Abstract
We studied the antifungal activity of anidulafungin (AFG) in combination with voriconazole (VRC) against experimental invasive pulmonary aspergillosis (IPA) in persistently neutropenic rabbits and further explored the in vitro and in vivo correlations by using Bliss independence drug interaction analysis. Treatment groups consisted of those receiving AFG at 5 (AFG5 group) and 10 (AFG10 group) mg/kg of body weight/day, VRC at 10 mg/kg every 8 h (VRC group), AFG5 plus VRC (AFG5+VRC group), and AFG10 plus VRC (AFG10+VRC group) and untreated controls. Survival throughout the study was 60% for the AFG5+VRC group, 50% for the VRC group, 27% for the AFG10+VRC group, 22% for the AFG5 group, 18% for the AFG10 group, and 0% for control rabbits (P < 0.001). There was a significant reduction of organism-mediated pulmonary injury, measured by infarct scores, lung weights, residual fungal burdens, and galactomannan indexes, in AFG5+VRC-treated rabbits versus those treated with AFG5 and VRC alone (P < 0.05). In comparison, AFG10+VRC significantly lowered only infarct scores and lung weights in comparison to those of AFG10-treated animals (P < 0.05). AFG10+VRC showed no significant difference in other outcome variables. Significant Bliss synergy was found in vivo between AFG5 and VRC, with observed effects being 24 to 30% higher than expected levels if the drugs were acting independently. These synergistic interactions were also found between AFG and VRC in vitro. However, for AFG10+VRC, only independence and antagonism were observed among the outcome variables. We concluded that the combination of AFG with VRC in treatment of experimental IPA in persistently neutropenic rabbits was independent to synergistic at a dosage of 5 mg/kg/day but independent to antagonistic at 10 mg/kg/day, as assessed by Bliss independence analysis, suggesting that higher dosages of an echinocandin may be deleterious to the combination.
Invasive pulmonary aspergillosis is an important cause of morbidity and mortality in patients with cancer, hematopoietic stem cell transplantation, solid organ transplantation, and other immunodeficiencies (1, 4, 8, 13, 21, 36). Despite the use of single agents, such as amphotericin B, its lipid formulations, antifungal triazoles, and echinocandins, mortality associated with invasive pulmonary aspergillosis remains high (22, 32). Combination therapy with the echinocandins and triazoles may be more active against invasive aspergillosis than therapy with a single agent alone (10, 26). The echinocandins are a class of semisynthetic lipopeptide antifungal compounds that inhibit synthesis of (1→3)-β-d-glucan, a key component of the cell walls of most pathogenic fungi (6, 14).
The antifungal triazoles inhibit fungal cell membrane biosynthesis through inhibition of ergosterol formation at the level of lanosterol C14-demethylase (9, 17, 28, 29). Analysis of pharmacodynamic interactions poses a challenge to assessing the efficacy of combination therapy and its superiority over monotherapy. Robust mathematical pharmacodynamic models are powerful tools for the detection of synergistic and antagonistic interactions and for correlating in vivo data with in vitro data. Bliss independence drug interaction analysis, which is based on the probability theory for independent events, was previously used to correlate in vitro and in vivo data on the antagonistic combination of ravuconazole with amphotericin B against invasive aspergillosis (16).
We hypothesized that the simultaneous inhibition of the biosynthesis of key components of the fungal cell wall and cell membrane by the combination of an echinocandin and an antifungal triazole may result in a synergistic interaction in vitro and in vivo. We further hypothesized that Bliss independence analysis of this possible in vitro and in vivo interaction may provide a useful tool by which to assess probable synergistic antifungal effects. We therefore examined the potential therapeutic utility of the combination of anidulafungin and voriconazole in the treatment of experimental invasive pulmonary aspergillosis in persistently neutropenic rabbits and studied the in vitro and in vivo correlations of this interaction by Bliss independence drug interaction analysis.
MATERIALS AND METHODS
Isolate.
NIH Aspergillus fumigatus isolate 4215 (ATCC MYA-1163), obtained from a patient with a fatal case of pulmonary aspergillosis, as previously described (26), was used in the experiments. The MIC of voriconazole (Pfizer Ireland Pharmaceuticals, Ringaskiddy, Ireland) and the minimum effective concentration of anidulafungin (Eraxis; Pfizer Inc., New York, NY) against A. fumigatus, determined according to CLSI standard M38-A microdilution methods (18), were 0.5 to 1 μg/ml and 0.25 μg/ml, respectively.
In vitro combination studies.
The combination of anidulafungin and voriconazole was tested against A. fumigatus in triplicate with an in vitro broth microdilution checkerboard assay in 96-well flat-bottomed microtitration plates (Corning Incorporated, Corning, NY), based on the CLSI M-38A method (18). Twofold serial dilutions of anidulafungin and voriconazole were prepared in 50 μl of RPMI 1640 buffered at pH 7.0 with 0.165 M MOPS (morpholinepropanesulfonic acid) at concentrations of four times the final concentrations, which ranged from 1 to 0.015 mg/liter and 0.25 to 0.0005 mg/liter for anidulafungin and voriconazole, respectively. After inoculation with 100 μl of 4 × 104 CFU/ml prepared from 5- to 7-day-old cultures on potato dextrose agar, microtiter plates were incubated (Steri-Cult 200 incubator; DoveBid Inc., CA) at 35°C for 48 h. Growth in each well was quantified spectrophotometrically at 405 nm (optical density at 405 nm [OD405]), using 16 scan points per well, in a spectrophotometer (Elx808; Bio-Tek Instruments, Winooski, VT). The percentage of growth inhibition in each well was calculated based on the following equation: 100% − (OD405 of a well − background OD405)/(OD405 of the drug-free well − background OD405 of the drug-free well) × 100% (equation 1). Background OD405s were measured from a plate inoculated with a conidium-free inoculum and handled in the same way as the inoculated plates with the conidium-containing inocula.
In order to describe the concentration-effect relationships of anidulafungin and voriconazole alone, a sigmoid Emax model was fitted to the % growth inhibition obtained at each concentration of the drugs alone for each replicate. The Emax model was described by the following equation: E = Emax × Dm/(EC50m + Dm) (equation 2), where E is the percentage of growth (dependent variable) at the drug concentration D (independent variable) and Emax is the maximum percentage of growth observed in the drug-free control. The EC50 and m were estimated with the Emax model regression analysis. EC50 is the drug concentration producing 50% of the Emax, and m is the slope of the concentration-effect curve (Hill constant). The interaction was assessed with the Bliss independence response surface analysis.
Pharmacodynamic Bliss independence-based drug interaction analysis.
Bliss independence is described by the equation EIND = EA + EB − EA × EB (equation 3) for a certain combination of x mg/liter of drug A and y mg/liter of drug B. EA is the % fungal growth inhibition at x mg/liter of drug A alone, EB is the % fungal growth inhibition at y mg/liter of drug B alone, and EIND is the expected % fungal growth inhibition of a noninteractive (independent) theoretical combination of x mg/liter of drug A with y mg/liter of drug B. The difference (ΔE = EOBS − EIND) between the expected % growth inhibition, EIND, and the experimentally observed % growth inhibition, EOBS, describes the interaction of each combination of the concentrations of the two drugs. If ΔE and its 95% confidence interval (CI) were >0 (i.e., EOBS > EIND, and hence, more growth inhibition was observed than if the two drugs were acting independently), Bliss synergy was concluded for that particular combination. If ΔE and its 95% CI were <0 (i.e., EOBS < EIND, and hence, less growth inhibition was observed than if the two drugs were acting independently), Bliss antagonism was concluded for that particular combination. In any other case where the 95% CI of ΔE would include 0, the conclusion was Bliss independence.
In each of the independent replicate experiments, % growth inhibition of anidulafungin (EAFG) and voriconazole (EVRC) alone was obtained using the Emax model parameters. Thus, theoretical % growth of an independent combination, EIND, was calculated based on the following equation, where EAFG and EVRC were obtained from the Emax model. Thus, EIND = EAFG × EVRC = Emax,AFG ×  /(
/( +
+  ) × Emax,VRC ×
) × Emax,VRC ×  / (
/ ( +
+  ) (equation 4), where the subscript in each parameter indicates the Emax parameter described above for the concentration-effect curves of anidulafungin and voriconazole alone. For each combination of x mg/liter of voriconazole with y mg/liter of anidulafungin, the ΔE (EOBS − EIND) was calculated and the interaction was assessed as described above. When the statistically significantly different from zero ΔEs of all combinations (7 × 10) were plotted in a three-dimensional plot, an interaction surface plot was obtained, with peaks above and below the 0 plane indicating synergistic and antagonistic combinations, respectively, while the 0 plane itself indicated no statistically significant interactions. As summary measures of the interaction surface, the sum and the mean of all statistically significant synergistic (ΔE ± 95% CI > 0) and antagonistic (ΔE ± 95% CI < 0) combinations were reported.
) (equation 4), where the subscript in each parameter indicates the Emax parameter described above for the concentration-effect curves of anidulafungin and voriconazole alone. For each combination of x mg/liter of voriconazole with y mg/liter of anidulafungin, the ΔE (EOBS − EIND) was calculated and the interaction was assessed as described above. When the statistically significantly different from zero ΔEs of all combinations (7 × 10) were plotted in a three-dimensional plot, an interaction surface plot was obtained, with peaks above and below the 0 plane indicating synergistic and antagonistic combinations, respectively, while the 0 plane itself indicated no statistically significant interactions. As summary measures of the interaction surface, the sum and the mean of all statistically significant synergistic (ΔE ± 95% CI > 0) and antagonistic (ΔE ± 95% CI < 0) combinations were reported.
Animals and inoculation.
Healthy female New Zealand White rabbits (Covance Research Products, Inc., Denver, PA) weighing 2.6 to 3.5 kg at the time of endotracheal inoculation were used in experiments. A total of 70 rabbits were used in four replicate experiments. All experimental groups were studied simultaneously. There were no significant differences between experiments, and the findings were consistently replicated. All rabbits were monitored under humane care and use standards in facilities accredited by the Association for Assessment and Accreditation of Laboratory Animal Care International, according to the guidelines for the care and use of laboratory animals of the National Research Council (19) and under the approval of the Animal Care and Use Committee of the National Cancer Institute. Rabbits were individually housed and maintained with water and standard rabbit feed ad libitum. Vascular access was established by the surgical placement of a Silastic tunneled central venous catheter as previously described.
For each experiment, an inoculum of 1 × 108 to 1.25 × 108 conidia of A. fumigatus in a volume of 250 μl to 350 μl was prepared. Endotracheal inoculation was performed on day 2 of the experiments, with rabbits under general anesthesia, as described previously (26).
Immunosuppression and maintenance of neutropenia.
Immunosuppression and profound and persistent neutropenia (a neutrophil concentration of <100 neutrophils/μl) were established and maintained using cytarabine (Cytosar-U; Pharmacia-Upjohn, Kalamazoo, MI) and methylprednisolone (Solu-Medrol; Pfizer for Pharmacia & Upjohn Corp., New York, NY) as described previously (26). Antibiotics (ceftazidime, gentamicin, and vancomycin) were used for prevention of opportunistic bacterial infections during neutropenia (26).
Antifungal compounds and treatment regimens.
Rabbits were grouped to receive anidulafungin at 5 (AFG5 group) (n = 9) and 10 (AFG10 group) (n = 11) mg/kg of body weight/day intravenously (i.v.), voriconazole at 10 mg/kg every 8 h (q8h) i.v. (VRC group) (n = 12), a combination of AFG5 with VRC (AFG5+VRC group) (n = 10) or AFG10 with VRC (AFG10+VRC group) (n = 11) for treatment of established invasive pulmonary aspergillosis, or no drug (control group) (n = 17). Anidulafungin was provided as a pharmaceutical-grade powder (50 mg/vial) and was reconstituted with sterile normal saline to achieve a 1-mg/ml concentration. Voriconazole (200 mg/vial) was reconstituted from pharmaceutical-grade powder with sterile water to achieve a final concentration of 10 mg/ml.
Outcome variables.
The following panel of outcome variables was used to assess antifungal efficacy: survival, pulmonary infarct score, lung weight, residual fungal burden (log CFU/g), pulmonary infiltrate volume, serum galactomannan index (GMI), bronchoalveolar lavage (BAL) fluid galactomannan level, and BAL fluid DNA level. The outcome variable panel was applied to all experimental rabbits when possible.
Survival.
The survival time in days postinoculation was recorded for each rabbit in each group. Following humane end points, rabbits were euthanized by i.v. administration of pentobarbital (65 mg of pentobarbital sodium/kg of body weight) (Beuthanasia-D Special [euthanasia solution]; Schering-Plough Animal Health Corp., Union, NJ) on day 13 postinoculation, 24 h after the last dose of study drug (37).
Pulmonary lesion scores, lung weights, and residual fungal burden.
The lungs were carefully resected at autopsy. Pulmonary lesion scores and lung weights were assessed and calculated as previously described (26). Lung tissue from each rabbit was sampled and cultured by a standard excision of tissue from each lobe as previously described (26). The number of CFU of A. fumigatus was counted and recorded for each lobe, and the CFU/g was calculated.
Multidimensional volumetric imaging by computerized tomography.
Computerized tomography was performed to measure the response of pulmonary infiltrates to antifungal therapy (38). A semiautomatic method was then used to measure the volume of lung lesions, as previously described (27).
BAL.
BAL was performed on each lung preparation, as described previously (25), by the instillation of 10 ml of sterile normal saline into the clamped trachea with a sterile 12-ml syringe and subsequent withdrawal. The instillation was repeated twice. The lavage fluid was then centrifuged for 10 min at 400 × g. Part of the supernatant was discarded, leaving the pellet and 2 ml of supernatant, which was then vortexed. A 0.1-ml sample of this fluid and 0.1 ml of a dilution (101) of this fluid were cultured on 5% Sabouraud glucose agar plates.
Galactomannan assay.
Blood from each rabbit infected with A. fumigatus was collected every other day for determination of serum galactomannan concentrations. Serum and BAL fluid galactomannan concentrations were determined by the Platelia Aspergillus EIA (Bio-Rad, Marnes la Coquette, France) one-stage immunoenzymatic sandwich microplate assay method (33). Enzyme immunoassay data were expressed as the serum GMI plotted over time. The GMI for each test serum sample was equal to the absorbance of a standard sample divided by the absorbance of a threshold serum provided by the manufacturer.
DNA extraction from BAL fluid.
Frozen BAL fluid samples were thawed before extraction was performed. As previously described (20), samples were vortexed for 1 min before a 500-μl aliquot was taken for processing. Following centrifugation for 10 min at 16,000 × g, the supernatant was discarded, and the pellet was gently resuspended in 100 μl spheroplast buffer (1.0 M sorbitol, 50.0 mM sodium phosphate monobasic, 0.1% 2-mercaptoethanol, 10 mg of lyticase/ml [Sigma]) and 10 μl of lysing enzymes and incubated at 37°C on a rocking platform for 60 min. After centrifugation for 20 min at 400 × g, the spheroplast-BAL fluid pellet was resuspended in 400 μl AP1 buffer (DNeasy plant kit; Qiagen, Valencia, CA). The sample was added to lysing matrix D tubes (Fastprep sample preparation system; QBIOgene/MP Biomedical, Irvine, CA) and processed using a FastPrep instrument (QBIOgene/MP Biomedical). Specimens were centrifuged at 16,000 × g for 30 to 60 s and then gently vortexed. An aliquot of 300 μl of the specimen was transferred to a 1.5-ml tube and adjusted to a volume of 400 μl with AP1 buffer. An aliquot of 4 μl of RNase A (100 mg/ml) was added, vortexed vigorously, and incubated for 10 min at 65°C in an Eppendorf thermomixer (Eppendorf, Westbury, NY) at 1,200 rpm. The DNeasy plant kit protocol was followed, with the following modification: after the 200 μl of preheated (65°C) AE buffer (Qiagen, Valencia, CA) was applied to the column, the entire apparatus (column and collection tube) was heated at 65°C in an Eppendorf thermomixer for 5 min. An aliquot of 100 μl of sterile water was also processed as described above as a control for any contamination from the DNA extraction kit components.
A real-time quantitative PCR assay targeting the ITS1, 5.8S, and ITS2 regions of the rRNA gene complex was designed. The primers and probes were designed using Oligo software (Molecular Biology Insights, Cascade, CO). Probes were purchased from Idaho Technologies (Salt Lake City, UT). The primers and probes were designed based on a multiple sequence alignment of rRNA sequences from GenBank, utilizing the Sequencher software package (Gene Codes Corp., Ann Arbor, MI). The NCBI BLAST database search program was used to determine the uniqueness of the primers and probes for A. fumigatus. The amplicon generated was 253 bp long.
The PCR master mix consisted of 0.5 μM of each of the primers, 5 mM MgCl2, 0.025% bovine serum albumin (Sigma-Aldrich Corp., St. Louis, MO), 0.05 U/ml Platinum Taq DNA polymerase (Invitrogen Corp., Carlsbad, CA), 10× PCR buffer (Invitrogen Corp., Carlsbad, CA), 0.2 mM PCR Nucleotide Mix Plus (dATP, dCTP, and dGTP at 10 mM each and dUTP at 30 mM; Roche Molecular Biochemicals, Indianapolis, IN), and 0.1 μM each of the fluorescein and LC Red-640 probes. In addition, HK-UNG thermostable uracil N-glycosylase (Epicentre, Madison, WI) was utilized as recommended by the manufacturer to prevent potential amplicon carryover. Each reaction mix contained an aliquot of 5 μl of extracted specimen, together with 15 μl of the master mix. The cycling conditions were as follows: uracil activation (37°C, 180 s), uracil heat inactivation (95°C, 60 s for 1 cycle), and denaturation (95°C, 0 s), annealing (58°C, 5 s), and extension (72°C, 15 s) for 50 cycles. Quantitation standards were performed in conjunction with each set of samples. The BAL fluid samples from each rabbit were screened with the following controls: (i) DNA extracted from normal BAL fluid and (ii) a negative control master mix (sterile water). Tenfold serial dilutions of genomic DNA extracted from A. fumigatus isolate 4215 were used as external quantitation standards for all quantitative PCRs.
In order to confirm the lack of PCR inhibitors in BAL fluid samples, a separate set of PCR/fluorescent resonance energy transfer reactions were performed which specifically did not target A. fumigatus (or mammalian) DNA. The primers and probes were designed to target the common plasmid cloning vector pBR322. The PCR master mix included a specific amount of target DNA (pBR322). The presence of inhibitors was tested by comparing the amplification efficiency of this reaction with the extracted samples against those performed with sterile water. Equivalent amplification efficiencies compared to reactions performed with water reflected the lack of inhibitors. Each lung and BAL fluid sample was tested for inhibitors as described above.
In vivo combination studies.
For the purpose of this analysis, the in vivo effects of percentage of fungal growth inhibition, E, were calculated by the following equation: 100% − MVtreated/MVcontrol, where MVtreated and MVcontrol were the measured variables for residual fungal burden (CFU/g), the number of pulmonary infarct lesions, the lung weight (g), serum GMI, BAL fluid GMI, BAL fluid DNA, and pulmonary infiltrate volume (computed tomography [CT] scan) for treated and untreated animals, respectively.
The expected effect EIND of a noninteractive (independent) theoretical combination of the voriconazole dosage with either dosage of anidulafungin was calculated with equation 1, where EA = EAFG was the effect of anidulafungin acting alone at a dosage of either 5 or 10 mg/kg (AFG5 or AFG10 group) and EB = EVRC was the effect of voriconazole acting alone at the dosage of 10 mg/kg (VRC group). The difference, ΔE, between the EIND and the experimentally observed effect EOBS for the combination groups AFG5+VRC and AFG10+VRC and Bliss interaction were assessed as described above.
Pharmacokinetic studies.
The plasma pharmacokinetics of voriconazole and anidulafungin were studied in five to eight infected animals per dosage cohort. Time points for sampling were determined by inspection of full plasma concentration profiles obtained for healthy rabbits following administration of similar dosages based upon previous plasma pharmacokinetic studies of anidulafungin (7) and voriconazole. Plasma sampling was performed on day 6 of antifungal therapy. Blood samples were drawn immediately postdosing and then at 0.25, 0.5, 1, 4, 8, and 24 h postdosing. Plasma was immediately separated by centrifugation and stored at −70°C until assayed.
Concentrations of anidulafungin were determined by employing a method developed at Lilly Research Laboratories (Indianapolis, IN) and then adapted, optimized, and validated in our laboratory, as described previously, by reversed-phased high-pressure liquid chromatography (7). Micafungin was used as an internal standard (IS) (50 μg/ml at 271 nm). Anidulafungin was extracted from heparinized plasma by solid-phase extraction (5). Quantification was based on the ratio of the peak areas of anidulafungin and IS. The coefficient of determination, r2, was ≥0.996, and the lower limit of quantification was 0.075 mg/liter. The intra- and interday coefficients of variation were <14%.
The assay for voriconazole extraction developed by Pennick and colleagues (23) was adapted and optimized in our laboratory. Concentrations of voriconazole were determined using high-performance liquid chromatography (Waters 2996 separation module, Alliance system, and photodiode array detector model 2996; Waters Inc., Milford, MA). The mobile phase consisted of acetonitrile-N,N,N′,N′-tetramethylethylenediamine (TEMED) phosphate buffer (Sigma-Aldrich, St. Louis, MO) (1.5 ml/liter, pH 7.4, adjusted with phosphoric acid; 55:45 [vol/vol]), delivered at 0.8 ml/min. Samples were maintained in the autosampler at 4°C in glass vials with 150-μl inserts. The injection volume was 75 μl. Fluconazole (100 μg/ml) was used as an IS. UV light absorbance for voriconazole was at 256.1 nm, and for fluconazole the wavelength was 262 nm. The retention time was 6.7 and 3.5 min, respectively, maintaining the analytical column at room temperature.
Prior to extraction, all plasma samples (500 μl) were spiked with 10 μl of IS, vortexed with 1 ml of borate buffer (BO3) (20 mM, pH 9) (Mallinckrodt Baker, Inc., Paris, KY) for 5 s, and incubated at room temperature for 15 min. Solid-phase extraction was performed on a RapidTrace (Caliper Life Science) workstation, using Varian Inc. Bond Elut C18 100-mg, 1-ml cartridges. Extraction was performed in the following order. Cartridges were conditioned with 1 ml of methanol followed by 1 ml of sterile water and 1 ml of BO3 buffer (0.2 M, pH 9). After the buffer was drained, samples, quality controls, or standards were applied onto cartridges at a speed of 1 ml/min, pushed by 5 ml of air at 42 ml/min. Cartridges were washed with 1 ml of BO3 buffer and 1 ml water-methanol (70/30) solution at 5 ml/min and dried under a current of air for 2 min. Voriconazole was eluted with 1 ml of ethyl alcohol (USP 200 proof; The Warner-Graham Co., Cockeysville, MD) containing 1% glacial acetic acid, placed in Fisher disposable culture tubes, and evaporated under a steady stream of air at 40°C in a Turbo-Vap LV evaporator (Zymark, Hopkinton, MA) for 45 min or until dry. The samples were reconstituted in 90 μl of mobile phase, transferred to vials, and injected onto a Waters SunFire C18 5 μm, 4.6- by 250-mm analytical column protected by a guard column (SunFire 5 μm C18 [20 × 4.5] column).
Standards and quality control samples were prepared by adding known amounts of voriconazole to normal rabbit plasma. A stock solution (10 mg/ml) was prepared by reconstituting voriconazole pharmaceutical-grade powder with 19 ml of sterile water, followed by a set of 10-fold dilutions in methanol in a range from 50 ng/ml to 50 μg/ml.
Quantification was based on the ratio of peak heights of voriconazole and the IS. Nine-point (0 to 2.5 ng/ml) and seven-point (0.75 to 50.000 ng/ml) standard nonweighted curves were linear, with r2 values of ≥0.9975 and ≥0.999, respectively.
Pharmacokinetic data analysis.
Pharmacokinetic parameters for anidulafungin and voriconazole were determined by population methodology, using the program nonparametric adaptive grid (NPAG) with adaptive gamma (14). A standard two-compartment pharmacokinetic model was used, with zero-order time-delimited input and first-order elimination from the central compartment. The entire data set (combination and monotherapy) was comodeled. The pharmacokinetic data were weighted by the inverse of the estimated assay variance for each drug. The fit of the model to the data was assessed using the log likelihood value and a visual inspection and coefficient of determination of the observed-versus-predicted values after the Bayesian step. The population mean and median parameter values were evaluated within the maximum a posteriori Bayesian analysis. The estimates of the pharmacokinetic parameters for each individual rabbit were obtained using the “population-of-one” utility within NPAG. The Bayesian estimates for each rabbit within the various treatment groups were collated. The AUC which developed in each rabbit at steady state was determined by integration.
Toxicity studies.
Blood was collected as previously described (26). Chemical determinations of creatinine, urea nitrogen, alanine aminotransferase (ALT), aspartate aminotransferase (AST), and potassium concentrations in serum were performed on the penultimate sample drawn from each rabbit.
Statistical analysis.
Comparisons between the groups were performed by Kruskal-Wallis test (nonparametric analysis of variance [ANOVA]) or the Mann-Whitney U test, as appropriate. The central hypothesis of this analysis was based upon the response of the combination treatment in comparison to that of anidulafungin alone and voriconazole alone. A two-tailed P value of ≤0.05 was considered to be statistically significant. Survival was plotted by Kaplan-Meier analysis. Differences in survival of treatment groups and untreated controls were analyzed by the log rank test. Values are expressed as means ± standard error of the means (SEMs). Pharmacokinetic parameters were compared using ANOVA or Student's t test, as appropriate.
RESULTS
Survival.
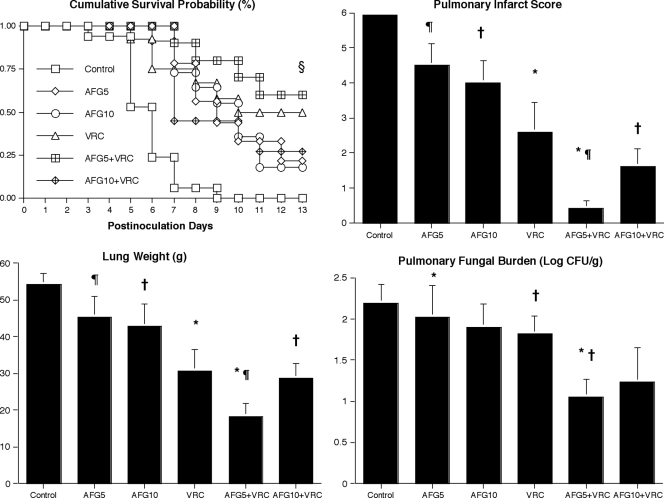
Improved survival was achieved through the entire study in 6 (60%) of 10 AFG5+VRC-treated rabbits, 6 (50%) of 12 VRC, 3 (27%) of 11 AFG10+VRC, 2 (22%) of 9 AFG5, and 2 (18%) of 11 AFG10-treated rabbits in comparison to 0 (0%) of 17 untreated control rabbits (P < 0.001) (Fig. 1). Even though the combination of AFG5+VRC demonstrated the highest survival rate (60%), there were no significant differences between either of the combination therapy groups and the monotherapy groups.
FIG. 1.
Response of primary pulmonary aspergillosis in persistently neutropenic rabbits to antifungal therapy measured by survival, mean pulmonary infarct score, mean lung weight, and mean pulmonary tissue residual fungal burden (log CFU/g) in untreated controls (Control (n = 17)) and rabbits treated with anidulafungin 5 mg/kg/day (AFG5 (n = 9)), anidulafungin 10 mg/kg/day (AFG10 (n = 11)), voriconazole 10 mg/kg/day Q8h (VRC (n = 12)), combination of AFG5 plus VRC (AFG5+VRC (n = 10)), and AFG10 plus VRC (AFG10+VRC (n = 11)). Values are given as means ± SEMs. For the measure of survival, the values on the y-axis are probability of survival, §, P ≤ 0.05. For all other comparisons, *, P ≤ 0.05; †, P ≤ 0.05; ¶, P ≤ 0.01.
Organism-mediated pulmonary injury.
There was a significant reduction in organism-mediated pulmonary injury as measured by infarct score, lung weight, and lesion volume. Rabbits receiving the AFG5+VRC combination had significantly lower infarct scores in comparison to that of AFG5 (P < 0.01), and VRC (P < 0.05) alone. In addition, rabbits treated with AFG10+VRC had significantly lower infarct scores in comparison to that of AFG10 (P < 0.05), but not of VRC-treated rabbits.
Lung weight was significantly decreased in AFG5+VRC-treated rabbits in comparison to that of AFG5 (P < 0.01) and VRC (P < 0.05) alone treated rabbits. Moreover, lung weights in AFG10+VRC combination were significantly lower in comparison to that of AFG10 (P < 0.05), but not to VRC monotherapies (Fig. 1).
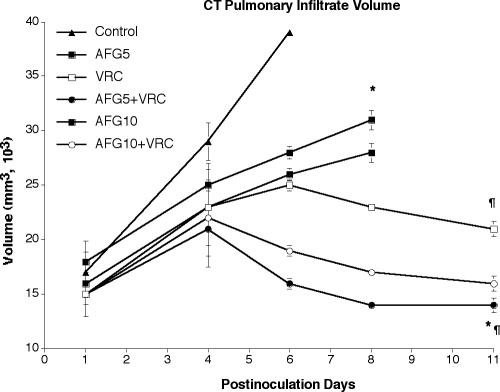
The pulmonary lesion volume measured by serial CT scans was consistent with these findings and demonstrated significant decrease in AFG5+VRC-treated rabbits in comparison to AFG5 and VRC (P ≤ 0.05) treated rabbits. On the other hand, there were no significant differences in AFG10+VRC group in comparison to that AFG10 or VRC monotherapies (Fig. 2).
FIG. 2.
Pulmonary infiltrate volume determined by image analysis of serial CT scans of untreated controls (Control) (n = 6), anidulafungin at 5 mg/kg/day (AFG5) (n = 4), at 10 mg/kg/day (AFG10) (n = 4), voriconazole at 10 mg/kg/day q8h (VRC) (n = 4), anidulafungin-voriconazole combinations (AFG5+VRC) (n = 4), and (AFG10+VRC) (n = 4) treated rabbits. Animals treated with AFG5+VRC combination demonstrated significant resolution of pulmonary infiltrate volume in comparison to that of anidulafungin (*, P ≤ 0.05), and VRC (¶, P ≤ 0.01) alone.
Residual fungal burden.
There was significant reduction of residual fungal burden (CFU/g) in AFG5+VRC-treated rabbits in comparison to AFG5 and VRC alone, (P < 0.05). There were no significant differences of AFG10+VRC-treated rabbits in comparison to that of AFG10 and VRC alone (Fig. 1).
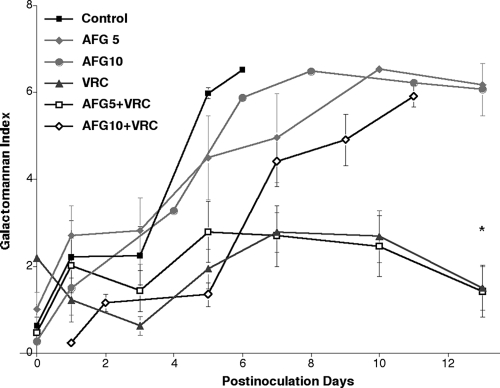
Serum galactomannan.
There was a significantly lower GMI on day 6 postinoculation in VRC, and AFG5+VRC-treated rabbits in comparison to that of all other groups (P < 0.05). The GMI progressively increased in untreated controls, AFG5, AFG10, and AFG10+VRC-treated rabbits during the experiment (Fig. 3).
FIG. 3.
Expression of galactomannan antigenemia in persistently neutropenic rabbits with pulmonary aspergillosis treated with anidulafungin at 5 (AFG5) (n = 6), anidulafungin at 10 mg/kg/day (AFG10) (n = 8), voriconazole at 10 mg/kg q8h (VRC) (n = 10), anidulafungin-voriconazole combinations (AFG5+VRC (n = 7) and AFG10+VRC (n = 8)), and untreared controls (Control) (n = 12). Animals treated with the AFG5+VRC combination and VRC alone had significantly lower levels of galactomannan antigenemia in comparison to all other groups (*, P ≤ 0.05).
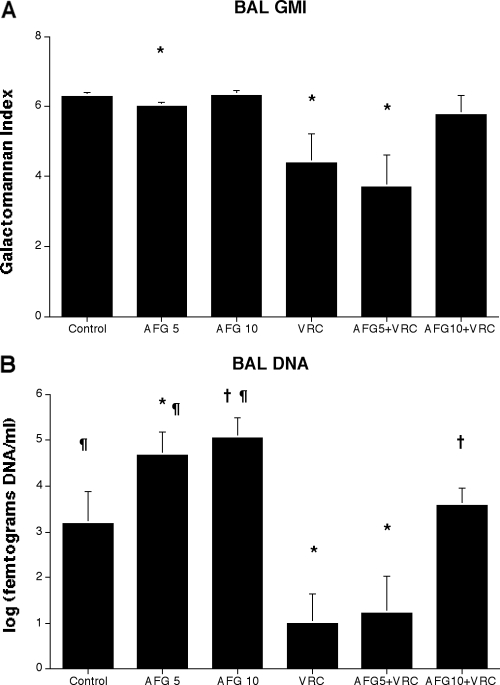
BAL fluid galactomannan.
Consistent with the response of other parameters, there was a significant decrease of BAL fluid GMI in rabbits treated with VRC alone or in combination of AFG5+VRC in comparison to that of AFG5-treated rabbits, (P < 0.05). There were no significant differences between AFG10+VRC-treated rabbits and rabbits treated with AFG10 and VRC alone (Fig. 4A).
FIG. 4.
Expression BAL fluid galactomannan antigen levels (A) and A. fumigatus DNA levels (B) in persistently neutropenic rabbits with pulmonary aspergillosis treated with anidulafungin at 5 (AFG5) (n = 6), anidulafungin at 10 mg/kg/day (AFG10) (n = 8), voriconazole at 10 mg/kg q8h (VRC) (n = 10), anidulafungin-voriconazole combinations (AFG5+VRC (n = 7) and AFG10+VRC (n = 8)), and untreated controls (Control) (n = 15). (A): Animals treated with the AFG5+VRC combination and VRC alone had significantly lower levels of galactomannan antigen (*, P ≤ 0.05) in BAL fluid. (B): Animals treated with the AFG5+VRC combination and VRC alone had significantly lower levels of DNA (*, P ≤ 0.05) in BAL fluid. AFG10+VRC treated rabbits showed a significant decrease of DNA in BAL fluid in comparison of that to AFG10-treated rabbits (†, P < 0.05), AFG5- and AFG10-treated rabbits significantly higher DNA concentrations in BAL in comparison to that of untreated controls (¶, P < 0.05).
BAL fluid DNA.
There also was a similarly significant decrease of the concentration of Aspergillus DNA in BAL fluid of rabbits treated with VRC alone or in combination of AFG5+VRC in comparison to that of AFG5-treated rabbits, (P < 0.05). In addition AFG10+VRC treated rabbits showed a significant decrease of DNA in BAL fluid in comparison of that to AFG10-treated rabbits (P < 0.05), On the other hand there was a significant increase of the DNA concentrations in BAL in AFG5 and AFG10-treated rabbits in comparison to that of untreated controls (Fig. 4B).
Pharmacodynamic interaction analysis.
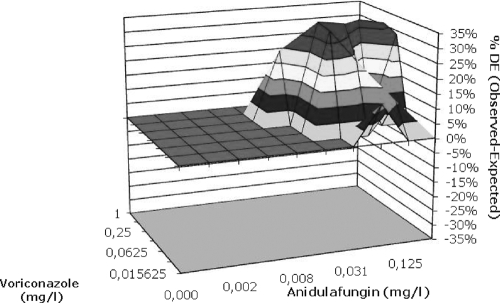
The results of Bliss independence drug interaction analysis for the in vivo pharmacodynamic interaction of voriconazole and anidulafungin are summarized in Table 1. Statistically significant Bliss synergy was found for the combination of AFG5+VRC based on residual fungal burden, pulmonary infarct scores, and pulmonary infiltrate volume (CT scan) for which the observed drug effects were 10 to 30% higher than the expected effects under the Bliss independent zero-interaction hypothesis (Table 1). Similarly, Bliss synergy was found in vitro when voriconazole was combined with anidulafungin (mean ΔE±SEM 27 ± 4%) (Fig. 5). Using the higher dosage of anidulafungin (10 mg/kg), there was Bliss independence (no synergy) based on residual fungal burden, pulmonary infarct scores, and pulmonary infiltrate volume. Moreover, Bliss antagonism was found based on BAL fluid DNA, GMI, and serum GMI (ΔE −14% to −37%) (Table 1).
TABLE 1.
Efficacies of monotherapy and combination therapy and results of Bliss independence pharmacodynamic interaction analysisa
| Biomarkerb | Efficacy of monotherapy
|
Efficacy of AFG5+VRC combination
|
Efficacy of AFG10+VRC combination
|
||||||
|---|---|---|---|---|---|---|---|---|---|
| EVRC10 | EAFG5 | EAFG10 | Observed | Expectedc | ΔE (95% confidence interval) (Bliss interaction)d | Observed | Expectedc | ΔE (95% confidence interval) (Bliss interaction)d | |
| RFB | 22 ± 9 | 8 ± 3 | 22 ± 11 | 51 ± 10 | 28 ± 5 | 23 (40-5)* (S) | 45 ± 14 | 40 ± 5 | 6 (20-−10) (I) |
| PIL | 44 ± 13 | 27 ± 12 | 30 ± 11 | 85 ± 7 | 59 ± 8 | 25 (42-8)** (S) | 73 ± 7 | 61 ± 7 | 13 (29-−3) (I) |
| LW | 48 ± 11 | 24 ± 13 | 26 ± 10 | 64 ± 6 | 60 ± 6 | 4 (18-−11) (I) | 50 ± 9 | 62 ± 5 | −12 (4-−28) (I) |
| BAL GMI | 30 ± 13 | 4 ± 1 | 0 ± 1 | 41 ± 14 | 33 ± 5 | 8 (45-−29) (I) | 8 ± 9 | 29 ± 5 | −21 (2-−44)* (A) |
| BAL DNA | 65 ± 13 | 7 ± 7 | 0 ± 4 | 76 ± 16 | 69 ± 4 | 6 (48-−35) (I) | 29 ± 7 | 67 ± 5 | −37 (−19-−55)*** (A) |
| Serum GMI | 62 ± 9 | 8 ± 6 | 8 ± 3 | 58 ± 12 | 65 ± 7 | −7 (20-−38) (I) | 47 ± 5 | 61 ± 4 | −14 (−5-−27)* (A) |
| CT scan | 66 ± 3 | 45 ± 1 | 45 ± 1 | 91 ± 5 | 81 ± 4 | 10 (1-19)* (S) | 85 ± 4 | 81 ± 4 | 4 (12-−4) (I) |
Data are mean ± SE % reductions compared to the control group.
RFB, residual fungal burden in lungs; PIL, pulmonary infarct lesions; LW, lung weight; BAL GMI, galactomannan index in BAL fluid; BAL DNA, Aspergillus DNA in BAL fluid; serum GMI, kinetics of galactomannan index in serum; CT scan, kinetics of lung lesion volumes.
Averages and SE for independent effects EEXP5 + 10 and EEXP10 + 10 were derived by using all possible combinations of the monotherapy data for each of the VRC- and AFG5- or AFG10-treated animals, respectively.
A, Bliss antagonism; I, Bliss independence; S, Bliss synergy; *, P < 0.05; ***, P < 0.001.
FIG. 5.
Interaction surfaces obtained from response surface analysis of Bliss independence drug interaction model for the in vitro combination of anidulafungin and voriconazole against A. fumigatus, with 48 h of incubation. The X- and Y- axis are the concentrations of anidulafungin and voriconazole, respectively. The Z- axis is the ΔE in %. The 0-plane represent Bliss independent interactions whereas the volumes above the 0-plane represent statistically significantly synergistic (positive ΔE) interactions. The magnitude of interactions is directly related to ΔE. The different tones in the three dimensional plots represent different percentile bands of synergy. The mean ΔE±SEM and sum ΔE were 27 ± 4% and 334%, respectively, after 48 h.
Pharmacokinetic analysis.
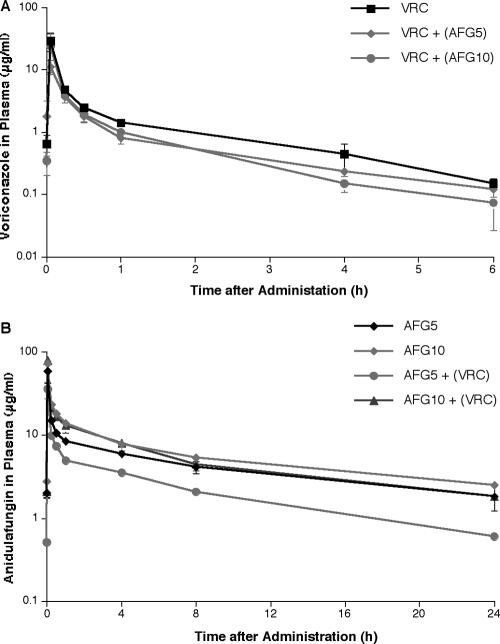
The observed plasma concentration-versus-time profiles of anidulafungin and voriconazole following administration of either compound alone and in combination with each other are depicted in Fig. 6. The corresponding pharmacokinetic parameters are tabulated in Table 2.
FIG. 6.
Plasma concentration profiles of voriconazole and voriconazole+anidulafungin (A), anidulafungin and anidulafungin+voriconazole (B), after multiple intravenous daily doses. All values represent the means ± standard errors of the mean.
TABLE 2.
Pharmacokinetic parameters for anidulafungin and voriconazole in rabbits with invasive pulmonary aspergillosis treated with either compound alone or in combinationa
| Drug and treatment regimen | Vc (liters)b | Kcp (h−1) | Kpc (h−1) | SCL (liters/h)c | AUC0-24 (mg·h/liter)f |
|---|---|---|---|---|---|
| Anidulafungin at 5 mg/kg | |||||
| Monotherapy | 0.85 (0.38) | 1.58 (1.49) | 0.68 (0.27) | 0.16 (0.06) | 96.1 (39.07)d |
| Combination | 0.94 (0.41) | 3.22 (2.65) | 1.55 (0.83) | 0.40 (0.10) | 38.1 (9.47) |
| Anidulafungin at 10 mg/kg | |||||
| Monotherapy | 1.02 (0.33) | 1.00 (0.31) | 0.36 (0.15) | 0.20 (0.05) | 136.29 (36.13)e |
| Combination | 1.22 (0.62) | 1.11 (0.94) | 0.48 (0.26) | 0.28 (0.17) | 121.89 (50.96) |
| Voriconazole at 10 mg/kg | |||||
| Monotherapy | 5.26 (4.44) | 1.69 (1.30) | 0.45 (0.57) | 5.40 (2.20) | 6.02 (2.52) |
| Combination at 5 mg/kg | 5.97 (2.25) | 1.93 (1.12) | 0.08 (0.03) | 8.58 (4.60) | 3.83 (1.49) |
| Combination at 10 mg/kg | 5.67 (4.28) | 1.43 (0.82) | 0.09 (0.04) | 6.19 (1.89) | 4.84 (1.60) |
Data are presented as means (SD). Vc, volume of central compartment; Kcp and Kpc, intercompartmental rate constants; SCL, clearance from central compartment.
P = 0.46 for comparison among groups for anidulafungin and 0.95 for comparison among groups for voriconazole, using ANOVA.
P = 0.003 for comparison among groups for anidulafungin and 0.15 for comparison among groups for voriconazole, using ANOVA.
P = 0.007 for monotherapy versus combination therapy at 5 mg/kg, using Student's t test.
P = 0.54 for monotherapy versus combination therapy at 10 mg/kg, using Student's t test.
P = 0.19 for comparison among groups for voriconazole, using ANOVA.
There was a significant difference in AUC0-24 h of anidulafungin in animals receiving single agent versus combination therapy, especially at 5 mg/kg (96.1 ± 39.07 to 38.1 ± 9.47, P = 0.007). On the other hand, there was no significant difference between the mean AUC0-24 h of anidulafungin at 10 mg/kg coadministered with voriconazole and that of monotherapy (P = 0.54). This interaction was mainly associated with faster clearance of anidulafungin, and lower mean trough plasma concentrations at the end of the 24 h dosing interval of anidulafungin (Table 2). Coadministration of anidulafungin was not associated with a significant change in the plasma pharmacokinetic parameters of voriconazole (Table 2). However, there was a similar trend in decreased AUC0-24 h of voriconazole from 6.02 ± 2.52 mg*h/L to 3.83 ± 1.49 mg*h/L in the animals treated with combination of AFG5+VRC.
Safety.
There were significantly lower levels of serum creatinine, urea nitrogen, ALT and AST in AFG5+VRC treated rabbits in comparison to that of AFG5 alone (P < 0.05). In addition AFG10+VRC treated rabbits had significantly lower levels of serum urea nitrogen and ALT in comparison to that of AFG10 (P < 0.05). On the other hand, there was significantly lower level of serum urea nitrogen, ALT, and AST in rabbits receiving combination therapy of AFG5+VRC in comparison to controls (P < 0.05), while combination of AFG10+VRC had significantly lower levels only of serum urea nitrogen in comparison to controls (P < 0.05) (Table 3).
TABLE 3.
Effects of anidulafungin-voriconazole combination on serum creatinine, serum urea nitrogen, serum ALT, serum AST, and potassium concentrations in persistently neutropenic rabbits with pulmonary aspergillosisa
| Treatment group (n) | Serum creatinine concn (mg/dl) | Serum urea nitrogen concn (mg/dl) | Serum ALT concn (U/liter) | Serum AST concn (U/liter) | Serum potassium concn (mmol/liter) |
|---|---|---|---|---|---|
| Controls (14) | 1.67 ± 0.57 | 33.2 ± 9.86† | 45.2 ± 13.5† | 71.4 ± 28.5† | 3.20 ± 0.21 |
| VRC (12) | 1.02 ± 0.06 | 12.8 ± 1.49 | 22.2 ± 5.52 | 26.8 ± 6.98 | 3.17 ± 0.32 |
| AFG5 (9) | 1.50 ± 0.24* | 29.8 ± 9.42* | 22.2 ± 3.65* | 34.3 ± 5.78* | 2.82 ± 0.13 |
| AFG5+VRC (10) | 0.98 ± 0.08* | 11.8 ± 1.20*† | 11.8 ± 1.40*† | 13.2 ± 3.37*† | 3.90 ± 0.08 |
| AFG10 (11) | 1.34 ± 0.25 | 22.4 ± 2.54* | 39.4 ± 7.22* | 48.3 ± 15.4 | 3.45 ± 0.22 |
| AFG10+VRC (11) | 0.94 ± 0.07 | 15.4 ± 1.86*† | 19.2 ± 3.57* | 16.0 ± 4.04 | 3.54 ± 0.35 |
All values are expressed as means ± SEM. *, for comparison between combination therapy and monotherapy, P < 0.05 (Mann-Whitney U test); †, for comparison between combination therapy and controls, P < 0.05 (Mann-Whitney U test).
DISCUSSION
This study demonstrated in vitro and in vivo concentration and dose dependent interactions between the echinocandin anidulafungin and the triazole voriconazole by Bliss independence drug interaction analysis of microbiological, radiological, and antigenic endpoints. To our knowledge, this is the first time that the potentially synergistic echinocandin-triazole interaction has been described by Bliss independence modeling. Using the panel of different outcome variables, application of Bliss independence analysis allowed us to demonstrate synergistic, independent, or antagonistic interactions of this potentially useful combination. There was a significant decrease of pulmonary infarct score, lung weight, residual fungal burden, and galactomannan antigenemia in combination with anidulafungin at 5 mg/kg/day and voriconazole, and only significant decrease of pulmonary infarct score and lung weight with anidulafungin at 10 mg/kg/day and voriconazole combination when compare to monotherapies. Notably, the magnitude of these interactions was similar for the in vitro and in vivo combination studies when analyzed by the Bliss independence drug interaction analysis.
When using voriconazole in combination with the lower dosage of anidulafungin (5 mg/kg) in combination, the results were synergistic or independent by Bliss pharmacodynamic drug interaction analysis. There also was a correlation between the synergy measured by echinocandin-triazole antifungal activity in causing hyphal damage of A. fumigatus and the synergistic interaction observed in vivo as measured by reduction of residual fungal burden (log CFU/g), improved survival, reduced galactomannan antigenemia, and decreased pulmonary injury (lung weights, infarct scores, and pulmonary infiltrate volume by CT) all of which were superior to the effects of the single agents and untreated controls.
This synergistic interaction between the echinocandin and the triazole is most likely due to simultaneous inhibition of biosynthesis of (1→3)-β-D-glucan in the fungal cell wall and ergosterol in the cell membrane. These apparently independent mechanisms of action on the cell wall and membrane would likely lead to an additive or synergistic interaction against filamentous fungi. This additive to synergistic interaction stands in contrast to the potential antagonism observed with azoles and polyenes (16, 30, 31, 35). Antifungal azoles deplete the fungal cell membrane of ergosterol and thereby diminish the principal biochemical target of amphotericin B. Both azoles and polyenes ultimately interact at the level of ergosterol and thus carry the potential for antagonism against A. fumigatus (34). However, in the setting of CNS aspergillosis where concentrations of amphotericin B are substantially lower in cerebral tissue, a different interaction may ensue to result in additive to synergistic interaction. This is exemplified by the combination therapy study of voriconazole and lipid formulations of amphotericin B in experimental murine CNS aspergillosis by Clemons et al. (2, 3). The synergistic interaction described between voriconazole and anidulafungin is likely applicable to the other combinations of the class of echinocandins and triazoles. For example, Perea and colleagues reported in vitro synergistic interactions between caspofungin and voriconazole (24). Manavathu and colleagues reported in vitro synergistic interactions between itraconazole and caspofungin, as well as between posaconazole and caspofungin (15). Patterson and colleagues described in vivo synergy between voriconazole and caspofungin in reducing the number of positive cultures in experimental disseminated aspergillosis in guinea pigs (11). In addition, we previously described in vivo synergistic interaction between ravuconazole and micafungin (26) in experimental invasive pulmonary aspergillosis in persistently neutropenic rabbits.
Our analysis demonstrates that echinocandin-triazole interactions may be concentration-dependent and dose-dependent. The higher dosage of anidulafungin (10 mg/kg) in combination with voriconazole resulted in Bliss independence and loss of the synergy observed at lower anidulafungin dosage. This loss of synergy at the higher dosage of anidulafungin (10 mg/kg) was consistent across several outcome variables, including residual fungal burden, pulmonary infarct score, and pulmonary infiltrate volume in replicate experiments. There also was antagonism as shown by BAL fluid galactomannan, DNA, and serum galactomannan levels at the higher dosage. Thus, when choosing combination therapy, one should be aware that not all doses might achieve the desired effect of synergistic interaction.
This dose dependent reduction of synergistic interaction may have several possible mechanisms. An increase of anidulafungin dosage from 5 to 10 mg/kg may cause increased cell wall injury and disruption of the tertiary structure of transmembrane proteins that otherwise would facilitate uptake of voriconazole. Alternatively, the higher dosage of anidulafungin may also result indirectly in secondary injury to the fungal cytoplasmic structures, including mitochondria, and potentially antagonize the effect of voriconazole on ergosterol biosynthesis.
At the same time, the effect of a given outcome variable should be considered when analyzing results of combination therapy. When combination therapy is not extremely superior, not all outcome variables or tests chosen to assess efficacy, can equally depict subtle differences. As evident from this study, when residual fungal burden and pulmonary lesion score were chosen for analysis using Bliss independence model, the interaction between echinocandin and triazole was synergistic. However, when lung weight and BAL fluid galactomannan index were analyzed, interaction demonstrated independence, with trends suggestive of the benefit of combination therapy. GMI and lung weight may be delayed in rapid return to normal when therapy is effective. These findings underscore the importance of studying multiple outcome variables in vivo and in clinical settings.
The dose-dependent increase in BAL DNA in Fig. 4 demonstrates that the rabbits treated with echinocandin (anidulafungin, 5 and 10 mg/kg) had paradoxically higher concentrations of DNA (log (femtograms DNA per ml)). This paradoxically increased amount of DNA may pertain to the mechanism of echinocandin where the effect of echinocandin fragments hyphal structures and contributes to an overall increase in the number of viable hyphal elements. In addition, echinocandins will inhibit germination of Aspergillus conidia, which will provide an additional source of DNA. The smaller hyphal fragments may be more readily lavaged and recovered in comparison to that of well-established hyphae invading tissue in untreated controls.
Anidulafungin dosages were selected carefully to approximate human AUC exposure. A single anidulafungin dosage of 5 mg/kg in rabbits as monotherapy conferred a mean AUC of 96.1 mg*h/L. Similarly, the phase I study of safety and pharmacokinetics of intravenous anidulafungin in children with neutropenia at high-risk for invasive fungal infections at a single dosage of 3 mg/kg conferred a mean AUC0-24 h of 89.7 mg*h/L and 1.5 mg/kg after multiple dosage yielded a mean AUCss of 99.5 mg*h/L. The plasma exposure is comparable to that achieved by the standard 100 mg adult dose in steady state. As the plasma pharmocokinetics appear to be linear, a dosage of 10 mg/kg in rabbits would be equivalent to a dosage of 6 mg/kg in pediatric patients or a 200 mg adult dose.
Given the life-threatening nature of invasive pulmonary aspergillosis in neutropenic and other immunocompromised hosts, the critical question arises as to whether a higher dosage of echinocandin further enhances the antifungal activity of the triazole echinocandin combination. Therefore, we tested whether a doubling of the standard dosage equivalent was beneficial. The doubling of the dosage led to an increase in mean AUC of 136 mg*h/L. Thus, the dosage selected in these experiments span the potential range of treatment of human fungal disease. Higher dosages would have little clinical relevance.
Thus, an increase in AUC beyond the approved equivalent dosage did not confer increased benefit. Additional studies exploring the lower ranges of anidulafungin may further elucidate the synergistic interactions; however, as these lower dosages would likely be below those of the approved therapeutic doses, these studies are beyond the scope of the current study.
The pharmacokinetic profiles of anidulafungin and voriconazole changed during combination therapy. These differences are unlikely to be related to direct drug interactions. Dowell et al. demonstrated that the pharmacokinetics of anidulafungin and voriconazole were not affected by coadministration in normal human volunteers (5). The exposure of anidulafungin in normal rabbits, as described by Groll and colleagues (7), is similar to that of rabbits treated with combination therapy AFG5+VRC, which also was the more effective antifungal regimen. Animals treated with the less active single agent AFG5 had higher circulating concentrations. A reasonable hypothesis, by which to explain these observations, is that rabbits with more advanced aspergillosis (those receiving monotherapy) had smaller circulating blood volume (related to insensible loss) and thus increased serum concentrations. Rabbits with more effectively treated aspergillosis had plasma AUCs comparable to those of noninfected rabbits. Similar trends of higher voriconazole exposures also were observed in single agent treatment versus combination therapy, although these differences did not achieve statistical significance.
That rabbits receiving the combination of AFG5+VRC physiologically approached the status of noninfected animals also can be observed in Table 3. Rabbits in the AFG5+VRC group had lower values of serum creatinine, urea nitrogen, ALT, and AST, as well as higher serum potassium in comparison to all other groups, particularly those in the AFG5 and AFG10. Thus, the improved efficacy of AFG5+VRC in treatment of invasive pulmonary aspergillosis correlates with improved renal and hepatic function.
Results from this study and those of other laboratories demonstrate the complexity and potential benefit of synergistic echinocandin-triazole interactions. These in vitro and in vivo studies may help guide the design and interpretation of echinocandin-triazole clinical trials in treatment of invasive pulmonary aspergillosis.
Footnotes
Published ahead of print on 23 March 2009.
REFERENCES
- 1.Anaissie, E. 1992. Opportunistic mycoses in the immunocompromised host: experience at a cancer center and review. Clin. Infect. Dis. 14(Suppl. 1):S43-S53. [DOI] [PubMed] [Google Scholar]
- 2.Clemons, K. V., M. Espiritu, R. Parmar, and D. A. Stevens. 2005. Comparative efficacies of conventional amphotericin B, liposomal amphotericin B (AmBisome), caspofungin, micafungin, and voriconazole alone and in combination against experimental murine central nervous system aspergillosis. Antimicrob. Agents Chemother. 49:4867-4875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Clemons, K. V., R. Parmar, M. Martinez, and D. A. Stevens. 2006. Efficacy of Abelcet alone, or in combination therapy, against experimental central nervous system aspergillosis. J. Antimicrob. Chemother. 58:466-469. [DOI] [PubMed] [Google Scholar]
- 4.Denning, D. W. 2001. Chronic forms of pulmonary aspergillosis. Clin. Microbiol. Infect. 7(Suppl. 2):25-31. [DOI] [PubMed] [Google Scholar]
- 5.Dowell, J. A., J. Schranz, A. Baruch, and G. Foster. 2005. Safety and pharmacokinetics of coadministered voriconazole and anidulafungin. J. Clin. Pharmacol. 45:1373-1382. [DOI] [PubMed] [Google Scholar]
- 6.Georgopapadakou, N. H. 2001. Update on antifungals targeted to the cell wall: focus on beta-1,3-glucan synthase inhibitors. Expert Opin. Investig. Drugs 10:269-280. [DOI] [PubMed] [Google Scholar]
- 7.Groll, A. H., D. Mickiene, R. Petraitiene, V. Petraitis, C. A. Lyman, J. S. Bacher, S. C. Piscitelli, and T. J. Walsh. 2001. Pharmacokinetic and pharmacodynamic modeling of anidulafungin (LY303366): reappraisal of its efficacy in neutropenic animal models of opportunistic mycoses using optimal plasma sampling. Antimicrob. Agents Chemother. 45:2845-2855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Groll, A. H., P. M. Shah, C. Mentzel, M. Schneider, G. Just-Nuebling, and K. Huebner. 1996. Trends in the postmortem epidemiology of invasive fungal infections at a university hospital. J. Infect. 33:23-32. [DOI] [PubMed] [Google Scholar]
- 9.Hope, W. W., and D. W. Denning. 2004. Invasive aspergillosis: current and future challenges in diagnosis and therapy. Clin. Microbiol. Infect. 10:2-4. [DOI] [PubMed] [Google Scholar]
- 10.Johnson, M. D., C. MacDougall, L. Ostrosky-Zeichner, J. R. Perfect, and J. H. Rex. 2004. Combination antifungal therapy. Antimicrob. Agents Chemother. 48:693-715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kirkpatrick, W. R., S. Perea, B. J. Coco, and T. F. Patterson. 2002. Efficacy of caspofungin alone and in combination with voriconazole in a guinea pig model of invasive aspergillosis. Antimicrob. Agents Chemother. 46:2564-2568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kurtz, M. B., I. B. Heath, J. Marrinan, S. Dreikorn, J. Onishi, and C. Douglas. 1994. Morphological effects of lipopeptides against Aspergillus fumigatus correlate with activities against (1,3)-beta-d-glucan synthase. Antimicrob. Agents Chemother. 38:1480-1489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Latge, J. P. 1999. Aspergillus fumigatus and aspergillosis. Clin. Microbiol. Rev. 12:310-350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Leary, R., R. Jelliffe, A. Schumitzky, and M. van Guilder. 2001. An adaptive grid, nonparametric approach to pharmacokinetic and dynamic (PK/PD) models, p. 389-394. In Proceedings of the Fourteenth IEEE Symposium on Computer Based Medical Systems. IEEE Computer Society, Bethesda, MD.
- 15.Manavathu, E. K., G. J. Alangaden, and P. H. Chandrasekar. 2003. Differential activity of triazoles in two-drug combinations with the echinocandin caspofungin against Aspergillus fumigatus. J. Antimicrob. Chemother. 51:1423-1425. [DOI] [PubMed] [Google Scholar]
- 16.Meletiadis, J., V. Petraitis, R. Petraitiene, P. Lin, T. Stergiopoulou, A. M. Kelaher, T. Sein, R. L. Schaufele, J. Bacher, and T. J. Walsh. 2006. Triazole-polyene antagonism in experimental invasive pulmonary aspergillosis: in vitro and in vivo correlation. J. Infect. Dis. 194:1008-1018. [DOI] [PubMed] [Google Scholar]
- 17.Murphy, M., E. M. Bernard, T. Ishimaru, and D. Armstrong. 1997. Activity of voriconazole (UK-109,496) against clinical isolates of Aspergillus species and its effectiveness in an experimental model of invasive pulmonary aspergillosis. Antimicrob. Agents Chemother. 41:696-698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.National Committee for Clinical Laboratory Standards. 2002. Reference method for broth dilution antifungal susceptibility testing of filamentous fungi. Approved standard M38-A. NCCLS, Wayne, PA.
- 19.National Research Council. 1996. Guide for the care and use of laboratory animals. National Academy Press, Washington, DC.
- 20.O'Sullivan, C. E., M. Kasai, A. Francesconi, V. Petraitis, R. Petraitiene, A. M. Kelaher, A. A. Sarafandi, and T. J. Walsh. 2003. Development and validation of a quantitative real-time PCR assay using fluorescence resonance energy transfer technology for detection of Aspergillus fumigatus in experimental invasive pulmonary aspergillosis. J. Clin. Microbiol. 41:5676-5682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Pannuti, C., R. Gingrich, M. A. Pfaller, C. Kao, and R. P. Wenzel. 1992. Nosocomial pneumonia in patients having bone marrow transplant. Attributable mortality and risk factors. Cancer 69:2653-2662. [DOI] [PubMed] [Google Scholar]
- 22.Patterson, T. F., W. R. Kirkpatrick, M. White, J. W. Hiemenz, J. R. Wingard, B. Dupont, M. G. Rinaldi, D. A. Stevens, J. R. Graybill, et al. 2000. Invasive aspergillosis. Disease spectrum, treatment practices, and outcomes. Medicine (Baltimore) 79:250-260. [DOI] [PubMed] [Google Scholar]
- 23.Pennick, G. J., M. Clark, D. A. Sutton, and M. G. Rinaldi. 2003. Development and validation of a high-performance liquid chromatography assay for voriconazole. Antimicrob. Agents Chemother. 47:2348-2350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Perea, S., G. Gonzalez, A. W. Fothergill, W. R. Kirkpatrick, M. G. Rinaldi, and T. F. Patterson. 2002. In vitro interaction of caspofungin acetate with voriconazole against clinical isolates of Aspergillus spp. Antimicrob. Agents Chemother. 46:3039-3041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Petraitiene, R., V. Petraitis, A. H. Groll, T. Sein, S. Piscitelli, M. Candelario, A. Field-Ridley, N. Avila, J. Bacher, and T. J. Walsh. 2001. Antifungal activity and pharmacokinetics of posaconazole (SCH 56592) in treatment and prevention of experimental invasive pulmonary aspergillosis: correlation with galactomannan antigenemia. Antimicrob. Agents Chemother. 45:857-869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Petraitis, V., R. Petraitiene, A. A. Sarafandi, A. M. Kelaher, C. A. Lyman, H. E. Casler, T. Sein, A. H. Groll, J. Bacher, N. A. Avila, and T. J. Walsh. 2003. Combination therapy in treatment of experimental pulmonary aspergillosis: synergistic interaction between an antifungal triazole and an echinocandin. J. Infect. Dis. 187:1834-1843. [DOI] [PubMed] [Google Scholar]
- 27.Petraitis, V., R. Petraitiene, J. Solomon, A. M. Kelaher, H. A. Murray, C. Mya-San, A. K. Bhandary, T. Sein, N. A. Avila, A. Basevicius, J. Bacher, and T. J. Walsh. 2006. Multidimensional volumetric imaging of pulmonary infiltrates for measuring therapeutic response to antifungal therapy in experimental invasive pulmonary aspergillosis. Antimicrob. Agents Chemother. 50:1510-1517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Pfaller, M. A., S. A. Messer, R. J. Hollis, and R. N. Jones. 2002. Antifungal activities of posaconazole, ravuconazole, and voriconazole compared to those of itraconazole and amphotericin B against 239 clinical isolates of Aspergillus spp. and other filamentous fungi: report from SENTRY Antimicrobial Surveillance Program, 2000. Antimicrob. Agents Chemother. 46:1032-1037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sambatakou, H., B. Dupont, H. Lode, and D. W. Denning. 2006. Voriconazole treatment for subacute invasive and chronic pulmonary aspergillosis. Am. J. Med. 119:527.e17-527.e24. [DOI] [PubMed] [Google Scholar]
- 30.Schaffner, A., and A. Bohler. 1993. Amphotericin B refractory aspergillosis after itraconazole: evidence for significant antagonism. Mycoses 36:421-424. [DOI] [PubMed] [Google Scholar]
- 31.Schaffner, A., and P. G. Frick. 1985. The effect of ketoconazole on amphotericin B in a model of disseminated aspergillosis. J. Infect. Dis. 151:902-910. [DOI] [PubMed] [Google Scholar]
- 32.Segal, B. H., N. G. Almyroudis, M. Battiwalla, R. Herbrecht, J. R. Perfect, T. J. Walsh, and J. R. Wingard. 2007. Prevention and early treatment of invasive fungal infection in patients with cancer and neutropenia and in stem cell transplant recipients in the era of newer broad-spectrum antifungal agents and diagnostic adjuncts. Clin. Infect. Dis. 44:402-409. [DOI] [PubMed] [Google Scholar]
- 33.Stynen, D., J. Sarfati, A. Goris, M. C. Prevost, M. Lesourd, H. Kamphuis, V. Darras, and J. P. Latge. 1992. Rat monoclonal antibodies against Aspergillus galactomannan. Infect. Immun. 60:2237-2245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Sugar, A. M. 1995. Use of amphotericin B with azole antifungal drugs: what are we doing? Antimicrob. Agents Chemother. 39:1907-1912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Sugar, A. M., and X. P. Liu. 1998. Interactions of itraconazole with amphotericin B in the treatment of murine invasive candidiasis. J. Infect. Dis. 177:1660-1663. [DOI] [PubMed] [Google Scholar]
- 36.Wald, A., W. Leisenring, J. A. van Burik, and R. A. Bowden. 1997. Epidemiology of Aspergillus infections in a large cohort of patients undergoing bone marrow transplantation. J. Infect. Dis. 175:1459-1466. [DOI] [PubMed] [Google Scholar]
- 37.Walsh, T. J., J. Bacher, and P. A. Pizzo. 1988. Chronic silastic central venous catheterization for induction, maintenance and support of persistent granulocytopenia in rabbits. Lab. Anim. Sci. 38:467-471. [PubMed] [Google Scholar]
- 38.Walsh, T. J., K. Garrett, E. Feurerstein, M. Girton, M. Allende, J. Bacher, A. Francesconi, R. Schaufele, and P. A. Pizzo. 1995. Therapeutic monitoring of experimental invasive pulmonary aspergillosis by ultrafast computerized tomography, a novel, noninvasive method for measuring responses to antifungal therapy. Antimicrob. Agents Chemother. 39:1065-1069. [DOI] [PMC free article] [PubMed] [Google Scholar]