ± 4.2 | 14.7 ± 10 |
| Tear area*‡(mm2) | Not applic. | 68.3 ± 38 | 267 ± 370 | Not applic. | 64.0 ± 43 | 354 ± 534 |
| Tear location†§ | Not applic. | Not applic. | ||||
| Infraspinatus | 1 (3%) | 0 | 1 (11%) | 1 (2%) | ||
| Supraspinatus | 26 (90%) | 37 (84%) | 6 (67%) | 34 (68%) | ||
| Supraspinatus and infraspinatus | 2 (7%) | 7 (16%) | 2 (22%) | 15 (30%) | ||
| Tear location category†§ | Not applic. | Not applic. | ||||
| Infraspinatus, or supraspinatus and infraspinatus | 3 (10%) | 7 (16%) | 3 (33%) | 16 (32%) | ||
| Supraspinatus | 26 (90%) | 37 (84%) | 6 (67%) | 34 (68%) | ||
| Visual analog pain score* | Not applic. | Not applic. | Not applic. | 6.33 ± 2.1 | 4.33 ± 1.7 | 4.80 ± 2.0 |
| Pain† | Not applic. | Not applic. | Not applic. | |||
| No | 0 | 5 (56%) | 16 (32%) | |||
| Yes | 3 (100%) | 4 (44%) | 34 (68%) | |||
The values are given as the mean and standard deviation.
The values are given as the number of shoulders with the percentage in parentheses.
The area is defined as the length multiplied by the width.
One full-thickness tear was excluded because of a lack of tear location data.
The mean visual analog pain scores (and standard deviation) associated with the symptomatic partial and full-thickness tears were 4.33 ± 1.7 and 4.80 ± 2.0, respectively. The difference in the visual analog scores between these groups was not significant (p = 0.52).
Ultrasound Findings
The average area of the partial-thickness tears was 68.3 ± 38 mm2 in the asymptomatic shoulders and 64.0 ± 43 mm2 in the symptomatic shoulders. The average areas of the full-thickness tears were 267 ± 370 mm2 and 354 ± 534 mm2 in the asymptomatic and symptomatic shoulders, respectively (Table I). No significant differences in length (p = 0.19), width (p = 0.15), or area (p = 0.15) were observed between the asymptomatic and symptomatic rotator cuff tears (Table II).
TABLE II.
Comparison of Variables Between Asymptomatic and Symptomatic Sides (N = 160)
| Variable | Asymptomatic Side (N = 98) | Symptomatic Side (N = 62) | P Value* |
|---|---|---|---|
| Migration for all shoulders in group†(mm) | −0.38 ± 1.3 | 0.21 ± 1.6 | 0.01‡ |
| Non-controls§ | |||
| Migration†(mm) | −0.28 ± 1.3 | 0.26 ± 1.6 | 0.03‡ |
| Tear length†(mm) | 12.0 ± 9.0 | 14.9 ± 13 | 0.19# |
| Tear width†(mm) | 11.6 ± 6.8 | 14.0 ± 9.6 | 0.15# |
| Tear area†(mm2) | 189 ± 304 | 310 ± 502 | 0.15# |
| Tear location category** | |||
| Infraspinatus, or supraspinatus and infraspinatus | 10 (14%) | 19 (32%) | 0.01‡ |
| Supraspinatus | 63 (86%) | 40 (68%) |
The p values were derived, with an unpaired t test or chi-square test, in a comparison of the asymptomatic and symptomatic sides.
The values are given as the mean and standard deviation.
The p value indicates significance (p < 0.05).
Non-controls indicate shoulders in which a rotator cuff tear was demonstrated by ultrasound.
The p value was derived with an unpaired t test with use of log-transformed data.
The values are given as the number of shoulders with the percentage in parentheses.
Sixty-three (86%) of the seventy-three asymptomatic tears were limited to the supraspinatus and ten (14%) included both the supraspinatus and the infraspinatus or the infraspinatus alone. Forty (68%) of the fifty-nine symptomatic tears involved only the supraspinatus and nineteen (32%) involved both the supraspinatus and the infraspinatus or the infraspinatus alone (Table II). This represented a significant difference in tear location between the two groups (p = 0.01).
Proximal Humeral Migration
Intraclass correlation coefficients were calculated for the analysis of proximal humeral migration by the three observers on the radiographs of 160 shoulders. The pooled correlation value was 0.81 with a 95% confidence interval of 0.76 to 0.85, indicating substantial interobserver agreement.
Proximal humeral migration in the asymptomatic shoulders with no evidence of a rotator cuff tear averaged −0.68 ± 1.3 mm (Table I). The mean migration in the shoulders with a symptomatic rotator cuff tear (0.26 ± 1.6 mm), both partial and full-thickness, was significantly greater (p = 0.03) than the mean migration in the shoulders with an asymptomatic rotator cuff tear (−0.28 ± 1.3 mm) (Table II).
Shoulders with an Asymptomatic Rotator Cuff Tear
In the asymptomatic group, the proximal humeral migration was significantly greater (p = 0.03) when the tear involved both the supraspinatus and the infraspinatus (or the infraspinatus alone) (0.50 ± 1.0 mm) than it was when the tear was limited to the supraspinatus (−0.44 ± 1.3 mm) (Table III). There was a direct, positive correlation between proximal migration and tear width (r = 0.21, p = 0.07), length (r = 0.24, p = 0.04), and area (r = 0.22, p = 0.06), but only the correlation with tear length reached significance.
TABLE III.
Migration Values According to Tear Location and Presence of Pain (N = 160)
| Migration
|
||||||
|---|---|---|---|---|---|---|
| Asymptomatic Side (N = 98)
|
Symptomatic Side (N = 62)
|
|||||
| Patient Category | No. of Shoulders | Mean and Stand. Dev. (mm) | P Value* | No. of Shoulders | Mean and Stand. Dev. (mm) | P Value* |
| Tear location category (non-controls†) | ||||||
| Infraspinatus, or supraspinatus and infraspinatus | 10 | 0.50 ± 1.0 | 0.03‡ | 19 | 1.01 ± 1.5 | 0.01‡ |
| Supraspinatus | 63 | −0.44 ± 1.3 | 40 | −0.09 ± 1.5 | ||
| Pain | Not applic. | 0.80 | ||||
| No | 21 | 0.14 ± 1.31 | ||||
| Yes | 41 | 0.25 ± 1.67 | ||||
The p values were derived, with an unpaired t test, in a comparison of the patient categories within the asymptomatic or symptomatic group.
Non-controls indicate shoulders in which a rotator cuff tear was demonstrated by ultrasound.
The p value indicates significance (p < 0.05).
Shoulders with a Symptomatic Rotator Cuff Tear
Proximal humeral migration in association with symptomatic tears involving both the supraspinatus and the infraspinatus tendons (or the infraspinatus alone) (1.01 ± 1.5 mm) was significantly greater (p = 0.01) than that associated with symptomatic tears limited to the supraspinatus alone (−0.09 ± 1.5 mm) (Table III).
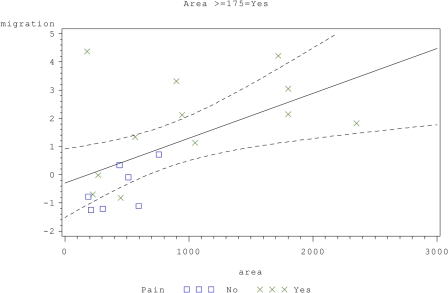
Analyses of the characteristics of the symptomatic tears, including length, width, and area, identified a tear-area threshold of 175 mm2 that directly influenced proximal humeral migration. We found a significant positive correlation between symptomatic tears with an area of ≥175 mm2 and humeral migration (r = 0.57, p = 0.01) (Fig. 2). Likewise, the analysis of the larger tears showed a positive correlation between both tear length (r = 0.57, p = 0.01) and width (r = 0.50, p = 0.03) and proximal humeral migration. The analysis of the smaller tears (those with an area of <175 mm2) did not demonstrate a significant correlation between the tear characteristics and humeral migration. Humeral migration in association with tears of ≥175 mm2 (0.98 ± 1.8 mm) was significantly greater (p = 0.01) than that associated with tears of <175 mm2 (−0.08 ± 1.3 mm) (Table IV). No significant difference in the visual analog pain score was observed between the tears of ≥175 mm2 (visual analog score, 4.42) and those of <175 mm2 (visual analog score, 4.88) (p = 0.42).
Fig. 2.
Linear regression line (and 95% confidence interval) for the association of migration (in millimeters) and tear area (in square millimeters) in symptomatic shoulders with a tear with an area of ≥175 mm2.
TABLE IV.
Variables According to Tear-Size Group on the Symptomatic Side
| Variable | Tear Area <175 mm2* (N = 40) | Tear Area ≥175 mm2* (N = 19) | P Value† |
|---|---|---|---|
| Migration (mm) | −0.08 ± 1.3 | 0.98 ± 1.8 | 0.01‡ |
| Tear length (mm) | 8.14 ± 3.1 | 29.2 ± 13 | <0.0001‡§ |
| Tear width (mm) | 9.08 ± 3.2 | 24.3 ± 11 | <0.0001‡§ |
| Tear area (mm2) | 76 ± 40 | 804 ± 656 | <0.0001‡§ |
| Visual analog pain score | 4.88 ± 1.9 | 4.42 ± 2.3 | 0.42 |
The values are given as the mean and standard deviation.
The p values were derived, with an unpaired t test, in a comparison of the tear-size groups.
The p value indicates significance (p < 0.05).
The p value was derived with an unpaired t test with use of log-transformed data.
Analysis of forty-nine symptomatic full-thickness cuff tears showed that, in the group with an area of <175 mm2, there was no significant correlation between pain and migration (r = −0.27, p = 0.14) or between pain and the tear area (r = 0.07, p = 0.71). Pain, however, was an important variable in the group of tears with an area of ≥175 mm2, with a significant correlation between the visual analog pain score and migration (r = 0.68, p = 0.002) and a significant correlation between pain and the tear area (r = 0.70, p = 0.001) (Table V). However, multivariate analysis with both pain and tear area considered to be independent variables (overall model r2 = 0.63, p = 0.0006) showed the tear area to be the single most important predictor of humeral migration (r2 = 0.63, p = 0.01). While pain was found to be an important factor in the univariate analysis, it did not appear to contribute unique information to the prediction of proximal humeral migration beyond the information contributed by the tear area (p = 0.24).
TABLE V.
Correlations (r) Between Variables for Full-Thickness Tears with an Area of <175 mm2 or ≥175 mm2 on the Symptomatic Side
| Tear Area <175 mm2 (N = 31)
|
Tear Area ≥175 mm2 (N = 18)
|
|||
|---|---|---|---|---|
| R Value | P Value | R Value | P Value | |
| Correlation with migration | ||||
| Tear length | −0.37 | 0.04* | 0.84 | <0.0001* |
| Tear width | −0.25 | 0.18 | 0.68 | 0.002* |
| Tear area | −0.42 | 0.02* | 0.77 | 0.0002* |
| Visual analog pain score | −0.27 | 0.14 | 0.68 | 0.002* |
| Correlation with visual analog pain score | ||||
| Tear length | 0.10 | 0.60 | 0.67 | 0.002* |
| Tear width | 0.10 | 0.61 | 0.61 | 0.01* |
| Tear area | 0.07 | 0.71 | 0.70 | 0.001* |
The p value indicates significance (p < 0.05).
Discussion
Proximal humeral migration is commonly observed in association with advanced rotator cuff disease2-4,6,8-10. Experimental, biomechanical studies of rotator-cuff-deficient shoulders have demonstrated altered glenohumeral mechanics that are dependent on the size of the cuff defect5,21,22. Clinical factors associated with the severity of proximal humeral migration include the presence of multiple torn rotator cuff tendons and fatty changes in the infraspinatus and subscapularis muscles2-4,8. Prior clinical studies have primarily focused on proximal humeral migration in painful cuff-deficient shoulders2,4,8. However, pain alone may have a significant effect on glenohumeral kinematics, as has been noted in certain patients with a painful impingement syndrome and an intact rotator cuff16.
The unique design of this study allowed us to examine proximal humeral migration in both symptomatic and asymptomatic cuff-deficient shoulders in a carefully controlled manner. By studying both asymptomatic and symptomatic shoulders, we were able to examine independently the effects of pain and the size of the rotator cuff tear on glenohumeral mechanics. The clinical implications of proximal humeral migration are important in that it indicates a tear of sufficient size to alter glenohumeral mechanics. Migration may be responsible, in part, for the development of pain and degenerative changes in the rotator-cuff-deficient shoulder. In addition, migration can be linked to several risk factors indicative of a poorer prognosis following rotator cuff repair, including a large tear size and advanced muscular atrophy and fatty infiltration11-15.
High-resolution ultrasonography of the shoulder provides accurate quantification of tear parameters (width and length), allowing a direct analysis of the effect of tear size on glenohumeral kinematics. More importantly, ultrasonography has been validated for accuracy in the evaluation of rotator cuff disease in our institution. In agreement with the observations of previous studies2-4,8,21, we found proximal humeral migration to be directly correlated with rotator cuff tear size and location. In both the asymptomatic and the symptomatic group, tears involving both the supraspinatus and the infraspinatus tendon (or the infraspinatus alone) were found to be associated with greater migration than were smaller, isolated supraspinatus tears. We identified a threshold for migration based on tear area in the symptomatic shoulders. Tears with an area of ≥175 mm2 resulted in greater migration than did smaller tears, and we found significant correlations between migration and all of the parameters (length, width, and area) of these larger-area tears. We found no significant relationship between proximal humeral migration and the parameters of the symptomatic tears with an area of <175 mm2. A tear with an area of 175 mm2 represents a full-thickness disruption of the supraspinatus tendon with slight retraction (1 cm). We hypothesize that tears larger than this threshold, with extension into the infraspinatus, begin to disrupt the normal humeral head-centering function of the rotator cuff, allowing proximal humeral migration. Burkhart et al. described the presence of the rotator cuff cable connecting the supraspinatus tendon to the infraspinatus tendon, theorizing the potential for this structure to compensate biomechanically for a torn supraspinatus tendon23. Rotator cuff tears that extend into the infraspinatus tendon may be too large to allow compensatory contraction through the rotator cuff cable, resulting in proximal humeral migration. We believe that the results of our study further demonstrate the importance of the infraspinatus tendon in maintaining normal glenohumeral kinematics.
One of us (K.Y.) and colleagues demonstrated increased proximal humeral migration, as compared with that in controls, both in shoulders with an asymptomatic rotator cuff tear and in those with a symptomatic tear7. In that study, detailed analysis of the effect of rotator cuff tear size on glenohumeral kinematics was limited by a lack of information regarding rotator cuff tear size and morphology in asymptomatic shoulders. In our study, we were able to accurately quantify the size and location of the rotator cuff tear in all subjects. There was significantly less proximal migration in the asymptomatic tear group than there was in the symptomatic tear group. Further analysis showed proximal migration to be significantly correlated with tear length (retraction) but not with tear width or area in asymptomatic shoulders. In addition, no tear-size threshold for migration was evident in the asymptomatic group. There are several possible explanations for these differences between the asymptomatic and symptomatic groups. Pain may influence the glenohumeral kinematics in symptomatic shoulders. Additionally, although there was no significant difference in tear size between the two groups, the area of the symptomatic tears was slightly greater than that of the asymptomatic tears and a significantly greater percentage of tears extended into the infraspinatus tendon in the symptomatic shoulders. Prior studies have highlighted the importance of the infraspinatus in maintaining normal kinematics of the shoulder during elevation21,22.
From our data, it appears that pain may play a role in proximal humeral migration in cuff-deficient shoulders, especially when the tear involves more than one tendon. The role of pain in proximal migration has not been explored previously, to our knowledge. A recent electromyographic study24 demonstrated that patients with a symptomatic tear involving the supraspinatus and infraspinatus had a dysfunctional firing pattern characterized by increased activation of torn muscles and a failure to recruit the subscapularis as compared with the findings in patients with an asymptomatic tear. These observations suggest that pain alone can lead to dysfunctional shoulder mechanics and possibly affect proximal migration.
In the present study, the influence of pain in the symptomatic shoulders was most evident with tears above the size threshold of 175 mm2, with pain having a significant positive correlation with both migration and all tear-size parameters, including width, length, and area, in that group. This indicates that, in the case of larger tears, increased pain was strongly associated with both greater proximal migration and increased tear size. Multivariate analysis, however, subsequently demonstrated that tear area was the strongest predictor of proximal migration.
We believe that the information gained from this study has direct clinical application. We identified a critical threshold of tear size in painful rotator-cuff-deficient shoulders at which changes in glenohumeral kinematics become more pronounced. Painful rotator cuff tears with extension into the infraspinatus consistently disrupted glenohumeral kinematics, whereas smaller tears demonstrated less consistent relationships with altered mechanics. We believe that early surgery should be considered for these larger tears, with the primary goal of reestablishment of the contribution of the infraspinatus to the rotator cuff force couple. Additionally, pain is an important factor that must be considered when evaluating tears of all sizes. Pain may explain the presence of proximal humeral migration in shoulders with an isolated supraspinatus tear and an otherwise intact rotator cuff force couple (infraspinatus and teres minor posteriorly and subscapularis anteriorly). Finally, findings from this study may support the use of rehabilitation for patients in whom a painful rotator cuff tear is managed nonoperatively. Strengthening of the remaining, intact muscles may decrease pain, possibly by improving glenohumeral kinematics. Future studies are warranted to determine the effect of various pain-relieving modalities such as corticosteroid injections and rehabilitation on glenohumeral kinematics. To further define the role of proximal humeral migration in the development of shoulder pain, a longitudinal cohort study of patients with asymptomatic rotator cuff tears followed until the onset of symptoms may be necessary.
Rather than measuring the acromiohumeral interval to determine proximal humeral migration, we used a modification of a technique established by Poppen and Walker20. With this technique, humeral migration is determined by establishing the relationship of the geometric center of the humeral head to the center of the glenoid subchondral articular surface. This has been a reliable and reproducible method in our experience7. However, although our technique is accurate and reliable for determining subchondral anatomy, we did not directly measure articular cartilage surfaces. It is possible that some error could have been introduced by our failure to directly reference the articular surface landmarks. However, because the measurement method was consistent in all groups, the potential for these errors should have been minimized and there should not have been directional bias. In contrast, when the acromiohumeral interval is measured, factors such as the radiographic projection angle, scapular position, humeral head rotation, and acromial morphology can make the identification of consistent anatomic landmarks and quantification of migration unreliable. The method of calculating proximal humeral migration in this study highlighted the often subtle presence of migration in association with rotator cuff lesions. The mean difference in the humeral head position between asymptomatic shoulders with no rotator cuff tear and symptomatic shoulders was approximately 1 mm. Despite this small mean difference, large shifts in migration were commonly noted with larger rotator cuff tears. The small differences in migration between these groups require a very sensitive method of quantification. The subtle effects of small rotator cuff tears on proximal humeral migration would be difficult to detect in the clinical setting alone or with measurements of the acromiohumeral interval.
Our study had several limitations that must be recognized. Incomplete or inadequate radiographic analysis led to exclusion of a number of shoulders from the study group. We chose to include only subjects with well-controlled radiographs in the migration analysis. In addition, we excluded tears that involved the subscapularis because the number of these tears noted with ultrasonography was too small to allow meaningful analysis. Although shoulder ultrasonography has been validated at our institution as an accurate means for the detection and quantification of rotator cuff disease, it is possible that diagnostic errors occurred. The reported accuracy of shoulder ultrasonography for the identification of partial and full-thickness rotator cuff tears has ranged between 87% and 96% at our institution17,18. We also found shoulder ultrasonography to be as accurate as conventional magnetic resonance imaging at our institution.
We conclude that, even when pain is controlled for, proximal humeral migration correlates most strongly with the size of a rotator cuff tear. Symptomatic cuff tears are also associated with greater proximal humeral migration than are asymptomatic tears. Tears that extend into the infraspinatus tendon are associated with greater proximal humeral migration than are tears isolated to the supraspinatus tendon. We identified a critical size of rotator cuff tendon tears that can result in proximal humeral migration in symptomatic shoulders. When a symptomatic full-thickness tear is ≥175 mm2, both the size of the tear and the degree of pain influence proximal humeral migration. However, the size of the rotator cuff tear appears to have a greater influence on proximal humeral migration than does pain in symptomatic shoulders. 
Disclosure: In support of their research for or preparation of this work, one or more of the authors received, in any one year, outside funding or grants in excess of $10,000 from the National Institutes of Health. Neither they nor a member of their immediate families received payments or other benefits or a commitment or agreement to provide such benefits from a commercial entity. No commercial entity paid or directed, or agreed to pay or direct, any benefits to any research fund, foundation, division, center, clinical practice, or other charitable or nonprofit organization with which the authors, or a member of their immediate families, are affiliated or associated.
Investigation performed at the Department of Orthopaedic Surgery and the Division of Biostatistics, Washington University, St. Louis, Missouri
References
- 1.Halder AM, Zhao KD, Odriscoll SW, Morrey BF, An KN. Dynamic contributions to superior shoulder stability. J Orthop Res. 2001;19:206-12. [DOI] [PubMed] [Google Scholar]
- 2.Nové-Josserand L, Edwards TB, O'Connor DP, Walch G. The acromiohumeral and coracohumeral intervals are abnormal in rotator cuff tears with muscular fatty degeneration. Clin Orthop Relat Res. 2005;433:90-6. [DOI] [PubMed] [Google Scholar]
- 3.Nové-Josserand L, Lévigne C, Noël E, Walch G. [The acromio-humeral interval. A study of the factors influencing its height]. Rev Chir Orthop Reparatrice Appar Mot. 1996;82:379-85. French. [PubMed] [Google Scholar]
- 4.Saupe N, Pfirrmann CW, Schmid MR, Jost B, Werner CM, Zanetti M. Association between rotator cuff abnormalities and reduced acromiohumeral distance. AJR Am J Roentgenol. 2006;187:376-82. [DOI] [PubMed] [Google Scholar]
- 5.Sharkey NA, Marder RA. The rotator cuff opposes superior translation of the humeral head. Am J Sports Med. 1995;23:270-5. [DOI] [PubMed] [Google Scholar]
- 6.Weiner DS, Macnab I. Superior migration of the humeral head. A radiological aid in the diagnosis of tears of the rotator cuff. J Bone Joint Surg Br. 1970;52:524-7. [PubMed] [Google Scholar]
- 7.Yamaguchi K, Sher JS, Andersen WK, Garretson R, Uribe JW, Hechtman K, Neviaser RJ. Glenohumeral motion in patients with rotator cuff tears: a comparison of asymptomatic and symptomatic shoulders. J Shoulder Elbow Surg. 2000;9:6-11. [DOI] [PubMed] [Google Scholar]
- 8.Bezer M, Yildirim Y, Akgün U, Erol B, Güven O. Superior excursion of the humeral head: a diagnostic tool in rotator cuff tear surgery. J Shoulder Elbow Surg. 2005;14:375-9. [DOI] [PubMed] [Google Scholar]
- 9.Burkhart SS. Fluoroscopic comparison of kinematic patterns in massive rotator cuff tears. A suspension bridge model. Clin Orthop Relat Res. 1992;284:144-52. [PubMed] [Google Scholar]
- 10.Norwood LA, Barrack R, Jacobson KE. Clinical presentation of complete tears of the rotator cuff. J Bone Joint Surg Am. 1989;71:499-505. [PubMed] [Google Scholar]
- 11.Ellman H, Hanker G, Bayer M. Repair of the rotator cuff. End-result study of factors influencing reconstruction. J Bone Joint Surg Am. 1986;68:1136-44. [PubMed] [Google Scholar]
- 12.Gerber C, Schneeberger AG, Hoppeler H, Meyer DC. Correlation of atrophy and fatty infiltration on strength and integrity of rotator cuff repairs: a study in thirteen patients. J Shoulder Elbow Surg. 2007;16:691-6. [DOI] [PubMed] [Google Scholar]
- 13.Gladstone JN, Bishop JY, Lo IK, Flatow EL. Fatty infiltration and atrophy of the rotator cuff do not improve after rotator cuff repair and correlate with poor functional outcome. Am J Sports Med. 2007;35:719-28. [DOI] [PubMed] [Google Scholar]
- 14.Vad VB, Warren RF, Altchek DW, O'Brien SJ, Rose HA, Wickiewicz TL. Negative prognostic factors in managing massive rotator cuff tears. Clin J Sport Med. 2002;12:151-7. [DOI] [PubMed] [Google Scholar]
- 15.Walch G, Marechal E, Maupas J, Liotard JP. [Surgical treatment of rotator cuff rupture. Prognostic factors]. Rev Chir Orthop Reparatrice Appar Mot. 1992;78:379-88. French. [PubMed] [Google Scholar]
- 16.Deutsch A, Altchek DW, Schwartz E, Otis JC, Warren RF. Radiologic measurement of superior displacement of the humeral head in the impingement syndrome. J Shoulder Elbow Surg. 1996;5:186-93. [DOI] [PubMed] [Google Scholar]
- 17.Teefey SA, Hasan SA, Middleton WD, Patel M, Wright RW, Yamaguchi K. Ultrasonography of the rotator cuff. A comparison of ultrasonographic and arthroscopic findings in one hundred consecutive cases. J Bone Joint Surg Am. 2000;82:498-504. [PubMed] [Google Scholar]
- 18.Teefey SA, Rubin DA, Middleton WD, Hildebolt CF, Leibold RA, Yamaguchi K. Detection and quantification of rotator cuff tears. Comparison of ultrasonographic, magnetic resonance imaging, and arthroscopic findings in seventy-one consecutive cases. J Bone Joint Surg Am. 2004;86:708-16. [PubMed] [Google Scholar]
- 19.Prickett WD, Teefey SA, Galatz LM, Calfee RP, Middleton WD, Yamaguchi K. Accuracy of ultrasound imaging of the rotator cuff in shoulders that are painful postoperatively. J Bone Joint Surg Am. 2003;85:1084-9. [DOI] [PubMed] [Google Scholar]
- 20.Poppen NK, Walker PS. Normal and abnormal motion of the shoulder. J Bone Joint Surg Am. 1976;58:195-201. [PubMed] [Google Scholar]
- 21.Mura N, O'Driscoll SW, Zobitz ME, Heers G, Jenkyn TR, Chou SM, Halder AM, An KN. The effect of infraspinatus disruption on glenohumeral torque and superior migration of the humeral head: a biomechanical study. J Shoulder Elbow Surg. 2003;12:179-84. [DOI] [PubMed] [Google Scholar]
- 22.Thompson WO, Debski RE, Boardman ND 3rd, Taskiran E, Warner JJ, Fu FH, Woo SL. A biomechanical analysis of rotator cuff deficiency in a cadaveric model. Am J Sports Med. 1996;24:286-92. [DOI] [PubMed] [Google Scholar]
- 23.Burkhart SS, Esch JC, Jolson RS. The rotator crescent and rotator cable: an anatomic description of the shoulder's “suspension bridge”. Arthroscopy. 1993;9:611-6. Erratum in: Arthroscopy. 1994;10:239. [DOI] [PubMed] [Google Scholar]
- 24.Kelly BT, Williams RJ, Cordasco FA, Backus SI, Otis JC, Weiland DE, Altchek DW, Craig EV, Wickiewicz TL, Warren RF. Differential patterns of muscle activation in patients with symptomatic and asymptomatic rotator cuff tears. J Shoulder Elbow Surg. 2005;14:165-71. [DOI] [PubMed] [Google Scholar]