Abstract
Purpose
The purpose of this study is to evaluate the clinical and radiological outcomes of hemiepiphysiodesis with a single medial staple of the proximal tibia in idiopathic genu valgum angular correction.
Methods
A retrospective review was performed identifying nine adolescents (18 knees) treated for idiopathic adolescent genu valgum by means of a bilateral hemiepiphysiodesis with a single staple of the proximal tibia. The intermalleolar distance (IMD) and hip–knee–ankle angle were measured at skeletal maturity.
Results
The IMD and hip–knee–ankle angle were reduced in all patients at skeletal maturity.
Conclusion
Hemiepiphysiodesis with a single medial staple of the proximal tibia seems to be a reliable and safe alternative method to achieve correction of an idiopathic genu valgum.
Keywords: Idiopathic genu valgum, Stapling, Epiphysiodesis
Introduction
Adolescent idiopathic genu valgum is a common frontal deformity. Surgical angular correction is admitted over a measured intermalleolar distance (IMD) of 8 cm [1] in order to avoid anterior knee pain, abnormal gait patterns or patellofemoral instability. The idiopathic genu valgum originates in the distal femoral metaphysis [2, 3]. Most surgical techniques are based on a progressive correction with an asymmetrical epiphyseodesis of the medial side of the distal femoral growth plate. Previously published techniques of permanent epiphysiodesis rely on destruction of the medial femoral growth plate by means of percutaneous curettage, drilling or screws [4–10]. Phemister’s technique is now considered as obsolete [11]. With these techniques stands the issue of the proper timing for surgery to avoid overcorrection [6]. Techniques of temporary epiphysiodesis are based on bridging the growth plate with staples. Since its description by Blount [12], femoral and tibial stapling has been widely used for the progressive correction of lower limb deformities. But medial femoral stapling for the correction of genu valgum has been discarded for postoperative knee pain [13]. In order to avoid complications of both techniques of femoral epiphysiodesis, an alternative method was developed consisting in hemiepiphysiodesis of the proximal medial growth plate of the tibia with a single staple. Tibial stapling alone has already been described for isolated deformities of the tibial physis and combined with femoral stapling for severe genu valgum deformities [14]. To our knowledge, tibial stapling alone for the correction distal femur deformities has not been reported in the published literature.
The purpose of this study was to evaluate the clinical and radiological outcomes of hemiepiphysiodesis with a single medial staple of the proximal tibia for idiopathic genu valgum angular correction.
Methods
A retrospective review was performed identifying nine adolescents (18 knees) treated for an idiopathic genu valgum treated by means of a bilateral medial proximal tibia hemiepiphysiodesis with a single staple. There were five boys and four girls. The mean age at surgery was 12.2 years (range 9–16). Growth potential was evaluated with bone-age estimation determined using the atlas of Greulich and Pyle [15]. The mean bone age was 11 (range 8–13) in girls and 13 (range 9–15) in boys. Surgery was indicated for skeletally immature patients with a painful genu valgum and a distance between the medial malleoli (IMD) of over 8 cm. One patient was 16 years old. Surgery was indicated because tibial physis were still widely opened and bone age estimation was 15 years old.
All patients had physical evaluation throughout followup recording the IMD in a standing position and the knee functional status. Each patient underwent plain radiographs of the lower limbs at skeletal maturity to document limb alignment according to Paley’s technique [16]. The hip–knee–ankle angle, the mechanical axis deviation (MAD; percentage ratio of the distance from the knee joint centre to the mechanical axis divided by half the width of the tibial plateau), the mechanical lateral distal femoral angle (mLDFA), the mechanical medial proximal tibial angle (mMPTA) and the mechanical lateral distal tibial angle (mLDTA) were measured (Fig. 1).
Fig. 1.
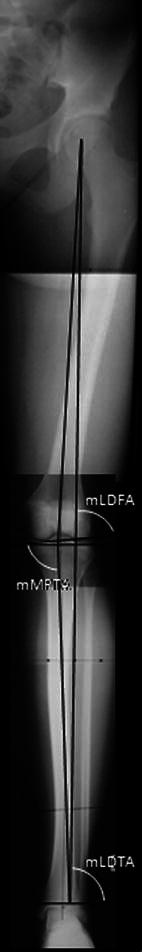
Anteroposterior radiograph showing the different angles measured (mLDFA, mMPTA, mLDTA)
Normal values for each angle were interpreted as a good outcome. A single abnormal value was interpreted as a bad outcome.
Surgical technique
With the patient supine on a radiolucent table and under tourniquet control, the proximal medial tibial physis was localised under fluoroscopic guidance. A 2-cm longitudinal incision was made and a single cobalt-chromium alloy Blount staple was placed across the physis. On the lateral view, the proper staple location was the middle of the physis (Figs. 2 and 3). The total duration of the procedure was 15 min per knee. Full weight-bearing was authorised after surgery. The staple was removed when correction of the IMD was achieved.
Fig. 2.

Postoperative anteroposterior radiograph showing the locations of the staples
Fig. 3.

Postoperative lateral radiograph showing the locations of the staples
Results
Preoperative plain radiographs of the lower limbs were available in cases 1, 3, 6, 7 and 9. In the other cases, only the preoperative hip–knee–ankle (HKA) angle could be extracted from the files, the radiographs being unavailable (Table 1). The initial IMD (IMDi) averaged 8.7 cm (range 7–11 cm). The initial HKA angle averaged 190° (range 188–193°). The mean mLDFA, mMPTA and mLDTA was, respectively, 84° (range 83–85°), 88° (range 86–90°) and 89° (range 88–90°). The initial MAD averaged 53% (range 47–65%). The initial clinical and radiological assessments are recorded in Table 1.
Table 1.
Initial clinical and radiological assessments
| Case | Gender | Age at surgery | IMDi | HKAr | HKAl | MADr (%) | MADl (%) | mLDFAr | mLDFAl | mMPTAr | mMPTAl | mLDTAr | mLDTAl |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | F | 12 | 9 | 192 | 191 | 65 | 65 | 83 | 84 | 90 | 90 | 89 | 89 |
| 2 | M | 13 | 10 | 193 | 193 | – | – | – | – | – | – | – | – |
| 3 | M | 12 | 8 | 189 | 189 | 48 | 52 | 84 | 84 | 87 | 86 | 90 | 90 |
| 4 | F | 9 | 8 | 190 | 190 | – | – | – | – | – | – | – | – |
| 5 | F | 10 | 10 | 192 | 193 | – | – | – | – | – | – | – | – |
| 6 | M | 13 | 8 | 188 | 189 | 47 | 48 | 85 | 85 | 88 | 90 | 90 | 90 |
| 7 | F | 13 | 8 | 189 | 189 | 50 | 54 | 84 | 85 | 90 | 89 | 89 | 88 |
| 8 | M | 16 | 7 | 190 | 189 | – | – | – | – | – | – | – | – |
| 9 | M | 12 | 11 | 193 | 192 | 50 | 52 | 84 | 83 | 89 | 89 | 89 | 89 |
IMDi initial intermalleolar distance; HKA hip–knee–ankle angle; MAD mechanical axis deviation; mLDFA mechanical lateral distal femoral angle; mMPTA mechanical medial proximal tibial angle; mLDTA mechanical lateral distal tibial angle; r right; l left; – not available
The staples remained in place for a median time of 2 years (range 1–3). At skeletal maturity, all patients were pain-free and had a normal range of motion. The average time of correction was 2.1 years (range 1–3 years). The final IMD (IMDf) was 2.5 cm (range 0–5 cm). The HKA angle averaged 181° (range 180–185°). The mean mLDFA, mMPTA and mLDTA was, respectively, 86° (range 83–88°), 88° (range 85–90°) and 89° (range 88–90°). The final MAD averaged 16.5% (range 0–38%). One patient was considered to have bad results (mLDFA of 84° and mMPTA of 83°). No rebound effect was observed after staple removal. The final clinical and radiological assessments are recorded in Table 2.
Table 2.
Final clinical and radiological assessments
| Case | Gender | Age at final followup | IMDf | HKAr | HKAl | MADr (%) | MADl (%) | mLDFAr | mLDFAl | mMPTAr | mMPTAl | mLDTAr | mLDTAl |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | F | 17 | 1 | 183 | 184 | 32 | 32 | 85 | 85 | 89 | 90 | 89 | 89 |
| 2 | M | 16 | 5 | 183 | 184 | 22 | 19 | 88 | 88 | 89 | 89 | 90 | 90 |
| 3 | M | 17 | 1 | 180 | 180 | 0 | 0 | 85 | 86 | 85 | 85 | 90 | 90 |
| 4 | F | 15 | 2 | 185 | 182 | 38 | 34 | 87 | 87 | 90 | 90 | 89 | 89 |
| 5 | F | 16 | 5 | 183 | 183 | 34 | 34 | 84 | 83 | 90 | 88 | 90 | 90 |
| 6 | M | 17 | 3 | 180 | 180 | 0 | 0 | 87 | 87 | 87 | 88 | 90 | 90 |
| 7 | F | 18 | 3 | 183 | 184 | 31 | 27 | 86 | 86 | 90 | 89 | 89 | 88 |
| 8 | M | 18 | 0 | 180 | 180 | 0 | 0 | 87 | 87 | 88 | 88 | 89 | 89 |
| 9 | M | 17 | 3 | 180 | 180 | 0 | 0 | 86 | 86 | 88 | 88 | 89 | 89 |
Abbreviations as per Table 1
Discussion
Correction of an idiopathic genu valgum using the proximal tibia growth plate appears to be unconventional, but our study showed improvement of the mean IMD, from 8.7 to 2.5 cm, the HKA angle, from 190 to 181° and the mean MAD, from 53 to 16.5%. These results are similar to other published series with either permanent or temporary femoral hemiepiphysiodesis [17–20]. Temporary arrest of the proximal medial growth plate of the tibia induces a tibia varus which compensates the femur valgum and explains the IMD correction. But the association of a tibia varus and a femur valgus would logically increase the obliquity of the frontal femorotibial articular line. No abnormal obliquity of the frontal femorotibial articular line was observed in our cases. The mean mLDFA values improved from 84 to 86°, suggesting adaptation of the distal femoral physis to the progressive tibial varus. All patients but one had normal range of mLDFA values (85–90°). The bad radiological result (mLDFA < 85°) in case 5 is probably due to a misevaluation of the residual growth potential associated with a great magnitude of initial deformity. No excessive tibial varus was encountered according to the normal range of mMPTA values recorded at skeletal maturity. The mMPTA values remained unchanged or decreased by 1°. The varus stress within the proximal tibia seems to have provided remodelling of both proximal tibial and distal femoral growth plates. Our findings sustain previous statements suggesting that a physis orientates perpendicularly to the limb’s mechanical axis. But it is difficult to evaluate the extent of correction needed in the tibia to induce the distal femoral re-alignment. The remodelling of both epiphysis is progressive. Sequential radiographs would have helped to identify when the correction occurred in the distal femur, but the followup was based on physical examination only. Contribution of the distal tibia growth plate in the correction was controlled with mLDTA values. This phenomenon is currently observed in mistreated post-traumatic tibia valgus [21, 22]. In our study, mLDTA values remained unchanged, attesting that the distal tibia growth plate was not involved in the correction.
Insertion of the staple should be at an equivalent distance from the anterior and posterior margin of the tibia. There is a potential risk of modification of the medial femorotibial slope. Insertion of the staple in the anterior tibial tuberosity would be a technical mistake, but a slight anterior or posterior translation of the staple has no consequence (Fig. 3). No alteration of the tibial slope was noted on standard followup radiographs. However, the tibial slope was not evaluated on plain lateral radiographs of the lower limb.
The proper site of angular correction site is usually located at the origin of the deformity. Conjunction of the segmental mechanical axis defines the origin of the deformity on radiographic anteroposterior views [16]. The origin is the so-called centre of rotation angle (CORA). The CORA of the idiopathic genu valgum stands in the distal femoral metaphysis. When the correction site is different from the CORA, a translation is necessary to obtain mechanical axis correction. In all cases, we noted a progressive alignment of the tibia mechanical axis, along with the femur mechanical axis with the same typical S-shaped tibia at the end of correction (Fig. 4). This minor deformity had no functional consequence at the last followup.
Fig. 4.

Anteroposterior radiograph shows the S-shaped tibia deformity at maturity
Other reports of hemiepiphysiodesis recommend the insertion of either two or three staples [2, 14, 17, 20]. We used only one staple in this study, without any breakage. However, there was, each time, widening of the distance between the two tips of the staple. We are not sure that a longer series would provide cases of staple breakage, but the growth potential is higher in the femur than in the tibia growth plate. Strain in the staple is correlated with the growth strength of the physis. This suggests that one staple is resistant enough to obtain growth retardation without breakage in the proximal tibia. However, a longer time of correction (2 years) was required in this study in comparison to published series of distal femoral hemiepiphysiodesis (1 year) [20, 23].
In our hands, an idiopathic genu valgum deformity is now treated with the technique described here. Thus, no comparison was possible between femoral and tibial stapling. Post-operative pain is the main problem of femoral stapling, but no quantitative data are available in the published series to perform a comparison. It is, therefore, difficult to assess if the technique of tibia stapling is less painful than femoral stapling. However, in each case, standard medication was sufficient during the post-operative period.
Although a small number of patients were collected, hemiepiphysiodesis with a single medial staple of the proximal tibia seems to be a reliable and safe alternative method to achieve correction of an idiopathic genu valgum.
References
- 1.Heath CH, Staheli LT. Normal limits of knee angle in white children—genu varum and genu valgum. J Pediatr Orthop. 1993;13:259–262. [PubMed] [Google Scholar]
- 2.Stevens PM, Maguire M, Dales MD, Robins AJ. Physeal stapling for idiopathic genu valgum. J Pediatr Orthop. 1999;19:645–649. [PubMed] [Google Scholar]
- 3.Zhang AL, Exner GU, Wenger DR. Progressive genu valgum resulting from idiopathic lateral distal femoral physeal growth suppression in adolescents. J Pediatr Orthop. 2008;28:752–756. doi: 10.1097/BPO.0b013e3181875b46. [DOI] [PubMed] [Google Scholar]
- 4.Bowen JR, Leahey JL, Zhang ZH, MacEwen GD. Partial epiphysiodesis at the knee to correct angular deformity. Clin Orthop Relat Res. 1985;198:184–190. [PubMed] [Google Scholar]
- 5.Métaizeau JP, Wong-Chung J, Bertrand H, Pasquier P. Percutaneous epiphysiodesis using transphyseal screws (PETS) J Pediatr Orthop. 1998;18:363–369. [PubMed] [Google Scholar]
- 6.Blair VP, 3rd, Walker SJ, Sheridan JJ, Schoenecker PL. Epiphysiodesis: a problem of timing. J Pediatr Orthop. 1982;2:281–284. doi: 10.1097/01241398-198208000-00007. [DOI] [PubMed] [Google Scholar]
- 7.Bowen JR, Johnson WJ. Percutaneous epiphysiodesis. Clin Orthop Relat Res. 1984;190:170–173. [PubMed] [Google Scholar]
- 8.Ferrick MR, Birch JG, Albright M. Correction of non-Blount’s angular knee deformity by permanent hemiepiphyseodesis. J Pediatr Orthop. 2004;24:397–402. doi: 10.1097/01241398-200407000-00010. [DOI] [PubMed] [Google Scholar]
- 9.Khoury JG, Tavares JO, McConnell S, Zeiders G, Sanders JO. Results of screw epiphysiodesis for the treatment of limb length discrepancy and angular deformity. J Pediatr Orthop. 2007;27:623–628. doi: 10.1097/BPO.0b013e318093f4f4. [DOI] [PubMed] [Google Scholar]
- 10.Nouth F, Kuo LA. Percutaneous epiphysiodesis using transphyseal screws (PETS): prospective case study and review. J Pediatr Orthop. 2004;24:721–725. doi: 10.1097/01241398-200411000-00023. [DOI] [PubMed] [Google Scholar]
- 11.Phemister DB. Epiphysiodesis for equalizing the length of the lower extremities and for correcting other deformities of the skeleton. Mem Acad Chir (Paris) 1950;76:758–763. [PubMed] [Google Scholar]
- 12.Blount PW. Epiphysiodesis by clamps. Rev Chir Orthop Reparatrice Appar Mot. 1963;49:171–176. [PubMed] [Google Scholar]
- 13.Dutoit M. Percutaneous epiphysiodesis in the treatment of adolescent genu valgum. Rev Chir Orthop Reparatrice Appar Mot. 1998;84:623–627. [PubMed] [Google Scholar]
- 14.Fraser RK, Dickens DR, Cole WG. Medial physeal stapling for primary and secondary genu valgum in late childhood and adolescence. J Bone Joint Surg Br. 1995;77:733–735. [PubMed] [Google Scholar]
- 15.Greulich WW, Pyle SI. Radiographic Atlas of skeletal development of the hand and wrist. 2. Stanford, CA: Stanford University Press; 1959. [Google Scholar]
- 16.Paley D, Tetsworth K. Mechanical axis deviation of the lower limbs. Preoperative planning of multiapical frontal plane angular and bowing deformities of the femur and tibia. Clin Orthop Relat Res. 1992;280:65–71. [PubMed] [Google Scholar]
- 17.Degreef I, Moens P, Fabry G. Temporary epiphysiodesis with Blount stapling for treatment of idiopathic genua valga in children. Acta Orthop Belg. 2003;69:426–432. [PubMed] [Google Scholar]
- 18.Craviari T, Bérard J, Willemen L, Kohler R. Percutaneous epiphysiodesis. Analysis of a series of 60 full-grown patients. Rev Chir Orthop Reparatrice Appar Mot. 1998;84:172–179. [PubMed] [Google Scholar]
- 19.Pistevos G, Duckworth T. The correction of genu valgum by epiphysial stapling. J Bone Joint Surg Br. 1977;59:72–76. doi: 10.1302/0301-620X.59B1.845231. [DOI] [PubMed] [Google Scholar]
- 20.Volpon JB. Idiopathic genu valgum treated by epiphyseodesis in adolescence. Int Orthop. 1997;21:228–231. doi: 10.1007/s002640050156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Stevens PM, Pease F. Hemiepiphysiodesis for posttraumatic tibial valgus. J Pediatr Orthop. 2006;26:385–392. doi: 10.1097/01.bpo.0000206515.84577.70. [DOI] [PubMed] [Google Scholar]
- 22.Nenopoulos S, Vrettakos A, Chaftikis N, Beslikas T, Dadoukis D. The effect of proximal tibial fractures on the limb axis in children. Acta Orthop Belg. 2007;73:345–353. [PubMed] [Google Scholar]
- 23.Mielke CH, Stevens PM. Hemiepiphyseal stapling for knee deformities in children younger than 10 years: a preliminary report. J Pediatr Orthop. 1996;16:423–429. doi: 10.1097/01241398-199607000-00002. [DOI] [PubMed] [Google Scholar]


