Abstract
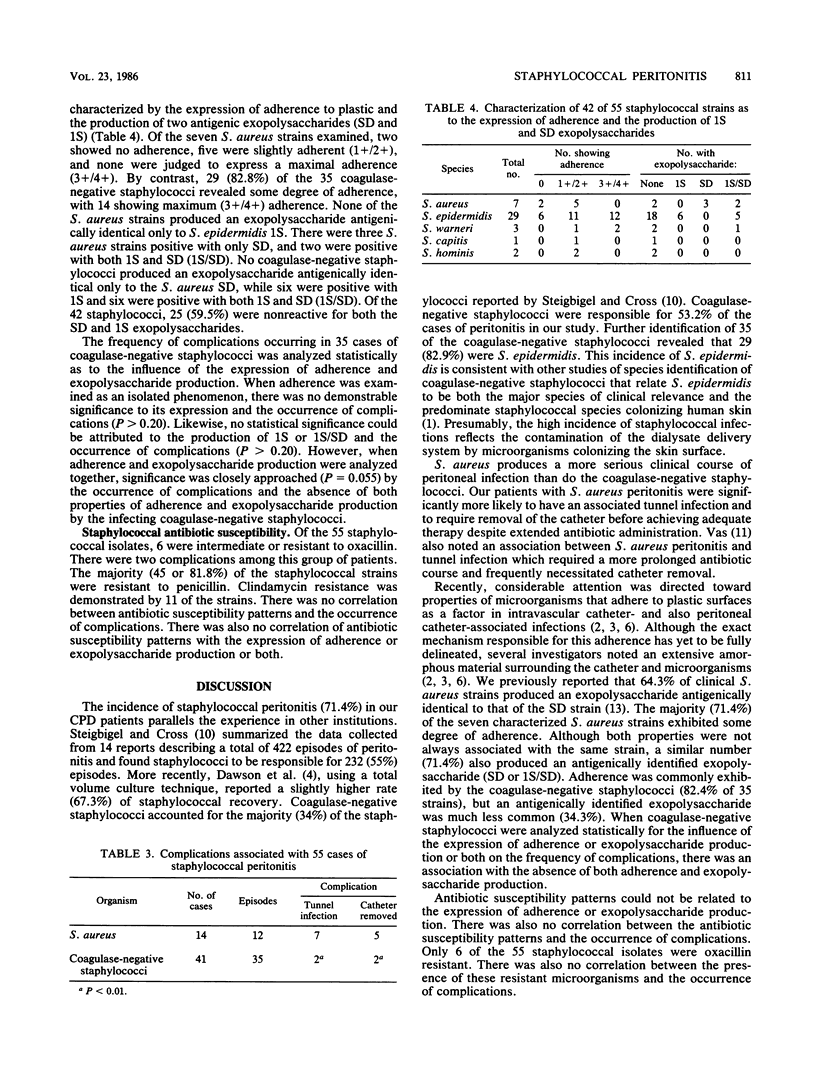
During 1984, 35 patients undergoing continuous peritoneal dialysis experienced 77 cases of peritonitis with 55 cases (71.4%) related to staphylococci. Coagulase-negative staphylococci were isolated in 41 cases, while Staphylococcus aureus was found in 14. A coexisting tunnel infection was more often associated with S. aureus (7/14) than with coagulase-negative staphylococci (2/41) (P less than 0.01). Likewise, eradication of the infection necessitated catheter removal more frequently with S. aureus (5/14) than with coagulase-negative staphylococci (2/41) (P less than 0.01). Of the 41 coagulase-negative staphylococci, 35 were characterized as to species, adherence, and production of two exopolysaccharides. Staphylococcus epidermidis was the most frequent coagulase-negative species (29/35). Peritonitis cases caused by coagulase-negative staphylococci that lacked adherence and exopolysaccharides were more frequently associated with complications (4/6) than were those organisms with either or both properties of adherence or exopolysaccharide production (5/29). There were no appreciable differences in antibiotic susceptibilities. Staphylococcal peritonitis remains a significant cause of morbidity in continuous peritoneal dialysis patients. The incidence of complications was not directly linked to staphylococcal properties of adherence or exopolysaccharide production.
Full text
PDF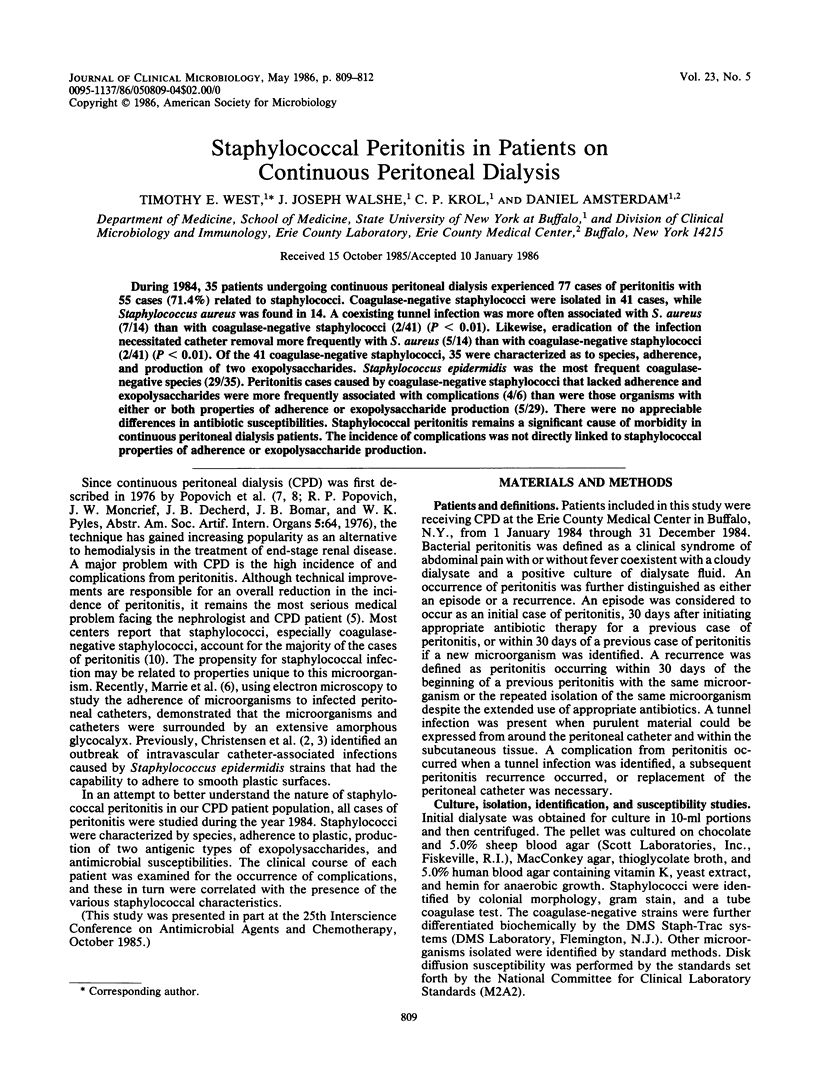


Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Christensen G. D., Bisno A. L., Parisi J. T., McLaughlin B., Hester M. G., Luther R. W. Nosocomial septicemia due to multiply antibiotic-resistant Staphylococcus epidermidis. Ann Intern Med. 1982 Jan;96(1):1–10. doi: 10.7326/0003-4819-96-1-1. [DOI] [PubMed] [Google Scholar]
- Christensen G. D., Simpson W. A., Bisno A. L., Beachey E. H. Adherence of slime-producing strains of Staphylococcus epidermidis to smooth surfaces. Infect Immun. 1982 Jul;37(1):318–326. doi: 10.1128/iai.37.1.318-326.1982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dawson M. S., Harford A. M., Garner B. K., Sica D. A., Landwehr D. M., Dalton H. P. Total volume culture technique for the isolation of microorganisms from continuous ambulatory peritoneal dialysis patients with peritonitis. J Clin Microbiol. 1985 Sep;22(3):391–394. doi: 10.1128/jcm.22.3.391-394.1985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harrington J. T. Chronic ambulatory peritoneal dialysis. N Engl J Med. 1982 Mar 18;306(11):670–671. doi: 10.1056/NEJM198203183061110. [DOI] [PubMed] [Google Scholar]
- Marrie T. J., Noble M. A., Costerton J. W. Examination of the morphology of bacteria adhering to peritoneal dialysis catheters by scanning and transmission electron microscopy. J Clin Microbiol. 1983 Dec;18(6):1388–1398. doi: 10.1128/jcm.18.6.1388-1398.1983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Popovich R. P., Moncrief J. W., Nolph K. D., Ghods A. J., Twardowski Z. J., Pyle W. K. Continuous ambulatory peritoneal dialysis. Ann Intern Med. 1978 Apr;88(4):449–456. doi: 10.7326/0003-4819-88-4-449. [DOI] [PubMed] [Google Scholar]
- SMITH J. M., DUBOS R. J. The behavior of virulent and avirulent staphylococci in the tissues of normal mice. J Exp Med. 1956 Jan 1;103(1):87–108. doi: 10.1084/jem.103.1.87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- West T. E., Apicella M. A. Detection of encapsulation in Staphylococcus aureus by use of antiserum agar. J Clin Microbiol. 1984 Aug;20(2):141–144. doi: 10.1128/jcm.20.2.141-144.1984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- West T. E., West M. E., Mylotte J. M. Antiserum agar method for identification of Smith type exopolysaccharides in clinical isolates of Staphylococcus aureus. J Clin Microbiol. 1985 Apr;21(4):490–492. doi: 10.1128/jcm.21.4.490-492.1985. [DOI] [PMC free article] [PubMed] [Google Scholar]


