Abstract
Purpose
The outcome of Perthes’ disease in children over 8 years tends to be poor. It is unclear whether any treatment modality alters the natural history. This study compares the results of four treatment modalities for this group of patients.
Methods
A retrospective review was performed of prospectively collected data for 44 children (48 hips) with Catterall grade 2, 3 or 4 Perthes’ disease with onset age 8 years or older followed to maturity. Patients were divided into four groups (a no-treatment group and three interventional groups). The interventional groups were demographically similar but the untreated patients were older and had poorer indices for most modalities.
Results
Overall for all treatment modalities only 19% had a satisfactory Stulberg grade II outcome. Poorer outcomes (as assessed by center–edge angle and percentage femoral head coverage) were associated with increasing age, greater initial head deformity, and more head involvement. Initial head deformity did not remodel for any group and progressed despite plaster treatment or varus osteotomy but not after acetabular augmentation. Acetabular augmentation gave better outcomes for C/B ratio and center–edge angle.
Conclusions
Whatever the treatment, the outcome is poorer with increasing age. No treatment guarantees a good result for significant head involvement or initial deformity but acetabular augmentation improves C/B ratio and center–edge angle and prevents progressive femoral head deformity compared with no treatment, varus osteotomy, and plaster treatment.
Keywords: Perthes’, Late onset, Outcomes, Shelf acetabuloplasty
Introduction
The results for children presenting with Perthes’ disease over the age of 8 years tend to be poor [1]. Nonoperative treatment, which may be appropriate in younger patients, is less successful in this age group. It has been suggested that older children with more severe disease have a better outcome when treated surgically [2]. Containment by means of a varus femoral osteotomy is well described [3]. However, because there is less time for remodeling, particularly of the acetabulum in the older child, results may be compromised in the longer term [4]. Furthermore a femoral varus deformity often persists, which patients find cosmetically unacceptable and which may require a corrective valgus femoral osteotomy once head healing is complete. With surgery to remove the metalwork used to hold the osteotomies, the patient may need as many as four procedures to achieve the desired outcome. More recently shelf acetabuloplasty has been advocated, with an improved outcome reported in several studies [5, 6]. This involves a single surgical procedure.
We wished to determine whether the type of treatment altered the natural history in these children. In particular, we wished to know if deformity of the femoral head at presentation could be improved by treatment and to determine which treatment method, if any, produced the best acetabular remodeling. This paper reviews the management and outcomes for Perthes’ disease in children over the age of 8 years from a single center.
Materials and methods
Complete clinical and radiological data up to the age of skeletal maturity were available for 44 patients (36 male, including four bilateral, and 8 female) diagnosed between 1987 and 2003 with Perthes’ disease and aged 8 years or older. All patients were treated in the same center by a total of seven surgeons. Mean age at presentation was 9.75 years (8–14.3 years). Mean follow-up was for 6.4 years (2.2–20 years). All children were treated at The Royal Hospital for Sick Children in Glasgow.
Full history and examination were recorded. Serial anteroposterior and frog-lateral radiographs were graded according to the Waldenström [7], Herring [8], and Catterall [9] classifications. Bone age (assessed independently by the Greulich and Pyle [10] method) was available for 20 of 44 patients.
Treatment was considered for patients aged over 8 years at presentation with Catterall grade II, III or IV involvement of the femoral head. For the intervention groups initial management comprised a period in abduction casts to restore hip motion, followed by an arthrogram or hip screening to assess whether the femoral head could be contained. Before 1994, ongoing containment by means of abduction casting or a varus femoral osteotomy was undertaken; the choice of which option was left to the parents and child. Abduction plasters were retained until healing was well established radiologically, at which stage patients were mobilized but remained on severely restricted activity for another 18–24 months until healing was well advanced.
After 1994 shelf acetabuloplasty was performed to maintain containment. The shelf procedure was performed as described by Staheli [11] except we did not repair the reflected head of rectus femoris over the top of the shelf. The nonintervention group comprised children presenting in the healing phase when intervention could not alter the outcome (though some had presented earlier to other hospitals but had received no treatment until it was too late to alter the outcome, by the time they were referred to our center).
Both varus osteotomy and shelf acetabuloplasty are contraindicated (though still sometimes done) in patients with evidence with “hinge abduction” when a valgus femoral osteotomy may be more appropriate [12]. Patients who presented with a hinge abduction deformity were managed by valgus osteotomy once healing was complete.
Details of all operative and nonoperative treatments were recorded. Patients were regularly reviewed clinically and radiologically up to and beyond skeletal maturity.
In an attempt to define head deformity both initially and finally, presentation and final radiographs were assessed using the method described by Mose [13]. Because the children were over 8 years old, the femoral head was fully ossified, allowing Mose assessment despite the technique applying to the mature hip. The initial measurement was performed on the first available film, whatever the Waldenstrom stage. In most patients this was in the sclerosis or early fragmentation phase. Where the involved femoral head showed equal curvature on both anteroposterior and lateral views the result was rated as good or undeformed. A difference in radius of curvature of up to 2 mm in either view was considered fair or with minor deformity. The result was classed as poor or deformed if the outline of the femoral head did not form the arc of a circle in either view (irregular) or if the difference between the femoral head in the two views was greater than 2 mm. Final radiographs were also classified by the method of Stulberg et al. [14]. In an effort to define the response of the acetabulum, the initial and final femoral epiphyseal width, the initial and final center–edge angle of Wiberg (CEA) [15], the initial and final C/B ratio [16], and the initial and final percentage femoral head coverage [17] were calculated. As for Mose the initial measurements were performed on the earliest available radiograph.
We also assessed whether the acetabulum had a stable or unstable configuration in three grades [18]. If the outer lip of the acetabulum sloped upwards the configuration was considered unstable (grade 3). If the slope of the outer lip was downwards the acetabulum was labeled as stable (grade 1), whilst a horizontal outer lip was described as neutral (grade 2) (Table 1).
Table 1.
Demographic and outcome data
| Treatment group | Age diagnosed (years) | Sex | Waldenström stage | Mose group | Herring classification | Stulberg classification | Follow-up (years) |
|---|---|---|---|---|---|---|---|
| No treatment | 10 | F | 2 | Poor | B | III | 6 |
| 12.8 | M | 1 | Poor | C | IV | 2.7 | |
| 9.8 | M | 1 | Fair | B | III | 4.6 | |
| 11.9a | M | 2 | Poor | C | IV | 6.4 | |
| 11.9 | M | 1 | Poor | B | IV | 6.4 | |
| 9 | M | 3 | Poor | C | III | 5.9 | |
| 8.6 | M | 3 | Poor | C | III | 5.2 | |
| 12.4 | F | 3 | Poor | C | V | 20 | |
| 9.2a | M | 3 | Poor | C | IV | 14.5 | |
| 8 | M | 3 | Fair | C | II | 5.3 | |
| 9.2a | M | 3 | Poor | C | V | 6.9 | |
| 10.5 | F | 3 | Fair | B | III | 3.4 | |
| 10 | F | 4 | Poor | C | V | 8.3 | |
| 14.3a | M | 3 | Poor | C | V | 3.7 | |
| Abduction cast | 8 | F | 3 | Poor | C | III | 5.4 |
| 8.6 | M | 2 | Fair | B | II | 14.1 | |
| 8 | M | 1 | Fair | B | III | 6 | |
| 8 | M | 3 | Poor | B | III | 2.3 | |
| 9.5 | M | 2 | Fair | B | II | 6.8 | |
| 9.9 | M | 3 | Fair | B | III | 7.10 | |
| 8.5 | M | 3 | Poor | B | IV | 12.8 | |
| 8 | M | 1 | Fair | B | II | 5.3 | |
| 8.8 | M | 2 | Fair | B | III | 4.6 | |
| 9.2 | M | 3 | Poor | C | IV | 16.1 | |
| 11.8 | M | 1 | Poor | C | IV | 4.9 | |
| 12.1 | M | 1 | Fair | B | III | 2.11 | |
| Varus osteotomy | 8.5 | M | 2 | Poor | C | III | 6.9 |
| 9.9 | M | 2 | Poor | B | III | 13.8 | |
| 8 | F | 3 | Fair | B | III | 6.5 | |
| 9.5 | M | 3 | Poor | B | III | 2.6 | |
| Shelf acetabuloplasty | 10.8 | M | 2 | Fair | B | II | 5.7 |
| 8 | M | 2 | Poor | C | III | 7 | |
| 9 | M | 3 | Fair | B | II | 5.8 | |
| 12.10 | M | 4 | Poor | B | IV | 3.2 | |
| 8.4 | M | 3 | Poor | C | III | 4.4 | |
| 9.11 | F | 2 | Poor | B | III | 10.10 | |
| 10.1 | M | 2 | Poor | C | III | 5.1 | |
| 8.9 | M | 2 | Fair | A | II | 4.11 | |
| 11.1 | M | 2 | Fair | B | III | 4..9 | |
| 9.10 | M | 3 | Poor | B | III | 6 | |
| 10.8 | F | 2 | Poor | C | III | 4.5 | |
| 8a | M | 3 | Poor | B | III | 5.10 | |
| 10.2 | M | 3 | Poor | C | III | 5.2 | |
| 12.1 | M | 3 | Poor | C | IV | 8 | |
| 10.5 | M | 1 | Fair | B | II | 2.2 | |
| 8.1 | M | 3 | Fair | B | III | 6.5 | |
| 10.1 | M | 3 | Fair | B | III | 4.1 | |
| 9.3 | M | 1 | Fair | C | II | 9.5 |
aValgus osteotomy
Statistical methods
All statistical analyses were performed using SPSS version 12 (SPSS Inc., Chicago, IL). The Wilcoxon signed rank sum test and Student’s T test were used to determine significant differences between categorical and numeric values, respectively. Spearman’s and Pearson’s rank correlation coefficients were used to detect significant relationship between different values. The results were considered to be significant for P < 0.05.
Results
We subdivided hips into groups according to their treatment. The first group comprised 14 hips treated conservatively with observation after presenting late. In group 2, abduction casts were employed for 12 patients, being retained until early healing was visible on X-ray. The four patients in group 3 were treated by varus femoral osteotomy after an initial period in abduction casts until full movement was regained. Statistical analysis showed no significant difference between groups 2 and 3 in demographic profile or for any outcome measures. We considered that varus osteotomy and abduction casting achieved the same containment by different methods. Group 4 comprised 18 patients who underwent shelf acetabuloplasty. Five patients who presented with hinge abduction (confirmed by dynamic arthrogram) underwent a valgus osteotomy but were grouped with their initial treatment modality. For these five the measurements taken immediately before the valgus osteotomy were used though there was no significant change to the indices following surgery.
As is almost invariably the case, none of our children had significant symptoms in the form of pain after the end of healing. Hip rotation was restricted in children with Stulberg grade IV and V outcomes. Hip abduction was reduced in patients with hinge abduction but following valgus osteotomy surgery their abduction was restored to normal.
Patient demographics for plaster/varus osteotomy versus shelf acetabuloplasty with regard to age at presentation, Catterall grade, Herring grade, initial Mose group, initial CEA, and initial percentage of femoral head cover were not significantly different, indicating comparable groups. However, these indices between the no-treatment group and the other groups were significantly different. The no-treatment group contained some patients who presented too late for the outcome to be altered by treatment and others, managed in other hospitals by observation. The indices were skewed by the late presenters who demonstrate the true untreated natural history of the condition. If the no-treatment group was truly different from the plaster/varus osteotomy patients the outcome measures should have been worse for the no-treatment group. However there were no significant differences in outcomes between the combined group (plaster/varus osteotomy) and the no-treatment group with respect to final Stulberg evaluation, percentage femoral head coverage, or C/B ratio. Therefore, we believe that the no-treatment group, which was skewed by the late presenters, was probably comparable to the combined group and that the initial indices would also have been comparable had it been possible to obtain them earlier in their history.
However, there were significant differences in outcome for these same variables (final Stulberg evaluation, percentage femoral head coverage, and C/B ratio) between the shelf acetabuloplasty and no-treatment group, between the shelf acetabuloplasty and abduction POP, and between the shelf acetabuloplasty and the varus osteotomy groups, which probably represent true differences.
Comparing the initial femoral head deformity by Mose against the final outcome showed no deterioration in this modality for shelf acetabuloplasty or no treatment. For the no-treatment group this was because the femoral head was already maximally deformed at the time of presentation for most patients, whereas for shelf acetabuloplasty the treatment appears to have prevented significant progression of femoral head deformity. Plaster or varus osteotomy management showed a statistically worse outcome for Mose at the end of treatment, indicating that these treatments did not prevent progressive deformation of the femoral head in our patients. Treatment also had no effect on outcome with regard to initial versus final percentage femoral head coverage or initial versus final CEA for the no treatment, abduction POP, and varus osteotomy groups. The shelf acetabuloplasty procedure, as might be expected, produced a significant improvement in the CEA and C/B ratio, though surprisingly the percentage head cover just failed to achieve significance (P = 0.068) (Table 2).
Table 2.
Effect of different treatments on femoral head containment (initial versus final)
| Significance | |
|---|---|
| No treatment | |
| Initial % head cover | NS |
| Final % head cover | |
| Initial CE angle | NS |
| Final CE angle | |
| Initial C/B ratio | NS |
| Final C/B ratio | |
| Abduction plaster | |
| Initial % head cover | Sig. 0.05 (final better) |
| Final % head cover | |
| Initial CE angle | NS |
| Final CE angle | |
| Initial C/B ratio | Sig. 0.05 (final worse) |
| Final C/B ratio | |
| Varus osteotomy | |
| Initial % head cover | Sig. 0.05 (final better) |
| Final % head cover | |
| Initial CE angle | NS |
| Final CE angle | |
| Initial C/B ratio | Sig. 0.05 (final worse) |
| Final C/B ratio | |
| Shelf acetabuloplasty | |
| Initial % head cover | NS |
| Final % head cover | |
| Initial CE angle | Sig. 0.05 (final better) |
| Final CE angle | |
| Initial C/B ratio | Sig. 0.01 (final better) |
| Final C/B ratio | |
At final follow-up, nine hips were classified as Stulberg II and were considered satisfactory. Twenty-five hips were assessed as Stulberg III, nine were rated as Stulberg IV, and four as Stulberg V; all of these groups were considered unsatisfactory. The average Stulberg grade was III for boys and IV for girls. This difference was significant (P = 0.0075).
The Herring classification has been shown to accurately predict the final degree of head deformity. This was certainly confirmed in our series where a worse Herring class produced a worse Stulberg outcome (P = 0.002). This would be expected because our Mose measurements demonstrated that head deformity, once present, did not remodel so a poor Herring initially indicates irreversible head deformity and therefore a poor final outcome.
Older patient age at presentation and greater head involvement (Catterall grading) proved to be the leading causes for poorer acetabular remodeling and consequently higher Stulberg grading for all groups. Lower percentage of femoral head coverage and poorer final Mose outline for the femoral head were significantly correlated with poorer Stulberg grades.
The mean bone age at presentation was the 35th centile (95% confidence interval: 27th–43rd centile). A significant correlation was found between both the chronological and the corrected ages and Stulberg outcome (P = 0.004). The four patients with the worst outcome (Stulberg V) were aged 10 years or over at presentation. All treatment groups developed a similar degree of coxa magna (as assessed by comparative epiphyseal width).
Discussion
It is generally accepted that Stulberg grade I and II results are satisfactory such that 0% and 16% of hips in these groups subsequently developed osteoarthritis. Stulberg grade III outcomes can be called fair, though 58% subsequently developed osteoarthritis. Grades IV and V generally have a poor outcome, with 75% and 78%, respectively, developing osteoarthritis [14]. Our results confirm that the outcome for Perthes’ presenting over 8 years of age is generally worse than that reported in younger children, with only 19% of our patients (for all treatment modalities) having a satisfactory radiological appearance (Stulberg II) at skeletal maturity. The Stulberg outcomes for each treatment modality are shown in Fig. 1. Questions have been raised regarding the reliability of the Stulberg classification [19] but it remains the most widely used means of predicting the onset of degenerative joint disease in Perthes’. The classification recognizes the prognostic importance of both femoral head deformity and acetabular remodeling for long-term outcomes. Sphericity and congruence are clearly important. It is not surprising that patients with the worst outcome tend to be those in whom there is less growth time available for remodeling [20], such that they develop a “square peg in a round hole” deformity [14] (Fig. 2). This problem may be compounded in girls, where skeletal maturity occurs at an earlier chronological age. This probably explains the poorer outcome for girls in our study, though there were only 8 females out of 44 patients.
Fig. 1.
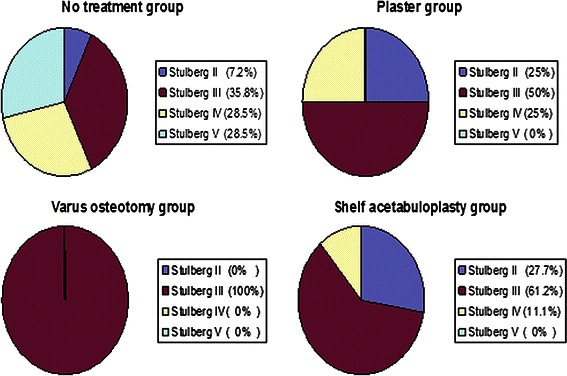
Stulberg outcomes for all treatment modalities, with better outcome in patients treated by acetabuloplasty
Fig. 2.
Results of no-treatment group showing aspherical congruent hip joint with early osteoarthritic changes
The aim of treatment in Perthes’ disease is to maintain hip motion whilst providing containment of the soft femoral head. This may be accomplished by shelf acetabuloplasty, a varus osteotomy or abduction plasters. However, even with a result of a satisfactory spherical femoral head there is always enlargement of the epiphysis which also requires remodeling of the acetabulum to provide adequate lateral cover. Acetabular remodeling seems less effective in older children Thus there is often a disparity in size between the enlarged femoral head and the acetabulum at maturity. However, partial acetabular remodeling may also produce a sloping, unstable acetabular roof (Fig. 3). Shelf acetabuloplasty appears more effective than varus femoral osteotomy in providing lateral femoral head coverage, thereby preventing lateral sublaxation even for a mushroom-shaped femoral head. Increased lateral cover is likely to reduce the joint reaction force and improve joint stability, thereby protecting against degenerative joint disease in the longer term (Fig. 4). Furthermore a larger acetabulum may allow more success for resurfacing arthroplasty when hip replacement becomes necessary. Interestingly, despite a significant improvement in lateral cover (=CEA) with the shelf acetabuloplasty procedure the resulting acetabulae were still smaller than the enlarged femoral head as measured by percentage femoral head coverage. However, the lack of deterioration of the C/B ratio suggests this was not due to lateral migration of the head in the acetabulum.
Fig. 3.

Results of varus osteotomy showing oval head, deficient lateral cover, and sloping unstable (grade 3) acetabular roof
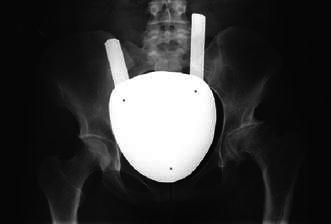
Fig. 4.

Results of lateral acetabuloplasty demonstrating well-covered (mushroom-shaped) femoral head and stable acetabulum
The study also confirms that femoral head deformity at presentation does not remodel, though worse deformity was prevented for the shelf acetabuloplasty group. This also explains why the Herring classification so accurately predicts the final outcome because the classification measures deformity which does not later remodel. The ideal classification would be one that predicts the likely outcome before deformity has occurred in the hope that treatment might prevent deformity and improve the outcome. The Salter and Thompson classification meets this criterion but a subchondral fracture is only visible in 15% of standard view X-rays [21]. The subchondral fracture would be visible with multiplanar X-rays but this would expose children to unacceptably high doses of irradiation. The Catterall classification can often be applied before deformity occurs but there are major problems with inter- and intra-observer reliability. Furthermore the degree of head involvement may increase as the disease progresses, which again affects reliability.
The logic of the shelf acetabuloplasty in the presence of significant hinge abduction must be questioned, since the femoral head deformity will not remodel and greater lateral cover may increase lateral pressure during hinging.
A limitation of this study is that it is not a randomized controlled trial (RCT) so it is possible that biases have occurred despite the apparent close matching of the demographic details in the four treatment groups. However, we are talking about a rare condition with a prevalence of between 1 in 5,000 and 1 in 125,000. It took 16 years to accrue 44 patients with Perthes’ onset over 8 years in a high-incidence area. It is virtually impossible to perform a RCT for such a rare condition. This is aside from the impossibility of persuading parents to allow a no-treatment option for a highly emotive chronic condition such as Perthes’, despite the genuine lack of knowledge as to whether treatment alters the natural history of the disease. Careful prospective cohort observational population studies, such as this one, are often the only way to investigate the outcomes for such rare conditions. Because our patients come from a single center possible geographical variations in the disease behavior are less likely than for a multicenter investigation. Another limitation is the well-known inter- and intra-observer variability is classifying Perthes’ hips by the Catterall and Stulberg systems. This variability probably also applies to some extent with the Mose, CEA, C/B ratio, and percentage femoral head coverage assessments, though a random sample of these assessments was repeated both by the initial assessor and the senior author with greater than 80% agreement.
We have noted that the demographics of the no-treatment group were different from the intervention groups in that no-treatment patients were older and had greater head involvement and head deformity. It might therefore be expected that the outcomes for the no-treatment group would be worse than the intervention groups solely for this reason. The fact that there was no significant difference in outcomes between the no-treatment and the abduction plaster or varus osteotomy groups further reinforces the argument that these interventions did not alter the natural history for our patients.
It is useful to compare our results with those of Herring and co-workers [2] in their multicenter examination of Perthes’ outcomes for various treatment modalities. Unfortunately they did not have the shelf group for direct comparison. Like us they found much poorer results in their over 8-year-old group, which comprised 141 patients. Of these only one was Herring group A, 19 were Herring group C, and 121 were Herring B or B/C. The Herring A patient did well and all group C patients did badly whatever their treatment. Surgery, either varus osteotomy or innominate osteotomy, significantly improved the outcome in the B and B/C patients compared with nonoperative treatment. They recommended no treatment for Herring group C patients. They advised operation as early as possible, even if the Herring grade was not yet clear, for all B and B/C patients to avoid increasing deformity which would not be reversed by surgery. We agree entirely with these recommendations which we feel are supported also with respect to shelf acetabuloplasty. We had 21 Herring C patients with only two Stulberg II, nine Stulberg III, six Stulberg IV, and four Stulberg V outcomes. In agreement with Herring, there was no difference in outcomes statistically between any of our treatment groups for Herring C patients. This confirms the poor outcome for Herring C patients over 8 years at onset of their disease. For Herring B children there was no statistical difference in outcome between the shelf, abduction plaster, and varus osteotomy groups (P = 0.91). Because of the small numbers, we also failed to show statistical improvement in outcome between the no-treatment and abduction plaster, varus osteotomy (P = 0.26) and between the no-treatment and shelf groups (P = 0.25) though the trend was suggestive of benefit.
In summary, for our patients presenting with Perthes’ over the age of 8 years, treatment by abduction plasters or varus femoral osteotomy did not improve any outcome measure compared with no treatment. Shelf acetabuloplasty did prevent further femoral head deformity and produce better lateral cover (CEA) and C/B ratio but did not improve percentage femoral head coverage or Stulberg outcomes. These results support recent evidence suggesting that shelf acetabuloplasty may offer the best chance of a favorable result. To be effective, surgery should be done before deformity develops [6, 22]. We believe this is the most important message from this paper. Many patients over 8 years with Perthes’ initially have minor symptoms and good hip movement so they are observed until suddenly there is head collapse and severe pain. By this stage it is no longer possible to prevent or reverse deformity and a poor outcome is assured. Prolonged management in abduction plasters is probably no longer socially acceptable. Neither plaster treatment nor varus femoral osteotomy prevented progressive femoral head deformity and the degree of acetabular remodeling and lateral cover was unsatisfactory. Furthermore, varus osteotomy patients may need additional surgery to correct coxa vara and to remove metalwork.
References
- 1.Ismail M, Macnicol MF. Prognosis in Perthes’ disease: a comparison of radiological predictors. J Bone Joint Surg Br. 1998;80(2):310–314. doi: 10.1302/0301-620X.80B2.8054. [DOI] [PubMed] [Google Scholar]
- 2.Herring JA, Kim HT, Browne R. Legg-Calvé-Perthes’ disease. Part II: Prospective multicenter study of the effect of treatment on outcome. J Bone Joint Surg Am. 2004;86-A:2121–2134. [PubMed] [Google Scholar]
- 3.Joseph B, Srinivas G, Thomas R. Management of Perthes’ disease of late onset in Southern India: the evaluation of a surgical method. J Bone Joint Surg Br. 1996;78-B:625–630. [PubMed] [Google Scholar]
- 4.Coates CJ, Paterson JMH, Woods KR, Catterall A, Fixsen JA. Femoral osteotomy in Perthes’ disease: results at maturity. J Bone Joint Surg Br. 1990;72-B:581–585. doi: 10.1302/0301-620X.72B4.2380208. [DOI] [PubMed] [Google Scholar]
- 5.Willet K, Hudson A, Catterall A. Lateral shelf arthroplasty: an operation for older children with Perthes’ disease. J Paediatr Orthop Surg. 1992;12:563–565. doi: 10.1097/01241398-199209000-00001. [DOI] [PubMed] [Google Scholar]
- 6.Daly K, Bruce C, Catterall A. Lateral shelf arthroplasty in Perthes’ disease. A review at the end of growth. J Bone Joint Surg Br. 1999;81-B:380–384. doi: 10.1302/0301-620X.81B3.9405. [DOI] [PubMed] [Google Scholar]
- 7.Waldenström H (1922–1923) On coxa plana: osteochonditis deformans coxae juveniles: Legg’s maladie de Calvé, Perthes Krankreit. Acta Chir Scand 55:577–590
- 8.Herring JA, Neustadt JB, Williams JJ, Early JS, Browne RH. The lateral pillar classification of Legg-Calve-Perthes disease. J Pediatr Orthop. 1992;12:143–150. doi: 10.1097/01241398-199203000-00001. [DOI] [PubMed] [Google Scholar]
- 9.Catterall A. The natural history of Perthes’ disease. J Bone Joint Surg Br. 1971;53-B:37–53. [PubMed] [Google Scholar]
- 10.Greulich WW, Pyle SI. Radiographic atlas of skeletal development of the hand and wrist. 2. Stanford: Stanford University Press; 1959. [Google Scholar]
- 11.Staheli LT. Slotted acetabular augmentation. J Pediatr Orthop. 1981;1:321. doi: 10.1097/01241398-198111000-00014. [DOI] [PubMed] [Google Scholar]
- 12.Yoo WJ, Choi IH, Chung CY, Cho TJ, Kim HY. Valgus femoral osteotomy for hinge abduction in Perthes’ disease. J Bone Joint Surg Br. 2004;86-B:726–730. doi: 10.1302/0301-620X.86B5.13897. [DOI] [PubMed] [Google Scholar]
- 13.Mose K. Methods of measuring in Legg-Calvé-Perthes’ disease with special regard to the prognosis. Clin Orthop Relat Res. 1980;150:103–108. [PubMed] [Google Scholar]
- 14.Stulberg D, Cooperman D, Wallensten R. The natural history of Legg-Calvé–Perthes’ disease. J Bone Joint Surg Am. 1981;63-A:1095–1108. [PubMed] [Google Scholar]
- 15.Wiberg G (1939) Studies on dysplastic acetabula and congenital sublaxation of the hip joint. With special reference to the complication of osteo-arthritis. Acta Chir Scand 83(Suppl 58):7–38
- 16.Smith WS, Badglevc E, Orwig JB, Harperj M. Correlation of Post reduction roentgenograms and thirty-one-year follow up in congenital dislocation of the hip. J Bone Joint Surg. 1968;50-A:1081–1098. [PubMed] [Google Scholar]
- 17.McCarthy JJ, Fox JS, Gurd AR. Innominate osteotomy in adolescents and adults who have acetabular dysplasia. J Bone Joint Surg Am. 1996;78:1455–1461. doi: 10.2106/00004623-199610000-00001. [DOI] [PubMed] [Google Scholar]
- 18.Patil S, Sherlock DA (2007) Curr Orthop 21:109–114. doi:10.1016/j.cuor.2007.04.004
- 19.Neyt JG, Weinstein SI, Spratt KF, Dolan L, Morcuende J, et al. Stulberg classification system for the evaluation of Legg-Calvé-Perthes’ disease: intra-rater and inter-rater reliability. J Bone Joint Surg Am. 1999;81-A:1209–1216. doi: 10.2106/00004623-199909000-00002. [DOI] [PubMed] [Google Scholar]
- 20.Mazda K, Pennecot G, Zeller R, Taussig G. Perthes’ disease after the age of twelve years; role of the remaining growth. J Bone Joint Surg Br. 1999;81-B:696–699. doi: 10.1302/0301-620X.81B4.9626. [DOI] [PubMed] [Google Scholar]
- 21.Salter RB, Thompson GH (1984) Legg-Calve-Perthes disease. The prognostic significance of the subchondral fracture and a two-group classification of the femoral head involvement. J Bone Joint Surg Am 66:479–489 [PubMed]
- 22.Joseph B, Sreekumaran N, Rao N, Malpuri J, Varghese G. Optimal timing for containment surgery for Perthes’ disease. J Pediatr Orthop. 2003;23:601–606. doi: 10.1097/01241398-200309000-00006. [DOI] [PubMed] [Google Scholar]


