Abstract
The dorsolateral medullary syndrome (Wallenberg's syndrome) is produced by infarction of a wedge of lateral medulla posterior to the inferior olivary nucleus, and is usually caused by vertebral artery occlusion. Ipsilateral axial lateropulsion as an initial symptom of vertebral artery occlusion is rare, and the responsible anatomical structure is still uncertain. Here we describe a patient presenting with ipsilateral axial lateropulsion as an initial symptom of vertebral artery occlusion.
Keywords: Lateral medullary syndrome, MRI
Lateropulsion is one of the symptoms of lateral medullary infarction. It is usually associated with ipsilateral Horner syndrome, ipsilateral limb ataxia, superficial sensory disturbance of the ipsilateral face and contralateral limbs, dysarthria, dysphagia, and vertigo, with isolated body lateropulsion being rare. The lesion responsible for axial lateropulsion is controversial,1 but recent studies have identified some possibilities.2-4 Lesions of the descending lateral vestibulospinal tract or the ascending dorsal spinocerebellar tract may induce ipsilateral axial lateropulsion, either as a consequence of impaired vestibulospinal posture control or impaired or absent proprioceptive information.2 Here we present a case of lateral medullary infarction in which axial lateropulsion and unilateral sensory loss were the unique manifestation. The presented findings raise the possibility that axial lateropulsion in the lateral medullary infarctionis attributable to a lesion of the vestibulospinal tract.
CASE REPORT
An 87-year-old woman presented with lateropulsion of her body to the right and dizziness 4 days after onset. She was a nonsmoker and had no known hypertension, cardiac disease, or previous stroke. However, diabetes mellitus was detected on admission. She denied vertigo, diplopia, hiccup, dysphagia, speech disturbance, numbness, and muscle weakness. On admission, her ocular movements were normal in all directions, and no spontaneous or gaze-evoked nystagmus was detectable. Eelectro-oculographic recording and bedside examinations revealed no skew deviation, ocular lateropulsion, saccadic pursuit, ocular dysmetria, or Horner's syndrome. Elevation of the soft palate was intact on phonation. There was no nasal voice, hoarseness, or dysarthria, and the tongue did not deviate on protrusion. Other cranial nerve functions were intact, and she had no muscular weakness. Her facial sensation was intact, but she showed decreased pinprick and thermal sensations in the left trunk and extremities. Position and vibration senses were intact in all limbs. Coordination of the extremities was intact. She was unable to keep standing without assistance due to marked lateropulsion to the right. Deep tendon reflexes were normal, and she had no pathological reflexes.
Brain MRI showed an acute small infarct in the right lateral aspect of the lowest medulla, and MR angiography showed severe stenosis of the right distal vertebral artery (Fig. 1). She was treated with aspirin at 300 mg a day and discharged on day 10 with only mild sensory impairment in the left trunk and extremities.
Figure 1.
Diffusion (A) and T2-weighted (B) MR images showing a high signal intensity in the right lateral medullar. MR angiography (C) disclosing severe stenosis in the distal portion of the right vertebral artery (arrow).
DISCUSSION
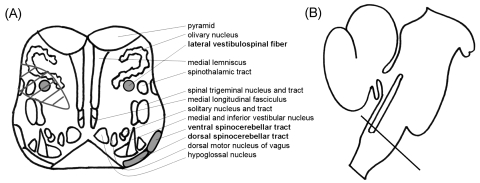
Isolated axial lateropulsion occurs with ischemic lesions in the inferior portion of the cerebellum and tonsil, and with a demyelinating lesion of the superior and inferior cerebellar peduncles.5 Thus, the critical structure for lateropulsion remains to be elucidated. A recent study found that body lateropulsion without limb ataxia was probably due to the impairment of vestibulospinal postural control caused by a lesion of the descending lateral vestibulospinal tract (Fig. 2), and body lateropulsion with limb ataxia was attributable to a lesion of the ascending dorsal spinocerebellar tract.2 The patient described here had pain and thermal sensory impairment in the contralateral lower limb and trunk, which was attributed to a lesion in the ventrolateral part of the spinothalamic tract. A very small lesion located superficially in the lateral medulla can cause an atypical spinothalamic sensory deficit, which in some cases appears a few days after the onset of other symptoms.6
Figure 2.
(A) Schematic of the anatomical structures located in the caudal medulla where the lesion was found in MRI and its sagittal level of the brainstem. The round gray areas indicate the presumed locations of the lateral vestibulospinal tract in the lower medulla oblongata, and the area with diagonal lines indicates the lesion in the patient. (B) Straight line indicates the level of the caudal medulla.
Structures located dorsal to the spinothalamic tract, including the spinal trigeminal tract and nucleus, and the ambiguus and vestibular nuclei were probably spared, because she did not have facial sensory impairment, pharyngeal or laryngeal palsy, or nystagmus. Conversely, it is highly likely that the lateral vestibulospinal tract was involved, because this structure is located just ventromedial to the spinothalamic tract in the medulla.5 The lateral vestibulospinal tract is considered to play an important role in the maintenance of posture by exerting strong excitatory influences on extensor muscles and inhibitory influences on flexor muscles.7 Thus, interruption of the lateral vestibulospinal tract decreases extensor muscle tone of the trunk and lower limb on the side of the lesion, which is likely to cause ipsilateral axial lateropulsion. The present findings raise the possibility that axial lateropulsion without limb ataxia in Wallenberg's syndrome is attributable to lesions of the lateral vestibulospinal tracts.
This case shows that axial lateropulsion and unilateral sensory loss can occur as the combination symptom of lateral medullary infarction. It also suggests that ipsilateral axial lateropulsion can be caused by lesions of different topographies involving the vestibular nuclei, lateral vestibulospinal tract, cerebellar peduncle, or spinocerebellar tracts.
References
- 1.Ropper AH, Brown RH. Disorders of stance and gait. In: Foltin J, Nogueira I, Edmonson KG, Sheinis LA, editors. Adam's and Victor's principles of neurology. 8th edn. New York: McGraw-Hill; 2005. pp. 100–108. [Google Scholar]
- 2.Thömke F, Marx JJ, Iannetti GD, Cruccu G, Fitzek S, Urban PP, et al. A topodiagnostic investigation of body lateropulsion in medullary infarcts. Neurology. 2005;64:716–718. doi: 10.1212/01.WNL.0000152040.27264.1A. [DOI] [PubMed] [Google Scholar]
- 3.Lee H, Sohn CH. Axial lateropulsion as a sole manifestation of lateral medullary infarction: aclinical variant related to rostral-dorsolateral lesion. Neurol Res. 2002;24:773–774. doi: 10.1179/016164102101200870. [DOI] [PubMed] [Google Scholar]
- 4.Kim SH, Cho YJ, Cho JH, Han SW, Kim SM, Park SC, et al. Isolated lateropulsion by a lesion of the dorsal spinocerebellar tract. Cerebrovasc Dis. 2004;18:344–345. doi: 10.1159/000080978. [DOI] [PubMed] [Google Scholar]
- 5.Arai M. Ipsilateral axial lateropulsion as an initial symptom of vertebral artery occlusion. J Neurol Neurosurg Psychiatry. 2004;75:1648. doi: 10.1136/jnnp.2003.035246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kim JS, Lee JH, Lee MC. Patterns of sensory dysfunction in lateral medullary infarction. Clinical-MRI correlation. Neurology. 1997;49:1557–1563. doi: 10.1212/wnl.49.6.1557. [DOI] [PubMed] [Google Scholar]
- 7.Brodal A, Rinvik E. Pathways mediating supraspinal influences on the spinal cord. The basal ganglia. In: Brodal A, editor. Neurological anatomy in relation to clinical medicine. 3rd edn. New York: Oxford University Press; 1981. pp. 180–293. [Google Scholar]