Abstract
Background and purpose
The advances in the diagnosis and treatment of acute stroke increase the importance of providing these patients with timely medical attention. This study was designed to assess time delays in neurological evaluation and neuroimaging and to determine whether they are important obstacles to performing thrombolytic therapy.
Methods
Data were obtained between May 2004 and September 2006 from 195 consecutive patients who were admitted to Cheju National University Hospital for acute ischemic stroke within 24 hours of the onset of symptoms. We determined the time of the onset of symptoms, arrival time at the emergency department (ED), and times of neurology notification, neurology evaluation, and neuroimaging using interviews and by reviewing the medical record.
Results
Short onset-to-door time, performing computed tomography rather than magnetic resonance imaging, presence of aphasia or motor weakness, and severe initial neurological deficit were significantly associated with reduced in-hospital delays. Seventeen (20%) of the 85 patients who arrived within 3 hours of the onset of symptoms received intravenous thrombolysis. Mild neurological deficit, rapidly improving symptoms, and insufficient time to workup were the main causes of the nonreceipt of thrombolytic therapy in these patients. Only one patient did not receive thrombolytic therapy due to delay in neurology consultation.
Conclusions
Whilst in-hospital delays were not major obstacles to performing thrombolytic therapy in this study, there is still a high probability of missing patients with mild-to-moderate stroke symptoms. More effective in-hospital organization is required for the prompt evaluation and treatment of patients with acute ischemic stroke.
Keywords: Cerebrovascular disorders, Thrombolytic therapy, Time factor, Emergency service
INTRODUCTION
Thrombolytic therapy with recombinant tissue plasminogen activator (rt-PA) is the only proven treatment for ischemic stroke, when it is administered within 3 hours of the onset of symptoms.1,2 Although 15-56% of the patients with acute ischemic stroke arrive at the emergency department (ED) within 3 hours of the onset of symptoms, currently only 2-8% of these patients receive thrombolytic therapy.3-5 A substantial proportion of patients who arrive early do not receive thrombolytic therapy due to avoidable reasons such as delays in physician evaluation and neuroimaging, incorrect application of criteria, and incorrect diagnosis.6-9 According to the guidelines for identifying and treating acute stroke,10 patients with acute stroke should be examined or notified to stroke expertise within 15 minutes of arrival at the ED. A computed tomography (CT) scan should be performed within 25 minutes, and the specific drug should be infused within 60 minutes. CT has been the principal neuroimaging modality in many previous studies investigating in-hospital delays in stroke therapy. 11-15 However, the development of multimodal magnetic resonance imaging (MRI) has led to this being increasingly used as the initial neuroimaging modality in acute stroke management. The aim of this study was to quantify the time delays in physician evaluation and neuroimaging in patients with acute stroke and to determine whether they are important obstacles to performing thrombolytic therapy.
MATERIALS AND METHODS
1. Study design, setting, and selection of participants
Cheju National University Hospital is a teaching university hospital located in the center of Jeju city, which has a population of 300,000. In our hospital, CT scanning is readily available 24 hours a day, but MRI is performed by a technologist who is not in-house from 1800 to 0800. Currently we do not have any specific stroke protocol for the rapid evaluation and treatment of patients with acute stroke. Our hospital has an ongoing prospective stroke registry for patients who are admitted this hospital within 7 days of the onset of symptoms, which was implemented in May 2004. In this study, we limited the study population to those who presented within 24 hours of the onset of symptoms because this group of acute stroke patients would more clearly show the acute stroke management in our hospital. Clinical variables including age, sex, mode of transportation, referral method, and subtype of ischemic stroke, National Institutes of Health Stroke Scale (NIHSS) score, vascular risk factors, and types of specific treatment were collected from the ongoing prospective stroke registry. Subtypes of ischemic stroke were determined according to the classification of the Trial of Org 10172 in Acute Stroke Treatment.16 The main symptoms of the patients were categorized into motor weakness, sensory deficit, disturbance of consciousness, aphasia, visual disturbance, eye movement abnormality, dizziness or ataxia, and headache.
2. Methods of measurement and data collection
The onset time was defined as the first time that the patient or an observer noticed a neurological deficit such as aphasia, motor weakness, or disturbance of consciousness. If symptoms were present upon awakening, the onset time was considered as the midpoint between falling asleep or the last time the patient had no symptoms and awakening. The door-to-neurology notification time (DNNT) was defined as the time delay between arrival at the ED and the time when the ED physician or duty intern notified the patient to neurology. The door-to-neurology evaluation time (DNET) was the time delay between arrival at the ED and the time that neurologist or neurology resident examined the patient. The door-to-neuroimaging time (DNIT) was the time delay between arrival at the ER and the time that reads on the first image of the scan. One of the authors (Y.J.K.) interviewed all the patients after admission, but when the patient was unable to communicate due to aphasia or severe deficits, the interviewer collected the information from a family member. The exact onset time, referral method, method of transportation, and history of stroke were collected by interview. We investigated whether or not patients who arrived within 3 hours of the onset of symptoms received intravenous thrombolytic therapy. When the patient did not receive the treatment, we investigated the possible reasons. DNNT, DNET, DNIT, and the reasons for nonreceipt of thrombolytic therapy were collected retrospectively using medical records and the stroke registry. We divided the patients into two groups based whether the onset-to-door time was less than 3 hours (group 1) or 3-24 hours (group 2), because this time is critical to thrombolytic therapy.
3. Statistical analysis
We used a descriptive analysis for general characteristics of the patients. Because DNNT, DNET, and DNIT were not normally distributed, we used medians as the representative values and analyzed them using the Mann-Whitney U test or Kruskal-Wallis test in relation to age, gender, onset-to-door time, referral method, type of initial neuroimaging, subtype of ischemic stroke, presence of aphasia or motor weakness, initial NIHSS score, and acute treatments. For the variables that showed significant results on univariate analysis, we performed linear regression analysis for DNNT, DNET, and DNIT. All analyses were performed using SPSS (version 10.0), and a probability value of p < 0.05 was considered to be indicative of statistical significance.
RESULTS
1. Clinical characteristics and demographic data
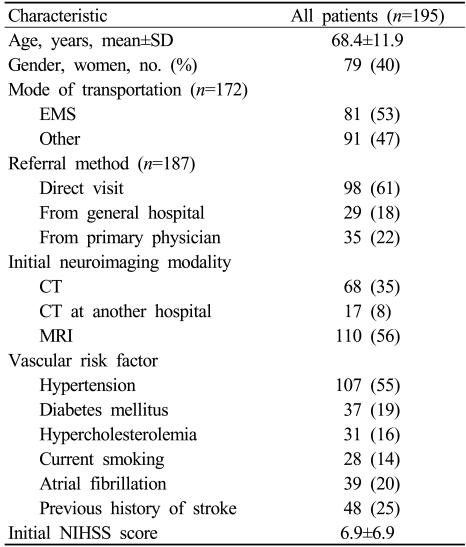
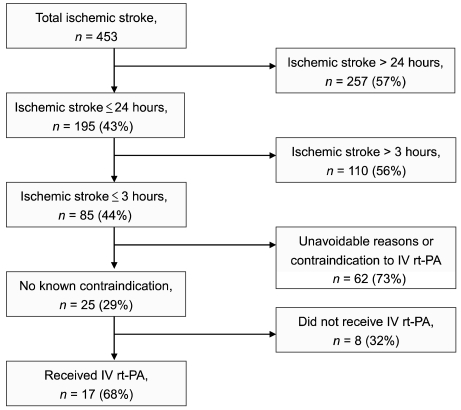
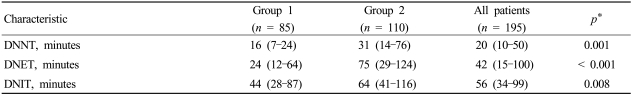
Between May 1, 2004 and September 30, 2006, 453 consecutive patients with acute ischemic stroke were admitted to Cheju National University Hospital within 7 days of the onset of symptoms, of which the 195 patients (43%) who visited the ED within 24 hours became the subjects of this study (Table 1). Eighty-five patients (44%) arrived at the hospital within 3 hours of the onset of symptoms (Fig. 1). Eighty-nine percent of the patients had cerebral infarctions and 11% had transient ischemic attacks. Large-artery atherosclerosis was the most frequent stroke subtype (30%), followed by cardioembolism (29%), stroke of undetermined etiology (21%), and small-vessel occlusion (19%). Seventeen patients (8.7%) received intravenous thrombolysis, of which seven patients also underwent combined intra-arterial thrombolysis. DNNT, DNET, and DNIT were significantly delayed in patients who arrived more than 3 hours after the onset of symptoms (Table 2).
Table 1.
Characteristics of the study patients.
CT; computed tomography, EMS; emergency medical service, NIHSS; National Institutes of Health Stroke Scale, MRI; magnetic resonance imaging.
Figure 1.
Admissions for acute ischemic stroke at Cheju National University Hospital during the study period. Times are relative to the onset of symptoms.
IV; intravenous, rt-PA; recombinant tissue plasminogen activator.
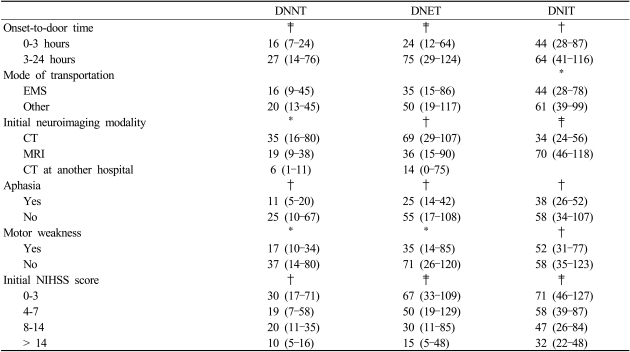
Table 2.
Values of the door-to-neurology notification time (DNNT), door-to-neurology evaluation time (DNET), and door-to-neuroimaging time (DNIT)
Values are medians and interquartile ranges.
*Group 1 vs. group 2 by Mann-Whitney U test.
2. Door-to-neurology evaluation time and door-to-neuroimaging time
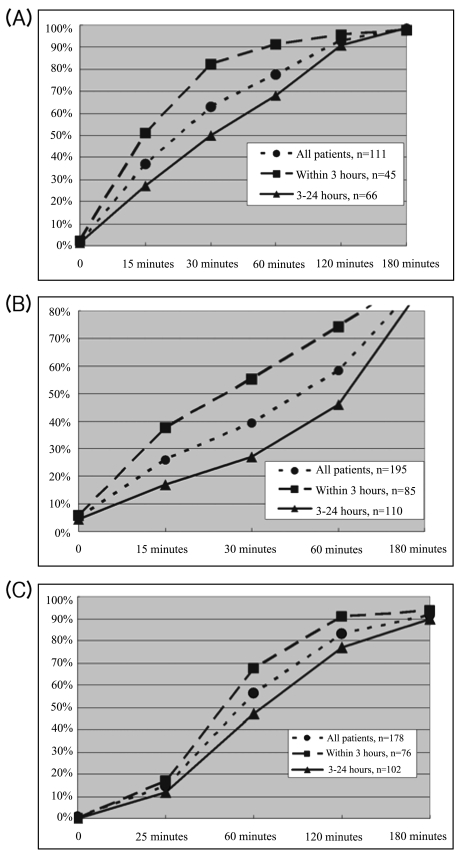
1) Door-to-neurology notification time (Fig. 2-A)
Figure 2.
Cumulative percentages of the patients according to values of the DNNT (A), DNET (B), and DNIT (C).
We were unable to determine the exact time of notification from the medical records of 111 patients. Overall, 37% of the patients were notified within 15 minutes: 51% and 27% in groups 1 and 2, respectively.
2) Door-to-neurology evaluation time (Fig. 2-B)
Twenty-six percent of the patients received a neurology evaluation by a neurology resident or a neurologist within 15 minutes of arrival at the ED. The median time between notification and neurology evaluation was 10 minutes for group 1 and 20 minutes for group 2.
3) Door-to-neuroimaging time (Fig. 2-C)
Seventeen patients who were referred from another general hospital after performing CT were excluded from the analysis. Overall, CT or MRI was performed within 25 minutes in only 15% of the patients. Seventeen percent of the patients in group 1 underwent neuroimaging within 25 minutes, even though they arrived at the ED within 3 hours of the onset of symptoms. The median time delays to performing CT and MRI were 34 and 69 minutes, respectively.
4) Univariate analysis
The onset-to-door time (dichotomized into within 3 hours and longer), type of initial neuroimaging (CT or MRI), presence of aphasia or motor weakness, and initial NIHSS score were significantly associated with DNNT, DNET, and DNIT (Table 3).
Table 3.
Factors related to DNNT, DNET, and DNIT: univariate analysis
Values (in minutes) are medians and interquartile ranges.
*p < 0.05, †p < 0.01, ‡p < 0.001 within the diagnostic groups as measured by a Mann-Whitney U test or Kruskal-Wallis test.
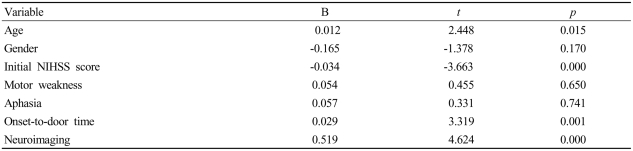
5) Multivariate analysis
Because DNNT, DNET, and DNIT did not exhibit normal distributions, we used their natural logarithmic values as dependent variables. Age, gender, and all other factors that showed significant results from univariate analysis were included in the multivariate analysis. The adjusted values of R2 for DNNT, DNET, and DNIT were 0.315, 0.218, and 0.222, respectively. The onset-to-door time, type of the initial neuroimaging, and initial NIHSS score significantly affected DNIT (Table 4).
Table 4.
Factors related to DNNT, DNET, and DNIT: multivariate analysis
B is the unstandardized coefficient, and t represents B divided by the standard error.
Age, onset-to-door time (in hours), and NIHSS score were analyzed as continuous variables. Gender, motor weakness (yes/no), aphasia (yes/no), and neuroimaging modality (CT/MRI) were entered as dichotomous variables.
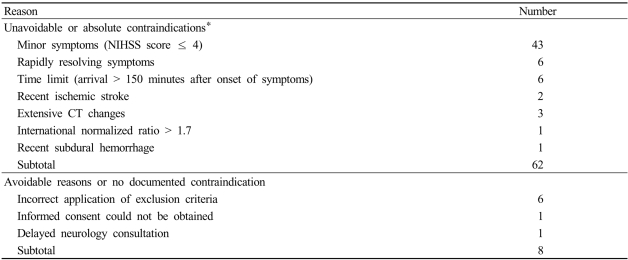
3. Rate of receiving thrombolytic therapy
Seventeen (20%) of the 85 patients who arrived within 3 hours of the onset of symptoms received intravenous thrombolysis. The mean and median times from ED arrival to infusion (the door-to-needle time) were 76 and 80 minutes, respectively. Six patients (35%) received thrombolytic therapy within 60 minutes, and this increased to 15 patients (94%) within 120 minutes. Most of the remaining 68 patients who did not receive thrombolytic therapy were excluded due to mild neurological deficit (NIHSS score ≤ 4), rapidly improving symptoms, insufficient time to workup, and other unavoidable reasons. Eight patients did not receive the treatment due to avoidable reasons including incorrect application of criteria and not obtaining informed consent, with the reason being delay in neurology consultation in one case (Table 5).
Table 5.
Reasons for nonreceipt of thrombolytic treatment (n = 68)
*Some patients had more than one exclusion.
DISCUSSION
This study revealed considerable in-hospital delays in neurology evaluation and neuroimaging relative to suggested guidelines. Overall, 37% of the patients were notified within 15 minutes, and only 26% of the patients received a neurology evaluation by a neurology resident or a neurologist within 15 minutes of arrival at the ED. Neuroimaging started within 25 minutes in only 15% of the patients. Only 8.7% and 20% of ischemic stroke patients who visited an ED within 24 hours and within 3 hours of the onset of symptoms, respectively, received rt-PA. Most patients who arrived early were excluded from thrombolytic therapy due to the presence of unavoidable reasons or absolute contraindications.
Previous studies found that minor neurologic deficits and rapidly improving symptoms were important reasons for the nonreceipt of thrombolytic therapy by patients who arrived early after the onset of symptoms. Other frequently reported absolute contraindications have been recent stroke, presence of intracerebral hemorrhage, bleeding tendency, high blood pressure, and early CT changes.5-9 However, 24-26% of patients reportedly did not receive thrombolytic therapy due to avoidable reasons such as delays in neurology evaluation or neuroimaging, incorrect diagnoses, and incorrect application of criteria.6-8 In the present study, in 12% of cases the patients did not receive thrombolytic therapy due to avoidable reasons such as incorrect application of criteria, not obtaining informed consent, and delayed neurology consultation. Although this represents a relatively small proportion of the patients, such avoidable factors are very important in acute-stroke management because, unlike absolute or unavoidable reasons, these problems can be resolved by educating personnel and making changes to hospital procedures.
The reported DNET and DNIT have varied greatly between studies due to different conditions, but many researchers have found that the severity of neurological deficit, use of an emergency medical service (EMS), and short onset-to-door time were significantly associated with reducing DNET or DNIT.11-15,17 The severity of neurological deficit and onset-to-door time also significantly affected DNET and DNIT in the present study. Fifty-three percent of the patients used an EMS in this study. Although such use tended to reduce the onset-to-door time, DNET, and DNIT, the difference did not reach statistical significance, possibly because an EMS was used more frequently by patients who arrived later in this study.
MRI is more sensitive than CT in diagnosing acute ischemic stroke and is also useful for detecting hemorrhage.18,19 Multimodal MRI can provide more details of ischemic tissue and thus may lengthen therapeutic windows in the acute treatment of ischemic stroke without increasing the incidence of cerebral hemorrhage.20 However, it is generally more expensive, time-consuming, and requires more knowledge for accurate interpretations. MRI was the initial neuroimaging modality in 56% of the patients in this study, and the rate of performing MRI did not differ significantly between patients who arrived within 3 hours of the onset of symptoms and those who arrived later than 3 hours. However, the median time delays to performing CT and MRI were 34 and 69 minutes, respectively, and the use of MRI significantly increased DNIT. Five of the 17 patients who received thrombolytic therapy underwent MRI as their initial neuroimaging modality, and the door-to-imaging time did not differ significantly between CT and MRI in these patients. However, screening all the patients with MRI before thrombolytic treatment would significantly delay neuroimaging because in our hospital MRI is performed by a technologist who is not present during the nighttime. The availability of MRI 24 hours a day reportedly results in no difference in the door-to-imaging time between CT and MRI.18,21
Despite the presence of such prominent in-hospital delays, only a small proportion of our patients were excluded from thrombolytic therapy due these delays or other avoidable reasons. Because most patients who received thrombolytic therapy had severe neurological deficits (mean initial NIHSS score = 14.29), they were evaluated more rapidly than other patients. However, if patients present with only mild-to-moderate stroke symptoms (e.g., NIHSS score of 5-14), they may not receive thrombolytic therapy due to delays in physician evaluation and neuroimaging. Because stroke treatment is more effective when it is initiated earlier, we should therefore attempt to reduce door-to-physician evaluation or neuroimaging time as well as onset-to-door time. The main problem of the current system at our hospital is that DNET and DNIT are greatly affected by the severity of the stroke. Therefore, we need to organize our stroke team and develop a specific protocol so that every acute-stroke patient receives rapid evaluation and treatment.
This study was subject to several limitations. First, the study was performed at a single center, which may limit the generalizability of its findings. Second, we obtained all the in-hospital data retrospectively and many data on neurology notifications were not available. Because the purpose of this study was to quantify time delays in physician evaluation and neuroimaging at our hospital and to provide baseline data for organizing the stroke team and developing a specific protocol, DNET and DNIT might have been shorter (and more accurate) if we had collected the data prospectively. Third, the overall multivariate statistical models for DNET and DNIT showed only moderate correlations, suggesting that significant predictive variables were omitted from the analyses.
In conclusion, we found significant delays in neurology evaluation and neuroimaging of patients with acute ischemic stroke in this study. Although such in-hospital delays were not major obstacles to performing thrombolytic therapy, there is a greater probability of missing patients with mild-to-moderate stroke symptoms. More effective in-hospital organization is required to ensure the prompt evaluation and treatment of patients with acute ischemic stroke.
Footnotes
The authors report no conflicts of interest and there is nothing to disclosure on financial support.
References
- 1.The National Institute of Neurological Disorders and Stroke rt-PA Stroke study group. Tissue plasminogen activator for acute ischemic stroke. N Engl J Med. 1995;333:1581–1587. doi: 10.1056/NEJM199512143332401. [DOI] [PubMed] [Google Scholar]
- 2.Hacke W, Donnan G, Fieschi C, Kaste M, von Kummer R, Broderick JP, et al. Association of outcome with early stroke treatment: pooled analysis of ATLANTIS, ECASS, and NINDS rt-PA stroke trials. Lancet. 2004;363:768–774. doi: 10.1016/S0140-6736(04)15692-4. [DOI] [PubMed] [Google Scholar]
- 3.Reeves MJ, Arora S, Broderick JP, Frankel M, Heinrich JP, Hickenbottom S, et al. Acute stroke care in the US: results from 4 pilot prototypes of the Paul Coverdell National Acute Stroke Registry. Stroke. 2005;36:1232–1240. doi: 10.1161/01.STR.0000165902.18021.5b. [DOI] [PubMed] [Google Scholar]
- 4.Schenkel J, Weimar C, Knoll T, Haberl RL, Busse O, Hamann GF, et al. R1 - systemic thrombolysis in German stroke units - the experience from the German Stroke data bank. J Neurol. 2003;250:320–324. doi: 10.1007/s00415-003-1004-5. [DOI] [PubMed] [Google Scholar]
- 5.Kleindorfer D, Kissela B, Schneider A, Woo D, Khoury J, Miller R, et al. Eligibility for recombinant tissue plasminogen activator in acute ischemic stroke: a population-based study. Stroke. 2004;35:e27–e29. doi: 10.1161/01.STR.0000109767.11426.17. [DOI] [PubMed] [Google Scholar]
- 6.Barber PA, Zhang J, Demchuk AM, Hill MD, Buchan AM. Why are stroke patients excluded from TPA therapy? An analysis of patient eligibility. Neurology. 2001;56:1015–1020. doi: 10.1212/wnl.56.8.1015. [DOI] [PubMed] [Google Scholar]
- 7.Cocho D, Belvis R, Marti-Fabregas J, Molina-Porcel L, Diaz-Manera J, Aleu A, et al. Reasons for exclusion from thrombolytic therapy following acute ischemic stroke. Neurology. 2005;64:719–720. doi: 10.1212/01.WNL.0000152041.20486.2F. [DOI] [PubMed] [Google Scholar]
- 8.Katzan IL, Hammer MD, Hixson ED, Furlan AJ, Abou-Chebl A, Nadzam DM. Utilization of intravenous tissue plasminogen activator for acute ischemic stroke. Arch Neurol. 2004;61:346–350. doi: 10.1001/archneur.61.3.346. [DOI] [PubMed] [Google Scholar]
- 9.Huang P, Chen CH, Yang YH, Lin RT, Lin FC, Liu CK. Eligibility for recombinant tissue plasminogen activator in acute ischemic stroke: way to endeavor. Cerebrovasc Dis. 2006;22:423–428. doi: 10.1159/000094994. [DOI] [PubMed] [Google Scholar]
- 10.National Institute of Neurological Disorders and Stroke. Proceedings of a national symposium on rapid identification and treatment of acute stroke; Washington: 1997. [Google Scholar]
- 11.Kothari R, Jauch E, Broderick J, Brott T, Sauerbeck L, Khoury J, et al. Acute stroke: delays to presentation and emergency department evaluation. Ann Emerg Med. 1999;33:3–8. doi: 10.1016/s0196-0644(99)70431-2. [DOI] [PubMed] [Google Scholar]
- 12.Bratina P, Greenberg L, Pasteur W, Grotta JC. Current emergency department management of stroke in Houston, Texas. Stroke. 1995;26:409–414. doi: 10.1161/01.str.26.3.409. [DOI] [PubMed] [Google Scholar]
- 13.Wester P, Radberg J, Lundgren B, Peltonen M, Seek-Medical-Attention-in-Time Study Group Factors associated with delayed admission to hospital and in-hospital delays in acute stroke and TIA: a prospective, multicenter study. Stroke. 1999;30:40–48. doi: 10.1161/01.str.30.1.40. [DOI] [PubMed] [Google Scholar]
- 14.Morris DL, Rosamond WD, Hinn AR, Gorton RA. Time delays in accessing stroke care in the emergency department. Acad Emerg Med. 1999;6:218–223. doi: 10.1111/j.1553-2712.1999.tb00159.x. [DOI] [PubMed] [Google Scholar]
- 15.Morris DL, Rosamond W, Madden K, Schultz C, Hamilton S. Prehospital and emergency department delays after acute stroke: The Genentech Stroke Presentation Survey. Stroke. 2000;31:2585–2590. doi: 10.1161/01.str.31.11.2585. [DOI] [PubMed] [Google Scholar]
- 16.Adams HP, Bendixen BH, Kappelle LJ, Biller J, Love BB, Gordon DL, et al. Classification of subtype of acute ischemic stroke. Definitions for use in a multicenter clinical trial. TOAST. Trial of Org 10172 in Acute Stroke Treatment. Stroke. 1993;24:35–41. doi: 10.1161/01.str.24.1.35. [DOI] [PubMed] [Google Scholar]
- 17.Jungehulsing GJ, Rossnagel K, Nolte CH, Muller-Nordhorn J, Roll S, Klein M, et al. Emergency department delays in acute stroke - analysis of time between ED arrival and imaging. Eur J Neurol. 2006;13:225–232. doi: 10.1111/j.1468-1331.2006.01170.x. [DOI] [PubMed] [Google Scholar]
- 18.Chalela JA, Kidwell CS, Nentwich LM, Luby M, Butman JA, Demchuk AM, et al. Magnetic resonance imaging and computed tomography in emergency assessment of patients with suspected acute stroke: a prospective comparison. Lancet. 2007;369:293–298. doi: 10.1016/S0140-6736(07)60151-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sims J, Schwamm LH. The evolving role of acute stroke imaging in intravenous thrombolytic therapy: patient selection and outcomes assessment. Neuroimaging Clin N Am. 2005;15:421–440. xii. doi: 10.1016/j.nic.2005.06.001. [DOI] [PubMed] [Google Scholar]
- 20.Thomalla G, Schwark C, Sobesky J, Bluhmki E, Fiebach JB, Fiehler J, et al. Outcome and symptomatic bleeding complications of intravenous thrombolysis within 6 hours in MRI-selected stroke patients: comparison of a German multicenter study with the pooled data of ATLANTIS, ECASS, and NINDS tPA trials. Stroke. 2006;37:852–858. doi: 10.1161/01.STR.0000204120.79399.72. [DOI] [PubMed] [Google Scholar]
- 21.Kang DW, Chalela JA, Dunn W, Warach S, NIH-Suburban Stroke Center Investigators MRI screening before standard tissue plasminogen activator therapy is feasible and safe. Stroke. 2005;36:1939–1943. doi: 10.1161/01.STR.0000177539.72071.f0. [DOI] [PubMed] [Google Scholar]