Abstract
We describe a 64-year-old man with scrub typhus who presented with both polyneuropathy and cerebral infarction. A eurological examination revealed a confused mental state, stiff neck, hearing impairment, symmetric weakness, sensory loss, and ataxia. Electrophysiologic studies showed demyelinating sensorimotor polyneuropathy and sensorineural hearing loss. Brain magnetic resonance imaging showed multiple infarctions. Brain involvement or polyneuropathy associated with scrub typhus has been rarely reported, and the pathogenic mechanism underlying the multiple neurological complications remains to be elucidated.
Keywords: Scrub typhus, Guillain-Barré syndrome, Cerebral infarction
Scrub typhus is a febrile illness caused by Orientia tsutsugamushi, and is characterized by fever, rash, eschar, myocarditis, and pneumonitis. Neurological involvement usually includes meningitis and hearing loss, possibly due to involvement of the eighth cranial nerve.1,2 However, involvement of the brain parenchyma and peripheral nerve is rarely reported.3-5 Here we report a case of scrub typhus with cerebral infarction and polyneuropathy.
CASE REPORT
A 64-year-old man was admitted due to fever, myalgia, dysarthria, dizziness, and headache that had first appeared several days previously. He had worked at a sewage disposal plant in the northern rural area of Seoul. He had suffered from mild conductive hearing impairment of undetermined cause in the left ear for several years. On admission, his body temperature was 39℃ and his blood pressure was normal (110/70 mmHg). Eschar was not evident. A neurological examination revealed a confused mental state and neck stiffness. Limb weakness was absent, but he exhibited multidirectional sway on tandem gait.
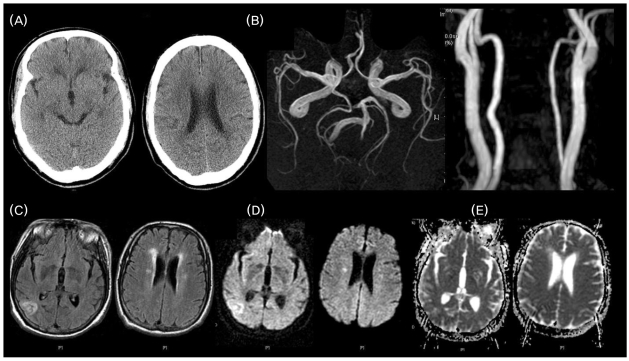
Laboratory tests showed leukocytosis (14.9×103 cells/µl) and thrombocytopenia (33×103 platelets/µl). Liver enzymes were elevated (aspartate aminotransferase = 214 IU/l, alanine aminotransferase = 151 IU/l) and renal function was impaired (blood urea nitrogen = 31creatinine = 1.6 mg/dl). Initial computed tomography (CT) of the brain was normal. (Fig. A), a chest radiograph indicated pulmonary edema, electrocardiography showed sinus tachycardia, and an echocardiogram was normal. Cerebrospinal fluid (CSF) was not examined due to the presence of thrombocytopenia. The patient was initially positive for serum indirect immunofluorescent antibody against O. tsutsugamushi (1:800), and this increased fourfold (1:3200) 2 weeks later. Tests for other antibodies against the Hantaan virus, Leptospira, Rickettsia typhi, human immunodeficiency virus, hepatitis B virus, hepatitis C virus, and herpes simplex virus were negative. Syphilis serology was also negative.
Figure.
Brain imaging findings. (A) Computed tomography scan on admission showing unremarkable findings. (B) Magnetic resonance (MR) angiography showing normal intra- and extracranial vessels. (C.E) MR imaging scans obtained 17 days after admission showing abnormally high signal intensities in the right parietooccipital cortex and the right corona radiata on a fluid-attenuated inversion recovery image (C) and a diffusion-weighted image (D), with elevated signals on the apparent-diffusion-coefficient map (E).
On day 4, the patient was transferred to the intensive care unit for mechanical ventilation. Under the impression of scrub typhus, doxycycline (200 mg/day) was prescribed for 2 weeks. On day 14, a follow-up neurological examination performed after mechanical ventilation had been tapered out revealed a normal mental state and bilateral sensorineural hearing impairment. His motor power was symmetrically impaired in all limbs (4/5). A sensory examination revealed decreased sensations to light touch, pain, and vibration. His gait was wide-based and ataxic, deep tendon reflexes were decreased in all joints, plantar responses were flexor, and Romberg's sign was positive.
A nerve conduction study (NCS) revealed decreased sensory and motor-nerve conduction velocities but sensory nerve and compound muscle action potentials with normal amplitudes, which was compatible with demyelinating sensorimotor polyneuropathy. An autonomic function test revealed orthostatic hypotension and no increase in diastolic blood pressure to isometric exercise. The valsalva ratio was 1.11 (normally ≥ 1.21), and the heart rate varied by less than 5 beats/min (normally ≥ 15 beats/min) during respiration. Audiometry showed sensorineural hearing loss in the right ear (51 dB) and mixed hearing loss in the left ear (61 dB). Brain magnetic resonance imaging (MRI) performed on day 17 showed abnormally high signal intensities in the right parietooccipital cortex and the right corona radiata on fluid-attenuated inversion recovery and diffusion-weighted images (Fig. C, D). A CSF examination showed no cells, an elevated protein content (151 mg/dl), and a normal glucose level (46 mg/dl).
His neurological deficit gradually improved over 3 months. Follow-up NCS and audiometry data were improved. He could hear with minimal difficulty and could walk unsupported with mild swaying at discharge.
DISCUSSION
Our patient suffered from multiorgan failure and multiple neurological problems caused by scrub typhus. At the initial presentation he appeared to have meningoencephalitis with mental confusion, dysarthria, gait disturbance, and stiff neck. Later he presented with bilateral sensorineural hearing loss and polyneuropathy, which suggested widespread involvement of the peripheral nervous system. Although brain MRI showed new cerebral infarctions, no specific symptom or signs could be ascribed to the lesion.
Aseptic meningitis reportedly occurs in about 11% of patients with scrub typhus.1 Neuroimaging data were obtained in only 1 patient with cerebellitis out of 72 patients with scrub typhus whose brain CT findings were normal.1 A patient with scrub typhus showing multiple high-signal-intensity lesions in the brainstem and spinal cord sparing supratentorial gray matter has been reported.3 Repeated MRI has shown progressive deterioration of white-matter lesions similar to acute disseminated encephalomyelitis (ADEM).4
Follow-up brain MRI in our patient revealed new infarctions that were not evident in the initial brain CT. There was no significant stenoocclusion of major intracranial or extracranial vessels, and cardiac workups were unremarkable. The well-known pathology of scrub typhus is vasculitis, which is caused by the destruction of endothelial cells with accompanying perivascular infiltration of leukocytes and endothelial proliferation, followed by thrombosis or closure of the lumen by endothelial proliferation and swelling.6 The endothelial dysfunction has been demonstrated previously.7 However, since no direct evidence of vasculitis such as angiographic abnormalities was obtained in our case, a causalrelation between the vasculitis associated with scrub typhus infection and cerebral infarction could not be firmly established. Moreover, multiple lesions with unremarkable magnetic resonance angiography findings could be related to transient vascular derangement such as cardioembolism associated with transient atrial fibrillation, but this was also not determined in our case. Further studies are neededto clarify the pathomechanism underlying cerebral lesions in scrub typhus.
A few studies have shown the close relationship between Guillain-Barré syndrome (GBS) and rickettsial diseases such as R. rickettsii and R. conorii.8 A case of scrub typhus complicated with GBS involving facial nerves was recently reported.5
In our patient, NCS showed demyelinating sensorimotor polyneuropathy, and an autonomic function test was abnormal. Clinical manifestations were progressive, with symmetric weakness with sensory loss and decreased reflexes appearing 4 weeks, which gradually improved. The final CSF study showed increased protein without pleocytosis. These findings supported a diagnosis of GBS, which has been rarely reported in scrub typhus. Since our patient suffered from sepsis with multiorgan failure, the critical illness polyneuropathy could be an alternative diagnosis. However, polyneuropathy is usually of the motor-dominant axonal type and is not associated with dysautonomia.9
Hearing loss is frequently reported in patients with scrub typhus, which has prompted some authors to suggest that scrub typhus should be suspected in patients who present with fever and acute hearing impairment.2 The hearing impairment in scrub typhus is usually sensorineural, which recovers after appropriate treatment.2 Audiometry showed sensorineural hearing loss in the right ear and mixed hearing loss in the left ear in our patient, which may have resulted from a sensorineural hearing defect combined with the pre-existing conductive hearing impairment of the left ear. Although involvement of the eighth cranial nerve is rare in GBS, a few studies employing the brainstem evoked potential have suggested the presence of demyelination of the acoustic nerve.10 It is therefore possible that eighth-nerve involvement in scrub typhus is a clinical manifestation of demyelinating polyneuropathy.
To our knowledge, the reported case of scrub typhus is the first to be complicated with cerebral infarctions and GBS with eighth-nerve involvement. Clinical syndromes such as GBS in our case and ADEM in the previous study suggest that an immune-mediated mechanism plays an important role in the pathogenesis of the neurological manifestations in scrub typhus.
References
- 1.Silpapojakul K, Ukkachoke C, Krisanapan S, Silpapojakul K. Rickettsial meningitis and encephalitis. Arch Intern Med. 1991;151:1753–1757. [PubMed] [Google Scholar]
- 2.Premaratna R, Chandrasena TG, Dassayake AS, Loftis AD, Dasch GA, de Silva HJ. Acute hearing loss due to scrub typhus: a forgotten complication of a reemerging disease. Clin Infect Dis. 2006;42:6–8. doi: 10.1086/498747. [DOI] [PubMed] [Google Scholar]
- 3.Kim DE, Lee SH, Park KI, Chang KH, Roh JK. Scrub typhus encephalomyelitis with prominent focal neurologic signs. Arch Neurol. 2000;57:1770–1772. doi: 10.1001/archneur.57.12.1770. [DOI] [PubMed] [Google Scholar]
- 4.Chen PH, Hung KH, Cheng SJ, Hsu KN. Scrub typhus-associated acute disseminated encephalomyelitis. Acta Neurol Taiwan. 2006;15:251–254. [PubMed] [Google Scholar]
- 5.Lee SH, Jung SI, Park KH, Choi SM, Park MS, Kim BC, et al. Guillain-Barré syndrome associated with scrub typhus. Scand J Infect Dis. 2007;39:826–828. doi: 10.1080/00365540701266755. [DOI] [PubMed] [Google Scholar]
- 6.Settle EB, Pinkerton H, Corbett AJ. A pathologic study of tsutsugamushi disease with notes on clinicopathologic correlation. J Lab Clin Med. 1945;30:639–661. [Google Scholar]
- 7.Levine HD. Pathologic study of 31 cases of scrub typhus fever with special reference to the cardiovascular system. Am Heart J. 1946;31:314–328. doi: 10.1016/0002-8703(46)90313-4. [DOI] [PubMed] [Google Scholar]
- 8.Toerner JG, Kumar PN, Garagusi VF. Guillain-Barré syndrome associated with Rocky Mountain spotted fever: case report and review. Clin Infect Dis. 1996;22:1090–1091. doi: 10.1093/clinids/22.6.1090. [DOI] [PubMed] [Google Scholar]
- 9.Visser LH. Critical illness polyneuropathy and myopathy: clinical features, risk factors and prognosis. Eur J Neurol. 2006;13:1203–1212. doi: 10.1111/j.1468-1331.2006.01498.x. [DOI] [PubMed] [Google Scholar]
- 10.Schiff JA, Cracco RQ, Cracco JB. Brainstem auditory evoked potentials in Guillain-Barré syndrome. Neurology. 1985;35:771–773. doi: 10.1212/wnl.35.5.771. [DOI] [PubMed] [Google Scholar]