Abstract
Objective:
To describe the development process of a protocol for a fear of falling interdisciplinary intervention program based on the main factors associated with fear of falling.
Design/methods:
The process of developing a protocol consisted of defining the target population, selecting the initial assessment components, adapting the intervention program based on findings about fear of falling and restriction of activities in this population.
Settings:
University-affiliated outpatient vertigo, dizziness and falls clinic in coffee-growers zone of Colombian Andes Mountains.
Results:
An intervention program was developed based on three main falling conceptual models. A medical intervention, based on a biomedical and pathophysiological model, a physiotherapeutic intervention based on a postural control model and a psychological intervention based on a biological-behavioral model.
Conclusion:
This interdisciplinary fear of falling intervention program developed is based on particular characteristics of target population, with differences in the inclusion criteria and the program intervention components; with emphasis on medical (recurrent falls and dizziness evaluation and management), psychological (cognitive-behavioral therapy) and physiotherapeutic (balance and transfers training) components.
Keywords: fear of falling, elderly programs, Colombian, intervention
Introduction
Fear of falling is common among elderly people. It is reported both by those who have experienced a fall and by those who have no previous fall experience. Definitions of fear of falling vary according to a combination of postural control, cognitive and behavioral elements. The most accepted definition is a low perceived self-efficacy at avoiding falls during essential non-hazardous activities of daily living (ADL) (Tinetti et al 1990).
The prevalence of fear of falling is estimated to be between 12% and 65% in community-dwelling older adults who have not previously fallen and between 29% and 92% for those who have fallen, with women being disproportionately adversely affected (Jorstad et al 2005). Few studies have been conducted among the elderly in long term care. Prevalence estimates for this group are between 41% and 50% (Gagnon and Flint 2003). Studies conducted in Colombia (South America) report about 45%–82% of the elderly living in community experience at least some fear of falling and according to literature, it is increasing both for women and people in advanced age (Curcio et al 1998; Gomez and Curcio 2004).
Restriction of activity is a common consequence of fear of falling. Among community living elderly, in the prevalence of restriction of activity related to fear of falling is estimated to be between 20% and 55% (Wilson et al 2005). In Colombia, it is estimated to range between 20% and 47%, to be more common in women and to increase in older groups (Curcio and Gomez 2006a). A restriction of activities can become a downward trend which can adversely affect the health of the elderly. Fear of falling can lead to decreased physical activity, which leads to increased fragility and decreased functional ability, and thus to social isolation and decreased quality of life (Fletcher and Hirdes 2004; Delbaere et al 2004).
In the past two decades, several cross-sectional and a few prospective studies have identified multiple factors associated with fear of falling, including advance age, female gender, past history of falling, history of fall-related injury, frailty, gait or balance impairments, slow physical performance, activities of daily living (ADL) deficit, use of psychotropic drug, poor self-efficacy related to falls, two or more chronic diagnoses, chronic dizziness, visual problems, recent weight loss >5 lbs, depressed mood, self-perceived poor health, restricted social activities participation, decreased quality of life, decreased mobility and institutionalization (Evitt and Quigley 2004; Andresen et al 2006).
Effective interventions to lessen fear of falling could therefore have significant consequences for individuals, their families and healthcare delivery systems. Few programs have been developed to reduce fear of falling in older people. The majority these are based on physical activity programs, especially basic tai chi exercise forms, or are based in an educational program (Cameron et al 2000; Brouwer et al 2003; Wolf et al 2003). Other interventions have been based on cognitive-behavioral programs (Tennstedt 1998). A multi-factorial interdisciplinary intervention program could reduce fear of falling (Sattin et al 2005).
The aim of this paper is to describe the development process of a protocol for an interdisciplinary fear-of-falling intervention program, based in the main factors associated with fear of falling in Colombian Andes Mountains elderly people.
Methods
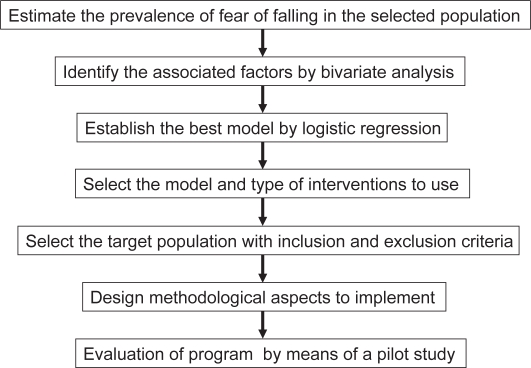
Identifying risk factors highlighted the need for a multi-factorial intervention program to avoid potential adverse consequences of fear-of-falling. It was decided that an intervention program should include components based on the particular characteristics of the target population. This approach was comprised of several activities that led to the preliminary version of the intervention program, as presented in Figure 1.
Figure 1.
The development process of a fear of falling intervention program.
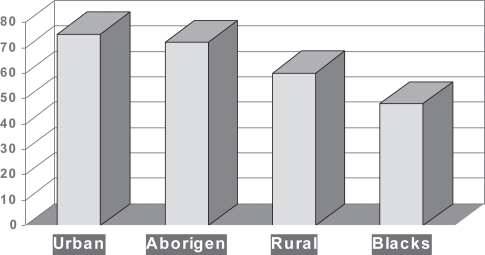
The first activity was to estimate the prevalence of fear of falling among the different groups (black, aboriginal, rural and urban groups) in the Andes Mountains coffee-grower population. With Colombia’s ethnic diversity, socioeconomic, geographical and topographical conditions, many different characteristics of aging could be identified (Gomez and Dulcey-Ruiz 1997). A single item asked, “In general, are you afraid of falling over?” (coding categories: not at all, a little, quite a bit, very much). The last two coding categories were combined for analysis. About activity restriction as consequence, specifically individuals were asked whether they limited going outdoors due to fear of falling (coding yes or not).
In order to examine the need to update the intervention with the main risk factors referred to above, we conducted a survey to find the factors most commonly associated with fear of falling. This was done by means of a randomized cross-sectional survey of 250 community inhabitants in Manizales, a 400,000 inhabitants-Colombian-Andes-Mountains city. The details of this study and the main variables covered by this study are described elsewhere (Curcio and Gomez 2006b). About self-perceived health, two questions were used, “Do you feel quite healthy? (coding yes or not) and “How would you evaluate your present health? (coding categories: very good, good, fairly, bad, very bad). The last two coding categories were combined for analysis as unhealthy feelings. Vision was evaluated by self-reported dichotomous scale, “Do you have difficulties in your vision?” An Spanish adapted form of the Barthel Index was used (Baztan et al 1993) and the assessment of physical performance included usual 6-meters-walking speed, ability to maintain balance for ten seconds in progressively more challenging positions (free position, feet side by side, semi-tandem and tandem), and Spanish adapted version of Tinetti’s performance oriented method assessment of balance and gait (Curcio, Gómez et al 2000).
In order to determine the appropriate eligibility criteria for participants in the program, inclusion and exclusion criteria from previous intervention programs were revised; the criteria were determined after comparing the profile of the elderly with fear of falling in the current study with profiles from other previous studies (Zijlstra et al 2005; Zijlstra et al 2006). Adaptations were made based on characteristics of the target population.
The next activity was the selection of the best components for an intervention program for this population. Intervention should be based on existing theoretical models that deal with instability, falls, near-falls and fear of falling in different settings. Three models were selected: A traditional biomedical and pathophysiological model (Studenski 1996), a postural control model based on a bio-mechanical model (Maki and McIlroy 1996) and a behavioral model (Peterson 2002).
Finally, a protocol for implementation was determined. The timeframe of the intervention, number of participants and other elements were based on previous exercise program experiences with the same population (Curcio, Franco et al 2000).
Results
The mean age of the sample was 74.1 (range 60–92, SD:7), 59% were female, and prevalence of fear of falling reported was 75.4% with half of them restricted their activities as consequence. It is higher in women than men and increase in older groups. This prevalence in urban elderly is higher than in subset elderly populations in coffee-growers Colombian Andes Mountains (Figure 2).
Figure 2.
Percentage of fear of falling in different subset elderly populations in coffee-growers region in Colombian Andes Mountains.
In bivariate analysis, several factors were found: age greater than 75 years, female gender, recurrent falls last year (2 or more), osteoarthritis, vertigo and dizziness (frequently or constantly), visual deficit, Mini-mental state examination (MMSE) score <23, subsyndromal depression (Geriatric depresion scale score >5), unhealthy feelings, poor self-perceived health, static balance and transfers impairments, decreased gait velocity (less than 0.64 mt/seg.) and gait deficits in Tinetti subscale. In multivariate analysis, by stepwise logistic regression, several factors were found associated with fear of falling in that population (as presented in the Table 1). With these both bivariate and multivariate risk factors associated with fear of falling the interdisciplinary intervention program was developed. As consequence, emphasis in medical, physiotherapy and psychological intervention was made. The contents of each discipline intervention are described in the appendix of this paper.
Table 1.
Logistic regression analysis for fear of falling in Andes Mountains elderly in Colombia
| Variable | Odds Ratio | 95% Confidence Interval |
|---|---|---|
| Age more than 75 years | 2.21 | (1.26–3.88) |
| Female gender | 4.48 | (2.49–5.10) |
| Osteoarthritis | 2.39 | (1.38–4.15) |
| Chronic dizzinessa | 2.20 | (1.23–3.96) |
| Visual deficit (self-perceived) | 2.28 | (1.32–3.94) |
| Transfers impairment (bed to sit)b | 3.03 | (1.31–3.03) |
| Unhealthy feelings | 2.17 | (1.25–3.76) |
| Depressionc | 2.12 | (1.07–4.23) |
3 months or later.
Barthel sub-scale.
Geriatric Depression Scale >5.
Medical aspects of this program were emphasized. It is essentially the biomedical and pathophysiological components of the protocol that permit identification and management of predisposing medical risk factors for falling. As a consequence, the medical intervention components selected were directed toward diagnosis and treatment of specific diseases, such as visual deficit, arthritis etc, with special emphasis on the assessment and treatment problems related to dizziness. Moreover, the management of anxiety and depression with both pharmacological and non-pharmacological treatments was integrated into the medical component of intervention program. As a consequence, the medical component is the main axis of the intervention program.
The functional ability component was selected with two objectives, one for increasing functional ability in physical and instrumental ADL (IADL) and another to obtain competent and safe performance. These components were directed toward adaptive and restorative rehabilitation with emphasis on balance and transfers training as well as advice on the appropriate use of assistive devices.
The only randomized trial specifically targeting fear of falling conducted by Tennstedt and colleagues focused on cognitive restructuring, or eliminating unrealistic concerns (Tennstedt 1998). As consequence, for the psychological intervention component, several session contents of ‘A Matter of Balance’ were adapted. This is a cognitive behavioral group intervention program, developed in the USA, designed to reduce fear of falling and promote physical, social and functional activity in elderly persons living in the community (Peterson 2002).
The inclusion criteria was based on results of the profile of elderly with fear of falling in that region such as a very old female with restriction of activities of daily living (physical and instrumental level), chronic dizziness and unhealthy perceived health, presence of depression symptoms, visual deficits and osteoarthritis that origin functional problems in activities of daily living (Table 2).
Table 2.
Target population of a fear of falling interdisciplinary intervention program
| Target population |
|---|
| Inclusion criteria |
| Reporting fear of falling with restriction of activities of daily living (physical and instrumental level) |
| Recurrent falls in the last year (2 or more) |
| Independently living in senior housing sites or in the community |
| Aged 65 and over with emphasis in old old people (80 and over) |
| Chronic dizziness and vertigoa |
| Exclusion criteria |
| Severe medical conditions |
| Unstable disability |
| Significant cognitive impairmentb |
| Confined to bed |
| Restricted by permanent use of wheelchair |
3 months or later.
Mini-Mental State Examination (MMSE) score <18.
Finally, a protocol for implementation was determined. The timeframe of the intervention, number of participants and other elements were based on previous exercise program experiences with the same population (Curcio, Franco et al 2000). Twelve group sessions constitute the intervention. Each session lasted 1 hour and sessions were held twice a week for a period of 4 weeks and once a week for a 2 week. On average, 10 people participate in each group. The early sessions focused on cognitive-behavioral intervention and solved medical problems identified on initial assessment. At the same time, physiotherapeutic intervention was initiated in order to solve problems identified in initial assessment, specially transfer problems and assistive devices adaptation. Each session were conducted by one physiotherapist and psychologist trained previously. Follow updates were scheduled with interdisciplinary reassessments each two weeks with group discussion about results.
Discussion
This program was developed for older persons living in the community who experience fear of falling and restrict their activities due to this fear of falling. In the process of developing this program, results of fear of falling among Andes Mountains inhabitants were obtained in order to better develop an intervention program adapted to the characteristics of this heterogeneous population. These characteristics include being a very old female, having chronic dizziness, poor perceived health (bad and very bad), presence of depression symptoms, visual deficits, osteoarthritis and transfers impairment. As consequence, emphasis on medical, physiotherapeutic and psychological interventions was made. The information collected indicated the existence of several medical, functional and psychological factors involved in the fear of falling in this population. Therefore, the intervention should be multi-factorial with major components in accordance with previous results (Tennstedt et al 1998; Zijlstra et al 2005; Zijlstra et al 2006).
Biomedical components of the intervention program are important to evaluate and implement, specially for women, because chronic diseases, functional limitations and disabilities occur more frequently among older women than among older men in Latino-American cities. Reyes-Ortiz, in a recent paper about falls among elderly persons in Latin America and the Caribbean, found that the main risk factors for falling are female gender, increased age, high depressive symptoms, and having any functional limitations and also included diseases such as diabetes, urinary incontinence and arthritis (Reyes-Ortiz et al 2005). Several of these risk factors were found both by bivariate and multivariate analysis in our target population and were included as intervention program components.
Functional evaluation and management of risk factors should be included in the intervention program, especially postural control assessment. Activities restriction, as a consequence of fear of falling, leads to deconditioning syndrome and functional impairment (Murphy et al 2002). Difficulties in instrumental ADL are among the first symptoms to appear in Latino-American older adults with chronic conditions (Menendez et al 2005). To prevent impairment caused by such difficulties was a main goal of our intervention program.
Depression was also an important risk factor to manage in this intervention program, as depressive symptoms are frequent among Latin-American elderly; women show higher percentages than men, partly because, in the region studied, women were more exposed to social and material disadvantages during their life course than men (Alvarado et al 2007). Furthermore, current socio-economic conditions and health status, as well as functional disabilities, account for much of the gender differences in depression (Zunzunegui et al 1998). In the current program, both pharmacological and non-pharmacological treatments of depression were included and carried out by all professionals in the interdisciplinary team.
With respect to inclusion criteria, several differences with other similar programs around the world can be identified (Tennstedt et al 1998; Zijlstra et al 2005, 2006). First, we excluded people who only reported fear of falling, without restriction of activities. Geographical difficulties related to the mountainous terrain is frequent in Colombia (altitude range between 1000 and 4000 mts.) and some fear of falling without restriction of activities could have a little protector effect as reported previously (Huang 2006). Second, a lower cut-off for the MMSE than the literature usually recommends is considered. An earlier report found that education, rurality and ethnicity contributed significantly to the variation in MMSE scores in an Hispanic elderly population (Mulgrew et al 1999). Similar conditions were also observed in the current sample.
In order to improve adherence and attendance rates, interventions components were designed feasible by most, allowing flexible time-frame, providing a comfortable environment and establishing a good relationship with family and caregivers, them are too invited to program sessions.
Conclusion
This paper describes the process of developing a interdisciplinary fear of falling and associated activities restriction intervention program for the elderly population in the Colombian Andes Mountains.
The results indicate that it is very important to select several conceptual models about instability and falls in order to decide which components to choose for an intervention program and before implementing it in different settings. By applying a systematic approach, as it was done in the present study, several characteristics of fear of falling in this population were identified and provided the basis for implementing an intervention program. Thus, an approach including several instability and falls models is better at the moment to initiate a fear of falling interdisciplinary intervention program. Our results lead us to conclude that the best model for our population integrates elements of a biomedical and pathophysiological model, elements of a postural control and bio-mechanical model and several components of a cognitive-behavioral model.
Recognizing the negative impact that fear of falling has on quality of life of many older adults we have begun a controlled trial to evaluate the efficacy of the final version of this interdisciplinary intervention program in different older populations in Andes Mountains in Colombia.
Appendix 1
Protocol of fear of falling interdisciplinary intervention program
Initial assessment
▪ Medical, psychological, social and functional diagnosis
▪ Visual acuity (Snellen scale)
▪ Falls, near-falls, injurious-falls presence and number
▪ Type of consequences of falling
▪ Fear of falling and activity restriction
▪ Performance based measures
▪ Quadriceps, gastrocnemios, gastrosoleos and hip muscles strength
▪ Assistive devices adaptation
▪ Propiocepción y palestesia
▪ Barthel scale for ADL
▪ Adapted Lawton scale for iADL
▪ Yesavage scale for depression (GDS)
▪ Anxiety scale (OMS)
▪ Self efficacy scale (Tinetti)
Steps of program
Interdisciplinary assessment based in main risk factors.
Interdisciplinary management plan was discussed.
Individual and group management plans were developed.
Follow updates were scheduled with interdisciplinary reassessments.
Interdisciplinary group discussion about results.
Medicine
Aim: Decreasing medical risk factors.
▪ Management of falling risk factors: visual deficit, arthritis etc.
▪ Assessment and treatment problems related with dizziness.
▪ Management of anxiety and depression.
▪ Preventing polipharmacy and drug reaction events.
▪ Management of orthostatic hypotension
▪ Patient and caregivers education.
Physiotherapy
Aim: Increasing functional ability in physical and instrumental ADL.
▪ Individualized and group-based interventions.
▪ Transfers training.
▪ Aerobic endurance, flexibility, strength, and balance training.
▪ Walking in extreme situations program (opened and closed eyes).
▪ Landing and standing strategies.
▪ Assistive devices adaptation.
▪ Health promotion and education in falling risk factors.
Psychology
Aim: Improving emotional functioning and adapting behavior change.
▪ Cognitive-behavioral therapy.
▪ Patient and caregiver training.
▪ Management of anxiety and depression.
Occupational therapy
Aim: Obtaining competent and safe performance.
▪ Adaptative rehabilitation in items of Self efficacy scale.
▪ Environmental risk assessment.
▪ Adaptative strategies in extreme situations.
Social work
Aim: Increasing social participation.
▪ Stimulating familiar activities and help support.
▪ Promoting social contacts and social participation.
▪ Case management as necessary.
▪ Patient and caregivers education.
Footnotes
This study was supported by a grant from Vicerrectoría de Investigaciones y Posgrados, Universidad de Caldas, Manizales, Colombia.
References
- Alvarado BE, Zunzunegui MV, Béland F, et al. Social and gender inequalities in depressive symptoms among urban elderly populations of Latin America and the Caribbean. Journal of Gerontology. 2007;62:S226–37. doi: 10.1093/geronb/62.4.s226. [DOI] [PubMed] [Google Scholar]
- Andresen EM, Wolinsky FD, Miller JP, et al. Cross-sectional and longitudinal risk factors for falls, fear of falling, and falls efficacy in a cohort of middle-aged African Americans. Gerontologist. 2006;46:249–57. doi: 10.1093/geront/46.2.249. [DOI] [PubMed] [Google Scholar]
- Baztán JJ, Perez de Molino J, Alarcón T, et al. Indice de Barthel: instrumento válido para la valoración funcional de pacientes con enfermedad cerebro vascular. Revista Española de Gerontología y Geriatría. 1993;28:32–40. [Google Scholar]
- Brouwer BJ, Walker C, Rydahl SJ, et al. Reducing fear of falling in seniors through education and activity programs: a randomized trial. Journal of American Geriatrics Society. 2003;51:829–34. doi: 10.1046/j.1365-2389.2003.51265.x. [DOI] [PubMed] [Google Scholar]
- Cameron ID, Stafford B, Cumming RG, et al. Hip protectors improve falls self-efficacy. Age and Ageing. 2000;29:57–62. doi: 10.1093/ageing/29.1.57. [DOI] [PubMed] [Google Scholar]
- Curcio CL, Franco M, Gómez JF. Effects of exercise program in physical ability in Colombian rural elderly. First International Conference Rural Aging. A Global Challenge; Charleston West Virginia, USA. 2000. p. 110. Book of abstracts. [Google Scholar]
- Curcio CL, Gomez JF. Restriction d′activité reliée á la peur de tomber chez les ágees de la région caféière colombienne. Canadian Journal on Aging. 2006a;25(Suppl 1):147–8. [Google Scholar]
- Curcio CL, Gómez JF. Factores predictores de temor a caer. Revista de la Asociación Colombiana de Gerontologia y Geriatria. 2006b;20:959–70. [Google Scholar]
- Curcio CL, Gómez JF, Galeano IC. Validez y reproducibilidad de las medidas basadas en la ejecución. Revista Española de Gerontología y Geriatría. 2000;35:82–8. [Google Scholar]
- Curcio CL, Gómez JF, García A. Caídas y capacidad funcional entre ancianos colombianos que realizan y no realizan ejercicio. Colombia Medica. 1998;29:125–8. [Google Scholar]
- Delbaere K, Kombez G, Vanderstraeten G, et al. Fear-related avoidance of activities, falls and physical frailty. A prospective community-based cohort study. Age and Aging. 2004;33:368–73. doi: 10.1093/ageing/afh106. [DOI] [PubMed] [Google Scholar]
- Evitt CP, Quigley PA. Fear of falling in older adults: a guide to its prevalence, risk factors, and consequences. Rehabilitation Nursing. 2004;29:207–10. [PubMed] [Google Scholar]
- Fletcher PC, Hirdes JP. Restriction in activity associated with fear of falling among community-based seniors using home care services. Age and Aging. 2004;33:273–9. doi: 10.1093/ageing/afh077. [DOI] [PubMed] [Google Scholar]
- Gagnon N, Flint A. Fear of falling in the elderly. Geriatrics and Aging. 2003;6:15–17. [Google Scholar]
- Gomez JF, Dulcey Ruiz E. Colombian gerontology scope. XVI World Congress of Gerontology. Adelaide, Australia: 1997. p. 263. Book of abstracts. [Google Scholar]
- Gomez JF, Curcio CL. Cuadernos de Investigación No. 3. Manizales: Universidad de Caldas; 2004. Envejecimiento rural: El anciano en las zonas cafeteras colombianas. [Google Scholar]
- Huang TT. Geriatric fear of falling measure: development and psychometric testing. International Journal of Nursing Studies. 2006;43:357–65. doi: 10.1016/j.ijnurstu.2005.04.006. [DOI] [PubMed] [Google Scholar]
- Jorstad E, Hauer K, Becker C. Measuring of psychological outcomes of falling: a systematic review. Journal of American Geriatrics Society. 2005;53:501–10. doi: 10.1111/j.1532-5415.2005.53172.x. [DOI] [PubMed] [Google Scholar]
- Maki BE, McIlroy WE. Postural control in the older adult. Clinics in Geriatric Medicine. 1996;12:635–58. [PubMed] [Google Scholar]
- Menéndez J, Guevara A, Arcia N. Enfermedades crónicas y limitación funcional en adultos mayores: estudio comparativo en siete ciudades de América Latina y el Caribe. Revista Panamericana de Salud Pública. 2005;17:353–61. doi: 10.1590/s1020-49892005000500007. [DOI] [PubMed] [Google Scholar]
- Mulgrew CL, Morgnestern NE, Shetterly SM, et al. Cognitive functioning and impairment among rural elderly Hispanics and non-Hispanic whites as assessed by the Mini-Mental State Examination. Journal of Gerontology: Psychological Sciences. 1999;54:P223–30. doi: 10.1093/geronb/54b.4.p223. [DOI] [PubMed] [Google Scholar]
- Murphy SL, Williams CS, Gill TM. Characteristics associated with fear of falling and activity restriction in community-living older persons. Journal of American Geriatrics Society. 2002;50:516–20. doi: 10.1046/j.1532-5415.2002.50119.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peterson EW. –2003. Using cognitive behavioral strategies to reduce fear of falling: A Matter of Balance. Generations. 2002;24:53–9. [Google Scholar]
- Reyes-Ortiz CA, Al Snih S, Markides KS. Falls among elderly persons in Latin America and the Caribbean and among elderly Mexican-Americans. Revista Panamericana de Salud Publica. 2005;17:362–9. doi: 10.1590/s1020-49892005000500008. [DOI] [PubMed] [Google Scholar]
- Sattin RW, Easley KA, Wolf SL. Reduction in fear of falling through intense tai Chi exercise training in older, transitionally adults. Journal of American Geriatrics Society. 2005;53:1168–78. doi: 10.1111/j.1532-5415.2005.53375.x. [DOI] [PubMed] [Google Scholar]
- Studenski S. Clinical overview of instability in the elderly. Clinics in Geriatric Medicine. 1996;12:679–88. [PubMed] [Google Scholar]
- Tennstedt S, Howland J, Lachman M, et al. A randomized, controlled trial of a group intervention to reduce fear of falling and associated activity restriction in older adults. Journal of Gerontology: Psychological Sciences. 1998;53:P384–92. doi: 10.1093/geronb/53b.6.p384. [DOI] [PubMed] [Google Scholar]
- Tinetti M, Richman D, Powel L. Falls efficacy as a measure of fear of falling. Journal of Gerontology: Psychological Sciences. 1990;45:P239–41. doi: 10.1093/geronj/45.6.p239. [DOI] [PubMed] [Google Scholar]
- Wilson MM, Miller D, Andrese E. Fear of falling and related activity restriction among middle-aged African American. Journal of Gerontology: Medical Sciences. 2005;60:M355–60. doi: 10.1093/gerona/60.3.355. [DOI] [PubMed] [Google Scholar]
- Wolf SL, Sattin RW, Kutner M, et al. Intense Tai Chi exercise training and fall occurrences in older, transitionally frail adults: a randomized, controlled trial. Journal of American Geriatrics Society. 2003;51:1693–701. doi: 10.1046/j.1532-5415.2003.51552.x. [DOI] [PubMed] [Google Scholar]
- Zijlstra GARR, Tennsted S, Van Haastregt JCM, et al. Reducing fear of falling and avoidance of activity in elderly persons: The development of a Dutch version o an American intervention. Patient Education and Counseling. 2006;62:220–7. doi: 10.1016/j.pec.2005.07.005. [DOI] [PubMed] [Google Scholar]
- Zijlstra GARR, Van Haastregt JCM, Van Eijk JThMgt JCM, et al. Study protocol. Evaluating an intervention to reduce fear of falling and associated activity restriction in elderly persons: design of a randomized controlled trial. BMC Public Health. 2005;5:26. doi: 10.1186/1471-2458-5-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zunzunegui MV, Béland F, Llacer A, et al. Gender differences in depressive symptoms among Spanish elderly. Social Psychiatry and Psychiatric Epidemiology. 1998;33:195–205. doi: 10.1007/s001270050043. [DOI] [PubMed] [Google Scholar]