Abstract
Background and Purpose
Restless legs syndrome (RLS) is a sleep disorder that frequently occurs in dialysis patients, which disturbs the sleep and reduces the quality of life. The aim of this study was to determine the risk factors for RLS in dialysis patients.
Methods
Patients who visited any of four outpatient dialysis clinics between September 2005 and May 2006 were included in this study. The diagnosis of RLS and the severity assessment were made using the criteria described by the International Restless Legs Syndrome Study Group. We collected basic demographic data, clinical information, and laboratory findings, and then analyzed their association with various aspects of RLS using univariate and multivariate analyses.
Results
RLS was present in 46 (28.0%) of 164 dialysis patients. We found no significant risk factor for inducing RLS. The predialysis serum blood urea nitrogen (BUN) level in the dialysis patients with RLS was significantly correlated with RLS symptom severity.
Conclusions
Predialysis BUN is related to RLS symptom severity. Further studies on the underlying mechanism are needed.
Keywords: restless legs syndrome, hemodialysis, blood urea nitrogen
Introduction
Restless legs syndrome (RLS) is one of the most commonly encountered sleep disorders, and it is diagnosed when the following four essential criteria are met: 1) the urge to move the legs, usually with unpleasant sensations; 2) the appearance of symptoms during inactivity or rest; 3) relief with movement; and 4) worsening of symptoms in the evening or at night.1 There have been significant recent advances in knowledge of the etiology, pathophysiology, risk factors, and treatment of RLS. The most frequently reported causes of secondary RLS are iron deficiency, neurological lesion on a peripheral nerve or the spinal cord, uremia, and medications, which are frequent medical problems among patients with chronic renal disease.2
Sleep disorders are common among patients undergoing dialysis for end-stage renal disease.3 Patients undergoing regular dialysis frequently complain of insomnia, RLS, sleep-disordered breathing, and excessive daytime sleepiness.3 The prevalence of RLS is higher in dialysis populations than in the general population, but there is a wide variation even after applying unified diagnostic criteria.2,4,5 It is suggested that racial differences in RLS susceptibility, environmental factors such as geographic location, and methodological limitations including small study samples and inconsistent interpretation of diagnostic criteria could result in this wide variation of the prevalence.6,7 Many authors have proposed risk factors for RLS, but many results of previous studies have been inconsistent. Being female, a longer duration of dialysis, iron deficiency, and the use of medications such as tricyclic antidepressant or dopaminergic antagonist have been considered risk factors for RLS among dialysis patients.2 It is important to be aware of the prevalence and risk factors of RLS because the presence of RLS might indicate incorrect dialysis treatment and reduce the quality of life in dialysis patients.8-10 The present study aimed to elucidate the prevalence of RLS in patients undergoing hemodialysis in Korea and to disclose the underlying causative factors.
Methods
Patients who visited any of four outpatient dialysis clinics in Seoul, Korea between September 2005 and May 2006 were included in this study. The patients had to have received regular hemodialysis for at least 3 months. Patients who refused to participate in the study or who were unable to communicate were excluded. A total of 164 out of 321 patients who were receiving regular dialysis treatment were included in this study. Demographic and clinical information was obtained by reviewing patient records. The basic data collected related to the age, gender, duration of dialysis therapy, renal-disease history, comorbid-disease history, body mass index (BMI), and weight. The following laboratory data were also obtained: predialysis blood urea nitrogen (BUN), creatinine, hemoglobin, serum iron, ferritin, total iron-binding capacity (TIBC), phosphate, total calcium, parathyroid hormone (PTH), total bilirubin, alanine aminotransferase (ALT), vitamin B12, and folate. Information was also obtained on the patients' current medications. One of the investigators (J.M.K.) performed face-to-face interviews based on the questionnaire during the dialysis sessions and, if necessary, examined patients to exclude other diseases mimicking RLS. The questionnaire comprised two pages. The first page included the Korean version of the Epworth sleep scale (ESS) and four diagnostic criteria proposed by the International RLS Study Group (IRLS-SG).1 An ESS score greater than nine was considered abnormal. Only patients who fulfilled the four criteria for RLS were asked to complete the second page of the questionnaire. The second page contained the 10-question IRLSSG Rating Scale, which was used to assess symptom severity.11
Continuous data are presented here as mean±standard deviation (SD) values. Univariate analysis was used to compare data between patients with and without RLS. A multivariate logistic model was created with RLS as the dependent variable. We applied Pearson's correlation analysis between multiple variables and scores on the IRLSSG Rating Scale in the patients with RLS. p<0.05 was considered statistically significant. Statistical analysis was carried out using SPSS 12.0 K software.
Results
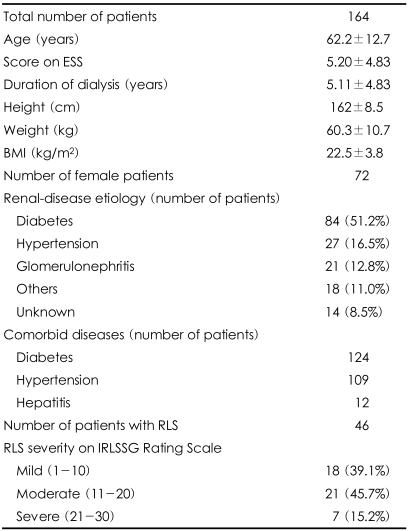
Forty-six (28.0%) of the 164 dialysis patients fulfilled the diagnostic criteria of RLS. The age of the study patients was 62.2±12.7 years. The etiology of renal disease included diabetic nephropathy in 84 patients, hypertensive nephropathy in 27 patients, glomerulonephritis in 21 patients, and miscellaneous conditions (e.g., autosomal dominant polycystic kidney disease, drug-induced nephritis, and paraproteinemia) in 18 patients. The etiology was inconclusive in 14 patients. Erythropoietin was prescribed in 151 (92.1%) patients, oral or parenteral iron supplements were prescribed in 152 patients (92.7%), and vitamin B12 was prescribed in 156 patients (95.1%). None of the patients were treated with a dopa agonist. The basic demographic data of the patients are presented in Table 1.
Table 1.
Baseline characteristics of patients enrolled from four dialysis clinics
ESS: Epworth sleep scale, BMI: body mass index, RLS: restless legs syndrome, IRLSSG: International Restless Legs Syndrome Study Group.
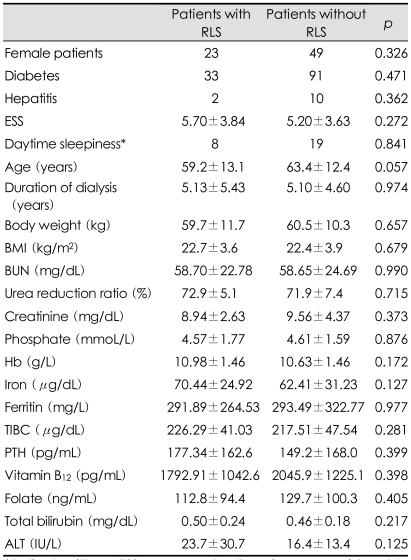
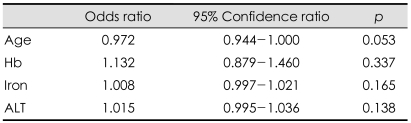
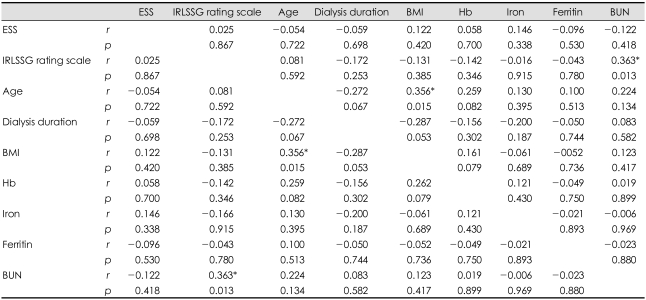
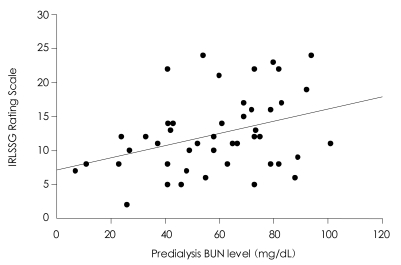
Comparing the clinical characteristics of patients with and without RLS by univariate analysis revealed that none of the variables was associated with the presence of RLS (Table 2). Daytime sleepiness as measured by the ESS did not differ between patients in the RLS and non-RLS groups (p=0.841). We conducted multivariate logistic regression analysis using variables for which the probability was less than 0.20; that is, age, hemoglobin, iron, and ALT (Table 3). None of the variables differed significantly between the RLS and non-RLS groups, but RLS patients tended to be younger (p=0.053). Predialysis BUN level and symptom severity as measured by the IRLSSG Rating Scale were correlated in the RLS group (p=0.05, r=0.363), as indicated in Table 4 and Fig. 1.
Table 2.
Summary of univariate analysis results
*Patients with an ESS score greater than 9 were considered to have daytime sleepiness.
RLS: restless legs syndrome, ESS: Epworth sleep scale, BMI: body mass index, BUN: blood urea nitrogen, Hb: hemoglobin, TIBC: total iron-binding capacity, PTH: parathyroid hormone, ALT: alanine aminotransferase.
Table 3.
Results of multivariate analysis of risk factors for RLS
RLS: restless legs syndrome, Hb: hemoglobin, ALT: alanine aminotransferase.
Table 4.
Results of pearson's correlation analysis
*p<0.05.
ESS: Epworth sleep scale, IRLSSG: International Restless Legs Syndrome Study Group, BMI: body mass index, Hb: hemoglobin, BUN: blood urea nitrogen.
Fig. 1.
The predialysis blood urea nitrogen (BUN) level was significantly correlated with scores on the IRLSSG (International Restless Legs Syndrome Study Group) Rating Scale.
Discussion
This study revealed that the frequency of RLS among dialysis patients in Korea is 28.0%, which is markedly higher than the prevalence of RLS in the general Korean population (12.1%).12 The diagnosis of RLS in this study was based on the four strict criteria proposed by the IRLSSG, and the patients were examined by an experienced neurologist in face-to-face interviews, which made the diagnoses highly reliable. The prevalence of RLS in our Korean population was higher than that reported for populations in Japan (12.2%) and India (6.6%), lower than that reported for China (62%),4,5,13 and similar to that reported for Chile (25.9%) and Italy (21.5%).14,15 This wide variation suggests different susceptibilities to RLS or methodological differences in study populations.2,6,7
Many studies have recently been conducted in dialysis clinics to clarify the risk factors for RLS, but the results have varied widely. We found no significant association between RLS and any of the following factors: age, gender, duration of dialysis, comorbid diseases, BMI, and laboratory data including hemoglobin, BUN, creatinine, iron, ferritin, TIBC, PTH, folate, phosphate, ALT, and total bilirubin. One of the interesting results of this study is that the predialysis BUN level was significantly correlated with symptom severity in the RLS group, although the predialysis BUN level did not differ between the RLS and non-RLS groups. The predialysis BUN level is not a recommended indicator of dialysis efficiency or disease severity because it is easily influenced by protein intake, body volume, and energy metabolism.16 Our results suggest that factors other than dialysis adequacy-such as dietary protein intake, recent infection, or body volume-are related to worsening of RLS. These factors might not play a major role in RLS development, but they could aggravate RLS symptoms once the syndrome appears. Detailed clinical data including body weight change, medication profile, and diet might help to disclose the underlying mechanism. Iron-deficiency anemia is a well-known risk factor for RLS, and the level of serum ferritin is known to be correlated with RLS severity in some RLS patients, suggesting a close relationship between iron metabolism and the pathophysiology of RLS.2 However, this relationship is less clear in RLS among dialysis patients, presumably due to the routine use of iron supplementation in this population.2,17 In our study, 92.7% of all patients were regularly supplemented with iron, and this could have alleviated the effects of hemoglobin, iron, and ferritin. The level of ferritin was also not correlated with symptom severity. Routine supplementation with iron could also explain the large proportion of patients with mild RLS (39.1%) in the RLS group. Aging is also believed to be a risk factor for idiopathic RLS.18 However, previous studies have shown that this is not always true in RLS patients undergoing dialysis.19 The RLS patients in our study tended to be younger, which suggests that RLS-inducing factors are stronger than the aging effect in dialysis patients. Some studies have found a female preponderance in RLS, while others have found no gender difference or even a possible male predominance in RLS.20,21 We found no female predominance in our RLS patients. The duration of dialysis therapy is generally regarded as a risk factor for RLS,22 but this was not evident in our study. We also could found no association between a high BMI and RLS in our dialysis patients.17,21
Daytime sleepiness as measured by the ESS did not differ between the two groups in the present study, which is inconsistent with previous reports.3,23 Since our study population included many diabetic patients, the accompanying retinopathy prevented us from obtaining accurate ESS scores because such patients are unable to drive a car, watch TV, or read newspapers. Therefore, this might not be an appropriate modality for assessing sleep disturbance in diabetic patients.
A previous study suggested that the prevalence of RLS among dialysis patients in Korea was 44.0%.24 The lower prevalence found in our study might be due to our method of face-to-face questioning combined with a neurological examination yielding more accurate diagnoses than those based on questionnaires and different biological properties, includeing age and duration of dialysis. Questionnaire-based diagnoses of RLS might be unreliable in uremic patients due to low sensitivity and specificity.25 False-positive results appear to be caused by the presence of other leg-related symptoms and neurologically objective signs suggestive of peripheral neuropathy.25
Our study had some limitations. The first is the inevitable selection bias from collecting data from only 164 out of a total of 321 patients. The main cause of exclusion was communication difficulties, which might have excluded all of the most severe patients. The second limitation was insufficient data on medication history. Our patients were taking many drugs, including benzodiazepines, gabapentin, tricyclic antidepressants, and calcium-channel antagonists, and we could not rule out their role in RLS. Finally, we did not obtain data on nerve conduction parameters because most of the patients did not agree to undergo such investigations. However, we attempted to exclude other diseases that could mimic RLS by performing a structured interview and neurological examination.
RLS is common in patients undergoing regular hemodialysis. More attention to this disease might aid its detection and reduce patient discomfort. Further studies are needed to disclose its detailed risk factors and the pathophysiological role of the BUN level in RLS.
References
- 1.Walters AS. Toward a better definition of the restless legs syndrome. The International Restless Legs Syndrome Study Group. Mov Disord. 1995;10:634–642. doi: 10.1002/mds.870100517. [DOI] [PubMed] [Google Scholar]
- 2.Kavanagh D, Siddiqui S, Geddes CC. Restless legs syndrome in patients on dialysis. Am J Kidney Dis. 2004;43:763–771. doi: 10.1053/j.ajkd.2004.01.007. [DOI] [PubMed] [Google Scholar]
- 3.Merlino G, Piani A, Dolso P, Adorati M, Cancelli I, Valente M, et al. Sleep disorders in patients with end-stage renal disease undergoing dialysis therapy. Nephrol Dial Transplant. 2006;21:184–190. doi: 10.1093/ndt/gfi144. [DOI] [PubMed] [Google Scholar]
- 4.Bhowmik D, Bhatia M, Gupta S, Agarwal SK, Tiwari SC, Dash SC. Restless legs syndrome in haemodialysis patients in India: a case controlled study. Sleep Med. 2003;4:143–146. doi: 10.1016/s1389-9457(03)00005-4. [DOI] [PubMed] [Google Scholar]
- 5.Hui DS, Wong TY, Ko FW, Li TS, Choy DK, Wong KK, et al. Prevalence of sleep disturbances in Chinese patients with end-stage renal failure on continuous ambulatory peritoneal dialysis. Am J Kidney Dis. 2000;36:783–788. doi: 10.1053/ajkd.2000.17664. [DOI] [PubMed] [Google Scholar]
- 6.Berger K, Kurth T. RLS epidemiology--frequencies, risk factors and methods in population studies. Mov Disord. 2007;22(Suppl 18):s420–s423. doi: 10.1002/mds.21589. [DOI] [PubMed] [Google Scholar]
- 7.Castillo PR, Kaplan J, Lin SC, Fredrickson PA, Mahowald MW. Prevalence of restless legs syndrome among native South Americans residing in coastal and mountainous areas. Mayo Clin Proc. 2006;81:1345–1347. doi: 10.4065/81.10.1345. [DOI] [PubMed] [Google Scholar]
- 8.Winkelman JW, Chertow GM, Lazarus JM. Restless legs syndrome in end-stage renal disease. Am J Kidney Dis. 1996;28:372–378. doi: 10.1016/s0272-6386(96)90494-1. [DOI] [PubMed] [Google Scholar]
- 9.Unruh ML, Levey AS, D'Ambrosio C, Fink NE, Powe NR, Meyer KB, et al. Restless legs symptoms among incident dialysis patients: association with lower quality of life and shorter survivial. Am J Kidney Dis. 2004;43:900–909. doi: 10.1053/j.ajkd.2004.01.013. [DOI] [PubMed] [Google Scholar]
- 10.Mucsi I, Molnar MZ, Ambrus C, Szeifert L, Kovacs AZ, Zoller R, et al. Restless legs syndrome, insomnia and quality of life in patients on maintenance dialysis. Nephrol Dial Transplant. 2005;20:571–577. doi: 10.1093/ndt/gfh654. [DOI] [PubMed] [Google Scholar]
- 11.Walters AS, LeBrocq C, Dhar A, Hening W, Rosen R, Allen RP, et al. Validation of the International Restless Legs Syndrome Study Group rating scale for restless legs syndrome. Sleep Med. 2003;4:121–132. doi: 10.1016/s1389-9457(02)00258-7. [DOI] [PubMed] [Google Scholar]
- 12.Kim J, Choi C, Shin K, Yi H, Park M, Cho N, et al. Prevalence of restless legs syndrome and associated factors in the Korean adult population: the Korean Health and Genome Study. Psychiatry Clin Neurosci. 2005;59:350–353. doi: 10.1111/j.1440-1819.2005.01381.x. [DOI] [PubMed] [Google Scholar]
- 13.Takaki J, Nishi T, Nangakku M, Shimoyama H, Inada T, Matsuyama N, et al. Clinical and psychological aspects of restless legs syndrome in uremic patients on hemodialysis. Am J Kidney Dis. 2003;41:833–839. doi: 10.1016/s0272-6386(03)00031-3. [DOI] [PubMed] [Google Scholar]
- 14.Miranda M, Araya F, Castillo JL, Durán C, González F, Arís L. [Restless legs syndrome: a clinical study in adult general population and in uremic patients] Rev Med Chil. 2001;129:179–186. [PubMed] [Google Scholar]
- 15.Gigli GL, Adorati M, Dolso P, Piani A, Valente M, Brotini S, et al. Restless legs syndrome in end-stage renal disease. Sleep Med. 2004;5:309–315. doi: 10.1016/j.sleep.2004.01.014. [DOI] [PubMed] [Google Scholar]
- 16.Locatelli F, Buoncristiani U, Canaud B, Köhler H, Petitclerc T, Zucchelli P. Dialysis dose and frequency. Nephrol Dial Transplant. 2005;20:285–296. doi: 10.1093/ndt/gfh550. [DOI] [PubMed] [Google Scholar]
- 17.Siddiqui S, Kavanagh D, Traynor J, Mak M, Deighan C, Geddes C. Risk factors for restless legs syndrome in dialysis patients. Nephron Clin Pract. 2005;101:c155–c160. doi: 10.1159/000087073. [DOI] [PubMed] [Google Scholar]
- 18.Rothdach AJ, Trenkwalder C, Haberstock J, Keil U, Berger K. Prevalence and risk factors of RLS in an elderly population: the MEMO study. Memory and Morbidity in Augsburg Elderly. Neurology. 2000;54:1064–1068. doi: 10.1212/wnl.54.5.1064. [DOI] [PubMed] [Google Scholar]
- 19.Kawauchi A, Inoue Y, Hashimoto T, Tachibana N, Shirakawa S, Mizutani Y, et al. Restless legs syndrome in hemodialysis patients: health-related quality of life and laboratory data analysis. Clin Nephrol. 2006;66:440–446. doi: 10.5414/cnp66440. [DOI] [PubMed] [Google Scholar]
- 20.Kageyama T, Kabuto M, Nitta H, Kurokawa Y, Taira K, Suzuki S, et al. Prevalence of periodic limb movement-like and restless legs-like symptoms among Japanese adults. Psychiatry Clin Neurosci. 2000;54:296–298. doi: 10.1046/j.1440-1819.2000.00685.x. [DOI] [PubMed] [Google Scholar]
- 21.Phillips B, Young T, Finn L, Asher K, Hening WA, Purvis C. Epidemiology of restless legs symptoms in adults. Arch Intern Med. 2000;160:2137–2141. doi: 10.1001/archinte.160.14.2137. [DOI] [PubMed] [Google Scholar]
- 22.Telarović S, Relja M, Trkulja V. Restless legs syndrome in hemodialysis patients: association with calcium antagonists. A preliminary report. Eur Neurol. 2007;58:166–169. doi: 10.1159/000104718. [DOI] [PubMed] [Google Scholar]
- 23.Holmes R, Tluk S, Metta V, Patel P, Rao R, Williams A, et al. Nature and variants of idiopathic restless legs syndrome: observations from 152 patients referred to secondary care in the UK. J Neural Transm. 2007;114:929–934. doi: 10.1007/s00702-006-0614-3. [DOI] [PubMed] [Google Scholar]
- 24.Cho YW, Lee H, Lee JH, Han SY, Lee MY. Sleep disorders in Maintenance dialysis patients with end-stage renal disease. J Korean Neurol Assoc. 2003;21:492–497. [Google Scholar]
- 25.Cirignotta F, Mondini S, Santoro A, Ferrari G, Gerardi R, Buzzi G. Reliability of a questionnaire screening restless legs syndrome in patients on chronic dialysis. Am J Kidney Dis. 2002;40:302–306. doi: 10.1053/ajkd.2002.34508. [DOI] [PubMed] [Google Scholar]