Abstract
Background/Aims
Coagulopathy is a common complication of snakebite, but there is little information on the clinical importance of coagulopathy. We analyzed the characteristics of coagulopathy after envenomation.
Methods
Ninety-eight patients who experienced snakebite were enrolled in this study. We divided all the patients into three groups by the ISTH DIC scoring system: the normal, simple coagulopathy and DIC groups. The coagulopathy group included both the simple coagulopathy and DIC groups. We then conducted a case-control study.
Results
There was a significant decrease in the Hct, protein, albumin, ALP and cholesterol levels in the coagulopathy group, and only the cholesterol level was deceased in the DIC group (p<0.05). Leukocytosis and rhabdomyolysis were significantly associated with coagulopathy, and hemolysis and rhabdomyolysis were associated with DIC (p<0.05). The presence of rhabdomyolysis was considered a risk factor for coagulopathy (p<0.05). These conditions continued for up to six to seven days after the snakebite.
Conclusions
Evaluation of coagulopathy with using these characteristics is helpful to properly manage the patients who experience snakebite.
Keywords: Coagulopathy, Snakebite
INTRODUCTION
After being bitten by a poisonous snake in Korea, many patients experience local pains, edema and systemic complications such as rhabdomyolysis, acute renal failure and neurologic abnormalities, and other complications may occur as well1, 2). Among these complications, coagulapathy results in hemorrhage and in rare cases, infarction and it may lead to death3). Coagulopathy is a clinically common disease; its clinical importance is well known and many case studies of coagulapathy with its associated complications have been conducted. However, its clinical pattern and progress in many cases are determined only by the abnormalities on a blood coagulation test and there are only a few references on its specific clinical characteristics, the evaluation of their seriousness and the length of the follow-up period. Therefore, we examined the clinical characteristics of coagulopathy after 98 patients were bitten by poisonous snakes, and these patients were hospitalized from 1999 to 2006 at the Wonju Christian Hospital, Yonsei University, Wonju College of Medicine.
MATERIALS AND METHODS
Subjects
We retrospectively investigated the age, gender, seasonal distribution, clinical examination results, clinical symptoms and complications of the 98 patients who were hospitalized due to poisonous snakebite from January, 1999 to December, 2006, based on their medical records. Those patients aged less than 15 or those without appropriate records or examination results were excluded from the study.
Methods
Coagulopathy is characterized by defects of the blood coagulation system and it is diagnosed from abnormalities on blood tests. For making the diagnosis, we used the disseminated intravascular coagulation (DIC) scoring system designed by the ISTH (International Society on Thrombosis and Hemostasis). The subjects who were classified according to the disseminated intravascular coagulopathy (DIC) scoring system were classified into the normal, non-overt DIC and overt DIC groups by adding the scores of the clinical symptoms of coagulopathy and the scores of the prothrombin time (PT), the fibrin degradation products (FDPs) and the D-dimer, fibrinogen and platelet count tests4, 5). For the DIC scoring system, non-overt DIC means simple coagulation abnormality without any remarkable DIC symptoms such as defibrination or isolated thrombocytopenia, and overt DIC is the typical DIC. The coagulopathy after snakebite that was investigated in this study included both simple coagulation abnormality and DIC. Metabolic acidosis was acidemia caused due to metabolic reasons and this was defined to be less than 22 mmol/L of HCO3- on the arterial blood gas study. Leukocytosis was diagnosed when the number of leukocytes increased to over 10,000 mm3 in the whole blood because of an inflammatory response. Rhabdomyolysis was defined to be a serum creatine kinase level over 1,000 IU/L or a myoglobin level over 110 ng/ml, and acute renal failure was defined as a level of serum creatinine over 1.3 mg/dL without a history of chronic renal disorder. Hemolysis that destroyed erythrocytes inside the blood was diagnosed when the serum haptoglobin level was less than 40 mg/dL.
The normal group and the coagulopathy group were compared to investigate the characteristics of coagulopathy after poisonous snakebite and the non-overt DIC group and the overt DIC group were compared to examine the characteristics of the DIC group with clinically significant complications. Comparison of their results on the blood and serum tests and their clinical symptoms following poisonous snakebite was performed.
Statistical analysis
SPSS (version 12.0) was used for conducting independent variable t-tests, Chi-square tests and multivariate logistic regression analysis. A p value less than 0.05 was considered to be significant statistically.
RESULTS
Gender and the seasonal distribution and frequency of complications among the patients who experienced snake bite
There were 68 males (69.4%) and 30 females (30.6%) among the 98 subjects. For the seasonal distribution, one snake bite occurred in spring (Feb.-Apr.) (1.0%), 44 occurred in summer (May-Jul.) (44.9%) and 53 occurred in autumn (Aug.-Oct.) (54.1%). The frequency was high from May to Oct.1, 2). As a complication following snakebite, rhabdomyolysis occurred in 37 cases (37.8%) and any acute renal failure was not found. Coagulopathy was shown in 51 cases (52.0%), and these 51 cases were made up of 20 simple coagulation abnormality cases (20.4%) and 31 DIC cases (31.6%).
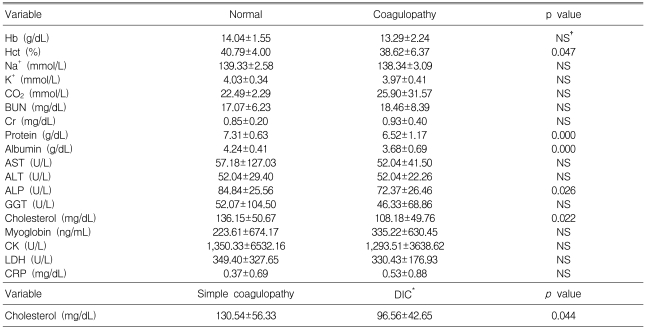
Hematological characteristics of the coagulopathy group and the DIC group
To examine the characteristics of the coagulopathy group, the mean values of the blood and serum tests were compared using the independent t-test by setting the normal group as the control group. Those values of the DIC groups were also compared with the same method by designating the simple coagulation abnormality group as the control group (Table 1). From the results, Hct, protein, albumin, ALP and cholesterol were significantly more decreased in the coagulopathy group than in the normal group (p<0.05) and cholesterol was more reduced in the DIC group than in the simple coagulation abnormality group (p<0.05).
Table 1.
Comparison of the laboratory data of the patients with or without coagulopathy
*Disseminated intravascular coagulation
†Non significant
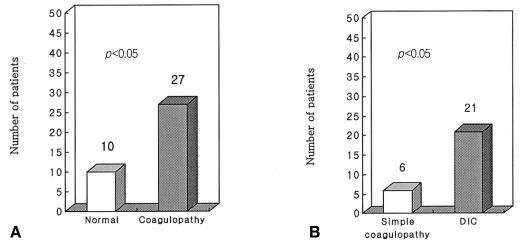
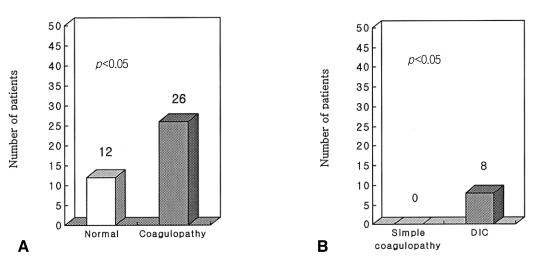
Clinical Characteristics of the coagulopathy group and the DIC group
The clinical symptoms such as metabolic acidosis, leukocytosis, hemolysis and rhabdomyolysis, which can be observed following snake bite, were analyzed by Chi-square tests. When the results of the coagulopathy group were compared with those of the normal group, leukocytosis and rhabdomyolysis were significantly associated with coagulopathy. On comparison of the simple coagulation abnormality group and the DIC group, hemolysis and rhabdomyolysis occurred significantly more often in the DIC group (Figure 1, 2).
Figure 1.
The incidence of rhabdomyolysis in the normal and coagulopathy groups (A), and in the simple coagulopathy and DIC (Disseminated Intravascular Coagulation) groups (B).
Figure 2.
The incidence of leukocytosis in the normal and coagulopathy groups (A), and the incidence of hemolysis in the normal and DIC (Disseminated Intravascular Coagulation) groups (B).
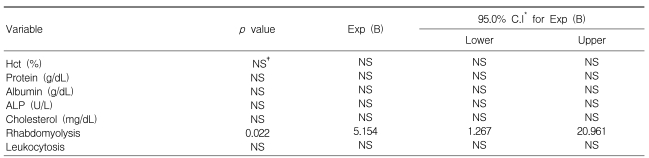
Risk factors of coagulopathy occurring after snakebite
Multivariate logistic regression tests were conducted to determine the risk factors related to coagulopathy following snake bite, and rhabdomyolysis was found to be its significant risk factor (Table 2).
Table 2.
Multivariate regression analysis for the risk factors of coagulopathy
*Confidence interval
†Non significant
Complications and clinical progress of coagulopathy occurring after snake bite
For coagulopathy after poisonous snake bite, complications caused by hemorrhage occurred in 10 cases (10.2%) and complications due to infarction were shown in 2 cases (2.0%). The complications following hemorrhage included systemic purpura in most cases, and both hematochezia and hematemesis occurred in one case, hemoperitoneum occurred in one, vaginal bleeding occurred in one and hematoma in the scrotum and abdomen occurred in one. One case of myocardial infarction and one case of cerebral infarction were reported as complications due to infarction. As only a few patients among the 98 subjects were hospitalized until they fully recovered from coagulopathy following poisonous snake bite, the period of morbidity from coagulopathy was investigated only for a limited number of cases. The period of extended PT averaged 6.17±4.30 days and it continued to 7.61±4.08 days after poisonous snake bite. The period showing thrombocytopenia was 6.383.25 days and the symptoms continued to 7.46±2.98 days.
DISCUSSION
Coagulopathy caused by poisonous snack bite is a clinically significant complication leading to hemorrhage, infarction and in some cases, fatal diseases. According to Retzios et al,6-8), snake venom forms fibrin by working like thrombin on the fibrinogen molecules. While stable fibrin polymers are made by condensing after eliminating both the fibrinopeptide A and B from the fibrinogen during normal fibrin formation, venom makes the unstable fibrin polymer vulnerable to fibrinolysis and phagocytosis by the reticuloendothelial system by removing only the fibrinopeptide A6, 9). As a result, venom can cause various types of coagulopathy, from simple coagulation abnormalities such as defibrination and isolated thrombocytopenia to serious coagulopathy like DIC, and the prevalence of coagulopathy was reported to be up to 36~50%10). The prevalence of coagulopathy observed in this study (52%) was similar with that in the previous research and the prevalence of DIC (31.6%) was also same as that of other studies (40%)2). Other researchers have shown that the prevalence of coagulopathy and DIC was different according to the types of venoms, and the location and time length of the bite affected the venoms' absorption into the blood. Although the previous studies suggested that serious coagulopathy such as DIC rarely happened because venom was absorbed into the blood in only a small number of cases9), in this study, the prevalence of DIC after poisonous snakebite was not considered to be low.
On comparison of the coagulopathy group and the normal groups to assess the characteristics of coagulopathy that occurred after snake bite, the Hct, protein, albumin, ALP and cholesterol levels of the coagulopathy group were significantly decreased compared to those levels of the normal group, and the cholesterol level of the overt DIC group was lower than that of the non-over DIC group. The decrease of Hct was considered to be caused by the venom's toxicity in blood, and the lower levels of protein, albumin and cholesterol were thought to be due to their leakage and loss outside the blood locally or systemically because of the loss of vessel walls and the increased permeability of the blood vessels due to the venom's cytotoxicity11). Winkler et al.11) reported that the more serious a snakebite was, the lower was the cholesterol level, and the albumin level also tended to decrease with serious snake bite, although the tendency was not statistically significant. The findings of this study that the cholesterol and albumin levels declined after poisonous snakebite in the coagulopathy group and that the cholesterol level was more decreased in the DIC group meant that the degree of coagulopathy was proportionally correlated with the toxicity of venoms and the seriousness of the bite. When the relations between the various clinical symptoms caused by poisonous snake bite and coagulopathy were analyzed statistically, leukocytosis and rhabdomyolysis were meaningfully associated for the coagulopathy group, and hemolysis and rhabdomyolysis were meaningfully associated for the DIC group. One of the characteristic things from this finding was that rhabdomyolysis showed a close correlation with coagulopathy and DIC and this was the same when assessing the risk factors of coagulopathy. The significant variables evaluated on univariate analysis, that is, Hct, protein, albumin, ALP, cholesterol, thrombocytosis, rhabdomyolysis and hemolysis, were analyzed by multivariate logistic regression analysis and rhabdomyolysis was found to be a significant risk factor for coagulopathy following snake bite. When rhabdomyolysis was observed after poisonous snake bite, coagulopathy occurred five times more often in the patients with rhabdomyolysis than that noted in the patients without rhabdomyolysis. The mechanism for rhabdomyolysis's critical role in inducing coagulopathy was thought to be as follows. Rhabdomyolysis extricates many tissue factors of the damaged tissues into the blood and the exposed factors activate the extrinsic pathway of blood coagulation and so this leads to consumption coagulopathy. If this progress is limited, then simple coagulation abnormality happens. Yet when activation of the pathway and consumption coagulopathy happen to a severe degree, then disseminated thrombosis and the following fibrinolysis can occur, along with inducing DIC. The role of rhabdomyolysis in the occurrence of coagulopathy after snake bite was considered to be additional or essential12).
Although the coagulopathy following snakebite improved without specific complications in most cases, its complications were mainly caused by hemorrhage and in rare cases, by infarction13). The period of morbidity of the disease was about 6~7 days, based on the increase of the PT and the consistency of the thrombocytopenia.
As a result, the progress and prognosis of coagulopathy after snake bite is proportional to the seriousness of the bite, so evaluation by interview is important to predict and assess the initial seriousness. Further, the decreased Hct, protein, albumin and cholesterol levels noted on the blood and serum tests are thought to be factors to indirectly examine the seriousness of a snakebite. In particular, as the rhabdomyolysis that follows the bite can indicate a high risk of coagulopathy, the presence of coagulopathy should be checked. When considering the high risk of coagulopathy, if the snakebite is serious and rhabdomyolysis occurs in spite of the normal results of the initial blood coagulation test, then the occurrence of delayed coagulopathy should be examined with performing blood and serum tests 1~2 days after the bite. It should be recognized that coagulopathy following poisonous snakebite can induce various complications that are caused by infarction, as well as that presence of hemorrhage and the treatments and responses should be predicted, evaluated and followed up with considering the morbidity period, which is around 6~7 days.
References
- 1.Lee JA, Kim SY, Hyun SC, Park SM, Park JS, Kim GT. Clinical features in snake bite. J Korean Soc Emerg Med. 1996;7:580–589. [Google Scholar]
- 2.Han BG, Choi SO, Kim HY, Kang NK, Ryu JS, Lee KH. A study of the complication of poisonous snake bite. Korean J Intern Med. 1996;50:399–404. [Google Scholar]
- 3.Hasiba U, Rosenbach LM, Rockwell D, Lewis JH. DIC-like syndrome after envenomation by the snake, Crotalus horridus horridus. N Engl J Med. 1975;292:505–507. doi: 10.1056/NEJM197503062921004. [DOI] [PubMed] [Google Scholar]
- 4.Levi M. Disseminated intravascular coagulation: what's new? Crit Care Clin. 2005;21:449–467. doi: 10.1016/j.ccc.2005.02.001. [DOI] [PubMed] [Google Scholar]
- 5.Bick RL. Disseminated intravascular coagulation, current concepts of etiology, pathophysiology, diagnosis, and treatment. Hematol Oncol Clin North Am. 2003;17:149–176. doi: 10.1016/s0889-8588(02)00102-8. [DOI] [PubMed] [Google Scholar]
- 6.Retzios AD, Markland FS., Jr A direct-acting fibrinolytic enzyme from the venom of Agkistrodon contortrix contortrix: effects on various components of the human blood coagulation and fibrinolysis systems. Thromb Res. 1988;52:541–552. doi: 10.1016/0049-3848(88)90127-2. [DOI] [PubMed] [Google Scholar]
- 7.Retzios AD, Markland FS., Jr Purification, characterization, and fibrinogen cleavage sites of three fibrinolytic enzymes from the venom of Crotalus basiliscus basiliscus. Biochemistry. 1992;31:4547–4557. doi: 10.1021/bi00134a003. [DOI] [PubMed] [Google Scholar]
- 8.Retzios AD, Markland FS. Fibrinolytic enzymes from the venoms of Agkistrodon contortrix contortrix and Crotalus basiliscus basiliscus: cleavage site specificity towards the alpha-chain of fibrin. Thromb Res. 1994;74:355–367. doi: 10.1016/0049-3848(94)90151-1. [DOI] [PubMed] [Google Scholar]
- 9.Nordt SP, Clark RF. Rattlesnakes and other crotalids. In: Ford MD, Delaney KA, Ling LJ, Erickson T, editors. Clinical toxicology. 1st ed. Philadelphia: WB Saunders; 2001. pp. 863–872. [Google Scholar]
- 10.Singletary EM, Rochman AS, Bodmer JC, Holstege CP. Envenomation. Med Clin North Am. 2005;89:1195–1224. doi: 10.1016/j.mcna.2005.07.001. [DOI] [PubMed] [Google Scholar]
- 11.Winkler E, Chovers M, Almog S, Pri-Chen S, Rotenberg M, Tirosh M, Ezra D, Halkin H. Decreased serum cholesterol level after snake bite (Vipera palaestinae) as a marker of severity of envenomation. J Lab Clin Med. 1993;121:774–778. [PubMed] [Google Scholar]
- 12.Liebman HA, Weitz IC. Disseminated intravascular coagulation. In: Hoffman R, Benz EJ Jr, Shattil SJ, Furie B, Cohen HJ, Silberstein LE, McGlave P, editors. Hoffman hematology: basic principles and practice. 4th ed. Churchill: Livingstone; 2004. pp. 2169–2182. [Google Scholar]
- 13.Lee HM, Hong HP, Kim DP, Kim MC, Ko YG. Cerebral infarction following snake bite. J Korean Soc Emerg Med. 2004;15:420–425. [Google Scholar]