Abstract
AIM: To investigate the persistence of side population (SP) cells in pancreatic cancer and their role and mechanism in the drug resistance.
METHODS: The presentation of side population cells in pancreatic cancer cell line PANC-1 and its proportion change when cultured with Gemcitabine, was detected by Hoechst 33342 staining and FACS analysis. The expression of ABCB1 and ABCG2 was detected by real-time PCR in either SP cells or non-SP cells.
RESULTS: SP cells do exist in PANC-1, with a median of 3.3% and a range of 2.1-8.7%. After cultured with Gemcitabine for 3 d, the proportion of SP cells increased significantly (3.8% ± 1.9%, 10.7% ± 3.7%, t = 4.616, P = 0.001 < 0.05). ABCB1 and ABCG2 expressed at higher concentrations in SP as compared with non-SP cells (ABCB1: 1.15 ± 0.72, 5.82 ± 1.16, t = 10.839, P = 0.000 < 0.05; ABCG2: 1.16 ± 0.75, 5.48 ± 0.94, t = 11.305, P = 0.000 < 0.05), which may contribute to the efflux of fluorescent staining and drug resistance.
CONCLUSION: SP cells with inherently high resistance to chemotherapeutic agents do exist in pancreatic cancers, which may be candidate cancer stem cells contributing to the relapse of the tumor.
Keywords: Side population cells, Hoechst 33342, Drug resistance, Cancer stem cells, Pancreatic cancer
INTRODUCTION
Pancreatic cancer is one of the most aggressive malignancies and it is virtually incurable. Even for the patients who undergo potentially curative resection, the 5-year survival is less than 24% due to local recurrence and metastasis[1,2]. Emerging evidence has shown that cancer stem cells (CSCs), a small subset of cells within a tumor, are responsible for its malignancy[3]. So far, the significance of CSCs in hematological malignancy has been well known[4]. Although the presence and roles of these stem cells in solid tumors are poorly understood, their implication in breast carcinoma[5], brain cancers[6], prostate cancer[7] and lung cancer[8] are clear. As these cells must be eliminated in curative anti-cancer therapy, it is very important to identify and study CSCs.
Side population (SP) analysis could be used to identify CSCs[9]. SP cells can rapidly efflux lipophilic fluorescent dyes to produce a characteristic profile based on fluorescence-activated flow cytometric analysis[10]. Although representing only a small fraction of the whole cell population, they appear to be enriched in stem cells. Thus, they could provide a useful tool and a readily accessible source for cancer stem cell studies[11].
In addition to the application of SP cells in bone marrow obtained from patients with acute myeloid leukemia, which might be candidate leukemic stem cells[12], they have also been identified in various human solid tumors and cancer cell lines. Therefore, we presume that pancreatic cancer might also harbor SP cells, whose intrinsic dye efflux capacity is expected to be associated with the ability to export many cytotoxic drugs, hence increasing the risk of early relapse, and they may be candidate CSCs. We analyzed pancreatic cancer cell line PANC-1 and identified SP cells. The findings suggest that SP cells represent a previously unrecognized population of human pancreatic cancer cells. Their high drug efflux capacity is related to the strong expression of drug-transporter proteins (including ABCB1 and ABCG2), which may be responsible for the malignancy of pancreatic cancer.
MATERIALS AND METHODS
Materials
Pancreatic cancer cell lines, PANC-1, were obtained from the Cancer Research Institute of the Chinese Academy of Sciences.
Hoechst, verapamil and propidium iodide (PI): Hoechst 33342 (Sigma), verapamil (Sigma) and PI (Sigma) were dissolved in distilled deionized water at 1 g/L, 5 mmol/L, and 1 g/L, respectively. All solutions were filter sterilized. Aliquots were kept frozen at -20°C. Hoechst and verapamil were allowed to thaw at room temperature protected from light before use. Under these conditions, the same aliquot could be re-frozen and re-used multiple times for Hoechst and up to five times for verapamil. PI was also thawed at room temperature and subsequently stored at 4°C.
DMEM+: Dulbecco’s modified Eagle’s medium (Gibco) containing 2% (v/v) fetal calf serum (Gibco) and 10 mmol/L HEPES (Gibco) can be stored up to 4 wk at 4°C.
HBSS+: Hanks’ balanced salt solution (Gibco) containing 2% (v/v) fetal calf serum and 10 mmol/L HEPES can be stored up to 4 wk at 4°C.
PANC-1 medium: DMEM with 10% FBS (Gibco), 100 U/mL penicillin, 100 μg/mL streptomycin was stored at 4°C.
Gemcitabine (Eli Lilly) was dissolved in distilled deionized water at 1 g/L.
Primers of ABCB1, ABCG2 and β-actin were synthesized by Invitrogen Shanghai, China. Sequences of human primers used for real-time PCR experiments are shown in Table 1.
Table 1.
Sequences of human primers used for real-time PCR experiments
| Target mRNA | Primer sequence (5’-3’) | Accession number | Size (bp) |
| ABCB1 | 5′AGGTTCCAGGATTGGCGTCTT3′ | AF399931 | 156 |
| 5′CCAGTCATTGCTGCGGTTTCA3′ | 1152-1307 | ||
| ABCG2 | 5′AATACATCAGCGGATACTACAGAG3′ | AY333756 | 179 |
| 5′AGCCACCATCATAAGGGTAAACAT3′ | 1382-1560 | ||
| β-actin | 5’GAACGGTGAAGGTGACAG3’ | NM_001101 | 293 |
| 5’TAGAGAGAGTGGGGTGG3’ | 915-1207 |
Cell culture
The human pancreatic cancer cell line, PANC-1 was cultured as described above, and maintained in a 50 mL/L CO2 atmosphere at 37°C in a humidified incubator.
Hoechst 33342 and Pi dual-labeled dyeing
The cells, cultured to logarithmic phase, were prepared to single cell suspension in pre-warmed DMEM+. One g/L Hoechst 33342 was added to a final concentration of 5 mg/L, the cells were then incubated in the 37°C water bath for exactly 90 min. The cells were centrifuged at 500 × g, 4°C for 5 min and resuspended in 1-3 mL ice-cold HBSS+. Finally, the cells were counterstained with 2 mg/L PI for 5 min. The stained cells were then examined and photographed under an AX70 fluorescence microscope (Olympus, Orangeburg, NY).
Flow cytometry of SP cells
The SP was isolated with the technique described by Goodell et al[10]. The cells were cultured to logarithmic phase, then removed from the culture flask with trypsin and EDTA, washed, suspended at 106 cells/mL in pre-warmed DMEM+. The cells were then labeled in the same medium at 37°C for 90 min with 5 mg/L Hoechst 33342 dye, either alone or in combination with 50 μmol/L verapamil (a calcium channel blocker and an inhibitor of some ABC transporters). Finally, the cells were counterstained with 2 mg/L PI to label dead cells.
Then, 3-5 × 104 cells were analyzed in a FACSVantage fluorescence- activated cell sorter (Becton Dickinson, Mountain View, CA) using a dual-wavelength analysis (blue, 424-444 nm; red, 675 nm) after excitation with 350 nm UV light. PI-positive dead cells (< 10%) were excluded from the analysis. The SP or non-SP cells were sorted.
Efflux and survival studies for cytotoxic drug gemcitabine
To examine whether increased drug efflux results in a survival advantage, 104 PANC-1 cells were cultured with or without Gemcitabine at a concentration of 5 mg/L for 3 d, and the percentage of SP cells was determined subsequently by the method as described above.
Real-time RT PCR
The SP cells or non-SP cells were harvested, RNA was isolated from them separately. Real-time RT-PCR was done to detect the expression of human ABCB1 and ABCG2, β-actin was used as a control. Total RNA was extracted from 10 samples of SP cells or non-SP cells each. In RT reaction process, 4 μL mRNA and 0.5 μL Oligo (dt) were added to 6.5 μL distilled water. After annealing for 5 min at 70°C and immediate cooling on ice, 4.0 μm of 5 × first strand buffer, 2.0 μL of 10 mmol/L dNTP, 0.5 μL of RNasin and 0.5 μL RTase were added to get a total reaction volume of 20 μL. The reaction was allowed to proceed for 60 min at 37°C, followed by 5 min at 95°C to inactivate the enzyme. In real-time PCR assay, each cDNA sample was repeated three times. The total PCR volume consisted of 1 μL cDNA, 1 μL SYBRGreen PCRI, 5 μL 10 × buffer, 1.6 μL primers, 7 μL MgCl2, 0.5 μL Taq DNA Polymerase, 1 μL dNTP and 33 μL distilled water. After denaturation of the enzyme for 2 min at 94°C, the PCR assays were carried out for 45 cycles, with denaturation at 94°C for 30 s, annealing at 57°C for 30 s and extension at 72°C for 30 s. Fluorometric PCR was performed with the FTC-2000 System. The level of expression of each transporter protein gene was determined relative to the β-actin gene.
Statistical analysis
All data were expressed as mean ± SD. Student’s t test was used to determine changes in different groups. P < 0.05 was considered statistically significant.
RESULTS
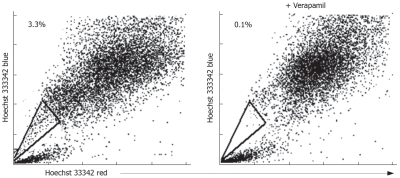
Morphology of SP cells under fluorescence microscope
To observe the morphology of SP cells under fluorescence microscope, we stained PANC-1 with Hoechst 33342 and PI. As SP cells are able to expel fluorescent dye, they were Hoechst 33342 negative, which were colorless, while non-SP cells were Hoechst 33342 positive, which generated blue fluorescence (Figure 1).
Figure 1.
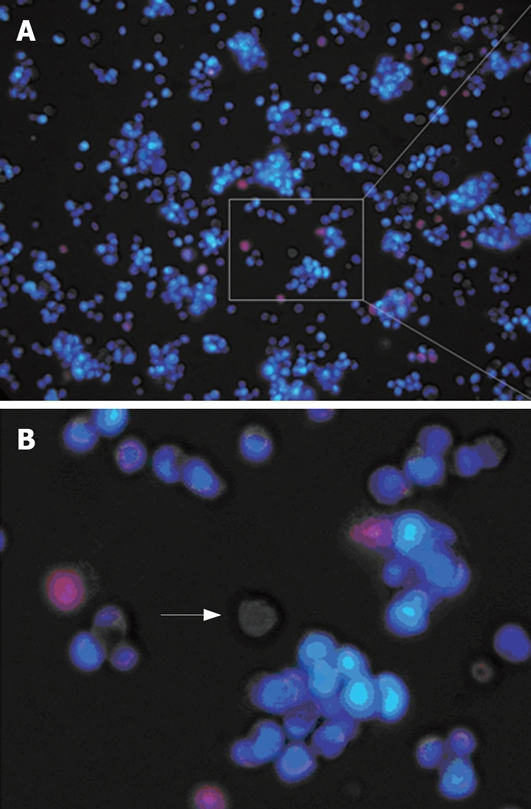
Hoechst 33342 and Pi dual-labeled dyeing.
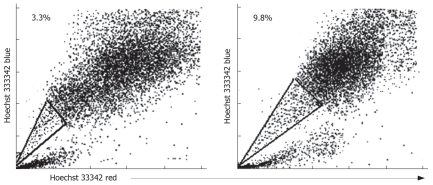
Prevalence of SP cells in PANC-1
To determine the prevalence of SP cells in PANC-1, we stained 10 samples with Hoechst 33342 and PI, and analyzed them by flow cytometry. PANC-1 contained SP cells ranged from 2.1% to 8.7% in the total viable cells. The SP population was decreased greatly after treatment with verapamil, indicating that the populations were bona fide SP cells (Figure 2). Thus, pancreatic cancer cell line, PANC-1, contains SP cells, despite being maintained in culture for many years.
Figure 2.
Existence of SP cells in PANC-1.
Efflux of gemcitabine from PANC-1 SP cells
To examine whether SP cells resist anti-cancer drugs more than non-SP cells do, we tested gemcitabine, which is usually used for the treatment of pancreatic cancer. The bulk cultures of PANC-1 cells were added 5 mg/L gemcitabine. By d 3, the proportion of SP cells increased (10.7% ± 3.7%, t = 4.616, P = 0.001, < 0.05), indicating the selection of this population (Figure 3).
Figure 3.
SP cells show a high resistance to anti-cancer-drugs.
Gene expression analysis
To investigate the association between SP phenotype and the expression of drug transporter genes, we isolated RNA from sorted SP and non-SP cells of PANC-1 and used a real-time RT-PCR assay to quantify the relative expression of two ABC transporter genes, ABCB1 and ABCG2. They were clearly expressed at higher concentrations in SP compared with non-SP cells (ABCB1: 1.15 ± 0.72, 5.82 ± 1.16, t = 10.839, P = 0.000 < 0.05; ABCG2: 1.16 ± 0.75, 5.48 ± 0.94, t = 11.305, P = 0.000 < 0.05) (Figure 4, Table 2).
Figure 4.
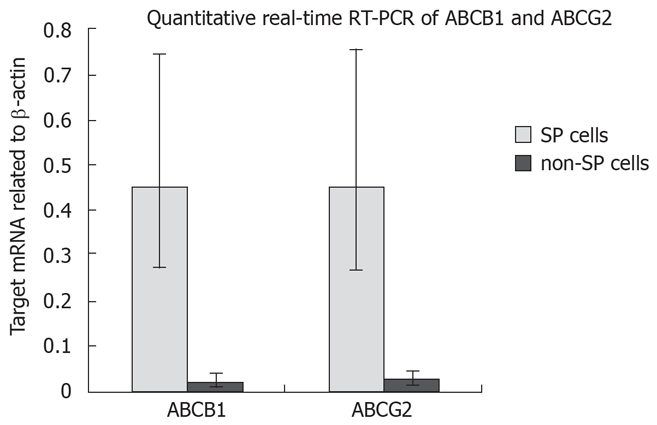
Relative expression of ABC transporter genes in PANC-1 SP and non-SP cells.
Table 2.
Relative quantitation of mRNA using the 2-ΔΔCT method
| Target mRNA | ΔCT |
Target mRNA |
|
| (Target mRNA-β-actin) | related to β-actin | ||
| non-SP cells | ABCB1 | 5.82 ± 1.16 | 0.0176 |
| (0.0079-0.0393) | |||
| ABCG2 | 5.48 ± 0.94 | 0.0224 | |
| (0.0116-0.0432) | |||
| SP cells | ABCB1 | 1.15 ± 0.72 | 0.4504 |
| (0.2731-0.7431) | |||
| ABCG2 | 1.16 ± 0.75 | 0.4483 | |
| (0.2662-0.7547) |
DISCUSSION
The discovery of CSCs in solid tumors has changed our view of carcinogenesis and chemotherapy. In the cancer stem cell model, only a rare subset of CSCs drives tumor formation, the new therapeutic strategies should account for the potential differences in drug sensitivity or target expression between the tumorigenic cells and the more frequent non-tumorigenic cells. Therefore, to identify CSCs is very important. Up to date, only two general approaches have been adopted to identify and characterize CSCs: (1) Molecular markers, i.e. CD44+/CD24- for breast CSCs[13], CD44+/alpha2 beta1hi/CD133+ for prostate CSCs[7], and CD34+/CD38- for leukemia stem cells[14]; (2) SP isolated from tumors which has been proven to be an alternative to study CSCs, for they are enriched in CSC. For example, Chiba et al[15] found that SP cells in hepatocellular carcinoma cells possessed extreme tumorigenic potential and provided heterogeneity to the cancer stem cell system characterized by distinct hierarchy. As specific cell surface markers are largely unknown, SP analysis becomes a more useful tool for stem cell studies. In addition, malignant SP cells’ intrinsic ability to expel anticancer drugs may directly improve their survival and sustain their clonogenicity during exposure to anticancer drugs, allowing disease recurrence when the therapy is withdrawn[16]. Identification of this tumor progenitor population might provide clues for improved therapeutic intervention.
Recently, SP cells have also been identified in various tumors and cancer cell lines, e.g. acute myeloid leukemia[12], neuroblastoma[17], melanoma[18], ovarian cancer[19], the C6 glioma cell line[20], human retinoblastoma cell line[21], human neuroblastoma cell lines[17], and various human gastrointestinal cancer cell lines[22]. However, no SP has been described in cell lines derived from Wilms’ tumor, rhabdomyosarcoma or osteosarcoma[17]. To investigate the prevalence of SP cells in human pancreatic cancers, we stained PANC-1 with Hoechst 33342 dye and identified the SP based on its characteristic fluorescent profile in dual-wavelength analysis, as described above. PANC-1 contained SP cells ranging from 2.1% to 8.7% (median 3.3%) of the total viable cells.
Our study of the SP covers one of the most interesting areas in cancer biology, regarding carcinogenesis and drug resistance in the cancer therapy. Our findings suggest that SP cells in PANC-1 have an enhanced efflux capacity not only for Hoechst 33342 dyes but also for anti-neoplastic drugs. After 72 h exposure to Gemcitabine, the viability of the SP cells became markedly higher than that of the non-SP cells. It is the drug efflux capacity of SP cells that affords them a survival advantage. These indicate that SP cells play an important role in maintaining cancer foci, which survive and proliferate after chemotherapy using their self-renewal and chemo-resistance capacities. They may be candidate pancreatic CSCs contributing to the relapse of the tumor.
The molecular mechanisms remain unclear that SP cells have intrinsic ability to expel dye and anticancer drugs. Goodell et al[10] demonstrated that multidrug resistance transporter 1 (MDR1), a member of ATP-binding cassette (ABC) transporter transmembrane proteins, may be involved in the efflux capacity of SP cells. But it cannot be taken as the single marker to identify and isolate SP cells, additional transporters should be analyzed. Zhou et al[23] demonstrated that ABCG2 has been shown to contribute to Hoechst 33342 efflux and produce an SP phenotype in a wild variety of tissues. Since SP is defined by ABC transporter activity, the expression of these transporters has been analyzed in various malignancies. For example, SP cells in a mouse glioma cell line and human neuroblastoma express high levels of ABCG2 and ABCA3[17], SP cells in hepatoma cell line, HuH7, express high levels of ABCG2 and ABCB1[22]. We also analyzed the expression of the ABC transporters in PANC-1, and found SP cells expressed higher levels of ABCB1 and ABCG2 than the non-SP cells. Therefore, ABCB1 and ABCG2 responsible for SP phenotype in pancreatic cancer could be speculated. However, some scholars proposed SP phenotype is not related to the presence of many “conventional” ABC transporter proteins such as MDR1, since MDR-1 knockout mice have normal numbers of SP cells[24]. So the SP cells’ intrinsic expel ability should be further studied.
As ABC transporters responsible for SP phenotype are implicated in drugs resistance and lower responses to cancer therapy[25,26], targeting the SP may offer an alternative option to improve drug resistance. Since ABC transporters are expressed in both normal and cancerous cells[27,28], they cannot be used to selectively target cancer cells unless specific strategies are applied. However, a whole genome DNA microarray analysis among normal SP cells, normal non-SP cells tumor SP cells and tumor non-SP cells, may be useful to identify potential candidates for specific CSCs markers, or even to define a CSCs pattern. The fact that CSCs specific surface markers are discovered, may permit isolation of this important population of cells, and revolutionize the cancer therapy and science[29,30].
COMMENTS
Background
Pancreatic cancer is one of the most aggressive malignancies and it is virtually incurable. Over the past two decades, major advances in the understanding of this cancer have shifted to only increment of survival for the patients. Recent data suggested that cancers arising from rare stem cells are biologically distinct from their more numerous differentiated progeny, which may explain this paradox.
Research frontiers
This study focuses on the persistence of side population cells in pancreatic cancer and their role and mechanism in the drug resistance.
Innovation and breakthroughs
The difference from other related or similar studies is that, it is a new point of view to study drug resistance in pancreatic cancer.
Application
Identification of side population cells in pancreatic cancer might provide clues for improved therapeutic intervention. New drug development in pancreatic cancer should focus on this tumor progenitor population.
Terminology
Side population (SP) cells are cells which can rapidly efflux lipophilic fluorescent dyes to produce a characteristic profile based on fluorescence-activated flow cytometric analysis. Although representing only a small fraction of the whole cell population, they appear to be enriched in stem cells.
Peer review
This report demonstrates that SP cells with inherently high resistance to chemotherapeutic agents exist in pancreatic cancer and may be candidate cancer stem cells contributing to the relapse of the tumor.
Acknowledgments
The authors are grateful to the technical assistance from the Research Laboratory of General Surgery, Union Hospital, Wuhan.
Supported by The National Natural Science Foundation of China, No. 30571817
Peer reviewer: James M Millis, Professor, University of Chicago, Section of Transplantation, MC 5027, 5841 S. Maryland Avenue, Chicago, IL 60637, United States
S- Editor Chen X L- Editor Ma JY E- Editor Liu Y
References
- 1.Griffin JF, Smalley SR, Jewell W, Paradelo JC, Reymond RD, Hassanein RE, Evans RG. Patterns of failure after curative resection of pancreatic carcinoma. Cancer. 1990;66:56–61. doi: 10.1002/1097-0142(19900701)66:1<56::aid-cncr2820660112>3.0.co;2-6. [DOI] [PubMed] [Google Scholar]
- 2.Cameron JL, Crist DW, Sitzmann JV, Hruban RH, Boitnott JK, Seidler AJ, Coleman J. Factors influencing survival after pancreaticoduodenectomy for pancreatic cancer. Am J Surg. 1991;161:120–124; discussion 124-125. doi: 10.1016/0002-9610(91)90371-j. [DOI] [PubMed] [Google Scholar]
- 3.Al-Hajj M, Clarke MF. Self-renewal and solid tumor stem cells. Oncogene. 2004;23:7274–7282. doi: 10.1038/sj.onc.1207947. [DOI] [PubMed] [Google Scholar]
- 4.Bonnet D, Dick JE. Human acute myeloid leukemia is organized as a hierarchy that originates from a primitive hematopoietic cell. Nat Med. 1997;3:730–727. doi: 10.1038/nm0797-730. [DOI] [PubMed] [Google Scholar]
- 5.Al-Hajj M, Wicha MS, Benito-Hernandez A, Morrison SJ, Clarke MF. Prospective identification of tumorigenic breast cancer cells. Proc Natl Acad Sci USA. 2003;100:3983–3988. doi: 10.1073/pnas.0530291100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Singh SK, Hawkins C, Clarke ID, Squire JA, Bayani J, Hide T, Henkelman RM, Cusimano MD, Dirks PB. Identification of human brain tumour initiating cells. Nature. 2004;432:396–401. doi: 10.1038/nature03128. [DOI] [PubMed] [Google Scholar]
- 7.Collins AT, Berry PA, Hyde C, Stower MJ, Maitland NJ. Prospective identification of tumorigenic prostate cancer stem cells. Cancer Res. 2005;65:10946–10951. doi: 10.1158/0008-5472.CAN-05-2018. [DOI] [PubMed] [Google Scholar]
- 8.Kim CF, Jackson EL, Woolfenden AE, Lawrence S, Babar I, Vogel S, Crowley D, Bronson RT, Jacks T. Identification of bronchioalveolar stem cells in normal lung and lung cancer. Cell. 2005;121:823–835. doi: 10.1016/j.cell.2005.03.032. [DOI] [PubMed] [Google Scholar]
- 9.Hadnagy A, Gaboury L, Beaulieu R, Balicki D. SP analysis may be used to identify cancer stem cell populations. Exp Cell Res. 2006;312:3701–3710. doi: 10.1016/j.yexcr.2006.08.030. [DOI] [PubMed] [Google Scholar]
- 10.Goodell MA, Brose K, Paradis G, Conner AS, Mulligan RC. Isolation and functional properties of murine hematopoietic stem cells that are replicating in vivo. J Exp Med. 1996;183:1797–1806. doi: 10.1084/jem.183.4.1797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Taga T. Identification of cancer stem cells in the “side population”. Gan To Kagaku Ryoho. 2006;33:295–299. [PubMed] [Google Scholar]
- 12.Wulf GG, Wang RY, Kuehnle I, Weidner D, Marini F, Brenner MK, Andreeff M, Goodell MA. A leukemic stem cell with intrinsic drug efflux capacity in acute myeloid leukemia. Blood. 2001;98:1166–1173. doi: 10.1182/blood.v98.4.1166. [DOI] [PubMed] [Google Scholar]
- 13.Ponti D, Costa A, Zaffaroni N, Pratesi G, Petrangolini G, Coradini D, Pilotti S, Pierotti MA, Daidone MG. Isolation and in vitro propagation of tumorigenic breast cancer cells with stem/progenitor cell properties. Cancer Res. 2005;65:5506–5511. doi: 10.1158/0008-5472.CAN-05-0626. [DOI] [PubMed] [Google Scholar]
- 14.Raaijmakers MH, de Grouw EP, Heuver LH, van der Reijden BA, Jansen JH, Scheper RJ, Scheffer GL, de Witte TJ, Raymakers RA. Breast cancer resistance protein in drug resistance of primitive CD34+38- cells in acute myeloid leukemia. Clin Cancer Res. 2005;11:2436–2444. doi: 10.1158/1078-0432.CCR-04-0212. [DOI] [PubMed] [Google Scholar]
- 15.Chiba T, Kita K, Zheng YW, Yokosuka O, Saisho H, Iwama A, Nakauchi H, Taniguchi H. Side population purified from hepatocellular carcinoma cells harbors cancer stem cell-like properties. Hepatology. 2006;44:240–251. doi: 10.1002/hep.21227. [DOI] [PubMed] [Google Scholar]
- 16.Dean M, Fojo T, Bates S. Tumour stem cells and drug resistance. Nat Rev Cancer. 2005;5:275–284. doi: 10.1038/nrc1590. [DOI] [PubMed] [Google Scholar]
- 17.Hirschmann-Jax C, Foster AE, Wulf GG, Nuchtern JG, Jax TW, Gobel U, Goodell MA, Brenner MK. A distinct "side population" of cells with high drug efflux capacity in human tumor cells. Proc Natl Acad Sci USA. 2004;101:14228–14233. doi: 10.1073/pnas.0400067101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Grichnik JM, Burch JA, Schulteis RD, Shan S, Liu J, Darrow TL, Vervaert CE, Seigler HF. Melanoma, a tumor based on a mutant stem cell? J Invest Dermatol. 2006;126:142–153. doi: 10.1038/sj.jid.5700017. [DOI] [PubMed] [Google Scholar]
- 19.Szotek PP, Pieretti-Vanmarcke R, Masiakos PT, Dinulescu DM, Connolly D, Foster R, Dombkowski D, Preffer F, Maclaughlin DT, Donahoe PK. Ovarian cancer side population defines cells with stem cell-like characteristics and Mullerian Inhibiting Substance responsiveness. Proc Natl Acad Sci USA. 2006;103:11154–11159. doi: 10.1073/pnas.0603672103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kondo T, Setoguchi T, Taga T. Persistence of a small subpopulation of cancer stem-like cells in the C6 glioma cell line. Proc Natl Acad Sci USA. 2004;101:781–786. doi: 10.1073/pnas.0307618100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Seigel GM, Campbell LM, Narayan M, Gonzalez-Fernandez F. Cancer stem cell characteristics in retinoblastoma. Mol Vis. 2005;11:729–737. [PubMed] [Google Scholar]
- 22.Haraguchi N, Utsunomiya T, Inoue H, Tanaka F, Mimori K, Barnard GF, Mori M. Characterization of a side population of cancer cells from human gastrointestinal system. Stem Cells. 2006;24:506–513. doi: 10.1634/stemcells.2005-0282. [DOI] [PubMed] [Google Scholar]
- 23.Zhou S, Schuetz JD, Bunting KD, Colapietro AM, Sampath J, Morris JJ, Lagutina I, Grosveld GC, Osawa M, Nakauchi H, et al. The ABC transporter Bcrp1/ABCG2 is expressed in a wide variety of stem cells and is a molecular determinant of the side-population phenotype. Nat Med. 2001;7:1028–1034. doi: 10.1038/nm0901-1028. [DOI] [PubMed] [Google Scholar]
- 24.Uchida N, Leung FY, Eaves CJ. Liver and marrow of adult mdr-1a/1b(-/-) mice show normal generation, function, and multi-tissue trafficking of primitive hematopoietic cells. Exp Hematol. 2002;30:862–869. doi: 10.1016/s0301-472x(02)00879-2. [DOI] [PubMed] [Google Scholar]
- 25.Hadnagy A, Gaboury L, Beaulieu R, Balicki D. SP analysis may be used to identify cancer stem cell populations. Exp Cell Res. 2006;312:3701–3710. doi: 10.1016/j.yexcr.2006.08.030. [DOI] [PubMed] [Google Scholar]
- 26.Staud F, Pavek P. Breast cancer resistance protein (BCRP/ABCG2) Int J Biochem Cell Biol. 2005;37:720–725. doi: 10.1016/j.biocel.2004.11.004. [DOI] [PubMed] [Google Scholar]
- 27.Donnenberg VS, Luketich JD, Landreneau RJ, DeLoia JA, Basse P, Donnenberg AD. Tumorigenic epithelial stem cells and their normal counterparts. Ernst Schering Found Symp Proc. 2006;5:245–263. doi: 10.1007/2789_2007_054. [DOI] [PubMed] [Google Scholar]
- 28.Raaijmakers MH. ATP-binding-cassette transporters in hematopoietic stem cells and their utility as therapeutical targets in acute and chronic myeloid leukemia. Leukemia. 2007;21:2094–2102. doi: 10.1038/sj.leu.2404859. [DOI] [PubMed] [Google Scholar]
- 29.Kakarala M, Wicha MS. Cancer stem cells: implications for cancer treatment and prevention. Cancer J. 2007;13:271–275. doi: 10.1097/PPO.0b013e318156da4e. [DOI] [PubMed] [Google Scholar]
- 30.Huff CA, Matsui WH, Douglas Smith B, Jones RJ. Strategies to eliminate cancer stem cells: clinical implications. Eur J Cancer. 2006;42:1293–1297. doi: 10.1016/j.ejca.2006.01.045. [DOI] [PubMed] [Google Scholar]