Abstract
Background
The purpose of this study was to report the effect of combining the Kestenbaum procedure with posterior fixation suture for infantile horizontal nystagmus with anomalous head posture (AHP) in children.
Methods
Nine consecutive patients who underwent combined Kestenbaum procedure plus posterior fixation suture to the recessed muscles at the same time were retrospectively studied. All patients were orthotropic before surgery and were followed for at least 6 months. Pre- and postoperative AHP and binocular corrected visual acuity (BCVA), and ocular alignment were assessed.
Results
Mean age at surgery was 4.8 ± 1.5 years. The average follow-up was 29.7 months. The average head turn preoperatively was 27.4° and postoperatively 7.2°. The average net change in AHP was 24.8° (P = 0.008). Seven of 9 patients (78%) achieved a residual head turn of 10° or less. The average Log Mar BCVA was 0.33 preoperatively and 0.31 postoperatively (P = 0.68). Only 1 patient needed additional surgery for residual horizontal AHP. No patient developed strabismus.
Conclusion
Combined Kestenbaum procedure with posterior fixation suture was an effective and stable procedure in reducing AHP of the range of 20° to 35° in children with infantile nystagmus.
Keywords: Infantile nystagmus, Anomalous head posture, Kestenbaum procedure, Posterior fixation suture
Introduction
Infantile nystagmus (IN) is an involuntary, oscillatory eye movement disorder of unknown etiology. IN may result from a motor defect in the efferent pathways in otherwise normal children and occur in association with congenital or acquired visual sensory system deficit. Often it has a null point or neutral zone, the range of gaze angles where the intensity is minimal, producing better visual acuity. Patients with an eccentric null zone will usually develop a compensatory anomalous head posture (AHP) to minimize the intensity of the nystagmus and thereby gain optimal visual acuity.
The surgical correction of AHP in IN began with the independent reports of Anderson [1], Goto [10], and Kestenbaum [13] in the early 1950s. These shift the eyes in the direction of head turn and away from the preferred direction of gaze. Anderson proposed recessing the agonist of the head turn on each eye and Goto resected the antagonist muscle of each eye. Kestenbaum advocated a combined and equal two-staged recession/resection of all four horizontal rectus muscles. In 1973, Parks developed the 5-6-7-8 guidelines with a total of 13 mm of surgery performed on each eye, 5 mm recession of the medial rectus and 8 mm resection of lateral rectus muscle for the eye in adduction, and 6 mm resection of medial rectus muscle and 7 mm recession of lateral rectus muscle of the fellow eye. This recommendation was based on a medial rectus recession of 5 mm which, at that time, was considered the largest amount that could be accepted to preserve full ductions [21]. The long term results of this surgery were variable, as many patients, at least partially readopted AHP after surgery. To enhance the effect and reduce the recurrence of AHP, modification or augmentations of Parks’ dosage were reported by Calhoun and Harley [5], Nelson et al [19], and others for larger degrees of AHP [15–17, 22, 23, 26, 28]. De Decker proposed an equatorial recession of the involved horizontal rectus muscles [9]. Gräf [12] performed Kestenbaum with artificial divergence surgery (recess-resect surgery on adducted eye) when convergence is effective but does not sufficiently correct AHP. Even with these modifications or augmentations of the amount of surgery, high rates of recurrence and undercorrection of head turns were reported with long term follow-up. In addition, larger augmented surgery resulted in possible motility limitations or secondary misalignment after operation.
After the description by Cüppers [7], Faden-operation (posterior fixation suture) has been commonly used to correct incomitant strabismus. This selectively weakens maximal ocular rotation in its field of action with little effect on other gaze positions. In nystagmus this technique was first proposed by Arruga [2] to dampen eye movements by suturing all four horizontal rectus muscles in case of severe retinal detachment with gross nystagmus. Muhlendyck [18] also used this technique as an immobilization surgery. For AHP in nystagmus, this technique has been used in conjunction with the traditional Kestenbaum procedure as a two stage approach in European literature [4, 27], but no long-term results were reported.
The purpose of this study was to evaluate outcomes of combining the Kestenbaum procedure and posterior fixation suture at the same time on head posture, visual acuity, and ocular deviation for the treatment of infantile horizontal nystagmus with a moderate AHP. The use of posterior fixation suture might result in better postoperative versions by requiring lesser amounts of recession and resection to achieve a specific amount of head turn correction.
Subjects and methods
A retrospective charts review of 9 consecutive patients who underwent combined Kestenbaum procedure plus posterior fixation suture to the recessed muscles at the same time for anomalous head posture (AHP) secondary to infantile horizontal nystagmus were performed. The surgeries were conducted at the Jules Stein Eye Institute, UCLA School of Medicine (Los Angeles, CA) by the same surgeon (S.J.I) over a ten year period from July 1995 to June 2005.
All patients were orthotropic before the nystagmus surgery and were followed at least 6 months. None had prior nystagmus surgery. One patient had a previous recession of both medial rectus muscles for infantile esotropia. Complete ophthalmologic examinations including measurement of binocular alignment using a prism cover test, and dilated fundus examination were performed. The nystagmus pattern in all fields of gaze was also evaluated, but an electronystagmogram (ENG) was not performed for this study. Pre-and postoperative AHP was measured in degrees with a goniometer while the patient was fixating with both eyes open on the smallest visual acuity line that could be read at 6 meters. The AHP was recorded in the vertical, sagittal and the horizontal axes. Binocular corrected visual acuity (BCVA) was measured with refraction in place using Snellen optotypes at 6 meters in the preferred head position preoperatively and in forced primary position postoperatively. Visual acuity measurements were converted to the log of the minimum angle of resolution (LogMar) for statistical analysis.
All patients underwent a similar surgical procedure under general anesthesia by one of authors (S.J.I.). The indication for surgery was an abnormal head turn of 20° or more. The procedure consisted of a combination of a Kestenbaum procedure (bilateral recession and resection) plus Faden-operation (posterior fixation suture) to the recessed muscles at the same time. The amount of Kestenbaum procedure was decided according to the degrees of head turn using the modified “classic plus one” method. Larger amounts of recession and resection were used for larger AHP (Table 2). The most common surgical dosage was to recess one medial rectus muscle 6.0 mm, resect the ipsilateral lateral rectus muscle 7.0 mm, recess the contralateral lateral rectus muscle 8.0 mm and resect the remaining medial rectus muscle 6.0 mm. The posterior fixation suture was placed at 11 mm from the original insertion line for recessed medial rectus muscles and 13 mm from the original insertion line for recessed lateral rectus muscle. Nonabsorbable sutures were placed as two scleral bites about 3 mm long and emerging about 5 mm apart, incorporating the upper and lower one-third of the muscle width.
Table 2.
Results of Kestenbaum with Posterior fixation suture (PFS)
| Patient | Surgery (mm) | Residual AHP (deg) after first surgery | Follow-up (mo) |
|---|---|---|---|
| 1 | RLR rc 8 PFS, RMR rs 6, LMR rc6 PFS LLR rs 7 | R12 | 9 |
| 2 | RLR rc 8 PFS, RMR rs 6, LMR rc6 PFS, LLR rs 7 | L4, LT15 | 6 |
| 3 | LLR rc 8.5 PFS, LMR rs 7, RMR rc6 PFS, RLR rs8 | R20 | 66 |
| 4 | LLR rc 9 PFS, LMR rs 8, RMR rc 6 PFS, RLR rs 7 (with all half tendon width infraplacement) | R3, CU25 | 72 |
| 5 | LLR rc 8 PFS, LMR rs 7, RMR rc 5.5 PFS, RLR rs 7 | 0 | 29 |
| 6 | RLR rc 9 PFS, RMR rs 7, LMR rc 6 PFS, LLR rs 7 | L7 | 6 |
| 7 | LLR rc 7 PFS, LMR rs 6, RMR rc 5.5 PFS, RLR rs 7 | L8 | 12 |
| 8 | LLR rc 9 PFS, LMR rs 7.5, RMR rc 6 PFS, RLR rs 8 | R21 | 36 |
| 9 | LLR rc 9 PFS, LMR rs 8, RMR rc 6 PFS, RLR rs 7 | 0 | 6 |
rc=recession, rs=resection, RLR=right lateral rectus muscle, RMR=right medial rectus muscle, LLR=left lateral rectus muscle, LMR=left medial rectus muscle, R=right head turn, L=left head turn, LT=left tilt, CU=chin up, AHP=anomalous head posture, deg=degrees.
Changes in abnormal head posture, binocular corrected visual acuity, ocular alignment and limitation of eye movements were assessed. The reduction of ocular movements was assessed using the method described by Clark and Isenberg [6]. The patients were examined one day, seven days and one month after the surgery and then every 3 months thereafter or as needed. Postoperative results utilized in this study were obtained from the last examination. A successful outcome was defined as a clinically manifest head turn 10° or less at distance fixation. Statistical analysis was performed using Wilcoxon signed rank test (SPSS Inc., Chicago, IL; 2005) and p values less than 0.05 were considered statistically significant.
Results
Nine patients with typical clinically diagnosed infantile nystagmus were analyzed. The age when first examined ranged from 3 months to 6 years, with an average of 28.3 months. The mean (±SD, standard deviation) age at the initial surgery was 4.8 ± 1.5 years (range 3–7). Six (56%) were female. The mean postoperative follow-up time was 29.7 months (range 6–82). All subjects had horizontal nystagmus and 67% had jerk nystagmus. Two patients had sensory nystagmus and 3 patients showed an additional cyclovertical anomalous head posture (AHP) pre-operatively. The clinical characteristics are summarized in Table 1.
Table 1.
Clinical characteristic of patients
| Patient | Sex | Age (yrs) | Diagnosis | AHP (deg) | Tilt/Chin (deg) | Prior Surgery |
|---|---|---|---|---|---|---|
| 1 | F | 7 | Oculomotor N | L25 | – | none |
| 2 | M | 4.5 | Infantile N, Foveal hypoplasia | L25 | LT7 | none |
| 3 | M | 3.5 | Oculomotor N | R32 | – | none |
| 4 | F | 3.5 | Congenital N | R35 | CD5 | none |
| 5 | F | 3 | Oculomotor N | R25 | – | none |
| 6 | F | 6.5 | Infantile N | L20 | – | aBMRrc |
| 7 | M | 5 | Septooptic dysplasia, ON hypoplasia | R20 | – | none |
| 8 | F | 4 | Infantilel N | R30 | – | none |
| 9 | M | 7 | Infantile N | R35 | LT7 | none |
N=nystagmus, L=left head turn, R=right head turn, LT=left head tilt, CD=chin down, ON=optic nerve, BMR=bilateral medial rectus muscle, rc=recession, AHP=anomalous head posture, deg=degrees.
aThis surgery was done for infantile esotropia in this patient.
Table 2 details the surgical amounts, residual head turn after initial surgery and follow-up period. All patients showed improvement of head turn after initial surgery. Two patients needed a further operation. Patient 3 showed a residual right head turn of 13° at 6 months after surgery but it slowly increased after two years to 20°, so further surgery was done after 66 months. After the second surgery, the final residual head turn was under 10° after 16 months of further follow-up. In patient 4, due to a chin down posture, a half tendon width infraplacement of all the horizontal rectus muscles was performed at the same time. After the initial surgery the head turn was improved but she showed a marked chin up posture. She underwent surgery for the vertical anomalous head posture 72 months following her initial surgery (Table 3).
Table 3.
Summaries for 2 re-operated patients
| Patient | Age | AHP | Additional Surgery | Follow-Up | |
|---|---|---|---|---|---|
| bPre-op | Post-op (mm) | ||||
| (yr) | (deg) | (mm) | (mo) | ||
| 3 | 6 | R20 | R10 | LLR re-rc 1.5, LMR rs 3, RMR re-rc 2, RLR rs 3 | 16 |
| 4 | 9 | R5 | R3 | LSR rc 5, LIO AT | 9 |
| CU25 | CU15 | ||||
AHP=abnormal head posture, R=right head turn, CD=chin down, CU, =chin up, LLR=left lateral rectus muscle, LMR=left medial rectus muscle, RMR, right medial rectus muscle, RLR=right lateral rectus muscle, LSR=left superior rectus muscle, LIO=left inferior rectus muscle, rc=recession, rs=resection, AT=anteriorization.
bpre-op means before the second surgery.
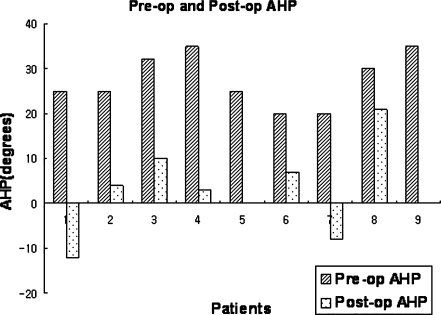
The mean preoperative head turn was 27.4 ± 5.8° (range 20–35) with mean postoperative head turn of 7.2 ± 6.6° (range −8 to 10,” -“indicates the opposite head direction). The average net change in AHP was 24.8 ± 9.6° (Wilcoxon signed rank test: P = 0.008). All patients had improvement in their anomalous head turn after surgery and seven of 9 patients (78%) achieved a residual head turn of 10° or less (Fig. 1).
Fig. 1.
Changes of AHP (anomalous head posture) after operation in each patient. Negative numbers represent the opposite head direction (overcorrection). 0 means a straight head position. The mean AHP improved significantly after surgery (P = 0.008)
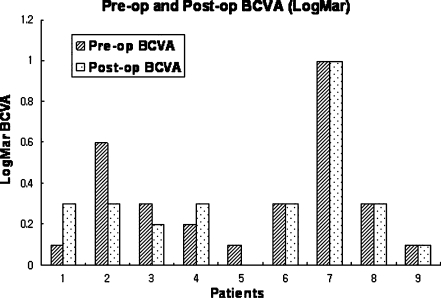
The average preoperative LogMar BCVA (binocular corrected visual acuity) in the preferred head position was 0.33 ± 0.29 preoperatively and 0.31 ± 0.28 postoperatively in primary position. The improvement in BCVA was not statistically significant (Wilcoxon signed rank test: P = 0.68). Three patients (33.3%) showed an improvement of at least one Snellen line. Figure 2 demonstrates the absolute change in LogMar BCVA of each patient after surgery.
Fig. 2.
Changes of BCVA (Binocular corrected visual acuity) after operation. Preoperative BCVA was measured in preferred head posture and postoperative BCVA in primary position. The improvement of BCVA after surgery was insignificant (P = 0.68)
Only three patients (patient 1, 2, and 3) had postoperative limitation of horizontal movements in the direction of muscle recession with posterior fixation. The loss of adduction was between zero and 10° and the decrease in abduction was between zero and 38°. Subsequent strabismus was not observed in any patient during follow-up period.
Two patients developed an overcorrection of the head turn, although the magnitude of the opposite turn, measuring 8° and 12°, was not sufficient to warrant further surgery.
Discussion
Attempts to eliminate anomalous head posture (AHP) in infantile nystagmus with eccentric null zone with various extraocular muscle surgeries have been tried, but the Kestenbaum procedure as modified by Parks [21] and others, is probably now the most commonly performed. In practice, this procedure not only shifts and broadens the null zone but can also decrease nystagmus outside the null zone [8].
Because of high rates of AHP recurrence or undercorrection, Parks’ modification was subsequently augmented. The amount of augmentation of previously reported studies was from 10% to 60% of Parks’ dosage and the success rates of these modifications varied between 50 to 100% [5, 15–18, 23, 24, 26,29] (Table 4). These augmentations increased the overall success rate, but inevitably led to a significant restriction of duction. Calhoun and Harley [5] proposed 40% augmentation and reported a 75% cure rate (no AHP) with a 75% incidence of mild gaze palsy after 5.8 months of follow-up. Nelson and coworkers [19] reported 40% augmentation for 30° face turn and 60% augmentation for 45° face turn, 53.3% were cured (no AHP), but majority of patients showed moderate restriction. Scott and Kraft [26] and Pratt-Johnson [23] also reported significant gaze restriction in some cases following augmented Parks’ operation. These results showed that the success rate of larger magnitude surgical correction was sometimes associated with restricted duction and gaze away from head turn. In contrary, some authors reported no limitation of duction after augmented surgery. Taylor [28] reported a larger 8–9 mm recession of lateral rectus muscle on the side of slow phase and a larger 6 mm resection of medial rectus of opposite eye in conjunction with smaller 6 mm resections of both respective antagonists. He reported 70% success rate and no limitation of eye movement over 17.8 months follow-up period. Mitchell et al [17] introduced a “plus one” operation (6-7-8-9) and even after the 40% to 60% augmentation surgery, they reported no duction limitation in any patients during 54 months of follow-up.
Table 4.
Reviews of major studies on Kestenbaum procedure for infantile nystagmus
| Authors | No. of Patients | Age at Surgery (yr) | Follow-Up(mo) | 10° or less residual AHP (%) | BCVA Improvement (%) |
|---|---|---|---|---|---|
| Parks [15] | 10 | 7.4 | 17 | 70 | – |
| Calhoun & Harley [5] | 19 | 8.5 | 13 | 32 | – |
| Taylor [21] | 10 | – | 17.8 | 70 | – |
| Sandall [18] | 7 | 12.5 | 100 | 14 | |
| Scott & Kraft [19] | 32 | 9.6 | 35 | 62.5 | 53.1 |
| Nelson et al [14] | 15 | 9.8 | 33 | 66.6 | – |
| Mitchell et al [12] | 38 | 7.5 | 54 | 50 | same or improved |
| Pratt-Johnson [17] | 16 | 11 | 32 | 56.3 | – |
| Kraft et al [10] | 20 | – | 6–40 | 75 | – |
| Zubcov et al [22] | 7 | 9.4 | 3 wks | 100 | 14 |
| Lee et al [11] | 63 | 10.3 | 13 | 89 | – |
| Kang & Isenberg | 9 | 4.8 | 29.7 | 78 | 33.3 |
AHP=anomalous head posture, BCVA=binocular corrected visual acuity.
–=unavailable data.
We intended to study the effect of our nystagmus surgery on head turn. The amount of AHP in our patients ranged from 20 to 35 degrees. We generally used the amount of Kestenbaum procedure “classic plus one” (6-7-8-9) [17], and placed posterior fixation sutures for additional AHP correction (Table 2). The use of posterior fixation suture allows weakening in the field of action of a given muscles and at the same time maintaining the primary position alignment. This can potentially correct more AHP than the usual Kestenbaum procedure without marked limitation of ocular movements. Seventy-eight percents of our patients achieved 10° or less residual AHP supporting this combined technique as effective for nystagmus with moderate head turn (20° to 35°) (Table 4). The main risks of posterior fixation suture are scleral perforation and difficult re-operation due to adhesion of the back muscle surface to the sclera.
The surgical technique we employed is a modification of the Faden-operation technique described by Bérard et al [4] and Spielmann [27] for nystagmus with torticollis. They used a posterior fixation suture in conjunction with the traditional Kestenbaum procedure as a two staged procedure when torticollis was more than 20°. The first stage was a standard Kestenbaum operation and the second was placement of a posterior fixation suture at 14 to 20 mm from the original insertion site three months later if a residual face turn was noted. Spielmann performed this technique in three horizontal and one vertical torticollis cases with nystagmus. Unfortunately there were no detailed descriptions on the long-term surgical results for these patients. We performed fixation suture placed at 11 mm from the original insertion site for recessed medial rectus muscle (MR) and 13 mm from the original insertion line for recessed lateral rectus muscle (LR). More correction of AHP may have been obtained, if the posterior fixation sutures have been placed at 14 mm for the MR and 16–17 mm for the LR.
Several different mechanisms explaining the effect of the Faden-operation have been proposed. Scott [25] described a decreased torque exerted by the operated muscle as the eye moved into the field of action of that muscle and calculated that posterior fixation at 10 mm in MR will exert decreased torque when the eye is adducted over 15°, and any recession added to Faden-operation, will be enhanced. Kushner [14] reported that after recession with posterior fixation suture, postoperative saccadic velocity did not decrease as the eye moved increasingly into the field of action of the operated muscle in convergence excess esotropia. This was due to the increased amount of slack created in functional part of the muscle after recession. Paliaga and Braga demonstrated that Faden-operation on the medial rectus muscle produces an augmentation of the passive resistance to adduction which increase with the degree of adduction and the resistance seems to decrease after the operation as time passes [20]. In our study, after posterior fixation with recession, our patients usually did not show limitation of movement in the direction of the posterior fixation. We speculate that a possible reason as is the smaller augmented Kestenbaum surgery (6-7-8-9) that we performed relative to other techniques and different location of posterior fixation suture than often performed elsewhere. The shorter distance of fixation from the original insertion may decrease the effect of weakening, but did not develop much restriction. Further studies will be needed to evaluate the limitation of ocular movement after posterior fixation with recession.
It is difficult to compare our results to many of the previous reports of Kestenbaum procedure, since these studies used different surgical amounts and follow-up times. These studies also included strabismic patients with a large range of AHP. For example, the dose used for correction of 30°AHP has ranged from about 12 mm to 20 mm surgery on each eye, according to previous reports. Concerning the dose-effect ratio of Kestenbaum surgery as Gräf et al [11] proposed, the ratio of the AHP reduction and the millimeter of surgery on each eye (°/mm ratio), might help to allow the comparison of efficacy of previous reported Kestenbaum surgeries with our results of adding posterior fixation suture. But it is difficult to determine the surgical dose of each patient in previous reports. Since our results showed a statistically significant improvement of head turns (P = 0.008) and a 78% success rate of functionally and aesthetically acceptable head position after a mean follow up of 29.7 months, this method is comparable or better than other studies. Two patients showed a small and cosmetically acceptable overcorrection (Fig. 1).
The age at the surgery in our patients was younger (4.8 ± 1.5 years) than patients in other studies of modified Kestenbaum procedures [5, 15, 17–19, 23, 24, 26, 29] (Table 4). In most other studies, nystagmus surgery was not done prior to 6 years of age because it was thought that a spontaneous decrease in head turn might be possible [21, 23], or the delay allows maturation of the binocular system. But there is no optimal time for nystagmus surgery and if reliable measurements were acquired, earlier surgery may be helpful. We agree with Dell’Osso and Flynn’s [8] recommendation of surgery during the pre-school years to alleviate the cosmetic defect prior to this very sensitive psychological period.
Generally, after a Kestenbaum procedure, improvement of visual acuity is unpredictable [23]. Scott and Kraft reported that two thirds of their patients showed a one Snellen line improvement of binocular visual acuity and four of 32 patients showed more than two Snellen lines improvement. Flynn and Dell’Osso [8] also reported an increase in visual acuity after Kestenbaum type operation, but Nelson et al [19] could not demonstrate any improvement in visual acuity postoperatively. Zubcov et al [29] showed only one of 7 patients had an insignificant improvement of one Snellen line. In our study, binocular visual acuity did not significantly improve (P = 0.68) after surgery. Only three of nine patients showed at least one Snellen line improvement (Fig. 2).
Only one of our patients (patient 3) required additional surgery due to recurrent horizontal AHP. Even in this case, the head turn recurred 2 years after the first surgery (Table 3). The other reoperation case (patient 4) was due to concomitant vertical AHP. Patients with nystagmus may have an abnormal head position directed vertically and/or tilted as well as horizontal. Arroyo et al [3] reported 21 horizontal nystagmus patients who had abnormal head posture in all three axes with a predominant head turn. In our patients, three had concomitant head tilt or abnormal chin posture. One patient (patient 4) had concomitant vertical AHP, so she received surgery for vertical AHP simultaneously. She underwent a half tendon width infraplacement of all four horizontal muscles but later she needed more surgery due to a vertical overcorrection.
In conclusion, we find our procedure safe and effective. On the basis of our results, we propose combining the Kestenbaum procedure with posterior fixation suture at the same time for correction of infantile nystagmus with moderate AHP (20°–35°) in children. This might improve the problems of largely augmented surgeries which result in a significant limitation of duction or strabismus in primary position. Further study with larger numbers of subjects with much longer follow-up is required.
Acknowledgments
Open Access This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Footnotes
Presented in part as a poster at the American Association for Pediatric Ophthalmology and Strabismus 32nd Annual Meeting in Keystone, Colorado, March 15-19, 2006.
The authors have no proprietary interest related to this article.
The authors have full control of all primary data and we agree to allow Graefes Archive for Clinical and Experimental Ophthalmology to review our data upon request.
Contributor Information
Nam Yeo Kang, Email: nyeokang@hanmail.net.
Sherwin J. Isenberg, Phone: +1-310-8258840, FAX: +1-310-7947905, Email: isenberg@ucla.edu
References
- 1.Anderson JR (1953) Causes and treatment of congenital eccentric nystagmus. Br J Ophthalmol 37:267–281 doi:10.1136/bjo.37.5.267 [DOI] [PMC free article] [PubMed]
- 2.Arruga A (1974) Posterior suture of rectus muscles in retinal detatchment with nystagmus: A preliminary report. J Pediatr Ophthalmol 11:36–37
- 3.Arroyo-Yllanes ME, Fonte-Vazquez A, Pérez-Pérez JF (2002) modified Anderson procedure for correcting abnormal mixed head position in nystagmus. Br J Ophthalmol 86:267–269 doi:10.1136/bjo.86.3.267 [DOI] [PMC free article] [PubMed]
- 4.Berad PV, Spielmann A, Reydy R (1976) L’operation du fil de Cuppers. Bull Soc Ophtalmol Fr 12:1111–1116 [PubMed]
- 5.Calhoun JH, Harley RD (1973) Surgery for abnormal head position in congenital nystagmus. Trans Am Ophthalmol Soc 71:70–83 [PMC free article] [PubMed]
- 6.Clark RA, Isenberg SJ (2001) Eye movements decrease with aging. J AAPOS 5:26–31 doi:10.1067/mpa.2001.111016 [DOI] [PubMed]
- 7.Cüppers C (1976) The so-called fadenoperation: surgical corrections by small-defined changes of the arc of contact. In: Fells P (ed) The 2nd Congress of the International Strabismology Association. Diffusion Generale de Librairie, Marseilles (France), p 395
- 8.Dell’Osso LF, Flynn JT (1979) Congenital nystagmus surgery: a quantitative evaluation of the effects. Arch Ophthalmol 97:462–469 [DOI] [PubMed]
- 9.De Decker W (1987) Kestenbaum transposition in nystagmus therapy. Transposition in horizontal and torsional plane. Bull Soc Belge Ophtalmol 221–222:107–120 [PubMed]
- 10.Goto N (1954) A study of optic nystagmus by the electrooculogram. Nippon Ganka Kakkai Zasshi 58:851–865
- 11.Gräf M, Droutsas K, Kaufmann H (2001) Surgery for nystagmus related head turn: kestenbaum procedure and artificial divergence. Graefes Arch Clin Exp Ophthalmol 239:334–341 doi:10.1007/s004170100270 [DOI] [PubMed]
- 12.Gräf M (2002) Kestenbaum and artificial divergence surgery for abnormal head turn secondary to nystagmus. Specific and nonspecific effects for artificial divergence. Strabismus 10:69–74 doi:10.1076/stra.10.2.69.8134 [DOI] [PubMed]
- 13.Kestembaum A (1953) Une nouvelle opération du nystagmus. Bull Soc Ophtalmol Fr 6:599–602 [PubMed]
- 14.Kushner BJ (1983) Evaluation of the posterior fixation plus recession operation with saccadic velocities. J Pediatr Ophthalmol Strabismus 20:202–209 [DOI] [PubMed]
- 15.Kraft SP, O’Donoghue EP, Rarty JD (1992) Improvement of compensatory head posture after strabismus surgery. Ophthalmology 99:1301–1308 [DOI] [PubMed]
- 16.Lee IS, Lee JB, Kim HS, Lew H, Han SH (2000) Modified Kestenbaum surgery for correction of abnormal head posture in infantile nystagmus: outcome in 63 patients with graded augmentation. Binocul Vis Strabismus Q 15:53–58 [PubMed]
- 17.Mitchell PR, Sheeler MB, Parks MM (1987) Kestenbaum surgical procedure for torticollis secondary to congenital nystagmus. J Pediatr Ophthalmol Strabismus 24:87–92 [DOI] [PubMed]
- 18.Muhlendyck H (1978) The fadenoperation in the treatment of congenital nystagmus. In: Reinecke RD (ed) Strabismus. Grune & Stratton, New York, pp 235–248
- 19.Nelson LB, Ervin-Mulvey LD, Calhoun JH, Harley RD, Keisler MS (1984) Surgical management for abnormal head position in nystagmus: the augmented modified Kestenbaum procedure. Br J Ophthalmol 68:796–800 doi:10.1136/bjo.68.11.796 [DOI] [PMC free article] [PubMed]
- 20.Paliagia GP, Braga M (1989) Passive limitation of adduction after Cüpper’s ‘Fadenoperation’ on medial recti. Br J Ophthalmol 73:633–635 doi:10.1136/bjo.73.8.633 [DOI] [PMC free article] [PubMed]
- 21.Parks MM (1973) Symposium: nystagmus. Congenital nystagmus surgery. Am Orthopt J 23:35–39 [PubMed]
- 22.Pratt-Johnson JA (1971) The surgery of congenital nystagmus. Can J Ophthalmol 6:268–277 [PubMed]
- 23.Pratt-Johnson JA (1991) Results of surgery to modify the null-zone position in congenital nystagmus. Can J Ophthalmol 26:219–223 [PubMed]
- 24.Sandall GS (1976) Surgical treatment of congenital nystagmus in patients with singular binocular vision. Ann Ophthalmol 8:227–238 doi:10.1159/000127868 [PubMed]
- 25.Scott AB (1977) The Faden operation: Mechanical effects. Am Orthopt J 27:44–47 [PubMed]
- 26.Scott WE, Kraft SP (1984) Surgical treatment of compensatory head position in congenital nystagmus. J Pediatr Ophthalmol Strabismus 21:85–95 [DOI] [PubMed]
- 27.Spielmann A (1991) Les strabismes: De lánalyse clinique á la synthése chirugicale. Masson, Paris, p252
- 28.Taylor JN (1973) Surgery for horizontal nystagmus; Anderson-Kestenbaum operation. Aust J Ophthalmol 1:114–116 doi:10.1111/j.1442-9071.1973.tb00116.x [DOI] [PubMed]
- 29.Zubcov AA, Stärk N, Weber A, Wizor SS, Reinecke RD (1993) Improvement of visual acuity for nystagmus. Ophthalmology 100:1488–1497 [DOI] [PubMed]