Abstract
Objective
To examine associations between exposure to physical violence (PV) or sexual violence (SV) and adverse health behaviours among a sample of children in five African countries.
Methods
In a cross-sectional analysis of data from Namibia, Swaziland, Uganda, Zambia and Zimbabwe – countries that participated in the Global School-based Student Health Survey in 2003 or 2004 – we compared the relative frequency of several adverse health behaviours among children (primarily students 13–15 years of age) who did and who did not report exposure to PV or SV. We estimated odds ratios (ORs) for such behaviours and their 95% confidence intervals (CIs) after adjusting for age and sex.
Findings
Exposure to PV during the 12 months preceding the survey was reported by 27–50% (average: 42%) of the children studied in the five countries, and lifetime exposure to SV was reported by 9–33% (average: 23%). Moderate to strong associations were observed between exposure to PV or SV and measures of mental health, suicidal ideation, current cigarette use, current alcohol use, lifetime drug use, multiple sex partners and a history of sexually transmitted infection (P ≤ 0.05 for all associations). For example, the odds of being a current cigarette smoker were higher in children involved in one fight (OR: 2.20; 95% CI: 1.77–2.75), 2–5 fights (OR: 3.43; 95% CI: 2.54–4.63), or 6 fights or more (OR: 5.95; 95% CI: 4.37–8.11) (P for trend < 0.001) during the 12 months preceding the survey than in children unexposed to PV.
Conclusion
Childhood exposure to PV and SV is common among African children in some countries and is associated with multiple adverse health behaviours. In developing countries, increased awareness of the frequency of exposure to violence among children and its potential health consequences may lead to heightened attention to the need for health promotion and preventive programmes that address the problem.
Résumé
Objectif
Examiner les associations entre exposition à des violences physiques (VP) ou à des violences sexuelles (VS) et comportements préjudiciables à la santé parmi un échantillon d’enfants de cinq pays africains.
Méthodes
Dans le cadre d’une analyse transversale des données provenant de Namibie, du Swaziland, d’Ouganda, de Zambie et du Zimbabwe - pays ayant participé à l’Enquête mondiale sur les comportements de santé des enfants d’âge scolaire en 2003 et 2004 - , nous avons comparé les fréquences de plusieurs comportements préjudiciables à la santé chez les enfants (principalement les enfants scolarisés de 13 à 15 ans) ayant rapporté ou n’ayant pas rapporté une exposition à des VP ou des VS. Nous avons estimé les Odds Ratios (OR) pour ces comportements et les intervalles de confiance à 95 % correspondants (IC), après ajustement pour l’âge et le sexe.
Résultats
27 à 50 % (42 % en moyenne) des enfants étudiés dans les cinq pays ont signalé avoir été exposés à des VP pendant les 12 mois précédant l’enquête et 9 à 33 % (23 % en moyenne) ont rapporté avoir été exposés à des VS leur vie durant. On a observé des associations modérées à forte entre l’exposition à des VP ou à des VS et des mesures de la santé mentale, les idées de suicide, le tabagisme actuel (cigarettes), la consommation d’alcool actuelle, l’usage de drogues sur la durée de vie, la multiplication des partenaires sexuels et les antécédents d’infection sexuellement transmissible (p ≤ 0,05 pour l’ensemble des associations). Par exemple, l’Odds ratio associé au tabagisme actuel (cigarettes) était plus élevé chez les enfants ayant participé à une bagarre (OR : 2,20 ; IC à 95 % : 1,77-2,75), à 2-5 bagarres (OR : 3,43 ; IC à 95 % : 2,54-4,63) et à 6 bagarres ou plus (OR : 5,95 ; IC à 95 % : 4,37-8,11) (p de tendance < 0,001) pendant les 12 mois précédant l’enquête, que chez les enfants non exposés à des VP.
Conclusion
L’exposition à des VP ou à des VS est courante chez les enfants de certains pays d’Afrique et on relève des associations entre cette exposition et plusieurs comportements préjudiciables à la santé. Dans les pays en développement, la prise de conscience grandissante de la fréquence des expositions à la violence chez les enfants et de leurs conséquences potentielles sur la santé pourrait rendre les responsables plus attentifs aux besoins en matière programmes de promotion de la santé et de prévention pour faire face à ce problème.
Resumen
Objetivo
Examinar la relación entre la exposición a violencia física (VF) o violencia sexual (VS) y los comportamientos de salud adversos en una muestra de niños de cinco países africanos.
Métodos
Mediante un análisis transversal de datos de Namibia, Swazilandia, Uganda, Zambia y Zimbabwe –países que participaron en el Estudio mundial de la salud de los alumnos en las escuelas en 2003 o 2004– procedimos a comparar la frecuencia relativa de varios comportamientos de salud adversos entre los niños (principalmente escolares de 13 a 15 años), según hubieran declarado o no que habían estado expuestos a VF o VS. Se estimaron las razones de posibilidades (OR) para tales comportamientos y sus intervalos de confianza (IC) del 95% después de ajustar los datos en función de la edad y el sexo.
Resultados
Entre el 27% y el 50% (promedio: 42%) de los niños estudiados en los cinco países declararon haber estado expuestos a VF durante los 12 meses previos a la encuesta, y un 9%–33% (promedio: 23%) declaró haber estado expuesto a VS en algún momento de su vida. Se observó una relación entre moderada y fuerte entre la exposición a VF o VS y la adopción de medidas de salud mental, las ideas suicidas, el consumo de cigarrillos del momento, el consumo de alcohol del momento, el uso de drogas a lo largo de la vida, la relación con varias parejas sexuales y la existencia de antecedentes de infección de transmisión sexual (p ≤ 0,05 en todos los casos). Por ejemplo, la probabilidad de que el niño fumara cigarrillos a la sazón fue mayor entre los que se habían visto implicados en una pelea (OR: 2,20; IC95%: 1,77–2,75), 2–5 peleas (OR: 3,43; IC95%: 2,54–4,63) o 6 peleas o más (OR: 5,95; IC95%: 4,37–8,11) (p de la tendencia < 0,001) en los 12 meses previos al estudio que en los niños no expuestos a VF.
Conclusión
La exposición a VF y VS es común entre los niños africanos en algunos países y se asocia a numerosos comportamientos de salud adversos. En los países en desarrollo, una mayor sensibilización sobre la frecuencia de la exposición de los niños a la violencia y sus posibles consecuencias sanitarias puede resaltar la necesidad de emprender programas de prevención y de promoción de la salud que aborden ese problema.
ملخص
الغرض
دراسة ترافق التعرُّض للعنف البدني أو العنف الجنسي مع السلوكيات الصحية الضائرة لدى الأطفال في 5 بلدان أفريقية.
الطريقة
في تحليل مقطعي مستعرض للمعطيات المستمدَّة من ناميبيا وسوازيلاند وأوغندا وزامبيا وزيمبابوي وهي البلدان التي شاركت في المسح العالمي لصحة طلاب المدارس في عام 2003 أو عام 2004 أجرى الباحثون مقارنة للتكرار النسبي للسلوكيات الصحية الضائرة المتعدِّدة لدى الأطفال (وبشكل أساسي الطلاب في أعمار 13 – 15 عاماً) والذين أبلغوا أو لم يبلغوا عن تعرُّضهم للعنف البدني أو العنف الجنسي. وقد قدروا نسبة الأرجحية لمثل هذه السلوكيات بفاصلة ثقة 95 بعد التعديل بالنسبة للعمر والجنس.
الموجودات
أبلغ 27% إلى 50% (الوسطي 42%) من الأطفال الذين دُرٍسوا في البلدان الخمسة عن التعُّرض للعنف الجسدي خلال الأشهر الاثني عشر التي سبقت المسح بينما تراوحت نسبة الإبلاغ عن التعرُّض للعنف الجنسي طيلة الحياة بين 9% و33% (الوسطي 23%). وقد لوحظ وجود ارتباط يتراوح بين المعتدل والشديد بين التعرُّض للعنف البدني والعنف الجنسي وتدابير الصحة النفسية والتفكير بالانتحار وتعاطي التبغ في ذلك الوقت ومعاقرة الكحول في ذلك الوقت وتعاطي المخدِّرات في أي وقت من الحياة، وتعدد القرناء في الممارسة الجنسية وسوابق العدوى بمرض منقول جنسياً (قوى الاحتمال P يساوي أو أقل من 0.05 في جميع الترافقات)، فعلى سبيل المثال كانت أرجحية تدخين السجائر بين الأطفال الذين تورطوا في عراك لمرة واحدة (نسبة الأرجحية 2.20 بفاصلة ثقة 95 تراوحت بين 1.77 و2.75)، وبين الأطفال الذين شاركوا في العراك 2 – 5 مرات (نسبة الأرجحية 3.43، فاصلة ثقة 95% إذ تراوحت بين 2.54 – 4.63) و الأطفال الذين تورطوا في 6 مرات أو أكثر من العراك (نسبة الأرجحية 5.95 وبفاصلة ثقة 95% وتراوحت 4.37 و8.11) وقيمة الاحتمال للنزوع أقل من 0.001) خلال الإثني عشر شهراً التي سبقت إجراء المسح، أعلى مما لدى الأطفال الذين لم يتعرضوا للعنف البدني.
الاستنتاج
يشيع تعرُّض الأطفال في بعض البلدان الأفريقية إلى العنف البدني والعنف الجنسي، ويترافق مع سلوكيات صحية ضائرة ومتعددة. وفي البلدان النامية قد يؤدِّي ازدياد الوعي بتكرار تعرُّض الأطفال للعنف والعواقب الصحية المحتملة له إلى إيلاء اهتمام أكثر بالحاجة إلى برامج تعزيز الصحة وحفظها التي تعالج هذه المشكلة.
Introduction
Exposure to violence and traumatic stressors among children is common1 and has both short- and long-term effects on multiple health behaviours (e.g. smoking, substance abuse, physical inactivity) and health outcomes (e.g. higher prevalences of heart, lung, and liver disease, diabetes, and depression).2,3 Moreover, such exposure appears to influence health behaviours and outcomes through a cumulative process.2
While our understanding of the burden of violence and its relationship with adverse health behaviours has increased globally, studies on such questions in children in Africa are lacking and until recently few data were available. An understanding of such relationships is important for policy and programme planning efforts. With this in mind, we estimated the prevalence of exposure to physical violence (PV), sexual violence (SV) or both among children from five African countries and examined the association between exposure to violence and several adverse health behaviours during childhood using data from the Global School-based Student Health Survey (GSHS).
Methods
The GSHS is a self-administered, school-based survey developed by WHO in collaboration with the United Nations Children’s Fund, the United Nations Educational, Scientific and Cultural Organization, and the Joint United Nations Programme on HIV/AIDS, and with technical and financial assistance from the United States Centers for Disease Control and Prevention in Atlanta, GA. The survey is conducted primarily among students 13–15 years of age and can be administered during one regular class period. In each country, the questionnaire comprises multiple core modules, core-expanded questions and country-specific questions, and a standardized scientific sample selection process and common school-based methods are followed. Further details of the GSHS can be obtained at http://www.who.int/chp/gshs and http://www.cdc.gov/gshs
In this analysis, we pooled data from five African countries – Namibia, Swaziland, Uganda, Zambia, Zimbabwe – where the survey was administered during 2003 or 2004 (Table 1). These countries were selected because each included questions on exposure to PV and SV as well as questions on mental health, tobacco use, the use of alcohol and other drugs, and sexual behaviours, though not all countries asked all questions under each domain. For example, Swaziland and Zambia had no questions on cigarette smoking, Swaziland had none on suicidal ideation, and Namibia and Uganda had none on the history of sexually transmitted infections (STI).
Table 1. Sampling method, response rates, and sample size for five African countries that participated in the GSHS, 2003–2004.
| Country | Year | Sampling method |
Response rate (%) |
n |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| School level | Class level | Schools | Students | Overall | Total | Analytica | ||||||
| Namibia | 2004 | All regular schools with grades 6–10 included in sampling frame. Systematic sampling with random start and probability proportional to enrollment in grades 6–10. Schools sampled: 100 | All classes with most students in grades 6–10 included in sampling frame. Systematic equal probability sampling with random start used to select classes from each school included in survey. Students sampled: 7374 | 95 | 86 | 82 | 6367 | 5912 | ||||
| Swaziland | 2003 | All regular schools with grades 6 or 7 or forms 1–4 included in sampling frame. Systematic sampling with random start and probability proportional to enrollment in grades 6 or 7 or forms 1–4. Schools sampled: 100 | All classes with most students in grades 6 or 7 or forms 1–4 included in sampling frame. Systematic equal probability sampling with random start used to select classes from each school included in survey. Students sampled: 7419 | 97 | 99 | 96 | 7341 | 6427 | ||||
| Uganda | 2003 | All regular schools with standards 1–3 included in sampling frame. Systematic sampling with random start and probability proportional to enrollment in standards 1–3. Schools sampled: 50 | All classes with most students in standards 1–3 included in sampling frame. Systematic equal probability sampling with random start used to select classes from each school included in survey. Students sampled: 4218 | 90 | 76 | 69 | 3215 | 2918 | ||||
| Zambia | 2004 | All regular schools with grades 6–10 included in sampling frame. Systematic sampling with random start and probability proportional to enrollment in grades 6–10. Schools sampled: 50 | All classes with most students in grades 6–10 included in sampling frame. Systematic equal probability sampling with random start used to select classes from each school included in survey. Students sampled: 3021 | 94 | 75 | 70 | 2257 | 1947 | ||||
| Zimbabwe | 2003 | All regular schools with forms 1–3 included in sampling frame. Systematic sampling with random start and probability proportional to enrollment in forms 1–3. | All classes with most students in forms 1–3 included in sampling frame. Systematic equal probability sampling with random start used to select classes from each school included in survey. | 5665 | 5452 | |||||||
| Bulawayo | Schools sampled: 26 | Students sampled: 2151 | 100 | 84 | 84 | 1804 | 1737 | |||||
| Harare | Schools sampled: 25 | Students sampled: 2380 | 100 | 84 | 84 | 1997 | 1950 | |||||
| Manicaland | Schools sampled: 25 | Students sampled: 2188 | 100 | 85 | 85 | 1864 | 1765 | |||||
GSHS, Global School-based Student Health Survey. a Observations with complete data for age, sex, involvement in a physical fight during the 12 months preceding the survey, and having ever been physically forced to have sexual intercourse.
Exposure to PV and SV
Survey questions about exposure to PV and SV and variable definitions are available in Appendix A, available at: http://www.who.int/bulletin/volumes/87/6/07-047423/en/index.html). To examine associations with the combined occurrence of exposure to PV and SV, we created a score variable that was assigned the values 0 in the absence of exposure to both PV and SV, 1 in the presence of exposure to one form of violence or the other, and 2 in the presence of exposure to both PV and SV.
Adverse health behaviours or events
We compared the relative frequency and likelihood of several adverse health behaviours or events in children who had and had not been exposed to PV and/or SV. Survey questions and variable definitions for these behaviours are available in Appendix B, available at: http://www.who.int/bulletin/volumes/87/6/07-047423/en/index.html.
Statistical analysis
When judging the appropriateness of combining GSHS data across countries, we took into consideration sampling design, sampling error and nonsampling error. Prior research from the United States has shown that pooling state-based survey data to obtain national estimates is feasible depending on sampling and nonsampling error.4 In the GSHS, sampling designs were similar across countries (Table 1). The sampling of students within each country was conducted at two levels: the school and the class. Schools and classes included in the sampling frame for each country are provided in Table 1. We examined country-level sampling errors (large sampling errors imply imprecise survey estimates) by using the coefficient of variation of survey weights and the design effect averaged across all survey items for each country. Averaged design effects ranged from 1.5 for Zimbabwe (Harare) to 2.2 for Namibia; coefficients of variation ranged from 0.3307 for Uganda to 0.7677 for Namibia. We examined nonsampling errors using survey response rates. Response rates ranged from 69% (Uganda) to 96% (Swaziland) (Table 1). Of the 24 845 observations available for analysis after pooling country data sets, 92% (n = 22 656) had complete information on age, sex and the variables for exposure to PV and SV.
We compared the relative frequency of each of the adverse health behaviours or events noted above in children who reported exposure to PV or SV and in those who did not report such exposure. A χ² test was used to compare differences in categorical variables across groups. We examined associations with exposure to PV and SV individually and to both PV and SV by using a score variable approach. After adjusting for age and sex, we used unconditional logistic regression to obtain adjusted odds ratios (aORs) and 95% confidence intervals (CIs) for associations between PV and/or SV and each of the adverse health behaviours. Ordinal trend tests used logistic regression with the dependent variable of interest and an ordinal independent variable. To make the GSHS data representative of each country included in the analysis, sample weights were used. To account for the complex sampling design and to obtain accurate variance estimates, we used Stata version 9 (Stata Corp., College Station, TX, USA) to complete all analyses. All statistical inferences were based on a 0.05 significance level.
Results
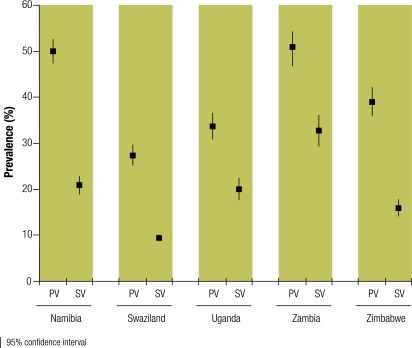
Of the children sampled, 42% (standard error, SE: 0.95) had been exposed to PV during the 12 months preceding the survey; and 23% (SE: 0.80) had been exposed to SV during their lifetime (Table 2). Exposure to both PV and SV was reported in 12% (SE: 0.66); to PV or SV but not both, in 41% (SE: 0.74); and to no violence, in 47% (SE: 1.00), with differences by age group noted (P ≤ 0.05). After age adjustment, the odds of having been exposed to PV were greater among boys than girls (aOR: 1.21; 95% CI: 1.06–1.39; P ≤ 0.01). Similarly, the odds of having been exposed to SV were greater among girls than boys (aOR: 1.29; 95% CI: 1.12–1.48; P ≤ 0.001) after age adjustment, although differences between genders were not large (Table 2). Exposure to violence differed across countries (P ≤ 0.001); exposure to PV ranged from 27% to 50% and exposure to SV, from 9% to 33% (Fig. 1).
Table 2. Exposurea to PV or SV, by age and sex, among 22 656 students from five African countries that participated in the GSHS, 2003-2004.
| N | Times involved in physical fight during 12 months preceding survey |
Ever physically forced to have sex |
|||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 0 times |
1 time |
2–5 times |
≥ 6 times |
||||||||||||
| n | % (SE) | n | % (SE) | n | % (SE) | n | % (SE) | n | % (SE) | ||||||
| Girls | |||||||||||||||
| Age, in years | |||||||||||||||
| ≤ 13 | 2523 | 1642 | 53.0 (2.76) | 456 | 21.0 (1.76) | 268 | 13.7 (1.43) | 157 | 12.3 (1.90) | 342 | 21.5 (2.17) | ||||
| 14 | 3816 | 2630 | 61.7 (1.88) | 627 | 18.0 (1.16) | 395 | 13.4 (1.21) | 164 | 6.9 (0.93) | 556 | 22.0 (1.62) | ||||
| 15 | 3906 | 2699 | 61.4 (1.99) | 606 | 16.6 (1.09) | 409 | 13.3 (1.23) | 192 | 8.8 (1.01) | 702 | 26.7 (1.86) | ||||
| ≥ 16 | 2359 | 1532 | 63.8 (1.65) | 359 | 14.1 (1.02) | 277 | 12.3 (1.16) | 191 | 9.8 (1.02) | 640 | 28.7 (1.69) | ||||
| Boys | |||||||||||||||
| Age, in years | |||||||||||||||
| ≤ 13 | 1610 | 832 | 48.8 (2.75) | 363 | 22.6 (2.33) | 289 | 17.0 (1.72) | 126 | 11.5 (1.24) | 270 | 23.8 (2.70) | ||||
| 14 | 2566 | 1440 | 55.6 (1.97) | 537 | 19.9 (1.29) | 399 | 14.5 (1.37) | 190 | 10.0 (1.24) | 328 | 16.7 (1.73) | ||||
| 15 | 3059 | 1740 | 57.3 (1.73) | 594 | 19.7 (1.15) | 455 | 13.8 (1.17) | 270 | 9.3 (0.89) | 466 | 22.1 (1.31) | ||||
| ≥ 16 | 2817 | 1652 | 59.6 (1.95) | 527 | 18.8 (1.26) | 377 | 12.0 (1.08) | 261 | 9.6 (1.00) | 545 | 21.4 (1.20) | ||||
GSHS, Global School-based Student Health Survey; PV, physical violence; SE, standard error; SV, sexual violence. a Data are presented as the unweighted number of observations, in the analytic sample, of exposure to physical fighting or to sex under physical force, and corresponding weighted prevalences.
Fig. 1.
Exposure to PVa during the 12 months preceding the survey and exposure to lifetime SVb in a sample of children from five African countries that participated in the GSHS, 2003–2004
GSHS, Global School-based Student Health Survey; PV, physical violence; SV, sexual violence.
a Exposure to PV was defined by response to the question, “During the past 12 months, how many times were you involved in a physical fight?”
b Exposure to SV was defined by response to the question, “Have you ever been physically forced to have sexual intercourse?”
Mental health and suicidal ideation
Approximately 16% (SE: 0.55) of the children reported feeling loneliness always or most of the time during the 12 months preceding the survey; 33% (SE: 0.67) reported never feeling lonely; 14% (SE: 0.68) reported rarely feeling lonely, and 37% (SE: 0.71) reported feeling lonely sometimes. The distribution did not vary by age or sex. Compared to unexposed children, those exposed to PV or SV had greater odds of reporting persistent loneliness (Table 3). Compared to children who did not experience either PV or SV, those exposed to both forms of violence had more than twice the odds of feeling lonely most or all of the time (Table 3).
Table 3. Relative frequency and aORs of lonelinessa or worry resulting in sleep lossb associated with PV and SV in a sample of African children, GSHS, 2003-2004.
| Lonely most or all of the timec |
So worried could seldom or never sleepc |
||||
|---|---|---|---|---|---|
| % (SE)d | aOR (95% CI)e | % (SE)d | aOR (95% CI)e | ||
| Times involved in physical fight during 12 months preceding survey | |||||
| 0f | 13.3 (0.64) | 1.00 | 13.7 (0.98) | 1.00 | |
| 1 | 15.7 (1.19) | 1.23 (1.01–1.51) | 16.7 (1.00) | 1.28 (1.07–1.54) | |
| 2–5 | 20.3 (1.18) | 1.68 (1.39–2.02) | 23.4 (1.48) | 1.95 (1.61–2.35) | |
| 6+ | 28.3 (1.78) | 2.59 (2.10–3.20) | 32.3 (2.17) | 3.02 (2.48–3.69) | |
| P for trend < 0.001 | P for trend < 0.001 | ||||
| Ever physically forced to have sexual intercourse | |||||
| Nof | 14.6 (0.56) | 1.00 | 14.6 (0.61) | 1.00 | |
| Yes | 21.3 (1.30) | 1.57 (1.32–1.86) | 26.5 (1.18) | 2.09 (1.81–2.41) | |
| Physical and sexual violence scoreg | |||||
| 0f | 12.2 (0.64) | 1.00 | 12.1 (0.58) | 1.00 | |
| 1 | 18.3 (0.72) | 1.62 (1.41–1.85) | 19.2 (0.91) | 1.75 (1.55–1.96) | |
| 2 | 24.4 (2.13) | 2.32 (1.79–3.02) | 32.1 (1.69) | 3.43 (2.86–4.13) | |
| P for trend < 0.001 | P for trend < 0.001 | ||||
aOR, adjusted odds ratio; CI, confidence interval; GSHS, Global School-based Student Health Survey; PV, physical violence; SE, standard error; SV, sexual violence. a The logistic regression models for feelings of loneliness were fit to the data of 15 974 respondents. b The logistic regression models for sleep loss resulting from worry were fit to the data of 16 096 respondents. c During the 12 months preceding the survey. d Data are reported as weighted percentages. e ORs and 95% CIs adjusted for age and sex. f Reference category for aORs. g The physical and sexual violence score is the sum of the points for involvement in a physical fight (yes, 1; no, 0) during the 12 months preceding the survey and for having ever been physically forced to have sexual intercourse (yes, 1; no, 0).
Persistent sleep problems as a result of worry were reported by 17% (SE: 0.61) of children, and their frequency was similar across age groups and in boys and girls. A third (35%; SE: 0.81) of the children reported no such sleep problems and 14% (SE: 0.68) reported rare occurrences. The odds of persistent sleep problems due to worry were three times greater among children with ≥ 6 exposures to PV and two times greater among children exposed to SV than among unexposed children (Table 3).
Nearly one in four (24%; SE: 0.84) children reported having considered suicide and 29% (SE: 0.93) reported having planned suicide during the 12 months preceding the survey. Associations between exposure to PV and both measures of suicidal ideation were strong and dose-related (P for trend < 0.001), and the odds of having had suicidal ideation were twice as high among children exposed to SV as among unexposed children (Table 4).
Table 4. Relative frequency and aORsa of having consideredb or planned suicide in a sample of African children, by exposure to PV and/or SV, GSHS, 2003-2004.
| Considered suicide |
Planned suicide |
||||
|---|---|---|---|---|---|
| % (SE)c | aOR (95% CI)d | % (SE)c | aOR (95% CI)d | ||
| Times involved in physical fight during the 12 months preceding survey | |||||
| 0e | 19.4 (0.74) | 1.00 | 23.5 (0.94) | 1.00 | |
| 1 | 24.7 (1.41) | 1.38 (1.18–1.61) | 30.9 (1.69) | 1.46 (1.22–1.76) | |
| 2–5 | 30.7 (1.98) | 1.86 (1.58–2.20) | 37.5 (1.85) | 1.97 (1.69–2.29) | |
| 6+ | 37.2 (2.12) | 2.48 (2.04–3.01) | 44.6 (2.28) | 2.63 (2.21–3.12) | |
| P for trend < 0.001 | P for trend < 0.001 | ||||
| Ever physically forced to have sexual intercourse | |||||
| Noe | 20.1 (0.70) | 1.00 | 25.2 (0.89) | 1.00 | |
| Yes | 35.3 (1.73) | 2.15 (1.86–2.48) | 40.5 (1.57) | 2.00 (1.76–2.28) | |
| Physical and sexual violence scoref | |||||
| 0e | 16.9 (0.64) | 1.00 | 20.7 (0.86) | 1.00 | |
| 1 | 26.7 (1.11) | 1.81 (1.61–2.04) | 33.4 (1.33) | 1.93 (1.70–2.19) | |
| 2 | 40.2 (2.50) | 3.30 (2.71–4.03) | 45.3 (2.25) | 3.15 (2.58–3.85) | |
| P for trend < 0.001 | P for trend < 0.001 | ||||
aOR, odds ratio; CI, confidence interval; GSHS, Global School-based Student Health Study; PV, physical violence; SE, standard error; SV, sexual violence. a The logistic regression models for suicide consideration were fit to the data of 15 653 respondents, and those for suicide planning were fit to the data of 15 567 respondents. Swaziland did not ask questions in this domain. b Over the 12 months preceding the survey. c Data are reported as weighted percentages, and standard errors are reported in parentheses. d ORs and 95% CIs adjusted for age and sex. e Reference category for aORs. f The physical and sexual violence score is the sum of the points for involvement in a physical fight (yes, 1; no, 0) during the 12 months preceding the survey and for having ever been physically forced to have sexual intercourse (yes, 1; no, 0).
Substance use
The frequency of current cigarette use (8%; SE: 0.52) was similar across age groups but slightly greater among boys (10%) than girls (6%) (P < 0.001). The associations between exposure to PV and current cigarette use were strong and dose-related (Table 5). Similarly strong associations were observed for current alcohol use (frequency, 24%; SE: 0.90) and lifetime drug use (frequency, 19%; SE: 1.03) (Table 5). Finally, current frequent alcohol use also was associated with exposure to PV (≥ 6 episodes versus 0, aOR: 14.00; 95% CI: 9.39–20.89) or SV (aOR: 3.65; 95% CI: 2.63–5.06) (data not shown).
Table 5. Relative frequency and aORs of current cigarette use,a current alcohol use,b or lifetime drug usec associated with PV and SV among African children, GSHS, 2003-2004.
| Current cigarette use |
Current alcohol use |
Lifetime drug use |
||||||
|---|---|---|---|---|---|---|---|---|
| % (SE)d | aOR (95% CI)e | % (SE)d | aOR (95% CI)e | % (SE)d | aOR (95% CI)e | |||
| Times involved in physical fight during the 12 months preceding survey | ||||||||
| 0f | 4.6 (0.39) | 1.00 | 15.7 (0.72) | 1.00 | 11.2 (0.74) | 1.00 | ||
| 1 | 9.8 (1.09) | 2.20 (1.77–2.75) | 26.9 (1.72) | 1.97 (1.64–2.37) | 23.6 (1.82) | 2.39 (1.87–3.05) | ||
| 2–5 | 14.5 (1.60) | 3.43 (2.54–4.63) | 37.7 (1.99) | 3.26 (2.71–3.91) | 29.4 (1.91) | 3.25 (2.72–3.90) | ||
| 6+ | 22.9 (2.60) | 5.95 (4.37–8.11) | 54.3 (3.13) | 6.31 (4.89–8.13) | 48.0 (3.11) | 7.19 (5.60–9.23) | ||
| P for trend < 0.001 | P for trend < 0.001 | P for trend < 0.001 | ||||||
| Ever physically forced to have sexual intercourse | ||||||||
| Nof | 6.6 (0.43) | 1.00 | 20.0 (0.82) | 1.00 | 15.7 (0.93) | 1.00 | ||
| Yes | 13.1 (1.37) | 2.29 (1.87–2.80) | 37.8 (1.59) | 2.48 (2.17–2.83) | 31.6 (1.83) | 2.54 (2.15–3.01) | ||
| Physical and sexual violence scoreg | ||||||||
| 0f | 4.0 (0.31) | 1.00 | 13.6 (0.74) | 1.00 | 9.7 (0.72) | 1.00 | ||
| 1 | 10.6 (0.83) | 2.82 (2.38–3.34) | 29.8 (1.22) | 2.71 (2.32–3.15) | 23.3 (1.26) | 2.79 (2.36–3.31) | ||
| 2 | 20.2 (2.30) | 6.15 (4.67–8.10) | 50.9 (2.42) | 6.56 (5.39–7.98) | 45.1 (2.75) | 7.63 (6.00–9.69) | ||
| P for trend < 0.001 | P for trend < 0.001 | P for trend < 0.001 | ||||||
aOR, adjusted odds ratio; CI, confidence interval; GSHS, Global School-based Student Health Survey; PV, physical violence; SE, standard error; SV, sexual violence. a The logistic regression models for current cigarette use were fit to the data of 12 041 respondents. Swaziland and Zambia did not ask questions related to cigarette smoking. b The logistic regression models for current alcohol use were fit to the data of 19 443 respondents. c The logistic regression models for lifetime drug use were fit to the data of 21 888 respondents. d Data are reported as weighted percentages. e ORs and 95% CIs adjusted for age and sex. f Reference category for aORs. g The physical and sexual violence score is the sum of the points for involvement in a physical fight (yes, 1; no, 0) during the 12 months preceding the survey and for having ever been physically forced to have sexual intercourse (yes, 1; no, 0).
Risky sexual behaviour
One in five (SE: 0.95) boys and one in 10 (SE: 0.90) girls reported multiple sex partners. More than one in five (SE: 1.19) children reported having had an STI. After adjustment for age and sex, children exposed to PV or SV had significantly greater odds of reporting risky sexual behaviours or a history of STI (Table 6).
Table 6. Relative frequency and aORs of having multiple sex partnersa or a history of STIb associated with PV and SV in a sample of African children, GSHS, 2003-2004.
| Multiple partners (lifetime) |
History of STI |
||||
|---|---|---|---|---|---|
| % (SE)c | aOR (95% CI)d | % (SE)c | aOR (95% CI)d | ||
| Times involved in physical fight during the 12 months preceding survey | |||||
| 0e | 11.5 (0.72) | 1.00 | 17.6 (1.19) | 1.00 | |
| 1 | 18.5 (1.37) | 1.77 (1.41–2.21) | 25.1 (2.67) | 1.58 (1.16–2.17) | |
| 2–5 | 23.2 (1.69) | 2.31 (1.85–2.88) | 23.4 (2.27) | 1.46 (1.14–1.87) | |
| 6+ | 38.7 (3.27) | 5.09 (3.73–6.94) | 33.2 (3.41) | 2.30 (1.64–3.22) | |
| P for trend < 0.001 | P for trend < 0.001 | ||||
| Ever physically forced to have sexual intercourse | |||||
| Noe | 12.8 (0.64) | 1.00 | 18.2 (1.22) | 1.00 | |
| Yes | 29.0 (1.65) | 3.14 (2.59–3.79) | 31.9 (1.73) | 2.09 (1.76–2.49) | |
| Physical and sexual violence scoref | |||||
| 0e | 9.9 (0.70) | 1.00 | 15.2 (0.95) | 1.00 | |
| 1 | 18.9 (0.85) | 2.18 (1.87–2.55) | 23.7 (1.98) | 1.72 (1.43–2.07) | |
| 2 | 39.6 (2.76) | 6.59 (4.93–8.80) | 35.7 (2.91) | 3.10 (2.24–4.29) | |
| P for trend < 0.001 | P for trend < 0.001 | ||||
aOR, adjusted odds ratio; CI, confidence interval; GSHS, Global School-based Student Health Survey; PV, physical violence; SE, standard error; STI, sexually transmitted infection; SV, sexual violence. a The logistic regression models for multiple sex partners were fit to the data of 14 961 respondents. b The logistic regression models for history of STI were fit to the data of 12 813 respondents. Namibia and Uganda did not ask the question on the history of STI. c Data are reported as weighted percentages. d ORs and 95% CIs adjusted for age and sex. e Reference category for aORs. f The physical and sexual violence score is the sum of the points for involvement in a physical fight (yes, 1; no, 0) during the 12 months preceding the survey and having ever been physically forced to have sexual intercourse (yes, 1; no, 0).
Gender
Through secondary analyses we explored whether the associations described above between exposure to PV or SV and the adverse health behaviours differed for girls and boys (i.e. whether the effect was modified by gender). Effect modification by gender (evaluated at P ≤ 0.05) was observed for the relationship between violence and some adverse health behaviours, but not all behaviours. For instance, the odds of using drugs were 9.53 (95% CI: 7.14–12.73) times greater among girls exposed to 6 or more physical fights than among girls exposed to none, while in boys exposed to 6 or more physical fights the odds were only 5.65 (95% CI: 4.04–7.89) times greater than in unexposed boys (P for interaction = 0.033). Stronger associations were also observed among girls between exposure to PV and multiple sex partners (girls, ≥ 6 versus 0 fights: OR: 8.36; 95% CI: 4.89–14.27; boys, ≥ 6 versus 0 fights: OR: 3.64; 95% CI: 2.52–5.26) (P for interaction = 0.039) and between exposure to SV and multiple sex partners (girls: OR: 4.45; 95% CI: 3.28–6.03; boys: OR: 2.37; 95% CI: 1.89–2.98) (P for interaction = 0.001). Only the association between forced sexual intercourse and planned suicide was slightly stronger for boys (OR: 2.43; 95% CI: 2.04–2.90) than for girls (OR: 1.63; 95% CI: 1.37–1.95) (P for interaction = 0.002).
Discussion
In the current study, exposure to PV or SV was found to be common among boys and girls in five African countries, where 1 in 10 children were exposed to both PV and SV. We found strong associations between exposure to PV, SV or both and multiple adverse health behaviours during childhood. In the case of exposure to PV, associations with health behaviours were dose-related, so that increases in exposure were associated with increased odds of showing the behaviours. In addition, the presence of multiple forms of violence was associated with increased odds of adverse health behaviours.
Our findings from five African countries contribute to the understanding of the relationship between violence and adverse health behaviours among children in several ways. First, they lend further support to research findings from developed countries that show exposure to violence is related to adverse health behaviours. Many of the health behaviours examined in our study are known to have implications for adult health behaviours and health outcomes later in life (e.g. smoking and cardiovascular and respiratory disease). Health behaviours such as cigarette smoking, alcohol use, or drug use may serve, either consciously or unconsciously, as coping mechanisms in the presence of stress resulting from exposure to violence. To the extent that such behaviours feel like effective and immediate solutions (through coping processes), they may become chronic and affect health in adulthood. Therefore, continued research is needed on the long-term implications of childhood exposure to violence. Researchers and programme managers trying to understand and prevent adverse health behaviours such as those discussed here may benefit from considering exposure to violence during childhood as a point of entry to intervene.
Second, we observed an association between exposure to PV among peers and adverse health behaviours. Studies of childhood maltreatment and its relationship to adverse health behaviours most often focus on maltreatment at the hands of parents or caretakers. Our findings expand this literature by showing that in some African countries peer violence is associated with similar adverse health behaviours, both among boys and girls.
Our findings also contribute to the understanding of the burden of exposure to PV and SV among boys and girls in Africa. First, few data exist on the burden of childhood violence outside of South Africa. Second, the data from the five African countries we studied suggest that physical fighting is more common among girls and SV more common among boys than data from other more developed countries would lead one to predict. For example, we observed exposure to PV (based on involvement in any physical fight during the 12 months preceding the survey) among 36–47% of the girls, depending on age (Table 2). A cross-sectional survey of grade 8 students conducted during 1997 and 2004 in Cape Town showed involvement in physical fighting during the 12 months preceding the survey in 16% (95% CI: 14–18%) of girls.5 Similarly, physical fighting during the 12 months preceding the survey varied from 13% among girls participating in the 2001/2002 Health Behaviour in School-Aged Children survey in Finland to 32% among those participating in Hungary.6
Much of the published evidence shows that more girls than boys are victims of sexual abuse. For instance, in a sample of Cape Town high school students King et al.7 found that 2.0% of male and 13.3% of female respondents had been victims of attempted rape; 5.0% of males and 6.0% of females had been victims of completed rape, and the odds of having been the victim of attempted or completed rape were four times as high among females as among males. Our findings highlight the importance of not neglecting SV among boys and show that among African children exposure to SV and its potential consequences are as common among boys as among girls, contrary to what the existing literature may lead one to assume.
In Africa, understanding the burden of PV or SV during childhood and its association with health problems is a challenge due to insufficient data for establishing these associations. While children homicide rates in Africa are known to be among the highest in the world,8 the magnitude of the problem of fatal and non-fatal violence in children is unclear for most African countries. Further investment is needed in information systems for routine monitoring of trends in violent behaviour, injuries and deaths. Surveillance systems being developed with uniform standards for defining and measuring violence should also incorporate information from other sources, including health services (e.g. emergency departments) and law enforcement, education and other authorities.8 In addition, a continued and expanded commitment to routinely collect survey data on exposure to violence and health risk behaviours will be required to provide the data needed to further understand the complex interrelationships between violence and health behaviours and outcomes throughout the lifespan.
Our results should be interpreted in light of the following limitations. The GSHS is a school-based survey, so these data do not include children who do not attend school or who were absent from school the day the survey was administered, who may have higher prevalences of adverse risk behaviours.9 Because of the cross-sectional nature of the data, determinations and statements of cause and effect are impossible. We adjusted for age and gender in multivariable logistic regression models but were unable to account for possible differences in socioeconomic status and other covariates that might be associated with the school one attends, the prevalence of PV and/or SV or the prevalence of adverse health behaviours. Also, the time frames for health behaviour questions varied, with reference to either 30 days preceding the survey, 12 months preceding the survey, or to the entire lifetime. Also, our measure of current smoking does not distinguish those who experiment with cigarettes from those who smoke on a regular basis; however, symptoms of serious nicotine addiction often occur just days or weeks after youths first begin to “experiment” with smoking.10,11
These data are self-reported. Conceivably, some respondents may have misreported their exposure to PV or SV or their adverse health behaviours either out of embarrassment or to provide a socially desirable response. In addition, the measure of STIs is intended to capture only those infections diagnosed by a doctor or nurse; thus, we may be underestimating the true prevalence of STIs. Despite the potential problems of self-reported data, there is no reason to believe that children would systematically misreport in a manner that reflects the associations observed herein. Any misreporting is likely to have been nondifferential and thus would have biased our results towards the null hypothesis.
We must also keep in mind that the survey question on exposure to PV is focused on physical fighting among peers. Other types of PV, such as beatings by parents or teachers or violence that occurs between boyfriend and girlfriend, may not have been captured, so the prevalence of exposure to PV may be underestimated. Similarly, the survey question on exposure to SV did not distinguish between a perpetrator who was a peer or someone older than the student (e.g. parent, family member, caretaker, etc.).
In summary, these are among the first estimates of the burden of PV or SV among African children and their associations with adverse health behaviours. Because childhood exposure to violence is common and has strong associations with multiple health behaviours, increased attention to primary, secondary and tertiary prevention is needed. Increased awareness of the frequency of exposure to violence among children and potential health consequences in developing countries may lead to improvements in health promotion and disease prevention programmes. Further research and training are needed to help health professionals and programme managers recognize and understand the linkages between childhood exposure to violence and adverse health behaviours during childhood and across the life span. Tools and information, such as the World report on violence and health,8 the World report on violence against children1 and Preventing child maltreatment: a guide to taking action and generating evidence,12 are available to guide organizations in their efforts to prevent and respond to childhood exposure to violence. ■
Acknowledgements
The authors thank the country coordinators from Namibia (Kornelia K. Abraham), Swaziland (Mildred Xaba), Uganda (Jermiahs Twa-Twa), Zambia (George Sikazwe) and Zimbabwe (Edwin Sithole) for their assistance in collecting the Global School-based Student Health Survey data.
This research was completed while David W Brown worked in the Department of Injuries and Violence Prevention at the World Health Organization.
Appendix A. Questions and variable definitions for exposure to PV and SV, GSHS, 2003–2004
Physical violence
Student question: “A physical fight occurs when two or more students of about the same strength or power choose to fight each other. During the past 12 months, how many times were you involved in a physical fight?”
Variable: Physical violence
Value: = 1 if student responds ≥ 1 times; = 0 otherwise
Variable: Physical violence
Value: = 0 if response is 0 times; = 1 if response is 1 time; = 2 if response is 2–5 times; = 3 if response is ≥ 6 times
Note: ≥ 6 physical fights represents the upper 10% of the distribution.
Sexual violence
Student question: “Have you ever been physically forced to have sexual intercourse when you did not want to?”
Variable: Sexual violence
Value: = 1 if response is “yes”; = 0 otherwise
GSHS, Global School-based Student Health Survey; PV, physical violence; SV, sexual violence.
Appendix B. Questions and variable definitions for several adverse health behaviours or events, GSHS, 2003–2004
Persistent feelings of loneliness
Student question: “During the past 12 months, how often have you felt lonely?”
Variable: Loneliness
Value: = 1 if response is “most of the time” or “always”; = 0 otherwise
Persistent sleep loss
Student question: “During the past 12 months, how often have you been so worried about something that you could not sleep at night?”
Variable: Sleep loss
Value: = 1 if response is “most of the time” or “always”; = 0 otherwise
Suicide ideation
Student question: “During the past 12 months, did you ever seriously consider attempting suicide?”
Variable: Considered suicide
Value: = 1 if response is “yes”; = 0 otherwise
Student question: “During the past 12 months, did you make a plan about how you would attempt suicide?”
Variable: Planned suicide
Value: = 1 if response is “yes”; = 0 otherwise
Current cigarette smoker
Student question: “During the past 30 days, on how many days did you smoke cigarettes?”
Variable: Smoker
Value: = 1 if response is smoked on ≥ 1 day within the past 30 days; = 0 otherwise
Alcohol use
Student question: “During the past 30 days, on how many days did you have at least one drink containing alcohol?”
Variable: Current alcohol use
Value: = 1 if had at least one drink on ≥ 1 day; = 0 otherwise
Variable: Current frequent alcohol use
Value: = 1 if response is alcohol on ≥ 20 days; = 0 otherwise
Note: ≥ 20 days is approximately the upper 5% of the variable distribution.
Lifetime drug use
Student question: “During your life, how many times have you used drugs, such as [country specific examples including marijuana njaga, bangi, opium, njaye, cocaine, crack, ecstasy, dagga, glue]?”
Variable: Drug use
Value: = 1 if response is ≥ 1 time during lifetime; = 0 otherwise
Sexual intercourse with multiple partners
Student question: “During your life, with how many people have you had sexual intercourse?”
Variable: Multiple partners
Value: = 1 if response is ≥ 2 partners; = 0 otherwise
History of sexually transmitted infection (STI)
Student question: “Have you ever been told by a doctor or nurse that you had a sexually transmitted infection, such as infection with HIV, AIDS, syphilis or gonorrhoea?”
Variable: STI
Value: = 1 if response is “yes”; = 0 otherwise
GSHS, Global School-based Student Health Survey.
Footnotes
Competing interests: None declared.
References
- 1.United Nations Secretary-General’s study on violence against children. World report on violence against children Geneva: UN; 2006.
- 2.Centers for Disease Control and Prevention. Adverse childhood experiences study. Publications on major findings by health outcomes. Atlanta, GA: CDC; 2009. Available from: www.cdc.gov/nccdphp/ACE/outcomes.htm [accessed on 1 July 2007].
- 3.Chartier MJ, Walker JR, Naimark B. Childhood abuse, adult health, and health care utilization: results from a representative community sample. Am J Epidemiol. 2007;165:1031–8. doi: 10.1093/aje/kwk113. [DOI] [PubMed] [Google Scholar]
- 4.Iachan R, Schulman J, Powell-Griner E, Nelson DE, Mariolis P, Stanwyck C. Pooling state telephone survey health data for national estimates: the CDC Behavioral Risk Factor Surveillance System, 1995. In: Cynamon ML, Kulka RA, eds. Seventh conference on health survey research methods Hyattsville, MD: US Department of Health and Human Services; 2001 (Publication No. PHS 01–1013). pp. 221–6. Available from: http://www.cdc.gov/nchs/data/conf/conf07.pdf [accessed on 15 July 2007].
- 5.Flisher AJ, Mathews C, Mukoma W, Lombard CJ. Secular trends in risk behavior of Cape Town grade 8 students. S Afr Med J. 2006;96:982–7. [PubMed] [Google Scholar]
- 6.Pickett W, Craig W, Harel Y, Cunningham J, Simpson K, Molcho M, et al. on behalf of theHSBC Violence and Injuries Writing Group. Cross-national study of fighting and weapon carrying as determinants of adolescent injury. Pediatrics 2005116e855–63. 10.1542/peds.2005-0607 [DOI] [PubMed] [Google Scholar]
- 7.King G, Flisher AJ, Noubary F, Reece R, Marais A, Lombard C. Substance abuse and behavioral correlates of sexual assault among South African adolescents. Child Abuse Negl. 2004;28:683–96. doi: 10.1016/j.chiabu.2003.12.003. [DOI] [PubMed] [Google Scholar]
- 8.World report on violence and health Geneva: World Health Organization; 2002. [DOI] [PubMed] [Google Scholar]
- 9.Flisher AJ, Chalton DO. High-school dropouts in a working-class South African community: selected characteristics and risk-taking behaviour. J Adolesc. 1995;18:105–21. doi: 10.1006/jado.1995.1008. [DOI] [Google Scholar]
- 10.DiFranza JR, Rigotti NA, McNeill AD, Ockene JK, Savageau JA, St Cyr D, et al. Initial symptoms of nicotine dependence in adolescents. Tob Control. 2000;9:313–9. doi: 10.1136/tc.9.3.313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.DiFranza JR, Savageau JA, Fletcher K, O’Loughlin J, Pbert L, Ockene JK, et al. Symptoms of tobacco dependence after brief intermittent use: the Development and Assessment of Nicotine Dependence in Youth-2 study. Arch Pediatr Adolesc Med. 2007;161:704–10. doi: 10.1001/archpedi.161.7.704. [DOI] [PubMed] [Google Scholar]
- 12.Preventing child maltreatment: a guide to taking action and generating evidence Geneva: World Health Organization and International Society for Prevention of Child Abuse and Neglect; 2006.