Abstract
Background and purpose
We investigated subsequent vascular events in patients with transient ischemic attack (TIA) and determined the predictors of such events among vascular risk factors including large-artery disease, TIA-symptom duration, and acute ischemic lesions on diffusion-weighted imaging (DWI).
Methods
We identified 98 consecutive patients with TIA who visited a tertiary university hospital and underwent DWI and brain magnetic resonance angiography within 48 hours of symptom onset. We reviewed the medical records to assess the clinical characteristics of TIA, demographics, and the subsequent vascular events including acute ischemic stroke, TIA, and myocardial infarction.
Results
Large-artery disease was detected in 55 patients (56%). Ten patients (10%) experienced TIA symptoms for longer than 1 hour, and acute infarctions on DWI were identified in 30 patients (31%). During the mean follow-up period of 19 months, seven patients (7%) had an acute ischemic stroke and 20 patients (20%) had TIA. Retinal artery occlusion in two patients, spinal cord infarction in one patient, and peripheral vascular claudication in one patient were also recorded. Cox proportional-hazards multivariate analysis revealed that large-artery disease was an independent predictor of subsequent cerebral ischemia (hazard ratio [HR], 2.8; 95% confidence interval [CI], 1.1-7.1; p=0.02) and subsequent vascular events (HR, 2.9; 95% CI, 1.2-6.7; p=0.01).
Conclusions
In patients with TIA, large-artery disease is an independent predictor of subsequent vascular events. Acute infarction on DWI and a symptom duration of more than 1 hour are not significantly correlated with a higher risk of subsequent vascular events. These findings suggest that the underlying vascular status is more important than symptom duration or acute ischemic lesion on DWI.
Keywords: Transient ischemic attack, Prognosis, Large-artery stenosis, Diffusion-weighted imaging
INTRODUCTION
The classic definition of a transient ischemic attack (TIA) is a sudden neurological dysfunction due to cerebral or optic ischemia lasting less than 24 hours.1-3 The rapid improvements in symptoms and signs in patients with TIA mean that it is not always possible to determine whether a transient neurological deficit is of vascular origin. In such cases diffusion-weighted imaging (DWI) may be helpful for confirming acute cerebral ischemic events.4-8 Acute ischemic lesions on DWI have been reportedly identified in about 50% of patients with TIA.8,9 In addition, TIA patients with acute ischemic lesions on DWI and a symptom duration of more than 1 hour reportedly have a higher risk of subsequent vascular events.10
However, since a symptom duration of more than 1 hour in patients with TIA was associated with emboligenic cardiac or arterial disease,11 it is not clear whether acute ischemic damage on DWI and a symptom duration of more than 1 hour are accurate predictors of further vascular events.
Therefore, we investigated subsequent vascular events in patients presenting with TIA and determined the predictors among vascular risk factors including large-artery disease, cardiac disease, TIA-symptom duration, and acute infarction on DWI.
MATERIALS AND METHODS
We identified 171 patients presenting with TIA who visited our hospital (a tertiary university hospital) between January 2002 and August 2005 from the electronic hospital database. TIA was defined as an episode of focal loss of brain function attributed to cerebral ischemia and lasting less than 24 hours.1 The diagnosis of TIA was made by the consensus of at least two neurologists. Patients with only transient monocular symptoms were not included.
Seventy-three patients were excluded from the analysis due to them conforming with at least one of the following criteria: (1) undergoing DWI and brain magnetic resonance angiography (MRA) more than 48 hours after symptom onset (n=40), (2) presence of an ambiguous description of TIA symptoms or their duration (n=19), (3) follow-up loss after initial presentation (n=1), and (4) not undergoing both DWI and MRA (n=13). Therefore, 98 subjects were finally enrolled and analyzed.
Brain DWI and MRA were performed with a 1.5-tesla MRI device (Signa Horizon Echospeed, General Electric Medical Systems), and DWI was performed with multisection single-shot spin-echo echo planar imaging sequences. Each of the 20 sections was acquired with diffusion gradient (b) values of 0 and 1000 sec/mm2. Diffusion gradients were applied to the three orthogonal spatial directions, and an isotropic diffusion-weighted image was generated by averaging the images obtained in these directions. The acquisition parameters of the DWI were a repetition time of 6500 ms, an echo time of 96.8 ms, a 128×128 matrix, a 280-mm field of view, a 5-mm slice thickness, and a 1-mm intersection gap. Apparent diffusion coefficient (ADC) maps were calculated from the DWI data. Acute infarction on DWI was defined as an area with a high signal intensity on the isotropic diffusion-weighted image and a low signal intensity on the ADC map.
MRA was performed using a standard protocol of three-dimensional time-of-flight sequences. Large-artery disease was defined as a reduction in luminal diameter of at least 50% in the intracranial arteries and the extracranial carotid artery using the methods described by the Warfarin-Aspirin for Symptomatic Intracranial Disease Study12 and the North American Symptomatic Carotid Endarterectomy Trial method,13 respectively. The extracranial vertebral artery was not included in the data analysis since by MRA cannot be used to clearly differentiate a normal variant of congenital hypoplasia from an acquired stenosis. The isotropic diffusion-weighted images, ADC maps, and MRA data were reviewed by two neurologists blinded to the clinical data. If there was a disagreement, a final decision was made by consensus.
Patients were diagnosed as hypertensive if they were currently undergoing treatment with antihypertensive drugs, their systolic blood pressure was greater than 140 mmHg, or their diastolic blood pressure was greater than 90 mm Hg on two separate examinations after discharge. Patients were diagnosed as diabetes mellitus if they were currently undergoing treatment with insulin or oral hypoglycemia agents, or if their fasting blood glucose level was greater than 140 mg/dL on two separate examinations. The smoking habit was defined as either smoking or nonsmoking, with smokers defined as either current smokers or current nonsmokers. Ischemic heart disease was defined as a history of either angina pectoris or myocardial infarction. Atrial fibrillation in electrocardiography EKG was defined as an irregularly spaced QRS complex without a discrete P wave. Patients were diagnosed as atrial fibrillation if they had a history of atrial fibrillation or the EKG revealed atrial fibrillation. Patients were diagnosed as hyperlipidemia if they were currently undergoing treatment with lipid-lowering agents, if their total cholesterol level was greater than 240 mg/dL, or if their LDL-cholesterol level was greater than 130 mg/dL.
All patients were initially treated with anticoagulants. After initial vascular evaluations, those with atrial fibrillation or an embolus cardiogenic origin received long-term oral anticoagulant therapy, and the others received antiplatelet drugs. Each patient was interviewed by a neurologist every 1-3 months during the follow-up period.
Medical records between January 2002 and December 2005 were retrospectively reviewed to assess the clinical characteristics of TIA, the patient demographics, and the subsequent vascular outcomes such as TIA, acute ischemic stroke, or myocardial infarction. The clinical endpoints were subsequent cerebral ischemia (e.g., acute ischemic stroke and TIA) and subsequent vascular events (e.g., acute ischemic stroke, TIA, and myocardial infarction).
Univariate analysis was performed with the Χ2 test or Fisher's exact test (with the latter used when at least one cell had an expected count of less than five) for the categorical data. Group means of continuous data were compared using the Mann-Whitney test. Univariate analysis was used to detect variables associated with subsequent vascular outcomes. Cox proportional-hazards multivariate analysis was performed to identify independent predictors of subsequent cerebral ischemia and subsequent vascular events. Factors such as age, gender, acute infarction on DWI, a TIA-symptom duration of more than 1 hour, and any variable with a p value of ≤0.1 on univariate analysis were included in the multivariate analysis. Subsequent cerebrovascular ischemic events and subsequent vascular events were defined as dependent variables. A p value of <0.05 was considered significant. Results were expressed as hazard ratios (HRs) together with their 95% confidence intervals (CIs).
RESULTS
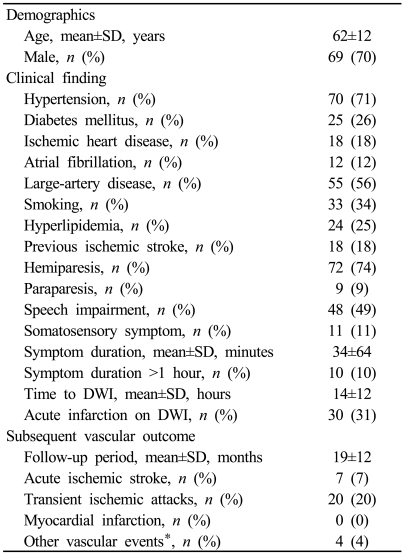
The ages of the 98 TIA patients ranged from 38 to 83 years (62±12 years, mean±standard deviation) (Table 1). Men accounted for 69 (70%) of the enrolled patients. Seventy patients (71%) had hypertension, 25 (26%) had diabetes mellitus, 55 (56%) had large-artery disease, and 18 (18%) had a history of ischemic stroke. Hemiparesis and speech impairment were the most common presenting symptoms, in 72 patients (74%) and 48 patients (49%), respectively. The duration of TIA symptoms was 34±64 minutes. Ten patients (10%) experienced TIA symptoms lasting more than 1 hour. The interval from symptom onset to DWI was 14±12 hours. Acute infarctions on DWI were identified in 30 patients (31%). During the mean follow-up period of 19 months (range 1.7 to 44.5 months), 7 patients (7%) had an acute ischemic stroke and 20 patients (20%) had TIA. Retinal artery occlusion in two patients, spinal cord infarction in one patient, and peripheral vascular claudication in one patient were also recorded during follow-up.
Table 1.
Demographics and clinical findings of transient ischemic attacks
DWI; Diffusion-weighted imaging, SD; standard deviation. *Other vascular events includes retinal artery occlusion (n=2), spinal cord infarction (n=1), and vascular claudication (n=1).
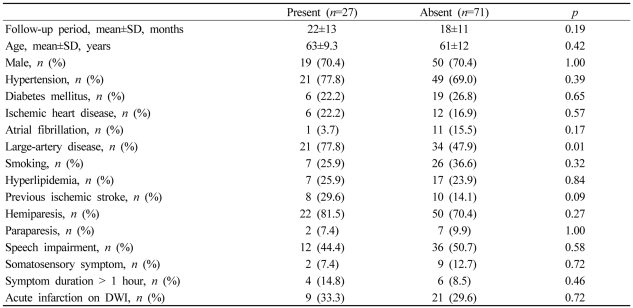
The follow-up period did not differ significantly (p=0.19) between patients with and without subsequent cerebral ischemia (Table 2). Univariate analysis revealed that subsequent cerebral ischemia was significantly associated with large-artery disease (p <0.01). A TIA-symptom duration of more than 1 hour was more frequent in those with than in those without subsequent cerebral ischemia, but the difference was not statistically significant (14.8% vs. 8.5%, p=0.46). The frequency of acute infarction on DWI was similar in those with and without subsequent cerebral ischemia (33.3% vs. 29.6%, p=0.72). Since large-artery disease and the previous history of ischemic stroke exhibited p values of ≤0.1, they were included in the multivariate analysis. Cox proportional-hazards multivariate analysis with variables of age, gender, acute infarction on DWI, symptom duration of more than 1 hour, previous history of ischemic stroke, and large-artery disease revealed that only large-artery disease was an independent predictor of subsequent cerebral ischemia (HR, 2.8; 95% CI, 1.1-7.1 p=0.02).
Table 2.
Risk factors for subsequent cerebral ischemia
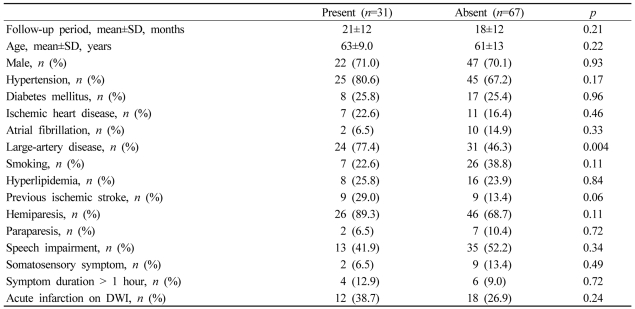
The follow-up period also did not differ significantly (p=0.21) between those with and without subsequent vascular events (Table 3). Univariate analysis revealed that large-artery disease was the only factor that significantly affected subsequent vascular events (p <0.01). A TIA-symptom duration of more than 1 hour and acute infarction on DWI were more frequent in those with than in those without subsequent vascular events, but the difference was not statistically significant (12.9% vs. 9.0%, p=0.72; 38.7% vs. 26.9%, p=0.24, respectively). The variables with a p value of ≤0.1 were large-artery disease and previous history of ischemic stroke, and both were included in the multivariate analysis. Cox proportional-hazards multivariate analysis in which the entered variables were age, gender, acute infarction on DWI, symptom duration of more than 1 hour, previous history of ischemic stroke, and large-artery disease revealed that only large-artery disease was an independent predictor of subsequent vascular events (HR, 2.9; 95% CI, 1.2-6.7; p=0.01).
Table 3.
Risk factors for subsequent vascular events
DISCUSSION
Large-artery disease on MRA was an independent risk factor for subsequent cerebral ischemia and subsequent vascular events in this study. Purroy et al. also reported that large-artery occlusive disease (as defined by an ultrasound protocol) was a predictor of further vascular events.10 They performed transcranial Doppler recordings to define intracranial arterial stenosis, but this has the limitations of being highly dependent on the skill of the operator and evaluating only a limited extent of the intracranial arteries. In comparison, we used MRA for a more objective and accurate evaluation of arterial stenosis.
The results of this study revealed that the 1-hour time limit was not significantly correlated with the vascular prognosis. Although the combination of acute infarction on DWI and a symptom duration of more than 1 hour is reportedly an independent risk factor for subsequent vascular events, there is no scientific explanation for this particular combination10 - the combination was as arbitrary as the 1-hour time limit. Johnston et al. showed that a TIA-symptom duration of more than 10 minutes was an independent predictor of short-term prognosis.14 However, they did not evaluate intracranial large-artery disease, which might have been a very important factor for the prognosis.
Acute infarction on DWI was not correlated with the subsequent vascular prognosis in our study. There is evidence that cerebral damage on computed tomography and DWI is associated with a poor vascular prognosis.15,16 However, the evaluations of large-artery disease by previous studies have been incomplete. Our inclusion of large-artery disease in the analysis revealed no significant association between acute infarction on DWI and subsequent vascular events. This is partly because most acute ischemic lesions on DWI in our study were either small or tiny, suggesting minimal cerebral damage. Moreover, acute infarctions on DWI may represent false-positive or false-negative errors in patients with TIA.4,9,17 The underlying pathophysiology is more important than the mere presence or absence of DWI abnormalities.3,18,19
The present study had the following limitations. First, this was retrospective study that might not have identified all vascular events. However, every follow-up interview was performed by a neurologist, and we consider it unlikely that any occurrences of subsequent ischemic stroke or TIA were missed. Second, although MRA is a convenient and noninvasive method for assessing vascular stenosis, there are technical difficulties in the evaluation of certain arteries, such as the siphon portion of the internal carotid arteries. In addition, embolic lesions may resemble vascular stenosis on MRA, although we defined vascular stenosis on MRA as an atherosclerotic lesion.
In conclusion, in patients with TIA, large-artery disease appears to be an independent risk factor for subsequent vascular events. Acute infarction on DWI and a symptom duration of more than 1 hour were not significantly correlated with the risk of subsequent vascular events. These findings suggest that the underlying vascular status is more important than the characteristics of the TIA symptoms or imaging abnormalities. Future large prospective studies should attempt to confirm these results.
References
- 1.Special report from the National Institute of Neurological Disorders and Stroke. Classification of cerebrovascular diseases III. Stroke. 1990;21:637–676. doi: 10.1161/01.str.21.4.637. [DOI] [PubMed] [Google Scholar]
- 2.Mohr JP. Historical perspective. Neurology. 2004;62:S3–S6. doi: 10.1212/wnl.62.8_suppl_6.s3. [DOI] [PubMed] [Google Scholar]
- 3.Albers GW, Caplan LR, Easton JD, Fayad PB, Mohr JP, Saver JL, et al. TIA Working Group Transient ischemic attack - proposal for a new definition. N Engl J Med. 2002;347:1713–1716. doi: 10.1056/NEJMsb020987. [DOI] [PubMed] [Google Scholar]
- 4.Inatomi Y, Kimura K, Yonehara T, Fujioka S, Uchino M. Hyperacute diffusion-weighted imaging abnormalities in transient ischemic attack patients signify irreversible ischemic infarction. Cerebrovasc Dis. 2005;19:362–368. doi: 10.1159/000085203. [DOI] [PubMed] [Google Scholar]
- 5.Schulz UG, Briley D, Meagher T, Molyneux A, Rothwell PM. Diffusion-weighted MRI in 300 patients presenting late with subacute transient ischemic attack or minor stroke. Stroke. 2004;35:2459–2465. doi: 10.1161/01.STR.0000143455.55877.b9. [DOI] [PubMed] [Google Scholar]
- 6.Rovira A, Rovira-Gols A, Pedraza S, Grive E, Molina C, Alvarez-Sabin J. Diffusion-weighted MR imaging in the acute phase of transient ischemic attacks. AJNR Am J Neuroradiol. 2002;23:77–83. [PMC free article] [PubMed] [Google Scholar]
- 7.Crisostomo RA, Garcia MM, Tong DC. Detection of diffusion-weighted MRI abnormalities in patients with transient ischemic attack: correlation with clinical characteristics. Stroke. 2003;34:932–937. doi: 10.1161/01.STR.0000061496.00669.5E. [DOI] [PubMed] [Google Scholar]
- 8.Kidwell CS, Alger JR, Di Salle F, Starkman S, Villablanca P, Bentson J, et al. Diffusion MRI in patients with transient ischemic attacks. Stroke. 1999;30:1174–1180. doi: 10.1161/01.str.30.6.1174. [DOI] [PubMed] [Google Scholar]
- 9.Warach S, Kidwell CS. The redefinition of TIA: the uses and limitations of DWI in acute ischemic cerebrovascular syndromes. Neurology. 2004;62:359–360. doi: 10.1212/wnl.62.3.359. [DOI] [PubMed] [Google Scholar]
- 10.Purroy F, Montaner J, Rovira A, Delgado P, Quintana M, Alvarez-Sabin J. Higher risk of further vascular events among transient ischemic attack patients with diffusion-weighted imaging acute ischemic lesions. Stroke. 2004;35:2313–2319. doi: 10.1161/01.STR.0000141703.21173.91. [DOI] [PubMed] [Google Scholar]
- 11.Kimura K, Minematsu K, Yasaka M, Wada K, Yamaguchi T. The duration of symptoms in transient ischemic attack. Neurology. 1999;52:976–980. doi: 10.1212/wnl.52.5.976. [DOI] [PubMed] [Google Scholar]
- 12.Samuels OB, Joseph GJ, Lynn MJ, Smith HA, Chimowitz MI. A standardized method for measuring intracranial arterial stenosis. AJNR Am J Neuroradiol. 2000;21:643–646. [PMC free article] [PubMed] [Google Scholar]
- 13.Beneficial effect of carotid endarterectomy in symptomatic patients with high-grade carotid stenosis. North American Symptomatic Carotid Endarterectomy Trial Collaborators. N Engl J Med. 1991;325:445–453. doi: 10.1056/NEJM199108153250701. [DOI] [PubMed] [Google Scholar]
- 14.Johnston SC, Gress DR, Browner WS, Sidney S. Short-term prognosis after emergency department diagnosis of TIA. JAMA. 2000;284:2901–2906. doi: 10.1001/jama.284.22.2901. [DOI] [PubMed] [Google Scholar]
- 15.Ay H, Koroshetz WJ, Benner T, Vangel MG, Wu O, Schwamm LH, et al. Transient ischemic attack with infarction: a unique syndrome? Ann Neurol. 2005;57:679–686. doi: 10.1002/ana.20465. [DOI] [PubMed] [Google Scholar]
- 16.Douglas VC, Johnston CM, Elkins J, Sidney S, Gress DR, Johnston SC. Head computed tomography findings predict short-term stroke risk after transient ischemic attack. Stroke. 2003;34:2894–2898. doi: 10.1161/01.STR.0000102900.74360.D9. [DOI] [PubMed] [Google Scholar]
- 17.Ay H, Buonanno FS, Rordorf G, Schaefer PW, Schwamm LH, Wu O, et al. Normal diffusion-weighted MRI during stroke-like deficits. Neurology. 1999;52:1784–1792. doi: 10.1212/wnl.52.9.1784. [DOI] [PubMed] [Google Scholar]
- 18.Caplan LR. TIAs: We need to return to the question, 'What is wrong with Mr. Jones?'. Neurology. 1988;38:791–793. doi: 10.1212/wnl.38.5.791. [DOI] [PubMed] [Google Scholar]
- 19.Fisher CM. Transient ischemic attacks. N Engl J Med. 2002;347:1642–1643. doi: 10.1056/NEJMp020129. [DOI] [PubMed] [Google Scholar]