Abstract
Introduction
Morning report is a traditional core teaching session in most departments of internal medicine where learners present cases to a facilitator who uses the material to teach clinical reasoning. It instills fear in both learners and teachers because they may embarrassingly miss diagnostic possibilities including even the actual diagnosis.
Aim
The two teaching tips described here enable the learner and the teacher to fall back on a routine approach to arriving at a differential diagnosis list.
Description
The first tip describes how to elicit the ten “focal findings” in the case that best summarize the data used to derive a diagnosis list. The second tip describes a matrix of etiologies and systems that can be used to generate the diagnostic probabilities.
Discussion
This approach is easy to teach and, where all else fails when coming up with a diagnosis, can be used to prompt the discussion of what is wrong with the patient.
KEY WORDS: diagnostic reasoning, morning report, analytic approach
INTRODUCTION
For decades morning report has been a core educational activity. The format varies but usually consists of a group of medical students and residents (i.e. the "learners") sitting around a table with a faculty member or chief resident (i.e. the "teacher") functioning as facilitator. One or more patients from a general internal medicine inpatient team are presented and the teacher uses the case as an opportunity to elucidate aspects of clinical reasoning. In the course of doing so, the teacher frequently asks specific questions about aspects of the case such as: “What are three reasons why alcoholics present with a low platelet count?” or “What is your approach to a patient who presents with a low hemoglobin?” In some cases, these questions reflect the comfort zone of the teacher and have limited relevance to the case, a practice which came to be known as "pimping"1,2. For learners, this process may instill fear because they are asked to perform academically in front of their colleagues. As a result, morning report can either be embarrassing, when learners have no idea how to answer a question, or exhilarating, when they do.
A well kept secret amongst faculty members is that they too are terrified of morning report. They believe that learners think that they know all the answers and are embarrassed when they miss diagnostic possibilities or have nothing to teach because of limitations in their knowledge. This is particularly true of subspecialists who may be presented a case in an area far away from their regular clinical practice.
Learners are at an obvious disadvantage in morning report due of their lack of experience. Teachers often use their breadth of personal experiences to generate differential diagnoses in a non-analytical fashion known as "pattern recognition".3,4 It is well known, however, that pattern recognition often predisposes the diagnostician to premature closure of the differential diagnosis and results in missing important possibilities.3–5 Some have proposed the use of structured analytical approaches to generating differential diagnoses in order to avoid embarrassing oversights.6
In this paper, we propose a hybrid analytical approach that can be easily learned, easily taught, and widely applied to differential diagnosis, both in the work-up of individual patients and at teaching events such as morning report. There are two components to this process. The first selects key pieces of information we refer to as "focal findings" from a typical case report. The second applies the findings generated in the first tip to a conceptual matrix which is a hybrid of etiologies and systems based approaches (the “hybrid matrix”). Together, these two components provide an analytical approach that is straightforward, easy to remember, and effective. In this paper, we use the example of a typical morning report case in order to present these two teaching tips.
TEACHING TIP 1: ORGANIZING THE CASE AND IDENTIFYING FOCAL FINDINGS
Learning Aims
The first tip involves identifying the key pieces of information contained in a case. This requires an organized framework to quickly select focal findings which will serve as “sign posts” in the diagnostic process. The objective of this tip is to provide an approach to identifying focal findings in a typical morning report and to effectively teach this approach to learners while performing it. The specific learning objectives for this tip include:
Learning criteria to quickly assess and flag important case points as focal findings.
Learning techniques for teaching these criteria to learners.
Preparing to Teach
The first component of this technique does not require any advanced preparation. It is designed to be used in a standard morning report with the teacher listening to the presentation of a case. It may be helpful to provide learners with a summary card that can be used for reference while learning and later applying this technique (Appendix 1).
Teaching Script
Begin by asking one of your learners to present the case. Record all points of the case regardless of relevance on a white board. Now that all of the facts of the case are visibly written, ask the audience to participate in choosing which facts constitute focal findings that will expand or limit the diagnostic possibilities. These key facts should expand or narrow diagnostic possibilities, not be redundant with previously selected points and in general be limited to 10 or fewer focal findings, to ensure that only key findings are considered. Any aspect of the presentation can be a focal finding (age and sex are usually the first), including the chief complaint, demographic data, elements of the history of present illness, past medical conditions, medications, genetic or social risk factors, or pertinent physical examination and lab findings (see Appendix 1 for specific criteria).
Once the concept of what constitutes a focal finding has been explained, offer your learners the opportunity to identify the focal findings for this case from the points written by you on the board. As the focal findings are being identified, circle or underline and number them on the white board using a different color and offer your comments regarding their choice. The goal of this process will be to identify the ten focal findings (some findings are grouped together) that best summarize the case in a way that leads to an appropriate differential diagnosis list.
The following case description, key points, and associated justification are intended to give a practical example of how to employ the above tip. We have highlighted the key focal findings from this case.
“A 75-year-old man presents to the ER with a 1-week history of dizziness#1. His past medical history includes atrial fibrillation, CAD, DM, diverticulosis, asthma#2, severe osteoarthritis limiting his mobility and BPH. His medications include Coumadin, glyburide, hydrochlorothiazide, and tamsulosin (which was recently increased) #3. He has an allergy to penicillin resulting in a rash. He has a 30-pack-year smoking history#4 and quit 5 years ago. He consumes three servings of alcohol daily, but no recreational drugs or herbal remedies. He has a family history of both myocardial infarction and colon cancer in his father#5 at age 70. He began experiencing episodes of dizziness and unsteadiness one week ago#6, each lasting several minutes and occurring 4–6 times daily. The patient cannot recall any specific trigger for the onset of the events but notes that they are associated with palpitations and dyspnea#7. He denies any other cardiac, neurological, respiratory or constitutional symptoms. On physical examination, the patient was mildly hypotensive#8 and had an irregular cardiac rhythm but the cardiovascular, respiratory, abdominal and neurological examinations were otherwise normal. General laboratory investigations were significant only for a mild microcytic anemia#9 compared with previous blood work. His electrocardiogram (EKG) showed frequent atrial premature beats#10.”
Applying the previously described standards for identifying focal findings to this case description (Appendix 1), several focal findings can be readily identified. First, the patient’s chief complaint of dizziness is an essential starting point diagnostically and will be expanded on in the history of present illness. Next, the patient’s age increases the likelihood of cardiovascular causes of dizziness and other etiologies common in the elderly. The various elements of the patient’s past medical history serve to broaden the differential diagnosis to include cardiovascular disease (CAD, DM, smoking history), stroke/TIA (atrial fibrillation), or anemia (diverticulosis). The patient’s medications also present several diagnostic possibilities including hyponatremia (hydrochlorothiazide), hypoglycemia (glyburide), hypotension (tamsulosin) and GI bleed (Coumadin). Family history raises the possibility of cardiovascular or neoplastic disease. The description of the episodes in the history of present illness is more consistent with presyncope than vertigo and thus greatly affects our differential as does the fact that these episodes appear to be acute in onset. The associated symptoms of dyspnea and palpitations along with the EKG findings raise the possibility of arrhythmia or even a respiratory etiology. Lastly, the physical and laboratory findings serve to encourage the learners to look more closely at potential causes of anemia and hypotension when considering their differential.
Rationale
This technique helps both teachers and learners sort through the deluge of information presented in a typical case and identify essential diagnostic points. Helping learners discern the important findings promotes a broader differential by precluding focus on only one or a handful of findings. Applying this technique also affords both the teacher and learner a “breathing space” during which they can reflect and have time to generate a broader differential. Ultimately, these findings will be employed to complete the hybrid matrix (the next tip) and generate a broad differential diagnosis.
TEACHING TIP 2: THE HYBRID MATRIX TABLE
Learning Aims
This method involves using a hybrid matrix: a table with an etiological differential forming the columns of the table and body systems comprising the rows. Once constructed, the table can be used to incorporate the focal findings identified in the previous tip to generate a broad differential. While this is being done in the context of morning report, it can be readily applied to other clinical teaching situations.
Preparing to Teach
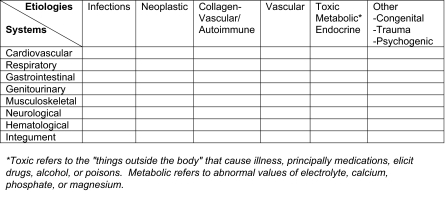
Construct a 6 × 8 table with possible etiologies listed along the columns and body systems along the rows (Table 1). It is helpful to construct this table beforehand on the whiteboard or a large flip chart in order to save time. Distributing a summary card with a sample matrix to learners facilitates their learning and subsequent application of the technique by providing a quick reference (Appendix 1).
Table 1.
Hybrid Matrix Table
Teaching Script
Start with the hybrid matrix on the white board as depicted in Table 1. Reflect on the focal findings identified in the previous step. Now orient your learners to the matrix and its two axes. Ask the learners to identify boxes that should be filled in based on the focal findings. Fill in these boxes if the justification is appropriate. Review unfilled boxes and ensure that they do not represent diagnostic possibilities based on the key case points. Review each focal finding to see if it is accounted for by at least one diagnosis in the matrix. The completed table readily allows the generation of a differential diagnosis. This differential can then be narrowed based on additional information that was not initially presented (e.g. the results of additional tests or procedures that clinched the diagnoses such as biopsy or angiogram).
In Table 2 we show a completed matrix based on the case described previously and also provide the subsequent differential diagnosis. The diagnostic possibilities have been graphically laid out and no important area has escaped consideration. The patient in this instance was ultimately found to be experiencing episodes of presyncope due to medication induced hypotension which resolved once his Tamsulosin was reduced. Gastrointestinal blood loss was ruled out by upper and lower endoscopy.
Table 2.
Completed Matrix Example
Rationale
This method allows broad diagnostic possibilities to be generated and combines systems and etiology based approaches to the differential diagnosis. It is easy to use and can be readily taught. This technique is very visual, which allows it to avoid the common criticism that analytic techniques are cumbersome and impractical. It also avoids premature closure of the differential diagnosis; the primary flaw of utilizing intuitive non-analytic approaches. Lastly, it provides a safe framework for discussion and can help promote presentation of unknown cases, even when both the learner and teacher are confused by the patient’s presentation.
Acknowledgments
Conflict of Interest None disclosed.
APPENDIX 1: QUICK REFERENCE CARD
STEP 1: Identify Focal Findings
Three criteria:
This point adds or eliminates a diagnostic possibility.
This point’s diagnostic contribution has not been made by a previous one.
In general, no more than ten (10) focal findings should be selected per case.
These focal findings should also fall into one of the following categories:
The chief complaint.
Demographic data that will introduce, eliminate, or change the likelihood of different diagnoses.
Past medical conditions or medications that may primarily or secondarily produce the chief complaint described by the patient.
Elements of the history of present illness that influence the diagnostic possibilities such as temporal course and prominent symptoms.
Genetic and social risk factors that are related to a disease process that could produce the presentation described in the case.
Pertinent positives and negatives on physical examination and lab.
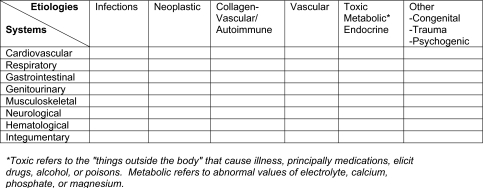
STEP 2: Review and Complete Hybrid Matrix
In Table 3 we show a blank hybrid matrix matrix.
Table 3.
Hybrid Matrix Blank
References
- 1.Brancati FL. The Art of Pimping. JAMA. 7 July 1989; 2621: 89–90. [PubMed]
- 2.Detsky AS. The Art of Pimping. JAMA in press. 1 April 2009. [DOI] [PubMed]
- 3.Charlin B, Boshuizen HP, Custers EJ, Feltovich PJ. Scripts and clinical reasoning. Med Educ. 2007 Dec; 4112: 1178–84. [DOI] [PubMed]
- 4.Eva K. What every teacher needs to know about clinical reasoning. Med Educ. 2004 Jan; 391: 98–106. [DOI] [PubMed]
- 5.Bowen J. Educational strategies to promote clinical and diagnostic reasoning. N Engl J Med. 2006 Nov 23; 35521: 2217–25. [DOI] [PubMed]
- 6.Eva KW. The ageing physician: changes in cognitive processing and their impact on medical practice. Acad Med. 2002; 77(Suppl): 1–6. [DOI] [PubMed]