Abstract
Solid-pseudopapillary tumor (SPT) is a rare neoplasm of the pancreas that usually occurs in young females. It is generally considered a low-grade malignant tumor that can remain asymptomatic for several years. The occurrence of infiltrating varieties of SPT is around 10%-15%. Between 1986 and 2006, 282 cystic tumors of the pancreas were observed. Among them a SPT was diagnosed in 8 patients (2.8%) with only one infiltrating variety. This was diagnosed in a 49-year-old female 13 years after the sonographic evidence of a small pancreatic cystic lesion interpreted as a pseudocyst. The tumor invaded a long segment of the portal-mesenteric vein confluence, and was removed with a total pancreatectomy, resection of the portal vein and reconstruction with the internal jugular vein. Histological examination confirmed the R-0 resection of the primary SPT, although a vascular invasion was demonstrated. The postoperative course was uneventful, but 32 mo after surgery the patient experienced diffuse liver metastases. Chemotherapy with different drugs was started. The patient is alive and symptom-free, with stable disease, 75 mo after surgery. Twenty-five patients with invasion of the portal vein and/or of mesenteric vessels were retrieved from the literature, 16 recent patients with tumor relapse after potentially curative resection were also retrieved. The best treatment remains a radical resection whenever possible, even in locally advanced or metastatic disease. The role of chemotherapy, and/or radiotherapy, is still to be defined.
Keywords: Solid-pseudopapillary tumor, Pancreatectomy, Vascular resection, Liver metastases, Follow-up
INTRODUCTION
Solid pseudopapillary tumor (SPT) of the pancreas was first reported by Frantz in 1959[1], and represents a rare tumor that occurs most frequently in young women (90%). The widespread use of imaging techniques, together with a better knowledge of the disease, has prompted a rapidly increasing number of case reports. A recent review of the English literature from 1933 to 2003 collected a total of 718 SPTs, including pediatric cases[2].
Although SPT is considered an indolent lesion with a low malignant potential and a favorable prognosis after surgical resection, some cases of locally infiltrating and metastatic variety, or recurrences after surgery, have been reported. Moreover, long-term survival is described even for metastatic disease, suggesting a widely variable and not clearly elucidated biology of this tumor.
We report a patient with an infiltrating SPT that underwent total pancreatectomy and wide vascular resection. The tumor recurred in the liver 32 mo after surgery and chemotherapy was started. Between 1986 and 2006, we observed 8 SPTs among 282 cystic tumors of the pancreas (2.8%), the remaining 7 patients were cured by surgery and are alive and disease-free (Table 1).
Table 1.
Patient characteristics
| Patient | Sex | Age | Site | Size | Treatment | Follow-up (mo) |
| 1 | F | 54 | Tail | 4 | DP | A, NED (252) |
| 2 | F | 13 | Body | 4 | CP | A, NED (171) |
| 3 | F | 32 | Tail | 7 | DP | A, NED (120) |
| 4 | F | 31 | Tail | 14 | DP | A, NED (108) |
| 5 | F | 49 | Body-tail | 10 | TP | A, WD (77) |
| 6 | F | 20 | Tail | 10 | DP | A, NED (75) |
| 7 | F | 14 | Tail | 10 | DP | A, NED (48) |
| 8 | M | 59 | Tail | 11 | DP | A, NED (12) |
DP: Distal pancreatectomy; CP: Central pancreatectomy; TP: Total pancreate-ctomy; A: Alive; NED: No evidence of disease; WD: With disease.
A literature review of infiltrating SPTs allowed us to find 25 patients with invasion of the portal vein and/or of mesenteric vessels, and 16 recent patients with tumor relapse after potentially curative resection.
CASE REPORT
A 49-year-old woman was admitted to another hospital in February 2001 because of an 8 mo history of palpable abdominal mass. A 2-cm cystic lesion of the tail of the pancreas was detected by an abdominal ultrasonography 13 years ago, and interpreted as a pancreatic pseudocyst. Physical examination revealed a hard mass in the left upper quadrant of the abdomen. Routine laboratory tests including carcinoembryonic antigen (CEA) and CA 19-9 were within the normal range. A CT-scan showed a 10-cm abdominal mass with an irregular low density pattern in the body and tail of the pancreas. At laparotomy a neoplastic mass involving the body and tail of the pancreas, with encasement of the portal and superior mesenteric vein confluence, was found. A core biopsy of the mass was performed, but it was referred as non diagnostic. The tumor was judged unresectable. Soon after the patient was referred to our department, MRI showed a mass of about 8 cm in diameter with an irregular intensity both in T1 and in T2 enhanced-images, surrounded by a capsule (Figure 1). The splenic vessels were encased by the tumor, but the portal vein, superior mesenteric vessels, and celiac trunk were apparently free. A positron emission tomography with 18-fluorodeoxyglucose (18FDG-PET) showed a peripheral, pathologic uptake with central absence of metabolism (SUV = 3.5). In the presumption of a cystadenocarcinoma of the pancreas the patient underwent explorative laparotomy. A thick-walled encapsulated mass, 10 cm × 10 cm in size, was found in the body and tail of the pancreas. There were no metastatic lesions in the liver or distant organs, but the portal-mesenteric vein confluence was infiltrated by the tumor. A pylorus-preserving total pancreatectomy with resection of the portal vein was performed. The mesenteric-portal vein was reconstructed with the interposition of the right internal jugular vein.
Figure 1.
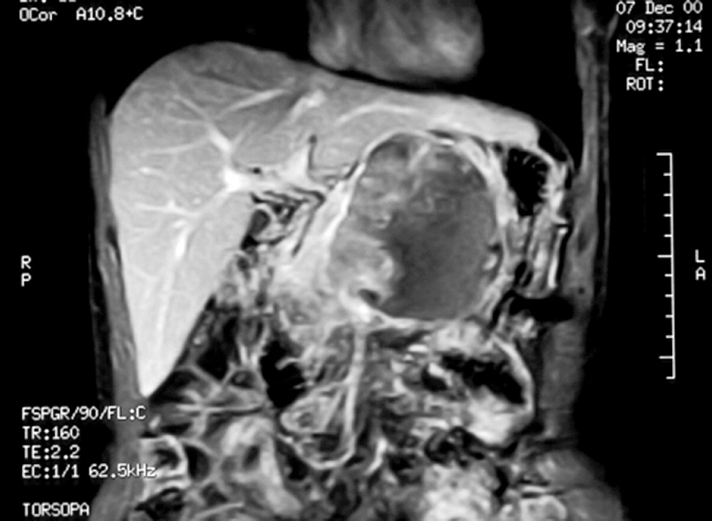
MRI of the abdomen showing a large, solid-cistyc mass of the pancreas.
The postoperative course was uneventful and no adjuvant therapy was given. The patient was discharged from the hospital 16 d after surgery.
Histopathology
The pathological investigation showed a 10.0 cm × 10.0 cm × 9.5 cm pancreatic tumor partially demarcated by a fibrous capsule. Gross pathomorphology of the cut surface showed an inhomogeneous solid appearance with areas of extensive necrosis. Although the mass was partially encapsulated, it directly invaded the peripancreatic fat tissue and the muscular layer of the portal vein with no involvement of the resection margins. Microscopically, solid areas composed of monomorphic epithelioid cells showing venous invasion and a moderate cellular atypia without mitotic activity were noted. Characteristic pseudopapillary formations were frequently observed. Twenty-seven lymph nodes examined were free of tumor. Immunohistochemistry was uniformly positive for vimentin, alfa-1-antitrypsin and CD10 staining. Strong immunoreactivity was also found for neuron-specific enolase (NSE). Focal reactivity was detected for synaptophysin, while negative reactions were found for cytokeratins (pan-cytokeratin, CAM 5.2), CEA, progesterone and estrogen receptors.
On the basis of these characteristic morphologic and immunohistochemical findings, the diagnosis of locally invasive SPT of the pancreas was made.
Follow-up
Follow-up included clinical examination, routine laboratory tests, abdominal US and/or CT/MRI every 6 mo. Thirty-two months after surgery, abdominal CT showed multiple metastatic lesions throughout the entire liver (Figure 2). The greater lesions (from 1.0 cm to 2.5 cm) were present in segments IV, VI, VII, and VIII of the liver. The patient was asymptomatic. A whole body 18FDG-PET confirmed some areas of pathological metabolic activity in the liver. A percutaneous liver biopsy under US guidance was performed. The histology showed a metastatic SPT of the pancreas. Immunoreactivity for estrogen and progesterone receptors was negative.
Figure 2.
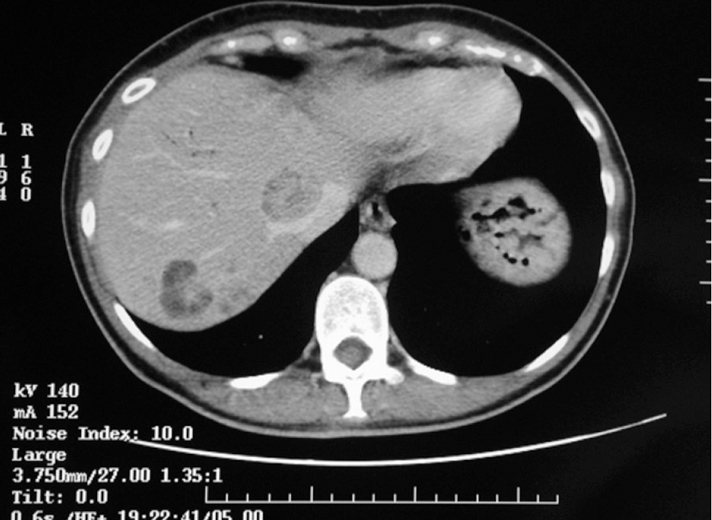
CT of abdomen showing multiple liver metastase with solid-cystic appearance.
Radical excision of metastatic nodules was considered unfeasible, and chemotherapy was started. The patient received 6 cycles of weekly gemcitabine (1000 mg/m2) and tolerated it quite well. Afterwards, different regimens of drugs were tested because of slow disease progression (size and number of liver metastases, lymph node metastases): 3 cycles of gemcitabine + irinotecan, 8 cycles of oxaliplatin + irinotecan + capecitabine, 6 cycles of gemcitabine + capecitabine, 2 mo of weekly 5-FU. Finally, from September 2006 until present, the patient received capecitabine (2000 mg/m2). CT-scan showed stable disease, and the patient was alive and symptom free at the time we wrote this paper.
DISCUSSION
SPT is a rare neoplasm of the pancreas, accounting for only 1%-2% of all exocrine pancreatic tumors[3]. We observed 8 SPTs among a total of 282 (2.8%) cystic tumors of the pancreas from 1986 to 2006 (Table 1). SPT is generally considered a tumor with a low malignant potential, usually occurring in young females in their second or third decade of life[2,4]. Although resection of the tumor provides a 5-year survival rate of 97%, local recurrence or distant metastases can occur in a significant number of patients[4]. Moreover, in a minority of patients a locally advanced or metastatic disease is discovered at their initial presentation, as in our 49-year-old patient. However, when she was 36-year-old, a 2-cm cystic mass was incidentally discovered in the tail of the pancreas and misinterpreted as a pancreatic pseudocyst and no further investigation was made until the palpable abdominal mass was discovered. Therefore it is reasonable to believe that a SPT was present at least 13 years before the mass was discovered. The doubling time, based on the Schwartz’ formula[5], was 677, a value between 240 and 765 d of the two other patients in whom the doubling time was reported[6]. This finding, together with the absence of mitotic activity, confirms the slow growing pattern of this neoplasm, but also the need of a regular follow-up for pancreatic cystic lesions left unresected.
At presentation, the tumor showed an infiltrative pattern invading a segment of the portal vein that was en-bloc resected with the entire gland in order to achieve tumor-free margins. Locally infiltrative SPTs of the pancreas occur infrequently. A recent review of the English literature until December 2003[2] showed that among 497 patients with data on invasion or metastases, portal vein was involved in 26 patients (5%), other organs (spleen, colon, duodenum, etc.) in 44 (9%), but the details on treatment and outcome of these patients were not reported. We retrieved 13 patients[7–15] previously reported as “invasion of portal and/or mesenteric vein” by Mao et al[3], two of them[14] were actually “histological venous invasion” and were then excluded from further consideration. Fourteen patients reported after 1995 were also retrieved[16–28] for a total of 26 patients including our patient, with SPT involving vascular structures (Table 2). Liver metastases were also present in three patients[10,16,23], invasion of colon[22] or peritoneal dissemination[11] in one each. Seventeen patients[7,8,12,13,15,16,19–24,28] underwent vascular resection and reconstruction without operative mortality. Liver metastases were also removed in two patients together with the primary tumor[16,23]. One died of unrelated disease[15] and all the others are still alive: one after enucleation of liver metastasis 18 mo after pancreatic resection, one (our patient) with liver metastases. The mean and median survival periods of time were 36.9 and 36 mo (range 5-84). Nine patients[9–11,15,17,25–27] were unresectable because of vascular infiltration, liver metastases or peritoneal dissemination. The mean and median survival periods of time were 55.5 and 47 mo (range 8-156). Two of them died of disease after 47 and 99 mo, one died of unrelated cause after 71 mo and one is alive with disease after 60 mo. Based on these data, vascular resection seems not so useful, but we must consider a publication bias due to the usual earlier publication of the results of resective surgery when compared to palliative and explorative surgery or to no surgery at all. Unfortunately, the long term results of many patients who underwent vascular resection have not been reported.
Table 2.
Treatment and outcome of patients with SPT involving vascular structures
| Author | Yr | Sex | Site of infiltration | Therapy | Follow-up (mo) |
| Sanfey et al[7]a | 1982 | F | SMV | TP, vascular resection and reconstruction | 7, A&W |
| Dales et al[8]a | 1983 | F | PV | TP, vascular resection and reconstruction, RT | A&Wd |
| Fried et al[9]a | 1985 | F | PV and HA | Unresectable, RT | 36, A&W |
| Matsuda et al[10]a | 1987 | F | PV and liver metastasis | Unresectable, Chemoembolization, CT | 60, AWD |
| Matsunou & Konishi[11]a | 1990 | F | PV and peritoneal dissemination | Unresectable, RT & CT | 47, DOD |
| Zinner et al[12]a | 1990 | F | PV | DP, vascular resection and reconstruction | 48, A&W |
| 1990 | F | PV | TP, vascular resection and reconstruction | 84, A&W | |
| Tsunoda et al[13]a | 1991 | M | PV | Whipple, vascular resection and reconstruction | 22, A&W |
| Nishihara et al[14]a | 1993 | F | Venous invasion | Resectedb | 3, A&W |
| F | Venous invasion | Resectedb | 13, A&W | ||
| F | PV | Whipple, vascular resection and reconstruction | 66, DUC | ||
| Jeng et al[15]a | 1993 | F | PV and SMA | Unresectable, Roux-en-Y cystojejunostomy | 83, DUC |
| F | PV | Whipple, vascular resection and reconstruction | 40, A&W | ||
| Saiura et al[16] | 2000 | F | PV with thrombus, liver metastases | DP with splenectomy, extended right lobectomy, partial resection of the liver, vascular resection | 8, A&W |
| Martin et al[17] | 2002 | NA | SMA encasement | Unresectable | 156, alive |
| NA | SMA encasement | Unresectable | 12, alive | ||
| Goh et al[18]c | 2003 | F | PV | PD, vascular resection and reconstruction | 67, NED |
| Podevin J[20] | 2003 | F | SMV | PD, vascular resection and reconstruction, segmental colectomy | 12, A&W |
| Usatoff et al[21] | 2004 | F | SMV | PD, vascular resection and reconstruction | 5, NED |
| Hassan et al[22] | 2005 | F | PV, colon | PD, vascular resection and reconstruction. Enucleation of liver metastases after 12 mo | 18, NED |
| Chen et al[23] | 2005 | F | PV, liver metastasis. | Resection of both primary and metastatic lesions and the portal vein | 36, A&W |
| Frago et al[24] | 2006 | F | PV | Duodenum preserving subtotal pancreatectomy, vascular resection and reconstruction | 76, A&W |
| Hao et al[25] | 2006 | F | SMA, SMV | Unresectable, internal drainage | 8, NED |
| Zauls et al[26] | 2006 | F | PV and SMV | Unresectable, RT | 18, alive |
| Tipton et al[27] | 2006 | NA | SMV | Unresectable, gastroenteroanastomosis | 92, DOD |
| Cheng-Hong et al[28] | 2006 | F | PV | PD, vascular resection and reconstruction | > 12, NA |
| F | SMV | PD, vascular resection and reconstruction | > 12, NA | ||
| Present case | 2007 | F | SMV | TP, vascular resection and reconstruction, CT | 77, AWD |
aPatients included in Mao's review[3];
Patients erroneously included as vascular invasion, histological venous invasion was only present; cPreviously reported by NG et al[18]; dDuration of follow-up not stated; SMA: Superior mesenteric artery; HA: Hepatic artery; PV: Portal vein; SMV: Superior mesenteric vein; RT: Radiotherapy; CT: Chemotherapy; PD: Pancreaticoduodenectomy; DP: Distal pancreatectomy; TP: Total pancreatectomy; NED: No evidence of disease; NA: Not available; DUC: Died of unrelated cause; AWD= Alive with disease.
Recurrence after apparently radical resection of a SPT can occur in 10%-15% of cases, and the liver is the most common site[2–4,16,29] (Table 3). Resection of liver metastases is possible if liver involvement is limited[16,23,32,34,36,37]. In our patient, the tumor recurred diffusely in the liver 32 mo after a R-0 resection. Unfortunately, radical excision of liver metastases was not possible, and the patient received chemotherapy with a substantially stable disease 77 mo after initial diagnosis and 45 mo after tumor relapse. The long term survival after appearance of liver metastases has been reported in some patients after surgical treatment[32,34,37], and even without radical treatment[17,39], because of the indolent nature of the disease. However, other patients died within 2 years from appearance of liver metastases[17,30,33,35–38]. Also the appearance of hepatic metastases varies greatly from patient to patient, from a minimum of 2[38] to a maximum of 168[35] mo. At present, there are no established clinical or histological criteria to predict the biological behavior of SPT. While invasion of blood vessels, perineural infiltration, invasion of adjacent structures, high degree of cellular polimorfism, and elevated mitotic rate are suggested to be associated with metastases and recurrence[3,11,14,20,27,33]. Absence of these features does not preclude malignant behavior[30,33,38]. Our patient showed only venous invasion and a moderate cellular atypia without mitotic activity. In a retrospective study on 33 patients (11 suggestive of malignant potential), Kang et al[36] failed to find features able to predict SPT malignant behavior in the clinical setting, although both patients with metastasis and recurrence belonged to a patient group with histopathology suggesting malignant potential. Thus, all patients require long-term follow-up.
Table 3.
Patients with recurrent disease after potentially curative resection
| Author | Yr | Extrapancreatic disease at diagnosis | Therapy | Site, time of recurrence (mo), therapy | Mo from 1st recurrence & follow-up |
| Levy et al[29] | 1997 | Peritoneal metastases | DP, Omentectomy, lymphadenectomy | Peritoneal carcinomatosis (8): complete resection. Liver (16) | 29, AWD |
| Shimizu et al[30] | 1999 | No | DP | Liver (17) | 3, DOP |
| Rebhandl et al[31] Martin et al[17] | 2001 2002 | No | SPDP | Peritoneum-omentum (24) radical resection. Spleen, peritoneum (36) tumor debulking; CT. Recurrence lesser omentum (>72) tumor resection, interferon. | > 54, NED |
| Liver | Resection | Liver, NA | 8, DOD | ||
| Liver | Resection | Liver, NA | 72, AWD | ||
| Gedaly et al[32] | 2002 | no | DCP | Liver (36), hepatectomy; liver (72), RF | 48, AWD |
| Tang et al[33] Takahashi et al[34] | 2005 2005 | No Liver (multiple nodules) | DCP DP, adrenalectomy & enucleation of 38 hepatic nodules | Liver, (3) | 13, DOD 46, AWD |
| Liver (14, 27, 38)/enucleation of 14, 21, 19 nodules; | |||||
| lung (41)/ lung resection | |||||
| Huang H-L et al[35] Kang et al[36] | 2005 2006 | No Peripancreatic nodes | SPDP DP | Liver (168) | 10, DOD 17, DOD |
| Liver, CT, TACE,( 9), | |||||
| Surgery + RF | |||||
| Tipton et al[27] Cao et al[37] | 2006 2006 | Incomplete resection | DP | Subcutaneous (14): removed; intra-abdominal recurrences removed (?) | 94, NED |
| no | UR | Liver, (57) | 3, DOD | ||
| no | UR | Liver, (72) | 0, AWD | ||
| no | UR | Liver (11), resection | 110, NED | ||
| Adamthwaite et al[38] | 2006 | nodes | DCP | Liver (2) | 0.5, DOD |
| Nagri et al[39] | 2007 | duodenum | Resection | Liver (48) | 48, AWD |
| Present patient | 2007 | No | Resection | Liver (32), CT | 45, AWD |
SPDP: Spleen preserving distal pancreatectomy; DP: Distal pancreatectomy; PD: Pancreaticoduodenectomy; UR: Unspecified resection; TACE: Transarterial chemoembolization; CT: Chemotherapy; RF: Radiofrequency; NA: Not available; DOD: Died of disease; DOP: Died of procedure (TAE); AWD: Alive with disease; NED: No evidence of disease.
In our patient, several different regimens were used. However, we do not know if the long term survival is due to the chemotherapy, or due to the natural course of a less aggressive tumor. The usefulness of chemotherapy for patients with SPT is substantially unknown, although some anecdotal studies have reported its benefit[11,31,40,41] or non benefit[10,17,36]. Two cases of resectable tumor underwent chemotherapy with cisplatin and 5-fluorouracil[40] or gemcitabine[41], but in the latter patient previous treatment with fluorouracil and 50.4 Gy failed to decrease the tumor size. Radiotherapy is seldom used for unresectable tumor[11] or as an adjuvant after tumor resection[8]. Two cases of radio sensitivity in unresectable tumors[9,26] are reported.
Transcatheter arterial embolization (TAE) or chemoembolization (TACE) are seldom used[10,30,36]. One patient was reported to have significant reduction metastases in the right lobe[10], one died after the procedure[30], one remained unchanged[36]. Radiofrequency is also seldom used[35,36].
In conclusion, malignant SPT is a low grade tumor with a good prognosis. Adequate surgical intervention is necessary for the long term survival of patients. Whenever possible, aggressive and reiterative surgery is justified for locally invasive or metastatic SPT. Regular follow-up is mandatory for all patients having undergone potentially curative resection. Particular attention should be paid to the patients with tumors larger than 5 cm in diameter and/or with histology suggesting a possible malignant behavior. The role of chemotherapy, radiotherapy, TAE, TACE, radiofrequency is still under scrutiny. Careful follow-up also for unresectable pancreatic cystic lesions may prevent tumor progression.
Peer reviewer: Dr. Massimo Raimondo, Division of Gastroenterology and Hepatology, Mayo Clinic, 4500 San Pablo Road, Jacksonville, FL 32224, United States
S- Editor Li DL L- Editor Wang XL E- Editor Ma WH
References
- 1.Frantz VK. Tumor of the pancreas. In Atlas of tumor pathology. Armed Forces Institute of Pathology. Washington DC. 1959. pp. 32–33. [Google Scholar]
- 2.Papavramidis T, Papavramidis S. Solid pseudopapillary tumors of the pancreas: review of 718 patients reported in English literature. J Am Coll Surg. 2005;200:965–972. doi: 10.1016/j.jamcollsurg.2005.02.011. [DOI] [PubMed] [Google Scholar]
- 3.Mao C, Guvendi M, Domenico DR, Kim K, Thomford NR, Howard JM. Papillary cystic and solid tumors of the pancreas: a pancreatic embryonic tumor? Studies of three cases and cumulative review of the world's literature. Surgery. 1995;118:821–828. doi: 10.1016/s0039-6060(05)80271-5. [DOI] [PubMed] [Google Scholar]
- 4.Madan AK, Weldon CB, Long WP, Johnson D, Raafat A. Solid and papillary epithelial neoplasm of the pancreas. J Surg Oncol. 2004;85:193–198. doi: 10.1002/jso.20019. [DOI] [PubMed] [Google Scholar]
- 5.Schwartz M. A biomathematical approach to clinical tumor growth. Cancer. 1961;14:1272–1294. doi: 10.1002/1097-0142(196111/12)14:6<1272::aid-cncr2820140618>3.0.co;2-h. [DOI] [PubMed] [Google Scholar]
- 6.Kato T, Egawa N, Kamisawa T, Tu Y, Sanaka M, Sakaki N, Okamoto A, Bando N, Funata N, Isoyama T. A case of solid pseudopapillary neoplasm of the pancreas and tumor doubling time. Pancreatology. 2002;2:495–498. doi: 10.1159/000064711. [DOI] [PubMed] [Google Scholar]
- 7.Sanfey H, Mendelsohn G, Cameron JL. Solid and papillary neoplasm of the pancreas. A potentially curable surgical lesion. Ann Surg. 1983;197:272–275. doi: 10.1097/00000658-198303000-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dales RL, Garcia JC, Davies RS. Papillary-cystic carcinoma of the pancreas. J Surg Oncol. 1983;22:115–117. doi: 10.1002/jso.2930220213. [DOI] [PubMed] [Google Scholar]
- 9.Fried P, Cooper J, Balthazar E, Fazzini E, Newall J. A role for radiotherapy in the treatment of solid and papillary neoplasms of the pancreas. Cancer. 1985;56:2783–2785. doi: 10.1002/1097-0142(19851215)56:12<2783::aid-cncr2820561211>3.0.co;2-q. [DOI] [PubMed] [Google Scholar]
- 10.Matsuda Y, Imai Y, Kawata S, Nishikawa M, Miyoshi S, Saito R, Minami Y, Tarui S. Papillary-cystic neoplasm of the pancreas with multiple hepatic metastases: a case report. Gastroenterol Jpn. 1987;22:379–384. doi: 10.1007/BF02774265. [DOI] [PubMed] [Google Scholar]
- 11.Matsunou H, Konishi F. Papillary-cystic neoplasm of the pancreas. A clinicopathologic study concerning the tumor aging and malignancy of nine cases. Cancer. 1990;65:283–291. doi: 10.1002/1097-0142(19900115)65:2<283::aid-cncr2820650217>3.0.co;2-x. [DOI] [PubMed] [Google Scholar]
- 12.Zinner MJ, Shurbaji MS, Cameron JL. Solid and papillary epithelial neoplasms of the pancreas. Surgery. 1990;108:475–480. [PubMed] [Google Scholar]
- 13.Tsunoda T, Eto T, Tsurifune T, Tokunaga S, Ishii T, Motojima K, Matsumoto T, Segawa T, Ura K, Fukui H. Solid and cystic tumor of the pancreas in an adult male. Acta Pathol Jpn. 1991;41:763–770. doi: 10.1111/j.1440-1827.1991.tb03349.x. [DOI] [PubMed] [Google Scholar]
- 14.Nishihara K, Nagoshi M, Tsuneyoshi M, Yamaguchi K, Hayashi I. Papillary cystic tumors of the pancreas. Assessment of their malignant potential. Cancer. 1993;71:82–92. doi: 10.1002/1097-0142(19930101)71:1<82::aid-cncr2820710114>3.0.co;2-y. [DOI] [PubMed] [Google Scholar]
- 15.Jeng LB, Chen MF, Tang RP. Solid and papillary neoplasm of the pancreas. Emphasis on surgical treatment. Arch Surg. 1993;128:433–436. doi: 10.1001/archsurg.1993.01420160071011. [DOI] [PubMed] [Google Scholar]
- 16.Saiura A, Umekita N, Matsui Y, Maeshiro T, Miyamoto S, Kitamura M, Wakikawa A. Successful surgical resection of solid cystic tumor of the pancreas with multiple liver metastases and a tumor thrombus in the portal vein. Hepatogastroenterology. 2000;47:887–889. [PubMed] [Google Scholar]
- 17.Martin RC, Klimstra DS, Brennan MF, Conlon KC. Solid-pseudopapillary tumor of the pancreas: a surgical enigma? Ann Surg Oncol. 2002;9:35–40. doi: 10.1245/aso.2002.9.1.35. [DOI] [PubMed] [Google Scholar]
- 18.Ng KH, Tan PH, Thng CH, Ooi LL. Solid pseudopapillary tumour of the pancreas. ANZ J Surg. 2003;73:410–415. doi: 10.1046/j.1445-2197.2003.t01-1-02634.x. [DOI] [PubMed] [Google Scholar]
- 19.Goh BK, Tan YM, Cheow PC, Chung AY, Chow PK, Wong WK, Ooi LL. Solid pseudopapillary neoplasms of the pancreas: an updated experience. J Surg Oncol. 2007;95:640–644. doi: 10.1002/jso.20735. [DOI] [PubMed] [Google Scholar]
- 20.Podevin J, Triau S, Miralliè E, Le Borgne J. Solid-pseudopapillary tumor of the pancreas: a clinical study of five cases, and review of the literature. Ann Chir. 2003;128:543–548. doi: 10.1016/s0003-3944(03)00214-1. [DOI] [PubMed] [Google Scholar]
- 21.Usatoff V, Wittkop B, Devalia K, Guest P, Buckels J. Solid papillary-cystic carcinoma of the pancreas with portal vein tumour thrombus. ANZ J Surg. 2004;74:291–293. doi: 10.1111/j.1445-2197.2004.02592.x. [DOI] [PubMed] [Google Scholar]
- 22.Hassan I, Celik I, Nies C, Zielke A, Gerdes B, Moll R, Ramaswamy A, Wagner HJ, Bartsch DK. Successful treatment of solid-pseudopapillary tumor of the pancreas with multiple liver metastases. Pancreatology. 2005;5:289–294. doi: 10.1159/000085285. [DOI] [PubMed] [Google Scholar]
- 23.Chen X, Zhou GW, Zhou HJ, Peng CH, Li HW. Diagnosis and treatment of solid-pseudopapillary tumors of the pancreas. Hepatobiliary Pancreat Dis Int. 2005;4:456–459. [PubMed] [Google Scholar]
- 24.Frago R, Fabregat J, Jorba R, Garcia-Borobia F, Altet J, Serrano MT, Valls C. Solid pseudopapillary tumors of the pancreas: diagnosis and curative treatment. Rev Esp Enferm Dig. 2006;98:809–816. doi: 10.4321/s1130-01082006001100002. [DOI] [PubMed] [Google Scholar]
- 25.Hao CY, Lu AP, Xing BC, Huang XF, Gao F, Ji JF. Solid pseudopapillary tumor of the pancreas: report of 8 cases in a single institution and review of the Chinese literature. Pancreatology. 2006;6:291–296. doi: 10.1159/000092691. [DOI] [PubMed] [Google Scholar]
- 26.Zauls JA, Dragun AE, Sharma AK. Intensity-modulated radiation therapy for unresectable solid pseudopapillary tumor of the pancreas. Am J Clin Oncol. 2006;29:639–640. doi: 10.1097/01.coc.0000190457.43060.fd. [DOI] [PubMed] [Google Scholar]
- 27.Tipton SG, Smyrk TC, Sarr MG, Thompson GB. Malignant potential of solid pseudopapillary neoplasm of the pancreas. Br J Surg. 2006;93:733–737. doi: 10.1002/bjs.5334. [DOI] [PubMed] [Google Scholar]
- 28.Peng CH, Chen DF, Zhou GW, Yang WP, Tao ZY, Lei RQ, Zhange SD, Li HW. The solid-pseudopapillary tumor of pancreas: the clinical characteristics and surgical treatment. J Surg Res. 2006;131:276–282. doi: 10.1016/j.jss.2005.11.585. [DOI] [PubMed] [Google Scholar]
- 29.Tang LH, Aydin H, Brennan MF, Klimstra DS. Clinically aggressive solid pseudopapillary tumors of the pancreas: a report of two cases with components of undifferentiated carcinoma and a comparative clinicopathologic analysis of 34 conventional cases. Am J Surg Pathol. 2005;29:512–519. doi: 10.1097/01.pas.0000155159.28530.88. [DOI] [PubMed] [Google Scholar]
- 30.Levy P, Bougaran J, Gayet B. Diffuse peritoneal carcinosis of pseudo-papillary and solid tumor of the pancreas. Role of abdominal injury. Gastroenterol Clin Biol. 1997;21:789–793. [PubMed] [Google Scholar]
- 31.Shimizu M, Matsumoto T, Hirokawa M, Monobe Y, Iwamoto S, Tsunoda T, Manabe T. Solid-pseudopapillary carcinoma of the pancreas. Pathol Int. 1999;49:231–234. doi: 10.1046/j.1440-1827.1999.00852.x. [DOI] [PubMed] [Google Scholar]
- 32.Rebhandl W, Felberbauer FX, Puig S, Paya K, Hochschorner S, Barlan M, Horcher E. Solid-pseudopapillary tumor of the pancreas (Frantz tumor) in children: report of four cases and review of the literature. J Surg Oncol. 2001;76:289–296. doi: 10.1002/jso.1048. [DOI] [PubMed] [Google Scholar]
- 33.Gedaly R, Toledano A, Millan G, Essenfeld H, Zambrano VJ. Treatment of liver metastases from a solid pseudopapillary tumor of the pancreas. J Hepatobiliary Pancreat Surg. 2006;13:587–590. doi: 10.1007/s00534-006-1122-4. [DOI] [PubMed] [Google Scholar]
- 34.Takahashi Y, Fukusato T, Aita K, Toida S, Fukushima J, Imamura T, Tanaka F, Amano H, Takada T, Mori S. Solid pseudopapillary tumor of the pancreas with metastases to the lung and liver. Pathol Int. 2005;55:792–796. doi: 10.1111/j.1440-1827.2005.01908.x. [DOI] [PubMed] [Google Scholar]
- 35.Huang HL, Shih SC, Chang WH, Wang TE, Chen MJ, Chan YJ. Solid-pseudopapillary tumor of the pancreas: clinical experience and literature review. World J Gastroenterol. 2005;11:1403–1409. doi: 10.3748/wjg.v11.i9.1403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kang CM, Kim KS, Choi JS, Kim H, Lee WJ, Kim BR. Solid pseudopapillary tumor of the pancreas suggesting malignant potential. Pancreas. 2006;32:276–280. doi: 10.1097/01.mpa.0000202956.41106.8a. [DOI] [PubMed] [Google Scholar]
- 37.Cao D, Antonescu C, Wong G, Winter J, Maitra A, Adsay NV, Klimstra DS, Hruban RH. Positive immunohistochemical staining of KIT in solid-pseudopapillary neoplasms of the pancreas is not associated with KIT/PDGFRA mutations. Mod Pathol. 2006;19:1157–1163. doi: 10.1038/modpathol.3800647. [DOI] [PubMed] [Google Scholar]
- 38.Adamthwaite JA, Verbeke CS, Stringer MD, Guillou PJ, Menon KV. Solid pseudopapillary tumour of the pancreas: diverse presentation, outcome and histology. JOP. 2006;7:635–642. [PubMed] [Google Scholar]
- 39.Nagri S, Abdu A, Anand S, Krishnaiah M, Arya V. Liver metastasis four years after Whipple's resection for solid-pseudopapillary tumor of the pancreas. JOP. 2007;8:223–227. [PubMed] [Google Scholar]
- 40.Strauss JF, Hirsch VJ, Rubey CN, Pollock M. Resection of a solid and papillary epithelial neoplasm of the pancreas following treatment with cis-platinum and 5-fluorouracil: a case report. Med Pediatr Oncol. 1993;21:365–367. doi: 10.1002/mpo.2950210511. [DOI] [PubMed] [Google Scholar]
- 41.Maffuz A, Bustamante Fde T, Silva JA, Torres-Vargas S. Preoperative gemcitabine for unresectable, solid pseudopapillary tumour of the pancreas. Lancet Oncol. 2005;6:185–186. doi: 10.1016/S1470-2045(05)01770-5. [DOI] [PubMed] [Google Scholar]


