Abstract
Nonnucleoside reverse transcriptase inhibitors (NNRTIs) are the mainstays of therapy for the treatment of human immunodeficiency virus type 1 (HIV-1) infections. However, the effectiveness of NNRTIs can be hampered by the development of resistance mutations which confer cross-resistance to drugs in the same class. Extensive efforts have been made to identify new NNRTIs that can suppress the replication of the prevalent NNRTI-resistant viruses. MK-4965 is a novel NNRTI that possesses both diaryl ether and indazole moieties. The compound displays potency at subnanomolar concentrations against wild-type (WT), K103N, and Y181C reverse transcriptase (RT) in biochemical assays. MK-4965 is also highly potent against the WT virus and two most prevalent NNRTI-resistant viruses (viruses that harbor the K103N or the Y181C mutation), against which it had 95% effective concentrations (EC95s) of <30 nM in the presence of 10% fetal bovine serum. The antiviral EC95 of MK-4965 was reduced approximately four- to sixfold when it was tested in 50% human serum. Moreover, MK-4965 was evaluated with a panel of 15 viruses with NNRTI resistance-associated mutations and showed a superior mutant profile to that of efavirenz but not to that of etravirine. MK-4965 was similarly effective against various HIV-1 subtypes and viruses containing nucleoside reverse transcriptase inhibitor or protease inhibitor resistance-conferring mutations. A two-drug combination study showed that the antiviral activity of MK-4965 was nonantagonistic with each of the 18 FDA-licensed drugs tested vice versa in the present study. Taken together, these in vitro data show that MK-4965 possesses the desired properties for further development as a new NNRTI for the treatment of HIV-1 infection.
Human immunodeficiency virus type 1 (HIV-1) reverse transcriptase (RT) converts single-stranded viral RNA into a double-stranded proviral DNA via polymerase and RNase H activities, and this is an obligate step in the HIV-1 replication cycle (15). Given the pivotal role that RT plays in the life cycle of HIV-1, the inhibition of RT has been one of the primary therapeutic strategies in suppressing the replication of HIV-1 (7, 24). Currently, two classes of RT inhibitors are available for the treatment of HIV-1 infection: nucleoside RT inhibitors (NRTIs; such as zidovudine [AZT] and lamivudine [3TC]) bind directly to the active site of RT polymerase and terminate DNA synthesis after incorporation into the newly synthesized DNA, while nonnucleoside RT inhibitors (NNRTIs; such as the first-generation NNRTIs efavirenz [EFV] and nevirapine [NVP]) bind to an allosteric site on RT.
NNRTIs are noncompetitive inhibitors of HIV-1 RT that bind to a hydrophobic pocket in the p66 subunit of the p66/p51 heterodimer near the polymerase active site (17). NNRTI binding causes conformational changes within p66 that reposition the active-site residues to an inactive conformation, thereby inhibiting the chemical step of polymerization (1). Mutations of residues around the NNRTI binding pocket can interfere with NNRTI binding, thus conferring resistance to this class of compounds. Although NNRTIs are key components of effective combination regimens, like all antiretroviral agents, their effectiveness can be hampered by the emergence of clinical drug resistance. Moreover, single mutations can lead to significant reductions in susceptibility, often to all available inhibitors within the class (3, 12). For instance, the increasingly common K103N mutation (which is present in 40 to 60% of NNRTI-resistant viruses) displays significant resistance to the first-generation NNRTIs, and the Y181C mutation (which is present in 15 to 25% of NNRTI-resistant viruses) confers a high degree of resistance to both NVP and delavirdine (DLV) and a moderate degree of resistance to the recently approved second-generation NNRTI etravirine (ETV).
Since NNRTIs have great therapeutic potential, extensive efforts have been made to identify novel NNRTIs that are highly active against the prevalent NNRTI-resistant viruses, that are suitable for once-daily dosing, and that have excellent safety profiles. In addition to the recently approved drug ETV, several other promising NNRTIs are in development (32).
MK-4965 is a novel NNRTI containing diaryl ether and indazole moieties (Fig. 1) (34). We report here that MK-4965 displays excellent activities against not only wild-type (WT) virus but also against a broad panel of NNRTI-resistant viruses, including viruses containing the K103N and/or the Y181C mutation. In addition, MK-4965 is highly potent against viral isolates representing different HIV-1 subtypes as well as against viruses that are resistant to protease inhibitors (PIs) or NRTIs, or both. Two-drug combination studies with MK-4965 and each of the FDA-licensed drugs tested in this study were conducted in cell culture. The results showed that MK-4965 did not display any antagonistic effect on the antiviral activities of the other antiviral agents tested.
FIG. 1.
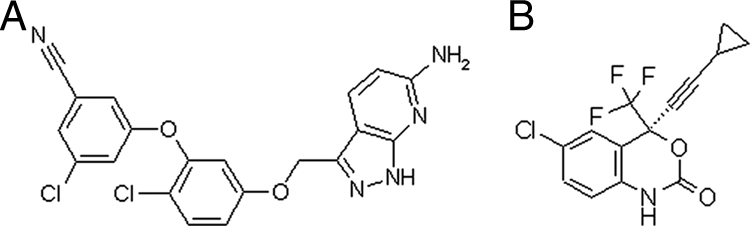
Structures of MK-4965 (A) and EFV (B).
MATERIALS AND METHODS
The full-length WT RT protein and two RT proteins with mutations (K103N and Y181C) were expressed in Escherichia coli BL21(DE3) cells and were purified as described previously (28). The t500 RNA template was made by IBA BioTAGnology (German), and the biotinylated DNA primer was made by Integrated DNA Technology (Coralville, IA). The R8 virus was a kind gift from Christopher Aiken (Vanderbilt University, Nashville, TN). SupT1 cells were provided by the NIH AIDS Research and Reference Reagent Program. Ruthenylated dUTP was custom-made by Midland Certified Reagents Company (Midland, TX).
Electrochemiluminescence (ECL) detector M-384 and streptavidin-coated magnetic beads were purchased from BioVeris (Gaithersburg, MD). Culture medium (RPMI 1640) and Dulbecco modified Eagle medium (DMEM) with 10% fetal bovine serum (FBS) were from Gibco (Carlsbad, CA). An enzyme-linked immunosorbent assay kit (AlphaLISA) for p24 detection was supplied by Perkin-Elmer (Waltham, MA). Alamar blue reagents for cytotoxicity testing were obtained from BioSource International, Inc. (Camarillo, CA). EDTA (Versene) was ordered from BioWhittaker (Walkersville, MD). Wallac Microbeta and Victor luminometers were from Perkin-Elmer (Wellesley, MA). A 384-well microplate was purchased from Falcon (Franklin Lake, NJ). The integrase strand transfer inhibitor raltegravir (RAL) and the NNRTI ETV were synthesized in-house.
The following antiviral agents and cells employed for the combination study were provided by Southern Research Institute (SRI, Birmingham, AL): the NRTIs 3TC, abacavir (ABC), AZT, stavudine (d4T), zalcitabine (ddC), didanosine (ddI), emtricitabine (FTC), tenofovir (TDF; 9-[2-(phosphonomethoxy)propyl]adenine), tenofovir DF, and ribavirin (RBV; an anti-hepatitis C virus drug); the NNRTIs DLV, EFV, and NVP; the PIs darunavir (DRV) and indinavir (IDV); the entry inhibitors maraviroc (MVC), enfuvirtide (ENF; T20); CEM-SS cells; MAGI-CCR5 cells; CXCR4-tropic HIV-1 strain IIIB; and CCR5-tropic HIV-1 strain Ba-L.
HIV-1 RT biochemical assay.
The ECL RT biochemical assay was performed on the basis of a previously described protocol (25). Briefly, HIV-1 RT enzyme (10 pM) was combined with an inhibitor or dimethyl sulfoxide (10%) in assay buffer (50 mM Tris-HCl, pH 7.8), and then the mixture was incubated at room temperature for 30 min. The polymerization reaction was initiated by the addition of a biotinylated template-primer substrate (5 nM) and deoxynucleoside triphosphates (0.6 μM of dATP, dGTP, and dCTP; 20 nM ruthenylated dUTP). The reactions were continued for 90 min at 37°C, followed by addition of 10 μl of 1 N NaOH to terminate the reaction. The resulting solution was incubated at room temperature for an additional 30 min and was then neutralized with 10 μl of 1 N HCl. Streptavidin-coated magnetic beads (80 μg/ml) were added to capture the product and the unreacted substrate. Quantification of the product was determined on the basis of the ECL signal measured with the ECL M-384 instrument.
HIV multiple-cycle replication assay.
MK-4965 was tested in cell culture multiple-cycle replication assays with genetically defined WT HIV-1 and three laboratory viruses with mutations (K103N, Y181C, and both K103N and Y181C). Antiviral activity assays were performed with a cell culture medium supplemented with 10% FBS or 50% human serum (HS). MK-4965 was diluted into an appropriate culture medium for each assay and was tested at concentrations ranging from 833 nM to 0.32 nM.
Antiviral assays were performed with variants of a laboratory HIV-1 isolate, R8, and MT-4 human T-lymphoid cells. Cells (2.5 × 105 cells/well) were infected with viral stocks at a low multiplicity of infection in the absence of inhibitor and were incubated at 37°C in a 5% CO2 atmosphere. Twenty-four hours later, the infected cells were washed, resuspended in fresh culture medium (RPMI 1640 with 10% FBS or RPMI 1640 with 50% type AB HS), and seeded into a 96-well cell culture plate at 5 × 104 cells per 125 μl. MK-4965 was added to the wells in serial threefold dilutions. The NNRTIs EFV, NVP, and ETV were used as comparators in the assay. The cells were incubated for an additional 72 h, and virus production in the individual culture wells was assessed by measuring the level of production of viral core p24 antigen in the culture medium with an Alphascreen kit from Perkin-Elmer. The 95% effective concentration (EC95) for virus inhibition was defined as the lowest concentration of test compound that inhibited virus p24 antigen production by at least 95% relative to the level of production by the untreated control cultures.
The cytotoxicities of MK-4965 and the comparator drugs at the concentrations tested (see above) were assessed by using Alamar blue, as recommended by the manufacturer (BioSource International), after incubation at 37°C in 5% CO2 for 24, 48, or 72 h. MK-4965 did not show any cytotoxicity even at concentrations much higher than its EC95 (EC50 for cytotoxicity, 2.8 μM).
HIV-1 single-cycle replication assay with viruses containing RT sequences from patient isolates.
Monogram Biosciences performed a single-cycle replication PhenoScreen assay with MK-4965 and EFV against a broader array of clinical NNRTI-resistant HIV-1 isolates using a variation of its clinical diagnostic assays. In addition, nine HIV-1 sybtypes and circulating recombinant forms (CRFs) were also evaluated for their susceptibilities to NNRTIs. Clade B viruses containing PI or NRTI resistance-conferring mutations were tested to determine whether the mutations confer any resistance to NNRTIs. RT inhibitor activity was evaluated with nine serial drug concentrations (26).
Combination study. (i) General information.
The combination study was conducted by SRI in a two-drug combination fashion with MK-4965 and each of the 18 FDA-approved antiviral agents described above, including RAL and ETV. RBV and d4T were used as the positive antagonism controls because the antiviral activity of d4T is antagonized by RBV.
The cells were quantified with a hemacytometer, and cell viability was determined by trypan blue exclusion. Cell viability was greater than 95% under the conditions utilized in the assay. For the study of each combination, MK-4965 was prepared by starting with 100 nM and then obtaining seven additional serial half-log dilutions. Each dilution of MK-4965 was tested in combination with five dilutions of a second anti-HIV drug starting from 10 times the EC50, followed by testing with four additional half-log dilutions. The dimethyl sulfoxide concentration was <0.25%, which has previously been shown to have no effect in the assays described.
Each combination study was carried out with CEM-SS cells or MAGI-CCR5 cells acutely infected with HIV-1IIIB and HIV-1Ba-L, respectively. Viral growth and inhibition were evaluated by measuring the virus-induced cytopathic effects in CEM-SS cells or the level of β-galactosidase reporter gene induction in MAGI-CCR5 cells at the experimental end point. The cytotoxicity of each two-drug combination was also evaluated in parallel with the evaluations of the antiviral activity. The combination of d4T and RBV was tested in parallel in each of the assays and was used as a positive antagonism control.
The preparation of HIV-1IIIB was accomplished by resuspending and diluting the viruses in tissue culture medium such that the amount of virus added to each well in a volume of 50 μl was the amount determined to give between 85 and 95% cell killing at 6 days postinfection. HIV-1Ba-L was grown in ghost Hi5/MAGI-CCR5 cell cocultures for the production of stock virus. The virus was suspended and diluted in complete DMEM such that the amount of virus added to each well in a volume of 50 μl was 10 times the 50% tissue culture infective dose (TCID50)/well (0.001 TCID50/cell). For each combination, the antiviral activity experiment was conducted in triplicate and the toxicity experiment was performed in duplicate.
All studies with drug combinations except the combination of MK-4965 and MVC were conducted with CEM-SS cells; study of the combination of MK-4965 and MVC was carried out with HIV-1Ba-L-infected MAGI-CCR5 cells. MAGI-CCR5 cells are derived from HeLa CD4 LTR β-gal cells. The cells were engineered to express high levels of CD4 and CCR5 and contain one copy of the HIV-1 long terminal repeat (LTR) promoter, which drives the expression of the β-galactosidase gene upon HIV-1 Tat transactivation.
(ii) Antiviral efficacy evaluation. (a) Anti-HIV-1 cytoprotection assay with CEM-SS cells.
Solutions of MK-4965 and the second anti-HIV agent to be tested were made at concentrations of 10×. The resulting compounds (20 μl each) were added to the plates in a matrix fashion (8 by 5 wells), followed by the introduction of CEM-SS cells (110 μl) at a density of 2.5 × 103 cells/well in complete RPMI 1640 medium. By using a predetermined titer, a HIV-1IIIB solution in complete RPMI 1640 medium (50 μl) was added to infect the cells at a multiplicity of infection of 0.01. For the plates used for the toxicity assay, each of the two drugs (20 μl at 10× concentrations), cells (110 μl), and medium (50 μl) were added to all wells. Extra medium was added to the cell and the virus control wells, which did not contain any compound. The resulting plates were incubated at 37°C in 5% CO2 for 6 days, followed by addition of 3-(4,5-dimethylthiazol-2-yl)-5-(3-carboxymethoxyphenyl)-2-(4-sulfophenyl)-2H-tetrazolium, inner salt (MTS; 25 μl), to all wells (20). The plates were covered with adhesive plate sealers and were inverted to disrupt the cell pellet. The plates were incubated for 4 to 6 h, and the absorbance at 490 and 650 nm were measured to determine the level of metabolism from MTS. The data were translated into the MacSynergy program to calculate the additivity, synergy, or antagonism that resulted from the combination of the two drugs.
(b) Antiviral assay with MAGI-CCR5 cells.
The antiviral assay procedure with MAGI-CCR5 cells was similar to that described above, except that the MAGI-CCR5 cells were prepared in the presence of 100 μl of complete DMEM at a density of 1.0 × 104 cells/well and were incubated at 37°C overnight. On the day of assay setup, the medium was removed from all wells. The plates for the cytotoxicity assay were incubated at 37°C in 5% CO2 for 2 days and were incubated for 1.5 h after addition of MTS. For all plates used for the assay of efficacy, the supernatant was removed, followed by addition of 50 μl per well of PBS and 50 μl per well of Gal-Screen reaction mixture at a 1:25 ratio of substrate to buffer. After incubation at room temperature for 1.5 h, the end-point chemiluminescence was determined with a Wallac Microbeta machine.
(iii) Data analysis.
The drug combination assay data were analyzed by the method of Prichard and Shipman (27) with the MacSynergy II program for data analysis and evaluation of statistical significance. Briefly, the MacSynergy II program calculates the theoretical interactions of the drugs on the basis of the Bliss independence mathematical definition of the expected effects of drug-drug interactions. The Bliss independence model is based on statistical probability and assumes that the drugs act independently to affect virus replication; this independent-effects model is also referred to as a dual-site model and was used for all analyses of drug combinations reported here. The theoretical additive surface interactions were calculated from the dose-response curves for each drug used individually. This calculated additive surface, which represents predicted additive interactions, was then subtracted from the experimentally determined dose-response surface to reveal regions of nonadditive activity. The resulting surface would appear as a horizontal plane at 0% inhibition if the interactions were merely additive. Any peak above this plane of additivity would be indicative of synergy. Similarly, any depression below the plane of additivity would indicate antagonism. The 95% confidence intervals around the experimental dose-response surface were used to evaluate the data statistically, and the volumes of the peaks and depressions were calculated and used to quantify the volume of synergy and volume of antagonism produced. The volumes of the peaks observed in the synergy plots (in units of concentration times concentration times percent; e.g., μM2%, nM2%, and nMμM%) was calculated by the program. This peak volume is the three-dimensional counterpart of the area under a three-dimensional dose-response surface and is a quantitative measure of synergy or antagonism. For these studies, synergy was defined as drug combinations that yielded synergy volumes greater than 50. Slightly synergistic activity and highly synergistic activity were operationally defined as yielding synergy volumes of 50 to 100 and >100, respectively. Additive drug interactions have synergy volumes in the range of −50 to 50, while synergy volumes between −50 and −100 are considered slightly antagonistic and those <−100 are highly antagonistic.
RESULTS
To identify compounds that are able to inhibit the prevalent NNRTI-resistant RTs, all compounds produced in the NNRTI medicinal chemistry program were screened for their activities against recombinant WT RT and RTs with the K103N and Y181C mutations (WT, K103N, and Y181C RTs, respectively). As shown in Table 1, MK-4965 displayed potency for the inhibition of RNA-dependent DNA polymerase activity at subnanomolar concentrations. The 50% inhibitory concentrations (IC50s) were 0.23 nM, 0.40 nM, and 0.39 nM for the WT, K103N, and Y181C RTs, respectively. These results indicate that RT containing the K103N or the Y181C mutation is still highly susceptible to MK-4965 and that the shift in potency against the K103N and Y181C RTs is less than twofold compared with that against the WT RT. ETV showed two- and threefold shifts in potency against the K103N and the Y181C RTs, respectively, compared with the potency against the WT RT. Consistent with the findings described in the literature, EFV displayed more than a 20-fold shift in potency against the RT containing K103N compared with the potency against the WT RT, whereas no shift in potency against RT containing the Y181C mutation was observed (11). Both the K103N and the Y181C RTs were highly resistant to NVP (IC50s, >8.5 μM).
TABLE 1.
Inhibitory potencies of MK-4965, NVP, EFV, and ETV against WT, K103N, and Y181C RTs
| Compound | IC50 (nM)a
|
||
|---|---|---|---|
| WT | K103N | Y181C | |
| MK-4965 | 0.23 ± 0.09 (136) | 0.40 ± 0.15 (148) | 0.39 ± 0.16 (143) |
| EFV | 0.42 ± 0.06 (5) | 10.2 ± 6.6 (4) | 0.31 ± 0.17 (5) |
| NVP | 137 ± 5.8 (3) | 9300 ± 500 (3) | 8900 ± 1800 (3) |
| ETV | 0.60 ± 0.12 (4) | 1.3 ± 0.17 (4) | 1.96 ± 0.9 (3) |
IC50s are means ± standard deviations. Numbers in parentheses indicate the number of assays performed.
The antiviral activity of MK-4965 was evaluated in a multiple-cycle replication assay in the presence of 10% FBS and 50% HS. As shown in Table 2, in the presence of 10% FBS, the EC95 of MK-4965 was 4.4 nM against WT virus. Moreover, the compound retained excellent activities against viruses with the K103N and Y181C mutations (EC95s, 13 and 30 nM, respectively). Under the same conditions, MK-4965 inhibited replication of the mutant virus containing both the K103N and the Y181C mutations and had an EC95 of 128 nM. Consistent with biochemical data, viruses containing the K103N mutation, the Y181C mutation, and both the K103N and the Y181C mutations conferred significant resistance to NVP. Not surprisingly, viruses harboring the K103N mutation or the K103N and the Y181C mutations were highly resistant to EFV, and viruses harboring the Y181C mutation were sensitive to EFV. MK-4965 displayed activities comparable to those of ETV when it was tested with WT and Y181C viruses. With respect to viruses harboring the K103N mutation and both the K103N and the Y181C mutations, ETV exhibited approximately twofold better potency than MK-4965 in the presence of 10% FBS.
TABLE 2.
Antiviral activities of MK-4965, EFV, NVP, and ETV against WT virus and viruses with K103N, Y181C, and K103N-Y181C mutations in the presence of 10% FBS and 50% NHS
| Additive and compound | EC95 (nM)a
|
|||
|---|---|---|---|---|
| WT | K103N | Y181C | K103N-Y181C | |
| 10% FBS | ||||
| MK-4965 | 4.4 ± 2.0 (80) | 13 ± 6 (80) | 30 ± 8.3 (24) | 128 ± 47 (20) |
| EFV | 3.8 ± 1.4 (69) | 245 ± 90 (55) | 8.4 ± 2.6 (17) | 322 ± 83 (15) |
| NVP | 438 ± 106 (4) | >8,000 | >8,000 | >8,000 |
| ETV | 4.0 ± 1.1 (10) | 6.0 ± 2.8 (8) | 26 ± 12 (8) | 56 ± 15 (8) |
| 50% HS | ||||
| MK-4965 | 29 ± 12 (78) | 58 ± 24 (24) | 184 ± 60 (21) | 447 ± 26 (7) |
| EFV | 38 ± 12 (70) | 1734 ± 322 (7) | 89 ± 19 (13) | 3394 ± 593 (8) |
| NVP | 464 ± 91 (4) | >8,000 | >8,000 | >8,000 |
| ETV | 38 ± 14 (8) | 43 ± 15 (10) | 266 ± 42 (9) | 542 ± 82 (7) |
EC95s are means ± standard deviations. Numbers in parentheses indicate the number of assays performed.
To reflect the actual inhibitory potencies of NNRTIs under physiological conditions which have high protein contents, the antiviral activities of the compounds were also evaluated in the presence of 50% HS. Under these conditions, the antiviral activities of the compounds were generally reduced due to a greater extent of serum protein binding. As shown in Table 2, MK-4965 exhibited approximately four- to sixfold shifts in potency against the WT and mutant viruses as the type of serum used was changed from 10% FBS to 50% HS. In comparison, the antiviral potency of ETV was reduced approximately 7- to 10-fold when it was tested in the presence of 50% HS. As a result, MK-4965 displayed antiviral potency similar to that of ETV when it was tested against the WT and the three mutant viruses in the presence of 50% HS. EFV also displayed ∼7- to 10-fold shifts in potency under the same conditions, while the potency of NVP was unaffected by the inclusion of 50% HS.
In the presence of 50% HS, EFV showed an EC95 of >1.5 μM for suppression of the replication of mutant viruses harboring the K103N or both the K103N and the Y181C mutations and had potency similar to that of MK-4965 when it was tested against WT and Y181C viruses. Moreover, in comparison to the potency against WT virus, MK-4965 displayed 2-, 6-, and 15-fold shifts in EC95s against the K103N, Y181C, and K103N-Y181C viruses, respectively. This profile of activity against mutants was similar to that of ETV, which displayed 1.1-, 7-, and 14-fold shifts in EC95s against the three mutant viruses, respectively.
A broader panel of NNRTI-resistant viruses was employed to further evaluate the profiles of activity of MK-4965 and EFV against mutants in a single-cycle replication assay. The magnitudes of resistance of K103N or Y181C viruses to MK-4965 or EFV in the single-cycle replication assay were consistent with the magnitudes determined by the multiple-cycle virus replication assay described above. Among 15 resistant mutant viruses tested, MK-4965 displayed a more than a 100-fold shift in potency against only 2 mutant viruses (a virus with a Y188L mutation and a virus with V106A, G190A, and F227L mutations) (Fig. 2). On the other hand, EFV showed a more than 100-fold shift in potency against eight mutant viruses. For instance, the K103N and G190A double mutation gave the virus a greater than 300-fold higher level of resistance to EFV and only a 5-fold resistance to MK-4965. Furthermore, the other mutant viruses tested also exhibited higher levels of resistance to EFV than to MK-4965. One example was a virus that contained an L100I mutation, which had a 23-fold higher level of resistance to EFV but which was very susceptible to MK-4965 with a change in the level of resistance of 0.9-fold.
FIG. 2.
Profiles of MK-4965 (A) and EFV (B) against mutants. *, the EC50 was not reached at the concentration tested. CNDO is a drug-sensitive standard reference strain that is used to determine the changes in susceptibility of patient isolates. MDRC4 is a multidrug-resistant virus control strain that is used to evaluate and monitor assay performance.
The presence of the error-prone HIV-1 RT enzyme coupled with the absence of an exonuclease with proofreading activity results in a high degree of genetic diversity among viral subtypes in different geographical regions. In addition, recombination between subtypes further contributes to genetic diversification (6). Currently, the prevalence of nine distinct viral subtypes (subtypes A, B, C, D, F, G, H, J, and K) is expanding across the globe (16). Viruses of some subtypes and/or from certain geographical regions might therefore display differential susceptibilities to new NNRTIs. To test this possibility, the antiviral activity of MK-4965 against multiple viral isolates derived from each of 10 different subtypes or CRFs was evaluated. In addition, subtype B viruses harboring mutations associated with NRTI resistance (four isolates), PI resistance (six isolates), or resistance to both classes of compounds (seven isolates) were also examined for their susceptibilities to MK-4965. A drug-sensitive reference strain (strain CNDO) with protease and RT sequences derived from laboratory HIV strain NL4-3 was employed as a control. 3TC and TDF were used as controls for NRTI-resistant viruses.
As shown in Table 3, in comparison to the drug-sensitive strain, all WT isolates exhibited similar susceptibilities to NNRTIs, which had less than twofold shifts in potency. For viruses containing PI resistance-associated mutations, the potencies of MK-4965, NVP, and EFV were not compromised by the mutations, as shown in Table 4. Interestingly, viruses harboring NRTI resistance-associated mutations showed hypersusceptibility to the NNRTIs, with changes in potency ranging from 0.38- to 0.18-fold relative to the potency control viruses (Table 4). Viruses harboring NRTI resistance-associated mutations conferred high-level resistance to 3TC and moderate levels of resistance (approximately twofold) to TDF.
TABLE 3.
Change in inhibitory potencies of NNRTIs and NRTIs against different HIV-1 clades
| Clade | Fold change in potency compared with that against adrug-sensitive straina
|
||||
|---|---|---|---|---|---|
| 3TC | TDF | EFV | NVP | MK-4965 | |
| Clade A (n = 4) | 0.92 ± 0.2 | 0.95 ± 0.075 | 0.73 ± 0.35 | 0.94 ± 0.71 | 0.73 ± 0.31 |
| CRF01_AE (n = 3) | 1.13 ± 0.13 | 0.78 ± 0.049 | 0.83 ± 0.10 | 0.67 ± 0.13 | 0.90 ± 0.11 |
| CRF02_AG (n = 5) | 1.31 ± 0.32 | 0.93 ± 0.15 | 0.71 ± 0.13 | 0.40 ± 0.09 | 0.92 ± 0.25 |
| Clade B (n = 5) | 1.06 ± 0.16 | 0.94 ± 0.09 | 1.16 ± 0.63 | 1.25 ± 1.04 | 1.25 ± 0.45 |
| CRF17_BF (n = 2) | 1.37 ± 0.1 | 0.83 ± 0.12 | 0.86 ± 0.09 | 0.83 ± 0.51 | 1.15 ± 0.41 |
| Clade C (n = 5) | 1.07 ± 0.2 | 0.97 ± 0.19 | 0.88 ± 0.44 | 0.70 ± 0.47 | 1.07 ± 0.56 |
| Clade D (n = 3) | 0.80 ± 0.04 | 0.74 ± 0.09 | 0.51 ± 0.01 | 0.35 ± 0.04 | 0.56 ± 0.01 |
| Clade F1 (n = 2) | 0.87 ± 0.16 | 0.96 ± 0.09 | 0.81 ± 0.43 | 0.73 ± 0.65 | 0.72 ± 0.25 |
| Clade G (n = 2) | 0.70 ± 0.06 | 0.96 ± 0.06 | 0.77 ± 0.23 | 1.25 ± 0.67 | 0.58 ± 0.13 |
| Clade H (n = 2) | 0.83 ± 0.26 | 0.67 ± 0.03 | 0.20 ± 0.02 | 0.13 ± 0.01 | 0.22 ± 0.01 |
The drug-sensitive strain was employed as the control to determine the changes in potency.
TABLE 4.
Changes in inhibitory potencies of NNRTIs and NRTIs against viruses containing resistance mutations to NRTIs, PIs, and both NRTIs and PIs
| Mutant virus | Fold change in potency compared with that against adrug-sensitive straina
|
||||
|---|---|---|---|---|---|
| 3TC | TDF | EFV | NVP | MK-4965 | |
| NRTI resistant (n = 4) | >103 | 1.97 ± 0.56 | 0.38 ± 0.09 | 0.49 ± 0.18 | 0.30 ± 0.07 |
| PI resistant (n = 6) | 1.15 ± 0.29 | 0.82 ± 0.15 | 0.90 ± 0.42 | 1.05 ± 0.5 | 0.84 ± 0.4 |
| NRTI and PI resistant (n = 7) | 5.96 ± 2.4a | 2.43 ± 2.41 | 0.2 ± 0.06 | 0.32 ± 0.15 | 0.18 ± 0.06 |
Four of seven viruses displayed >100-fold shifts.
HIV-1 is known to infect resting cells as well as proliferating cells; thus, it is important to assess the impacts of antiviral agents on the viabilities of these cell types. Consequently, the cytotoxicity of MK-4965 was tested in stationary and activated primary cells (CD4 cells, monocytes, peripheral blood mononuclear cells, and macrophages). Proliferating cells (MT4, SupT1, and HL60 cells) were also evaluated for their ability to tolerate MK-4965. The results showed that MK-4965 possesses a low level of cytotoxicity against the cell lines tested in the present study (EC50s, >3 μM) (data not shown).
The need to use combination therapy for the treatment of HIV-1 infection often presents challenges owing to potential drug-drug interactions. In particular, one component of combination therapy may potentially have an effect on the antiviral activity of some other component(s), which could be synergistic, additive, or antagonistic. For instance, RBV displays significant antagonistic effects on the anti-HIV activity of d4T, and the use of such combinations should be avoided. To test whether MK-4965 has any antagonistic interactions with other anti-HIV agents, extensive studies with two-drug combinations were conducted to evaluate the antiviral activity in cell culture obtained when MK-4965 was combined with each of 18 licensed anti-HIV agents.
The Prichard and Shipman (27) MacSynergy II three-dimensional model was employed for statistical evaluation of the results of the combination assays. An additive effect suggests that the total antiviral activity of the two compounds at different concentrations should be equal to the sum of the antiviral activity of the individual compounds at the corresponding concentrations. As a result, on the basis of a three-dimensional model, a merely additive effect results in a horizontal plane at 0% inhibition (plane of additivity) when the antiviral activity of each compound is subtracted from the total antiviral activity determined in the two-drug combination study. Synergistic and antagonistic effects, on the other hand, render surfaces above and below the plane of additivity, respectively. Four representative three-dimensional plots are presented in Fig. 3. Figure 3A to D presents the results of a study of MK-4965 in combination with an integrase inhibitor (RAL), an NRTI (TDF), a CCR5 antagonist (MVC), and a PI (DRV), respectively. All results show that the percent inhibition after subtraction was on or close to the plane of additivity, which suggests a nonantagonistic effect on the basis of the criteria described in Materials and Methods. In contrast, the positive antagonism control for the combination study (d4T in combination with RBV) exhibited a highly antagonistic interaction in all experiments (mean antagonism volumes, −311 μM2% with CEM-SS cells and −591 μM2% with MAGI-CCR5 cells). The results are summarized in Table 5.
FIG. 3.
Mean three-dimensional plot of MK-4965 and other antiviral agents in the two-drug combination study. (A) MK-4965 and RAL; (B) MK-4965 and tenofovir DF; (C) MK-4965 and MVC; (D) MK-4965 and DRV.
TABLE 5.
Antiviral efficacy results for MK-4965 in combination with 18 FDA-approved antiretroviral compounds in CEM-SS or MAGI-CCR5 cellsa
| Compound class and compoundb | Mean synergy vol/antagonism vol (nM2%, μM2%, or nMμM%)c | Antiviral effect |
|---|---|---|
| NRTIs | ||
| 3TC | 27.9/−3.75 | Nonantagonistic |
| ABC | 47.0/−10.9 | Nonantagonistic |
| AZT | 76.5/−12.6 | Nonantagonistic |
| d4T | 19.1/−6.74 | Nonantagonistic |
| ddC | 12.5/−4.46 | Nonantagonistic |
| ddI | 45.1/−4.07 | Nonantagonistic |
| FTC | 17.0/−0.52 | Nonantagonistic |
| TDF | 22.6/−4.88 | Nonantagonistic |
| Tenofovir DF | 40.5/−7.49 | Nonantagonistic |
| NNRTIs | ||
| DLV | 19.2/−4.43 | Nonantagonistic |
| EFV | 29.5/−1.50 | Nonantagonistic |
| ETR | 14.6/−1.24 | Nonantagonistic |
| NVP | 28.2/−19.6 | Nonantagonistic |
| PIs | ||
| DRV | 35.8/−2.14 | Nonantagonistic |
| IDV | 19.4/−0.08 | Nonantagonistic |
| Entry inhibitors | ||
| MVC | 6.22/−24.3 | Nonantagonistic |
| ENF | 23.8/−2.16 | Nonantagonistic |
| Integrase strand transfer inhibitor (RAL) | 24.6/−3.38 | Nonantagonistic |
| d4T-RBV (positive control) | ||
| CEM-SS cells | 3.80/−311 | Highly antagonistic |
| MAGI-CCR5 cells | 0.53/−591 | Highly antagonistic |
The 95% confidence intervals around the experimental dose-response surface were used to evaluate the data statistically.
Studies of the antiviral efficacy of MK-4965 in combination with MVC were performed with MAGI-CCR5 cells. All other evaluations were performed with CEM-SS cells.
The antiviral synergy plot (95%) data sets from multiple experiments (n = 3) were combined, and the arithmetic means were calculated for each drug-drug concentration. The positive and negative values are individually summed to give the mean volumes for synergistic and antagonistic interactions, respectively.
On the basis of the synergy criteria defined earlier, no antagonistic interactions in antiviral efficacy between MK-4965 and each of the 18 FDA-approved antiretroviral drugs tested in this study were observed over the concentration ranges examined. A slightly synergistic interaction was observed between MK-4965 and AZT, suggesting possible beneficial interactions with the use of this combination. However, the slight synergy observed with AZT was the result of the findings of a single experiment, and clear additive interactions were observed in the other two experiments. The interactions of MK-4965 with the remaining drugs resulted in nonantagonistic effects. The overall interpretation of these data suggests that no antagonism of the antiviral effects of MK-4965 when it was used in combination with each of the drugs from the same or different classes of drugs was observed in the study.
DISCUSSION
MK-4965 displayed only a twofold shift in potency against both the K103N and the Y181C RTs in comparison to the potency against the WT RT (Table 1). In a cell-based assay (Table 2), MK-4965 also showed two- to threefold shifts in EC95s against the K103N virus compared to the EC95 against WT virus. For the Y181C virus, however, a higher shift in potency was observed, with the EC95 shifting six- to sevenfold. For a specific compound, it is anticipated that the profile of activity against mutants should maintain the same trend irrespective of the type of assay performed (i.e., a biochemical or a cell-based assay). The results described above indicate that the Y181C virus displayed a greater extent of resistance than the Y181C RT when the corresponding WT virus and WT RT were used as the control. The discordance in the extent of resistance for the Y181C variant between the biochemical and cell-based assays cannot be attributed to experimental error, as the phenomenon was also observed with other compounds tested in this study and the experimental results were averaged from at least seven repeats in the cell-based assay. The potential factors associated with Y181C virus that contribute to these discrepancies require further investigation.
Compounds that have a higher degree of protein binding often exhibit greater reductions in potency when they are tested in the presence of a higher percentage of serum (from 10% FBS to 50% HS). As shown in Table 2, both EFV and ETV displayed approximately 7- to 10-fold shifts in antiviral activity when the serum concentration was increased from 10% to 50%. MK-4965 exhibited an approximately four- to sixfold shift in potency in the presence of 50% HS. These results are not surprising, as MK-4965 is less protein bound (96.5%) than either EFV or ETV (>99.5%) (5, 13). NVP, which is only 60% protein bound (19), did not show any shift in EC95 for the WT virus when the serum concentration was increased from 10% to 50%.
Virus containing a single mutation (Y188L) conferred more than 100-fold resistance to both MK-4965 and EFV. On the basis of the X-ray structure of the RT-MK-4965 complex, MK-4965 has a close interaction with Y188 via π-π stacking (34). Replacement of the aromatic side chain of the Y188 residue with the aliphatic side chain of the leucine residue would eliminate the π-π stacking interaction, thereby significantly reducing the binding affinity of MK-4965 to the NNRTI pocket. The Y188L mutation is present in only ∼5% of patients who have experienced the virologic failure of therapy with NNRTI-containing regimens (4), even though the replication capacity of viruses containing a Y188L mutation is reportedly comparable to that of viruses containing a K103N mutation (18). One possible explanation for its relative rarity in clinical isolates is that the Y188L mutation requires two base changes, while K103N requires only a single base change. The Y188L mutation is derived from an intermediate mutant, either Y188H or Y188F. Mutants with either of these mutations are highly susceptible to NNRTIs, so the opportunity for either Y188H or Y188F to further develop into a Y188L mutation may be limited (30).
ETV, in contrast, showed only a minor shift in potency (approximately fivefold) against the Y188L virus (2). However, mutants with the L100I and K103N double mutations and mutants with the Y181C and K103N double mutations displayed greater than 10-fold increases in the levels of resistance to ETV (2) and MK-4965 compared with the level of resistance of the WT. The L100I and K103N double mutation is reported to be the most frequent combination of mutations associated with ETV resistance (22). Single mutations that reduce susceptibility to ETV more than 10-fold compared with that of the WT include Y181I, F227C, K101P, and M230L (14). The novel mutations V179F and V179I were identified by resistance selection with ETV in vitro (36). Although these two mutations alone do not confer resistance to ETV, each of them is associated with virologic failure when they coexist with other mutations (2, 14). However, the role of V179 in the emergence of ETV resistance remains uncertain. In addition, V179I is a common polymorphism in viruses of clade A, which is the dominant HIV-1 variant in West and Central Africa (31). These observations raise the question of whether patients infected with subtype A virus would experience higher rates of virologic failure than patients infected with other subtypes when they are treated with ETV-containing regimens. In clinical trials with ETV, it was found that the decline in the viral load was not affected by the preexistence of K103N but was reduced in the presence of Y181C (14). Y181C was also selected by in vitro resistance selection with ETV (35). Moreover, ETV-specific resistance mutations usually associate with the Y181C mutation, and the number of additional NNRTI resistance mutations that coexisted with Y181C was inversely associated with the level of the viral load reduction in clinical trials. In the DUET trial, it was concluded that the concurrent presence of three or more of 13 NNRTI resistance-specific mutations (V90I, A98G, L100I, K101E/P, V106I, V179D/F, Y181C/I/V, G190A/S) was associated with a decreased virological response to ETV (21, 23).
When the activity of MK-4965 against different HIV-1 isolates was tested, subtype D and H viruses showed greater susceptibility to the NNRTIs than the other subtypes tested. In particular, subtype H virus appeared to be more vulnerable to NNRTIs, with the reduction in the EC50 in comparison to that for the control virus being more than fivefold. When the consensus RT amino acid sequences of subtypes D and H within the NNRTI binding pocket were compared with the consensus sequence of subtype B, there were a total of 11 amino acid differences at various positions. However, it remains to be verified if those amino acids contribute to the hypersensitivity of the viruses to NNRTIs.
As expected, viruses with resistance to NRTIs or PIs were not cross-resistant to NNRTIs (Table 4). All of the NRTI-resistant viruses tested, however, were hypersensitive to the NNRTIs tested. On the basis of the sequence data, all NRTI-resistant viruses in the panel evaluated in this study contained a T215Y mutation in RT, which has been shown to be associated with hypersusceptibility to NNRTIs (10, 29, 33).
In the two-drug combination studies, there was no evidence of antagonistic interactions between MK-4965 and any other agent employed. Importantly, there was no evidence of synergistic cytotoxicity within the range of drug concentrations examined for MK-4965 (high test concentration, 100 nM). This was not unexpected, because none of the drugs are cytotoxic over the concentration ranges evaluated; much higher concentrations of all compounds (near the 50% toxic concentration) would be required to correctly examine potential synergistic cytotoxicity interactions. It should also be noted that the MacSynergy II software utilizes the individual triplicate data for 40 different drug combinations to generate the three-dimensional surface plots and their associated statistical 95% confidence intervals. As such, the drug interactions observed between MK-4965 and 18 FDA-approved drugs predicted by the Prichard and Shipman (27) MacSynergy II model have statistical significance associated with them. Analysis of the data for drug combinations by other analytical methods (9) typically yields similar synergy observations, but the median-effect equation derived by Chou (8) lacks the statistical confidence intervals associated with the MacSynergy II analysis. The overall performances of the assays were validated by use of a positive control for antagonism (d4T in combination with RBV), which exhibited the expected levels of antagonism in each of the assays (Table 5). Macroscopic observation of the cells in each well of the microtiter plates confirmed the cytotoxicity and cytopathogenicity results obtained following staining of the cells with the metabolic dye MTS.
In summary, MK-4965 is a novel NNRTI containing diaryl ether and indazole moieties. It exhibits excellent activity against RT enzymes containing K103N or Y181C mutations and also against viruses containing the same RT mutations. All HIV subtypes tested in this study had similar susceptibilities to MK-4965, and PI and NRTI resistance-conferring mutations did not compromise the antiviral activity of MK-4965. Given the absence of antagonistic effects with the other antiviral agents tested in the combination study, MK-4965 has in vitro properties consistent with the high potential to be a new NNRTI for treatment of HIV-1 infection.
Acknowledgments
We thank John Wai in the Merck Department of Medicinal Chemistry for providing the RAL used in the combination study. We also thank Amy Jackson in the Visual Communication Department for assistance with the revision of Fig. 2 and 3.
Footnotes
Published ahead of print on 16 March 2009.
REFERENCES
- 1.Ambrose, Z., J. G. Julias, P. L. Boyer, V. N. Kewalramani, and S. H. Hughes. 2006. The level of reverse transcriptase (RT) in human immunodeficiency virus type 1 particles affects susceptibility to nonnucleoside RT inhibitors but not to lamivudine. J. Virol. 80:2578-2581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Andries, K., H. Azijn, T. Thielemans, D. Ludovici, M. Kukla, J. Heeres, P. Janssen, B. De Corte, J. Vingerhoets, R. Pauwels, and M. P. de Bethune. 2004. TMC125, a novel next-generation nonnucleoside reverse transcriptase inhibitor active against nonnucleoside reverse transcriptase inhibitor-resistant human immunodeficiency virus type 1. Antimicrob. Agents Chemother. 48:4680-4686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bacheler, L., S. Jeffrey, G. Hanna, R. D'Aquila, L. Wallace, K. Logue, B. Cordova, K. Hertogs, B. Larder, R. Buckery, D. Baker, K. Gallagher, H. Scarnati, R. Tritch, and C. Rizzo. 2001. Genotypic correlates of phenotypic resistance to efavirenz in virus isolates from patients failing nonnucleoside reverse transcriptase inhibitor therapy. J. Virol. 75:4999-5008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bacheler, L. T., E. D. Anton, P. Kudish, D. Baker, J. Bunville, K. Krakowski, L. Bolling, M. Aujay, X. V. Wang, D. Ellis, M. F. Becker, A. L. Lasut, H. J. George, D. R. Spalding, G. Hollis, and K. Abremski. 2000. Human immunodeficiency virus type 1 mutations selected in patients failing efavirenz combination therapy. Antimicrob. Agents Chemother. 44:2475-2484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Boffito, M., A. Winston, A. Jackson, C. Fletcher, A. Pozniak, M. Nelson, G. Moyle, I. Tolowinska, R. Hoetelmans, D. Miralles, and B. Gazzard. 2007. Pharmacokinetics and antiretroviral response to darunavir/ritonavir and etravirine combination in patients with high-level viral resistance. AIDS 21:1449-1455. [DOI] [PubMed] [Google Scholar]
- 6.Carr, J. K., M. O. Salminen, J. Albert, E. Sanders-Buell, D. Gotte, D. L. Birx, and F. E. McCutchan. 1998. Full genome sequences of human immunodeficiency virus type 1 subtypes G and A/G intersubtype recombinants. Virology 247:22-31. [DOI] [PubMed] [Google Scholar]
- 7.Castro, H. C., N. I. V. Loureiro, M. Pujol-Luz, A. M. T. Souza, M. G. Albuquerque, D. O. Santos, L. M. Cabral, I. C. Frugulhetti, and C. R. Rodrigues. 2006. HIV-1 reverse transcriptase: a therapeutical target in the spotlight. Curr. Med. Chem. 13:313-324. [DOI] [PubMed] [Google Scholar]
- 8.Chou, T. 1974. Relationships between inhibition constants and fractional inhibition in enzyme-catalyzed reactions with different numbers of reactants, different reaction mechanisms, and different types and mechanisms of inhibition. Mol. Pharmacol. 10:235-247. [PubMed] [Google Scholar]
- 9.Chou, T. C., and P. Talalay. 1984. Quantitative analysis of dose-effect relationships: the combined effects of multiple drugs or enzyme inhibitors. Adv. Enzyme Regul. 22:27-55. [DOI] [PubMed] [Google Scholar]
- 10.Clark, S. A., N. S. Shulman, R. J. Bosch, and J. W. Mellors. 2006. Reverse transcriptase mutations 118I, 208Y, and 215Y cause HIV-1 hypersusceptibility to non-nucleoside reverse transcriptase inhibitors. AIDS 20:981-984. [DOI] [PubMed] [Google Scholar]
- 11.Das, K., P. J. Lewi, S. H. Hughes, and E. Arnold. 2005. Crystallography and the design of anti-AIDS drugs: conformational flexibility and positional adaptability are important in the design of non-nucleoside HIV-1 reverse transcriptase inhibitors. Prog. Biophys. Mol. Biol. 88:209-231. [DOI] [PubMed] [Google Scholar]
- 12.Delaugerre, C., R. Rohban, A. Simon, M. Mouroux, C. Tricot, R. Agher, J. M. Huraux, C. Katlama, and V. Calvez. 2001. Resistance profile and cross-resistance of HIV-1 among patients failing a non-nucleoside reverse transcriptase inhibitor-containing regimen. J. Med. Virol. 65:445-448. [PubMed] [Google Scholar]
- 13.DiCenzo, R., D. Peterson, M. Cruttenden, G. Morse, G. Riggs, H. Gelbard, and G. Schifitto. 2004. Effects of valproic acid coadministration on plasma efavirenz and lopinavir concentrations in human immunodeficiency virus-infected adults. Antimicrob. Agents Chemother. 48:4328-4331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Geretti, A. M. 2008. Shifting paradigms: the resistance profile of etravirine. J. Antimicrob. Chemother. 62:643-647. [DOI] [PubMed] [Google Scholar]
- 15.Gotte, M., X. G. Li, and M. A. Wainberg. 1999. HIV-1 reverse transcription: a brief overview focused on structure-function relationships among molecules involved in initiation of the reaction. Arch. Biochem. Biophys. 365:199-210. [DOI] [PubMed] [Google Scholar]
- 16.Harris, M. E., S. Maayan, B. Kim, M. Zeira, G. Ferrari, D. L. Birx, and F. E. McCutchan. 2003. A cluster of HIV type 1 subtype C sequences from Ethiopia, observed in full genome analysis, is not sustained in subgenomic regions. AIDS Res. Hum. Retrovir. 19:1125-1133. [DOI] [PubMed] [Google Scholar]
- 17.Hopkins, A. L., J. S. Ren, R. M. Esnouf, B. E. Willcox, E. Y. Jones, C. Ross, T. Miyasaka, R. T. Walker, H. Tanaka, D. K. Stammers, and D. I. Stuart. 1996. Complexes of HIV-1 reverse transcriptase with inhibitors of the HEPT series reveal conformational changes relevant to the design of potent non-nucleoside inhibitors. J. Med. Chem. 39:1589-1600. [DOI] [PubMed] [Google Scholar]
- 18.Huang, W., T. Wrin, and A. V. Gamarnik. 2002. RT mutations that confer NNRTI resistance may also impair replication capacity. Antivir. Ther. 7:S79. [Google Scholar]
- 19.Jackson, J. B., S. Barnett, E. Piwowar-Manning, L. Apuzzo, C. Raines, C. Hendrix, F. Hamzeh, and J. Gallant. 2003. A phase I/II study of nevirapine for pre-exposure prophylaxis of HIV-1 transmission in uninfected subjects at high risk. AIDS 17:547-553. [DOI] [PubMed] [Google Scholar]
- 20.Kaltenbach, J. P., M. H. Kaltenbach, and W. B. Lyons. 1958. Nigrosin as a dye for differentiating live and dead ascites cells. Exp. Cell Res. 15:112-117. [DOI] [PubMed] [Google Scholar]
- 21.Lazzarin, A., T. Campbell, B. Clotet, M. Johnson, C. Katlama, A. Moll, W. Towner, B. Trottier, M. Peeters, J. Vingerhoets, G. de Smedt, B. Baeten, G. Beets, R. Sinha, and B. Woodfall. 2007. Efficacy and safety of TMC125 (etravirine) in treatment-experienced HIV-1-infected patients in DUET-2: 24-week results from a randomised, double-blind, placebo-controlled trial. Lancet 370:39-48. [DOI] [PubMed] [Google Scholar]
- 22.Llibre, J. M., J. R. Santos, T. Puig, J. Molto, L. Ruiz, R. Paredes, and B. Clotet. 2008. Prevalence of etravirine-associated mutations in clinical samples with resistance to nevirapine and efavirenz. J. Antimicrob. Chemother. 62:909-913. [DOI] [PubMed] [Google Scholar]
- 23.Madruga, J. V., P. Cahn, B. Grinsztejn, R. Haubrich, J. Lalezari, A. Mills, G. Pialoux, T. Wilkin, M. Peeters, J. Vingerhoets, G. de Smedt, L. Leopold, R. Trefiglio, and B. Woodfall. 2007. Efficacy and safety of TMC125 (etravirine) in treatment-experienced HIV-1-infected patients in DUET-1: 24-week results from a randomised, double-blind, placebo-controlled trial. Lancet 370:29-38. [DOI] [PubMed] [Google Scholar]
- 24.Moore, J. P., and M. Stevenson. 2000. New targets for inhibitors of HIV-1 replication. Nat. Rev. Mol. Cell Biol. 1:40-49. [DOI] [PubMed] [Google Scholar]
- 25.Munshi, V., M. Lu, P. Felock, R. J. Barnard, D. J. Hazuda, M. D. Miller, and M. T. Lai. 2008. Monitoring the development of non-nucleoside reverse transcriptase inhibitor-associated resistant HIV-1 using an electrochemiluminescence-based reverse transcriptase polymerase assay. Anal. Biochem. 374:121-132. [DOI] [PubMed] [Google Scholar]
- 26.Petropoulos, C. J., N. T. Parkin, K. L. Limoli, Y. S. Lie, T. Wrin, W. Huang, H. Tian, D. Smith, G. A. Winslow, D. J. Capon, and J. M. Whitcomb. 2000. A novel phenotypic drug susceptibility assay for human immunodeficiency virus type 1. Antimicrob. Agents Chemother. 44:920-928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Prichard, M. N., and C. Shipman, Jr. 1990. A three-dimensional model to analyze drug-drug interactions. Antivir. Res. 14:181-205. [DOI] [PubMed] [Google Scholar]
- 28.Shaw-Reid, C. A., V. Munshi, P. Graham, A. Wolfe, M. Witmer, R. Danzeisen, D. B. Olsen, S. S. Carroll, M. Embrey, J. S. Wai, M. D. Miller, J. L. Cole, and D. J. Hazuda. 2003. Inhibition of HIV-1 ribonuclease H by a novel diketo acid, 4-[5-(benzoylamino)thien-2-yl]-2,4-dioxobutanoic acid. J. Biol. Chem. 278:2777-2780. [DOI] [PubMed] [Google Scholar]
- 29.Shulman, N. S., R. J. Bosch, J. W. Mellors, M. A. Albrecht, and D. A. Katzenstein. 2004. Genetic correlates of efavirenz hypersusceptibility. AIDS 18:1781-1785. [DOI] [PubMed] [Google Scholar]
- 30.Soriano, V., and C. de Mendoza. 2002. Genetic mechanisms of resistance to NRTI and NNRTI. HIV Clin. Trials 3:237-248. [DOI] [PubMed] [Google Scholar]
- 31.Spira, S., M. A. Wainberg, H. Loemba, D. Turner, and B. G. Brenner. 2003. Impact of clade diversity on HIV-1 virulence, antiretroviral drug sensitivity and drug resistance. J. Antimicrob. Chemother. 51:229-240. [DOI] [PubMed] [Google Scholar]
- 32.Sweeney, Z. K., and K. Klumpp. 2008. Improving non-nucleoside reverse transcriptase inhibitors for first-line treatment of HIV infection: the development pipeline and recent clinical data. Curr. Opin. Drug Discov. Dev. 11:458-470. [PubMed] [Google Scholar]
- 33.Tachedjian, G., and A. Mijch. 2004. Virological significance, prevalence and genetic basis of hypersusceptibility to nonnucleoside reverse transcriptase inhibitors. Sex. Health 1:81-89. [DOI] [PubMed] [Google Scholar]
- 34.Tucker, T. J., J. T. Sisko, R. M. Tynebor, T. M. Williams, P. J. Felock, J. A. Flynn, M.-T. Lai, Y. Liang, G. McGaughey, M. Liu, M. D. Miller, G. Moyer, V. Munshi, R. Perlow-Poehnelt, S. Prasad, J. C. Reid, R. Sanchez, M. Torrent, J. P. Vacca, B. Wan, and Y. Yan. 2008. Discovery of 3-{5-[(6-amino-1H-pyrazolo[3,4-b]pyridine-3-yl)methoxy]-2chlorophenoxy}-5-chlorobenzonitrile (MK-4965): a potent, orally bioavailable HIV-1 non-nucleoside reverse transcriptase inhibitor with improved potency against key mutant viruses. J. Med. Chem. 51:6503-6511. [DOI] [PubMed] [Google Scholar]
- 35.Vingerhoets, J., H. Azijn, E. Fransen, I. De Baere, L. Smeulders, D. Jochmans, K. Andries, R. Pauwels, and M. P. de Bethune. 2005. TMC125 displays a high genetic barrier to the development of resistance: evidence from in vitro selection experiments. J. Virol. 79:12773-12782. [DOI] [PMC free article] [PubMed] [Google Scholar]




