Abstract
Background
Acute onset of a sensory alien hand phenomenon has been observed only from a supratentorial lesion involving the non-dominant hand, mostly from a right posterior cerebral artery infarction. A single acute vascular lesion resulting in a dominant hand sensory alien hand syndrome has not been previously documented.
Case Report
A 78-year old right-handed woman exhibited right sensory alien hand phenomenon from a left pontine hemorrhage. Disturbance of proprioceptive input and visuospatial perception are likely to play a role in manifesting the sign.
Conclusions
Dominant-hand sensory alien hand phenomenon may occur in an acute setting from a left pontine hemorrhage.
Keywords: sensory alien hand, dominant limb, pontine hemorrhage
Introduction
Acute lateralized movement disorder from a stroke generally involves the lenticular or thalamic nucleus or its connecting pathways. Sensory function remains undisturbed and perceptual dysfunction does not occur, representing a pure motor outflow disturbance. Rarely, a more complex movement disorder occur, characterized by constantly moving semi-purposeful hand accompanied by proprioceptive loss with a perceptual disturbance of self control. This sensory alien hand (SAHd) phenomenon, when seen acutely, has only been reported involving the nondominant limb (left hand in right-handed individuals) from a right posterior cerebral stroke.
The following case illustrates right-dominant SAHd phenomenon maybe seen from a left pontine hemorrhage.
Case Report
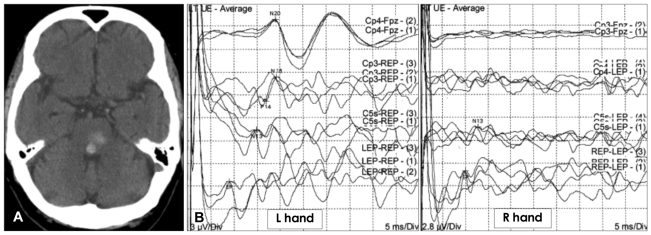
A 78-year old healthy right-handed woman slumped over while playing cards, minutes later she started to awake and vomited. Following intubation she was drowsy with mild left facial weakness. Pupils were mid-size and reactive. Mild exotropia with absent horizontal ocular movements but with full vertical excursion was noted. Right hand tonic posturing was observed without the limb weakness. Emergent CT confirmed left dorsal tegmental pontine hemorrhage (Fig. 1A). On the second hospital day, nursing staff reported intermittent right arm levitation. Right hand would rise off of bed spontaneously as if wanting to grab for few seconds. During this time the patient remained drowsy and did not respond to simple verbal command or make any visual contact. After extubation she was mildly confused with intermittent ocular bobbing. Motor examination showed symmetric strengths but right hand was clumsy with increased tone. Under visual guidance finger-to-nose task showed mild clumsiness without terminal tremor, over-shoot or rebound phenomenon. With eyes closed, the right arm drifted upward and outward and the fingers started to flex. When the attention was diverted, constant slow semi-purposeful movement on the right limbs obvious on the hand and minimal on the foot was observed. The hand moved as if manipulating the bed covering, grabbing and untwisting. Rotatory foot and ankle movement as if looking for the bed cover was occasionally seen. Sensory proprioceptive loss was marked despite intact pain and cold sensation. A week later, she was lucid without confusion. Horizontal gaze paresis improved and ocular bobbing cleared. She stated she was aware the right hand was constantly moving but could not control the limb. She screamed when her right hand unknowingly grabbed and pulled her left hand while watching television in the dark. She requested her right hand to be restrained. Despite the complaint she managed to put on her socks using both hands under visual guidance although the right hand remained clumsy. Somatosensory evoked potential study revealed absent cortical response from the right arm (Fig. 1B). Brain MRI further confirmed presence of only the pontine hemorrhage, and the MR angiogram showed no underlying vascular abnormality.
Fig. 1.
A: Non-enhanced CT at the level of mid-upper pons demonstrating foci of hemorrhage adjacent to the floor of the 4th ventricle. Less dense hemorrhage extends to the left pontine tegmentum. B: Somatosensory evoked potentials (SSEP) from median nerve stimulation demonstrating absence of cortical response from the right hand.
Discussion
Alien hand syndrome can be suspected when an upper limb performs complex motor activities outside of volitional control. Typically in the classic motor type, frontal or anterior corpus callosal lesions are responsible. The sensory type with proprioceptive loss and estrangement has only been reported from the right posterior cerebral involvement in acute clinical setting. Semi-purposeful constantly moving, deafferented clumsy hand not under voluntary control as observed in this case identifies the limb as a dominant SAHd phenomenon from a left pontine hemorrhage.
Although dominant SAHd phenomenon have been documented in chronic neurodegenerative disorders,1,2 a single vascular lesion causing a dominant SAHd have not been reported to best of our knowledge. Complex interaction of proprioceptive deafferented limb in the setting of impaired visuospatial perception, a right hemispheric physiologic domain, may play a role in manifesting the sign.1 Similar perceptual disturbance has been documented in pontine strokes ranging from anosognosia for hemiplegia3 to supranumerary phantom limb phenomenon (more than a single arm and leg on each side).4 Importance of afferent system in these perceptual disturbances is further demonstrated by the fact all of these cases have variable degree of sensory loss. Clinical observation in our case further suggests right hemispheric derived pathway may cross in the pontine tegmentum analogous to more classic cortico-ponto-cerebellar motor fibers.
Traditional view of movement disorders had been based on the cortico-striatal-thalamic pathway model. Recent clinical observation and animal studies have broadened our understanding to include additional pathways that may be involved.5 Positron emission tomography scan studies have documented brainstem and cerebellar hyperactivity in various movement disorders. A case of cervical dystonia from a pontine hemorrhage with subsequent progressive sternocleidomastoid muscle hypertrophy provides further support.6 Despite mounting evidence documenting importance of cerebellar afferent system in generating complex cognitive perceptual impairment,7 documentation of an acute brainstem stroke resulting in abnormal complex movement disorder remain distinctly rare. Undoubtedly, the presence of accompanying drowsiness, confusion, and other confounding physical signs in brainstem strokes may hamper its recognition.
Acute onset of dominant limb SAHd sign from vascular insult can occur and may localize to the left pons. Strategically placed lesion interrupting both the left medial lemniscus and cortically derived pathway may be required in generating dominant SAHd phenomenon.
Acknowledgments
The authors thank Dr. Neal Hermanowicz for helpful comments.
References
- 1.Scepkowski LA, Cronin-Golomb A. The alien hand: cases, categorizations, and anatomical correlates. Behav Cogn Neurosci Rev. 2003;2:261–277. doi: 10.1177/1534582303260119. [DOI] [PubMed] [Google Scholar]
- 2.Kikkert MA, Ribbers GM, Koudstaal PJ. Alien hand syndrome in stroke: a report of 2 cases and review of the literature. Arch Phys Med Rehabil. 2006;87:728–732. doi: 10.1016/j.apmr.2006.02.002. [DOI] [PubMed] [Google Scholar]
- 3.Evyapan D, Kumral E. Pontine anosognosia for hemiplegia. Neurology. 1999;53:647–649. doi: 10.1212/wnl.53.3.647. [DOI] [PubMed] [Google Scholar]
- 4.Tanaka H, Arai M, Kadowaki T, Takekawa H, Kokubun N, Hirata K. Phantom arm and leg after pontine hemorrhage. Neurology. 2008;70:82–83. doi: 10.1212/01.wnl.0000265394.80360.b5. [DOI] [PubMed] [Google Scholar]
- 5.Pizoli CE, Jinnah HA, Billingsley ML, Hess EJ. Abnormal cerebellar signaling induces dystonia in mice. J Neurosci. 2002;22:7825–7833. doi: 10.1523/JNEUROSCI.22-17-07825.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.LeDoux MS, Brady KA. Secondary cervical dystonia associated with structural lesions of the central nervous system. Mov Disord. 2003;18:60–69. doi: 10.1002/mds.10301. [DOI] [PubMed] [Google Scholar]
- 7.Mariën P, Verhoeven J, Brouns R, De Witte L, Dobbeleir A, De Deyn PP. Apraxic agraphia following a right cerebellar hemorrhage. Neurology. 2007;69:926–929. doi: 10.1212/01.wnl.0000267845.05041.41. [DOI] [PubMed] [Google Scholar]