Abstract
Introduction:
The relationship between attention-deficit/hyperactivity disorder (ADHD) and sleep is a complex one which poses many challenges in clinical practice.
Methods:
Studies of sleep disturbances in children with academic and behavioral problems have underscored the role that primary sleep disorders play in the clinical presentation of symptoms of inattention and behavioral dysregulation. In addition, recent research has shed further light on the prevalence, type, risk factors for, and impact of sleep disturbances in children with ADHD.
Results:
The following discussion of the multi-level and bi-directional relationships among sleep, neurobehavioral functioning, and the clinical syndrome of ADHD synthesizes current knowledge about the interaction of sleep and attention/arousal in these children.
Conclusion:
Guidelines are provided, outlining a clinical approach to evaluation and management of children with ADHD and sleep problems.
Keywords: sleep, attention deficit hyperactivity disorder, sleep disorders
Résumé
Introduction:
La relation qui existe entre le trouble du déficit d’attention avec hyperactivité (TDAH) et le sommeil est complexe et pose de nombreux défis aux cliniciens.
Méthodologie:
Les études sur les troubles du sommeil chez les enfants qui ont des difficultés scolaires et comportementales sous-estiment le rôle que ces troubles jouent dans les symptômes cliniques de l’inattention et du dérèglement comportemental. En outre, les récents travaux de recherche expliquent mieux la prévalence, le type, les facteurs de risque et l’impact des troubles du sommeil sur les enfants souffrant de TDAH.
Résultats:
La discussion sur les relations bidirectionnelles et les divers niveaux qui existent entre le sommeil, le fonctionnement neurocomportemental et le syndrome clinique du TDAH fera la synthèse des connaissances actuelles sur l’interaction sommeil-attention/éveil chez ces enfants.
Conclusion:
Les directives présentent l’approche clinique qui permet d’évaluer les enfants atteints de TDAH et de gérer leurs problèmes de sommeil.
Keywords: sommeil, trouble du déficit d’attention avec hyperactivité, troubles du sommeil
Introduction
Sleep problems, particularly difficulty initiating and maintaining sleep, are frequently reported in children and adolescents with ADHD in mental health practice settings (Owens, 2005a). In fact, the 3rd Edition of the Diagnostic and Statistical Manual of Mental Disorders listed restless sleep as a diagnostic criterion for ADHD, although this criterion was eliminated from subsequent DSM editions. However, the relationship between sleep problems and ADHD is hardly a straightforward one, and may present clinically in a number of different guises. For example, psychotropic medications used to treat ADHD or comorbid psychiatric conditions associated with ADHD (i.e., mood disorders, anxiety) may themselves result in sleep problems in some patients, daytime manifestations of primary sleep disorders such as obstructive sleep apnea may “mimic” ADHD symptomatology in others, comorbid sleep problems may exacerbate ADHD symptoms, and/or sleep problems may in some cases represent an “intrinsic” dysregulation of sleep and wakefulness associated with ADHD-related CNS dysfunction. Thus, from a clinical standpoint, sleep difficulties in children with ADHD not only potentially have a direct negative impact on the nature and severity of daytime ADHD symptoms as well as the quality of life for these patients (Sung, Hiscock, Sciberras, & Efron, 2008), but they present a considerable challenge for the clinician in elucidating the nature and etiology of the sleep problems and in developing effective treatment strategies.
Although a detailed discussion of the neurophysiologic mechanisms and neuroanatomical pathways underlying the relationships among sleep, alertness, attention, and arousal is beyond the scope of this brief review, it is important for the clinician to have some basic understanding of the neurobiology involved. From a theoretical perspective, there is substantial empirical evidence supporting an overlap in those central nervous system centers that regulate sleep and those that regulate attention/arousal, suggesting disruptions in one system might well have parallel effects on the other. Furthermore, similar perturbations in neurotransmitter pathways, particularly noradrenergic and dopaminergic systems, are found in both ADHD and sleep disturbances (Biederman & Spencer, 1999; Dahl, 1996). The framework for the common underlying CNS pathology linking sleep disruption/deprivation and ADHD primarily involves the prefrontal cortex (PFC) and associated integrative functions (Horne, 1993). For example, a number of functional neuroimaging studies have demonstrated similar metabolic changes in the prefrontal cortex in ADHD (Lee et al., 2005; Sowell et al., 2003) and sleep deprivation (Chee & Chuah, 2008), and other studies in adults have documented the effects on neuropsychological performance measures of PFC function, resulting in impairments in attention, working memory, and other executive functions, as well as behavioral disinhibition. A potential role for a primary circadian disruption in ADHD has also been proposed, which may involve alterations in the normal timing and pattern of melatonin secretion or responsiveness to environmental cues such as light (van der Heijden, Smits, van Someren, & Gunning, 2005). Finally, the few studies which have examined the issue of arousal level and daytime sleepiness in children with ADHD (Golan, Shahar, Ravid, & Pillar, 2004; Lecendreux, Konofal, Bouvard, Falissard, & Mouren-Simeoni, 2000), have reported that children with ADHD demonstrate an increase in objectively-measured sleep propensity compared to control children, suggesting that hyperactivity, at least in some children, may be an adaptive behavior that counteracts the effects of hypoarousal and underlying daytime sleepiness.
Despite these common neuroanatomical/neurophysiologic pathways and clinical observations which support a high prevalence of sleep problems in children with ADHD, studies attempting to systematically examine differences in sleep in these children compared to typically-developing controls do not consistently support an increase in sleep problems, nor do they demonstrate reliable differences in sleep architecture and/or sleep patterns (Corkum, Tannock, & Moldofsky, 1998). In order to examine these apparent discrepancies, it is important to make a distinction between studies which have examined attention and behavioral problems in children with primary sleep disorders and vice versa, and those studies which have addressed the issue of sleep and sleep problems in children with ADHD compared to controls. The former body of literature addresses the overlap in symptomatology between presumably separate clinical entities, i.e., the daytime manifestations of sleep disturbances and ADHD, while the latter group of studies have largely examined the question of intrinsic “differences” in the sleep of children with ADHD.
Primary Sleep Disorders and ADHD Symptoms
Clinical experience, as well as empirical evidence from numerous studies and case reports, have demonstrated that childhood sleep disorders that are primarily medical in etiology, such as obstructive sleep apnea (OSA), restless legs syndrome (RLS), and Delayed Sleep Phase Disorder, and those that are related to behavioral or environmental factors, such as behavioral insomnia of childhood and voluntary sleep curtailment, may present primarily with daytime sleepiness and neurobehavioral symptoms, many of which overlap with the cardinal symptoms of ADHD. These observational and treatment studies have demonstrated that insufficient and poor quality sleep related to primary sleep disorders result in daytime sleepiness and behavioral/mood dysregulation, and impact on neurocognitive functions in children. The two primary sleep disorders about which there exists the most empirical evidence (OSA and RLS/periodic limb movement disorder PLMD) regarding impact on daytime functioning are discussed below.
Sleep disordered breathing (SDB) in childhood includes a spectrum of disorders that vary in severity, ranging from OSA at one end to primary snoring (snoring without behaviour abnormalities) at the other, and in prevalence, from 10% in habitual snoring to 1–3% in OSA (Schecter, 2002). Common manifestations of SDB in childhood include loud, nightly snoring, choking/gasping arousals, and increased work of breathing characterized by nocturnal diaphoresis, paradoxical chest and abdominal wall movements, and restless sleep. Risk factors include adenotonsillar hypertrophy, obesity, allergies/asthma, hypotonia, congenital syndromes (achondroplasia, Down syndrome), race (e.g., African-American), and family history of SDB (Redline, Tischler, Schluchter, Clark, & Graham, 1999). Although repeated intermittent nocturnal episodes of hypoxia leading to systemic inflammatory changes most likely comprise an important etiologic factor for neurobehavioral deficits in OSA, sleep fragmentation resulting from frequent nocturnal arousals, which in turn leads to the daytime sleepiness, is also felt to play a key role.
A large number of pediatric studies have now been published which provide compelling evidence of a wide range of neurobehavioral and neurocognitive deficits in children with both clinical symptoms of and polysomnographically-confirmed SDB, including inattention, impaired memory, and executive functions, mood disturbance, externalizing and internalizing behavior problems, and academic difficulties (Chervin & Archbold, 2001; Chervin, Dillon, Bassetti, Ganoczy, & Pituch, 1997; Huang et al., 2007; Beebe, 2006). Several recent reports have documented a significant increase in parent-reported SDB symptoms specifically in children being evaluated for or diagnosed with ADHD, and have suggested that as many as 25% of ADHD diagnoses may be linked to symptoms of sleep-disordered breathing such as habitual snoring (Chervin & Archbold, 2001; Chervin et al., 1997); habitual snoring is also reported to be three times more common in children with ADHD (33%) than in other child psychiatric (11%) or general pediatric populations (9%) (O’Brien et al., 2003a). However, it should be pointed out that not all studies have found an association between polysomnographically (PSG)-confirmed SDB and ADHD (Sangal, Owens, & Sangal, 2005), and that furthermore, the severity of neurobehavioral and neurocognitive deficits does not appear to be “dose-dependent”, suggesting that disease severity alone does not account for the extent of impairment. Finally, studies which have looked at changes in behavior and neuropsychological functioning in children following treatment (usually adenotonsillectomy) for SDB have also largely documented significant improvement in daytime sleepiness, neuropsychological measures of impairment, behavior, and academic performance post-treatment (Wei, Mayo, Smith, Reese, & Weatherly, 2007; Gozal, 1998; Ali, Pitson, & Stradling, 1996); in one study, 50% of children initially meeting DSM-IV criteria for ADHD no longer did so one year after adenotonsillectomy (Chervin et al., 2006).
Significant neurobehavioral consequences may also occur related to RLS and PLMD, and may present as symptoms of ADHD (Picchetti & Stevens, 2008; Picchietti, & Walters, 1996; Walters et al., 2000; Cortese et al., 2005; Chervin et al., 2002). RLS is a clinical disorder characterized by the urge to move the lower extremities which is exacerbated at rest and in the evening, and is accompanied by sensory discomfort; PLM’s are rhythmic leg flexions detectable on PSG which often accompany RLS and result in sleep fragmentation. Neither are uncommon disorders; a recent study found that 2% of healthy children ages 8–17 years met “definite” RLS diagnostic criteria (Picchietti et al., 2007). Studies have further suggested that up to 44% of children with ADHD have RLS symptoms, and 26% of RLS pediatric patients have symptoms of ADHD. Although the underlying mechanism for this relationship remains unclear, some researchers have postulated that ADHD and RLS/PLMD may share a common pathophysiology involving dopamine deficiency and low iron stores. In fact, treatment of children with RLS with dopamine antagonists has been shown to result not only in improved sleep quality and quantity, but also in improvement in “ADHD” behaviors previously resistant to treatment with psychostimulants (Walters et al., 2000).
Is Sleep in Children with ADHD “Different”?
It is safe to say that most of the “objective” studies have failed to find consistent significant differences in sleep architecture and patterns between children with ADHD and controls (Cohen-Zion & Ancoli-Israel, 2004; Sadeh, Pergamin, & Bar-Haim, 2006), although some researchers have postulated that there may be more subtle changes in sleep microarchitecture (i.e., “cyclic alternating patterns”) in children with ADHD that are not captured on routine PSG scoring (Miano et al., 2006). Furthermore, actigraphy studies (using lightweight activity monitors to record sleep wake patterns across time in the home setting) have also failed to demonstrate striking, consistent differences between children with ADHD and controls on the typical actigraphic sleep parameters (sleep onset, sleep duration, sleep efficiency, night wakings); however, these studies have suggested that activity levels during sleep in children with ADHD may be greater and one study reported more night-to-night variability in sleep patterns (Gruber, Sadeh, & Raviv, 2000).
In direct contrast to studies which have utilized more objective measures, parental report studies have almost universally reported a high frequency of significant sleep problems in children with ADHD (Hvolby, 2008, Owens, 2005a; Corkum et al., 1998), which is reflected in the clinical experience of most mental health practitioners who work with these children. Parent-reported sleep problems, particularly difficulties in initiating and maintaining sleep, are reported in an estimated 25–50% of children and adolescents with ADHD in clinical practice (Corkum et al., 1998). These prevalence rates and/or levels of intensity are generally two- to three-fold that of control group children (Ring et al., 1998; Marcotte et al., 1998; O’Brien et al., 2003c); differences in the rates of sleep problems are also found within ADHD samples as a function of ADHD subtype, psychiatric comorbidities, and medication use (Mayes et al., 2008). Surveys of parents and children with ADHD also consistently report an increased prevalence of poor sleep quality, shortened sleep duration, and daytime sleepiness, compared with healthy controls, siblings, or children with other psychiatric, behavioral and learning problems. In addition, problematic “evening” behaviors during the time period preceding bedtime, such as arguing with siblings and difficulty transitioning, appear to be more common in these children (Owens et al., 2008).
A number of theories have been put forward to explain the apparent discrepancy between subjective and objective reports of sleep in children with ADHD, all of which are currently largely speculative. For example, it has been suggested that these differences may be related to the fact that parents of behaviorally-disordered children may be more likely to perceive and report high levels of both daytime and sleep-related disruptive behaviors (bedtime struggles, difficulty with morning waking) in a “negative halo effect.” In addition, both caregivers and clinicians may be relatively more vigilant about observing and eliciting evidence of sleep problems in these children, based on the perception that they are commonly present and frequently associated with medication treatment. The night-to-night variability in sleep patterns in children with ADHD may also play a role in clinical settings, in that caregivers are more likely to remember and report extremes in sleep behaviors such as prolonged sleep onset latency, even if these occur only occasionally. Finally, because the definition of what subjectively constitutes a “sleep problem” varies widely across studies, methodological issues may account for some of the discrepancies between subjective and more objective sleep findings.
Sleep Problems in ADHD: Clinical Approaches
It is clear from the above discussion that sleep problems commonly co-exist with ADHD symptoms and that the reasons for this are multi-factorial; therefore, a systematic approach is necessary to tease out the relevant contributory factors in a given clinical situation, and a treatment approach which is diagnostically-driven is paramount. The first guiding principle is that all children initially presenting with symptoms of ADHD should be routinely screened for primary or comorbid sleep disorders (i.e., OSA, RLS). This may be accomplished in the context of the clinical evaluation with the use of simple screening tools (“BEARS”) (Owens & Dalzell, 2005c) or pediatric sleep questionnaires (Owens, Spirito, & McGuinn, 2000; both measures may be accessed at www.kidzzzsleep.org; additional screening tools are available through the American Academy of Sleep Medicine website, www.aasmnet.org under Professional Development – Education – MedSleep Resources). The evaluating clinician must be familiar with both the symptoms of (e.g., snoring, leg discomfort) and risk factors (e.g., family history of OSA/RLS, adenotonsillar hypertrophy/obesity, iron deficiency) for various common sleep disorders in children.
Once potential symptoms are identified, a systematic approach to diagnosis and appropriate use of diagnostic tools should follow. In particular, sleep diaries are essential in assessing sleep patterns and sleep behaviors such as bedtime resistance and night wakings. PSG is considered the “gold standard” for the diagnosis of SDB and PLMD, and a multiple sleep latency test (MSLT) should be reserved for situations in which the documentation of pathologic sleepiness (i.e., narcolepsy) is indicated. A prudent approach would then be to treat any documented sleep disorder (i.e., adenotonsillectomy for OSA) before confirming (or rejecting) the diagnosis of ADHD and initiating treatment.
While it should be emphasized that it is vitally important for mental health practitioners to routinely screen on an ongoing basis for symptoms of primary sleep disorders (e.g., snoring, restless sleep, daytime sleepiness) in all children with emotional, behavioral, and/or cognitive deficits, including ADHD, the focus of the following discussion will be on developing an approach to sleep problems presenting in clinical practice. When faced with the common clinical scenario of sleep complaints (either caregiver or self-reported) in a child or adolescent with ADHD, the mental health practitioner needs to adopt an organized and step-wise approach to evaluation and management, as there are many potential etiologies for the same constellation of presenting complaints and thus it is imperative that treatment be diagnostically-driven.
Figure 1 illustrates an evaluation strategy for the child who presents with the most common sleep complaint reported in ADHD, bedtime refusal/resistance and/or delayed sleep onset (i.e., time to fall asleep once in bed). In younger children, these two symptoms are often indistinguishable; i.e., children who have difficulty falling asleep for a variety of reasons often exhibit protest behavior (crying, getting out of bed, calling out to parents) at bedtime. In contrast, older children and adolescents may lie in bed quietly after “lights out” and parents may not even be aware of the sleep onset difficulties; thus it is important to question the child directly as well as the caregiver about symptoms. In addition to assessing the severity (e.g., time to fall asleep), frequency (e.g., nights/week), and duration (e.g., number of months/years symptom has been present) of the presenting complaint, the following specific characteristics are important to assess:
Sleep hygiene: Many families of children with ADHD have either never developed or abandoned basic good sleep habits. These include environmental (e.g., cool temperature, low noise and ambient light levels), scheduling (e.g., regular bedtime, sleep-wake schedule), sleep practice (e.g., bedtime routine, no television viewing at bedtime), and physiologic (e.g., exercise, timing of meals, limited caffeine use) factors which promote optimal sleep. While studies have suggested that adoption of good sleep hygiene alone may be adequate to successfully treat sleep initiation problems in children with ADHD (Weiss, Wasdell, Bomben, Rea, & Freeman, 2006), at the least this is a necessary component of every treatment package.
-
Anxiety/mood symptoms: An estimated 30% of children with ADHD have a comorbid anxiety disorder and 10–30% a comorbid mood disorder. Sleep onset problems, particularly relating to bedtime fears and need for parental presence at bedtime, are common presenting complaints in children with anxiety disorders; sleep initiation complaints are common in depression. The treatment focus for sleep problems in the former case should be on the anxiety symptoms, and may involve progressive muscle relaxation, anti-anxiety agents, and/or psychotherapy. In the case of comorbid mood disorders, the use of sedating antidepressants to treat both mood and sleep symptoms may be considered, as treating the underlying mood disorder will often result in improved sleep, and the reverse is clearly true as well.
Anxiety, specifically about difficulty falling asleep, is a hallmark of primary (or “psychophysiologic”) insomnia. This type of insomnia is frequently the result of the presence of predisposing factors (such as genetic vulnerability, underlying medical or psychiatric conditions) combined with precipitating factors (such as acute stress) and perpetuating factors (e.g., poor sleep habits, caffeine use, maladaptive cognitions about sleep). In this disorder, the individual develops conditioned anxiety around difficulty falling or staying asleep, which leads to heightened physiologic and emotional arousal and further compromises the ability to sleep (Hohagen, 1996). Treatment usually involves some combination of behavioral interventions, including sleep restriction and stimulus control, psychoeducation about principles of sleep hygiene, relaxation techniques to reduce anxiety, and cognitive restructuring of maladaptive thoughts regarding sleep.
Finally, the need for parental presence at bedtime, as well as during night wakings, is the cardinal feature of the Sleep Onset Association subtype of Behavioral Insomnia of Childhood. In this disorder, the child has learned to fall asleep only under certain conditions or in the presence of specific sleep associations, such as being held or comforted by parents, and is unable to fall asleep independently, either at bedtime or following night wakings. The introduction of more appropriate sleep associations which will be readily available to the child during the night (comfort objects) in addition to positive reinforcement (e.g., rewards for remaining in bed) are often beneficial. A recent review of 52 treatment studies indicates that behavioral therapies, such as unmodified and graduated extinction, positive routines, and parent education, produce reliable and durable changes for both bedtime resistance and night wakings in children (Mindell, Kuhn, Lewin, Meltzer, & Sadeh, 2006); see Table 1 for a description of behavioral interventions.
-
ADHD symptoms in the evening/at bedtime: As noted above, children with ADHD frequently exhibit “ADHD” behaviors such as increased fidgetiness/restlessness and hyperactivity during the time leading up to or at bedtime. In the child treated with psychostimulant medication, this may be due to a direct medication effect which interferes with sleep. Studies have demonstrated an increase in subjective parental perception of severe sleep difficulties, including sleep onset delay and night wakings, in children on psychostimulants for ADHD (Corkum, Panton, Ironside, Macpherson, & Williams, 2008; Sangal et al., 2006; O’Brien et al., 2003b; Mick, Biederman, Jetton, & Faraone, 2000; Stein, 1999); however, other studies have failed to find evidence of significant sleep difficulties associated specifically with long-acting stimulant treatment after adjusting for the presence of pre-existing sleep problems (Farone et al., 2008). In addition, results of studies assessing objective measures of direct psychostimulant effects on sleep have shown less consistent effects. This scenario may be responsive to a decrease in drug dosage, as sleep-related effects of stimulants are often dose-dependent. Alternatively, ADHD symptoms may return to baseline as a result of the medication waning effect at the end of the day, or even intensify in a “rebound” effect. In the latter case, late-day supplementation with a short-acting psychostimulant may be effective. For some children, this difficulty in settling occurs independent of medication status, suggesting an “intrinsic” ADHD-related mechanism. One approach in this case would be to treat with an ADHD medication with 24 hour coverage; an alternative strategy frequently employed in clinical practice is the use of medication to reduce adrenergic tone (i.e., alpha agonists).
Finally, nighttime “ADHD” symptoms (motor restlessness), as well as symptoms associated with sensory integration deficits, may be confused with symptoms of RLS. The key characteristics differentiating RLS from ADHD include the “urge” to move, symptoms specific to the lower extremities, and the sensory component of leg discomfort. Children with sensory integration deficits typically have additional symptoms, such as hypersensitivity to tactile (e.g., tags, seams) and auditory stimuli. Additional clinical clues suggestive of RLS include a family history of RLS and iron deficiency anemia (i.e., low serum ferritin level <50 mcg/ml).
Timing of sleep onset relative to bedtime: It is first important to establish that the current bedtime is developmentally appropriate; occasionally, parents will attempt to put a child to bed earlier in an effort to reduce sleep onset delay. More frequently, there is a “mismatch” between the child’s and the caregiver’s “preferred” bedtime. Older children, and particularly adolescents, who fall asleep easily at a later bedtime (and adopt this later bedtime, as well as a later waketime, on weekends and during school vacations) may have a circadian-based phase delay. Several studies have suggested that this is a common phenomenon in children with ADHD, as evidenced by a delayed onset of nocturnal melatonin secretion in these children compared to controls. Furthermore, these studies have shown that supplementation with exogenous melatonin in these children results in significant improvements in sleep onset delay (van der Heijden, Smits, van Someren, Ridderinkhof, & Gunning, 2007; Weiss et al., 2006).
Degree and persistence of bedtime resistance: As noted above, bedtime resistance in the younger child may be largely a behavioral reaction to difficulty falling asleep at the proscribed time. In families in which limit setting is particularly problematic, this bedtime behavior may be a corollary of the caregivers’ inability or resistance to setting limits in general; in this situation, parents may need assistance in developing and implementing appropriate bedtime schedules, rules, and routines. Children with ADHD and disruptive behavior disorders (ODD/CD) may be particularly prone to develop bedtime conflicts. Problems with limit setting generally respond to some combination of decreased parental attention for bedtime-delaying behavior, establishment of a consistent bedtime routine that does not include stimulating activities such as television viewing, bedtime fading (temporarily setting bedtime to the current sleep onset time and then gradually advancing bedtime), and positive reinforcement (e.g., sticker charts) for appropriate behavior at bedtime.
Figure 1:
Sleep and ADHD: Bedtime Resistance/Prolonged Sleep Onset
Table 1:
Behavioral Interventions for Sleep Problems in Children and Adolescents
|
Finally, it should be noted that the role of medication in the treatment of sleep problems in children with ADHD is controversial; although there are no medications currently approved in the United States for treatment of pediatric insomnia, studies have suggested that the use of hypnotic/sedating medications in children with ADHD, both by community-based pediatric and child psychiatry practitioners, is quite common (Owens, Rosen, & Mindell, 2003). However, the rationale for the use of specific medications is much less clear. In order to assess the potentially appropriate role of medication, the clinical emphasis must first and foremost be on elucidating the specific etiology of the sleep problem in the individual ADHD patient, as described above. As an adjunct to behavioral intervention, in cases of severe insomnia, or in that subgroup of ADHD children for whom sleep problems appear to be “intrinsic” and not apparently attributable to other modifiable factors, medication may be an appropriate intervention. The focus in making medication decisions should be on choosing the most appropriate drug for the underlying condition (i.e., melatonin for delayed sleep phase, iron supplementation or dopamine agonists for RLS, sedating antidepressants for children with comorbid mood disorders, antihistamines, benzodiazepine receptor agonists, or melatonin receptor agonists for primary insomnia), safety profile, duration of action (short-acting medications for sleep onset problems; longer-acting medications for sleep maintenance), possible interaction with current psychotropic medications, and potential exacerbation of sleep disorders by psychotropic medication (i.e., SSRIs and TCAs may exacerbate RLS/PLMD) (Owens et al., 2005b).
Conclusions
Sleep problems in children and adolescents with ADHD are challenging from a diagnostic and therapeutic standpoint, but elucidation and successful management of sleep issues in these patients may result in considerable mitigation of daytime neurobehavioral symptoms. All children presenting with ADHD symptoms should be systematically screened for primary sleep disorders (Mindell & Owens, 2003). The relative contributions of psychotropic medication, comorbid psychiatric conditions, circadian rhythm issues, and sleep hygiene to sleep problems in the individual patient should be carefully assessed. Sedative/hypnotic medications may be indicated in select cases, in combination with behavioral and sleep hygiene strategies.
Evaluation and Management of Pediatric Sleep Problems: Nightwakings
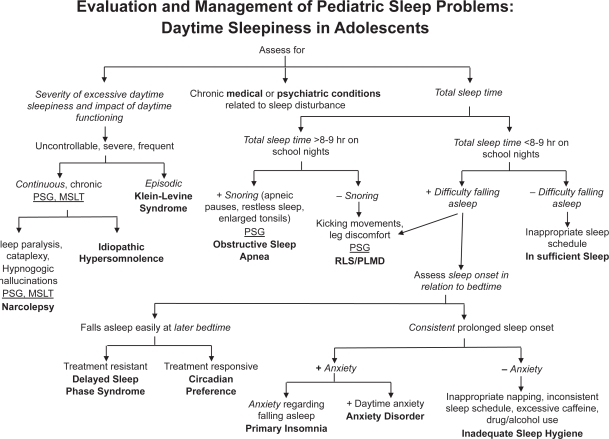
Evaluation and Management of Pediatric Sleep Problems: Daytime Sleepiness in Adolescents
Acknowledgments
Acknowledgements/Conflict of Interest
The authors have no financial relationships or conflicts to disclose.
References
- Ali NJ, Pitson D, Stradling JR. Sleep disordered breathing: effects of adenotonsillectomy on behaviour and psychological functioning. European Journal of Pediatrics. 1996;155(1):56–62. doi: 10.1007/BF02115629. [DOI] [PubMed] [Google Scholar]
- Beebe DW. Neurobehavioral morbidity associated with disordered breathing during sleep in children: a comprehensive review. Sleep. 2006;29(9):1115–1134. doi: 10.1093/sleep/29.9.1115. [DOI] [PubMed] [Google Scholar]
- Biederman J, Spencer T. Attention-deficit/hyperactivity disorder (ADHD) as a noradrenergic disorder. Biological Psychiatry. 1999;46(9):1234–1242. doi: 10.1016/s0006-3223(99)00192-4. [DOI] [PubMed] [Google Scholar]
- Chee MW, Chuah LY. Functional neuroimaging insights into how sleep and sleep deprivation affect memory and cognition. Current Opinion in Neurology. 21(4):417–23. doi: 10.1097/WCO.0b013e3283052cf7. [DOI] [PubMed] [Google Scholar]
- Chervin RD, Archbold KH. Hyperactivity and polysomnographic findings in children evaluated for sleep-disordered breathing. Sleep. 2001;24(3):313–320. doi: 10.1093/sleep/24.3.313. [DOI] [PubMed] [Google Scholar]
- Chervin RD, Archbold KH, Dillon JE, Pituch KJ, Panahi P, Dahl RE, et al. Associations between symptoms of inattention, hyperactivity, restless legs, and periodic leg movements. Sleep. 2002;25(2):213–218. [PubMed] [Google Scholar]
- Chervin RD, Dillon JE, Bassetti C, Ganoczy DA, Pituch KJ. Symptoms of sleep disorders, inattention, and hyperactivity in children. Sleep. 1997;20(12):1185–1192. doi: 10.1093/sleep/20.12.1185. [DOI] [PubMed] [Google Scholar]
- Chervin RD, Ruzicka DL, Giordani BJ, Weatherly RA, Dillon JE, Hodges EK, et al. Sleep-disordered breathing, behavior, and cognition in children before and after adenotonsillectomy. Pediatrics. 2006;117(4):e769–778. doi: 10.1542/peds.2005-1837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen-Zion M, Ancoli-Israel S. Sleep in children with attention-deficit hyperactivity disorder (ADHD): a review of naturalistic and stimulant intervention studies. Sleep Medicine Review. 2004;8(5):379–402. doi: 10.1016/j.smrv.2004.06.002. [DOI] [PubMed] [Google Scholar]
- Corkum P, Panton R, Ironside S, Macpherson M, Williams T. Acute impact of immediate release methylphenidate administered three times a day on sleep in children with attention-deficit/hyperactivity disorder. Journal of Pediatric Psychology. 2008;33(4):368–79. doi: 10.1093/jpepsy/jsm106. [DOI] [PubMed] [Google Scholar]
- Corkum P, Tannock R, Moldofsky H. Sleep disturbances in children with attention-deficit/hyperactivity disorder. Journal of the American Academy of Child and Adolescent Psychiatry. 1998;37(6):637–646. doi: 10.1097/00004583-199806000-00014. [DOI] [PubMed] [Google Scholar]
- Cortese S, Konofal E, Lecendreux M, Arnulf I, Mouren MC, Darra F, et al. Restless legs syndrome and attention-deficit/hyperactivity disorder: a review of the literature. Sleep. 2005;28(8):1007–1013. doi: 10.1093/sleep/28.8.1007. [DOI] [PubMed] [Google Scholar]
- Dahl RE. The regulation of sleep and arousal: Development and psychopathology. Development and Psychopathology. 1996;8:3–27. [Google Scholar]
- Faraone SV, Glatt SJ, Bukstein OG, Lopez FA, Arnold LE, Findling RL. Journal of Attention Disorders. 2008. Apr 9, Effects of once-daily oral and transdermal methylphenidate on sleep behavior of children With ADHD. [DOI] [PubMed] [Google Scholar]
- Golan N, Shahar E, Ravid S, Pillar G. Sleep disorders and daytime sleepiness in children with attention-deficit/hyperactive disorder. Sleep. 2004;27(2):261–266. doi: 10.1093/sleep/27.2.261. [DOI] [PubMed] [Google Scholar]
- Gozal D. Sleep-disordered breathing and school performance in children. Pediatrics. 1998;102(3 Pt 1):616–620. doi: 10.1542/peds.102.3.616. [DOI] [PubMed] [Google Scholar]
- Gruber R, Sadeh A, Raviv A. Instability of sleep patterns in children with attention-deficit/hyperactivity disorder. Journal of the American Academy of Child and Adolescent Psychiatry. 2000;39(4):495–501. doi: 10.1097/00004583-200004000-00019. [DOI] [PubMed] [Google Scholar]
- Hohagen F. Nonpharmacologic treatment of insomnia. Sleep. 1996;19(8):S50–51. [Google Scholar]
- Horne JA. Human sleep, sleep loss and behaviour. Implications for the prefrontal cortex and psychiatric disorder. British Journal of Psychiatry. 1993;162:413–419. doi: 10.1192/bjp.162.3.413. [DOI] [PubMed] [Google Scholar]
- Hvolby A, Jørgensen J, Bilenberg N. Actigraphic and parental reports of sleep difficulties in children with attention-deficit/hyperactivity disorder. Archives of Pediatric and Adolescent Medicine. 2008;162(4):323–9. doi: 10.1001/archpedi.162.4.323. [DOI] [PubMed] [Google Scholar]
- Huang YS, Guilleminault C, Li HY, Yang CM, Wu YY, Chen NH. Attention-deficit/hyperactivity disorder with obstructive sleep apnea: a treatment outcome study. Sleep Medicine. 2007;8(1):18–30. doi: 10.1016/j.sleep.2006.05.016. [DOI] [PubMed] [Google Scholar]
- Lecendreux M, Konofal E, Bouvard M, Falissard B, Mouren-Simeoni MC. Sleep and alertness in children with ADHD. Journal of Child Psychology and Psychiatry. 2000;41(6):803–812. [PubMed] [Google Scholar]
- Lee JS, Kim BN, et al. Regional cerebral blood flow in children with attention deficit/hyperactivity disorder: comparison before and after methylphenidate treatment. Human Brain Mapping. 2005;24:157–164. doi: 10.1002/hbm.20067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marcotte AC, Thacher PV, Butters M, Bortz J, Acebo C, Carskadon MA. Parental report of sleep problems in children with attentional and learning disorders. Journal of Developmental and Behavioural Pediatrics. 1998;19(3):178–186. doi: 10.1097/00004703-199806000-00005. [DOI] [PubMed] [Google Scholar]
- Mayes SD, Calhoun SL, Bixler EO, Vgontzas AN, Mahr F, Hillwig-Garcia J, Elamir B, Edhere-Ekezie L, Parvin M. ADHD subtypes and comorbid anxiety, depression, and oppositional-defiant disorder: differences in sleep problems. Journal of Pediatric Psychology. 2008 Aug 1; doi: 10.1093/jpepsy/jsn083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miano S, Donfrancesco R, Bruni O, Ferri R, Galiffa S, Pagani J, et al. NREM sleep instability is reduced in children with attention-deficit/hyperactivity disorder. Sleep. 2006;29(6):797–803. [PubMed] [Google Scholar]
- Mick E, Biederman J, Jetton J, Faraone SV. Sleep disturbances associated with attention deficit hyperactivity disorder: the impact of psychiatric comorbidity and pharmacotherapy. Journal of Child and Adolescent Psychopharmacology. 2000;10(3):223–231. doi: 10.1089/10445460050167331. [DOI] [PubMed] [Google Scholar]
- Mindell JA, Kuhn B, Lewin DS, Meltzer LJ, Sadeh A. Behavioral treatment of bedtime problems and night ehavi in infants and young children. Sleep. 2006;29(10):1263–1276. [PubMed] [Google Scholar]
- Mindell J, Owens J. A Clinical Guide to Pediatric Sleep: Diagnosis and Management of Sleep Problems in Children and Adolescents. Philadelphia: Lippincott Williams and Wilkins; 2003. [Google Scholar]
- O’Brien LM, Holbrook CR, Mervis CB, Klaus CJ, Bruner JL, Raffield TJ, et al. Sleep and neurobehavioral characteristics of 5- to 7-year-old children with parentally reported symptoms of attention-deficit/hyperactivity disorder. Pediatrics. 2003a;111(3):554–563. doi: 10.1542/peds.111.3.554. [DOI] [PubMed] [Google Scholar]
- O’Brien LM, Ivanenko A, Crabtree VM, Holbrook CR, Bruner JL, Klaus CJ, et al. The effect of stimulants on sleep characteristics in children with attention deficit/hyperactivity disorder. Sleep Medicine. 2003b;4(4):309–316. doi: 10.1016/s1389-9457(03)00071-6. [DOI] [PubMed] [Google Scholar]
- O’Brien LM, Ivanenko A, Crabtree VM, Holbrook CR, Bruner JL, Klaus CJ, et al. Sleep disturbances in children with attention deficit hyperactivity disorder. Pediatric Research. 2003c;54(2):237–243. doi: 10.1203/01.PDR.0000072333.11711.9A. [DOI] [PubMed] [Google Scholar]
- Owens J, Sangal RB, Sutton VK, Bakken R, Allen AJ, Kelsey D. Subjective and objective measures of sleep in children with attention-deficit/hyperactivity disorder. Sleep Medicine. 2008 Aug 5; doi: 10.1016/j.sleep.2008.03.013. [DOI] [PubMed] [Google Scholar]
- Owens JA. The ADHD and sleep conundrum: a review. Journal of Developmental and Behavioural Pediatrics. 2005a;26(4):312–322. doi: 10.1097/00004703-200508000-00011. [DOI] [PubMed] [Google Scholar]
- Owens JA, Babcock D, Blumer J, Chervin R, Ferber R, Goetting M, et al. The use of pharmacotherapy in the treatment of pediatric insomnia in primary care: rational approaches. A consensus meeting summary. Journal of Clinical Sleep Medicine. 2005b;1(1):49–59. [PubMed] [Google Scholar]
- Owens JA, Dalzell V. Use of the ‘BEARS’ sleep screening tool in a pediatric residents’ continuity clinic: a pilot study. Sleep Medicine. 2005c;6(1):63–69. doi: 10.1016/j.sleep.2004.07.015. [DOI] [PubMed] [Google Scholar]
- Owens JA, Rosen CL, Mindell JA. Medication use in the treatment of pediatric insomnia: results of a survey of community-based pediatricians. Pediatrics. 2003;111(5 Pt 1):e628–635. doi: 10.1542/peds.111.5.e628. [DOI] [PubMed] [Google Scholar]
- Owens JA, Spirito A, McGuinn M. The Children’s Sleep Habits Questionnaire (CSHQ): psychometric properties of a survey instrument for school-aged children. Sleep. 2000;23(8):1043–1051. [PubMed] [Google Scholar]
- Picchietti DL, Stevens HE. Early manifestations of restless legs syndrome in childhood and adolescence. Sleep Medicine. 2008;9(7):770–81. doi: 10.1016/j.sleep.2007.08.012. [DOI] [PubMed] [Google Scholar]
- Picchietti D, Allen RP, Walters AS, Davidson JE, Myers A, Ferini-Strambi L. Restless legs syndrome: prevalence and impact in children and adolescents–the Peds REST study. Pediatrics. 2007;120(2):253–266. doi: 10.1542/peds.2006-2767. [DOI] [PubMed] [Google Scholar]
- Picchietti D, Walters A. Restless legs syndrome and period limb movement disorders in children and adolescents. Child & Adolescent Psychiatric Clinics of North America. 1996;5:729–740. [Google Scholar]
- Redline S, Tishler PV, Schluchter M, Aylor J, Clark K, Graham G. Risk factors for sleep-disordered breathing in children. Associations with obesity, race, and respiratory problems. American Journal of Respiratory Critical Care Medicine. 1999;159(5 Pt 1):1527–1532. doi: 10.1164/ajrccm.159.5.9809079. [DOI] [PubMed] [Google Scholar]
- Ring A, Stein D, Barak Y, Teicher A, Hadjez J, Elizur A, et al. Sleep disturbances in children with attention-deficit/hyperactivity disorder: a comparative study with healthy siblings. Journal of Learning Disabilities. 1998;31(6):572–578. doi: 10.1177/002221949803100607. [DOI] [PubMed] [Google Scholar]
- Sadeh A, Pergamin L, Bar-Haim Y. Sleep in children with attention-deficit hyperactivity disorder: a meta-analysis of polysomnographic studies. Sleep Medicine Review. 2006;10(6):381–398. doi: 10.1016/j.smrv.2006.03.004. [DOI] [PubMed] [Google Scholar]
- Sangal B, Owens J, Sangal J. Patients with attention deficit hyperactivity disorder without observed apneic episodes in sleep or daytime sleepiness have normal sleep on polysomnography. Sleep. 2005;28(9):1143–48. [PubMed] [Google Scholar]
- Sangal B, Owens J, Allen A, Sutton V, Feng W, Schuh K, Kelsey D. Effects of atomoxetine and methylphenidate on children with attention deficit hyperactivity disorder. Sleep. 2006;29(12):1573–1585. doi: 10.1093/sleep/29.12.1573. [DOI] [PubMed] [Google Scholar]
- Schecter M. AAP technical report: diagnosis and management of childhood obstructive sleep apnea. Pediatrics. 2002;9(4):704–712. doi: 10.1542/peds.109.4.e69. [DOI] [PubMed] [Google Scholar]
- Sowell ER, Thompson PM, et al. Cortical abnormalities in children and adolescents with attention deficit hyperactivity disorder. Lancet. 2003;362:1699–1707. doi: 10.1016/S0140-6736(03)14842-8. [DOI] [PubMed] [Google Scholar]
- Stein MA. Unravelling sleep problems in treated and untreated children with ADHD. Journal of Child and Adolescent Psychopharmacology. 1999;9(3):157–168. doi: 10.1089/cap.1999.9.157. [DOI] [PubMed] [Google Scholar]
- Sung V, Hiscock H, Sciberras E, Efron D. Sleep problems in children with attention-deficit/hyperactivity disorder: prevalence and the effect on the child and family. Archives of Pediatric and Adolescent Medicine. 2008;162(4):336–42. doi: 10.1001/archpedi.162.4.336. [DOI] [PubMed] [Google Scholar]
- Van der Heijden KB, Smits MG, Van Someren EJ, Ridderinkhof KR, Gunning WB. Effect of melatonin on sleep, behavior, and cognition in ADHD and chronic sleep-onset insomnia. Journal of the American Academy of Child and Adolescent Psychiatry. 2007;46(2):233–41. doi: 10.1097/01.chi.0000246055.76167.0d. [DOI] [PubMed] [Google Scholar]
- Van der Heijden KB, Smits MG, van Someren EJ, Boudewijn Gunning W. Prediction of melatonin efficacy by pretreatment dim light melatonin onset in children with idiopathic chronic sleep onset insomnia. Journal of Sleep Research. 2005;14(2):187–194. doi: 10.1111/j.1365-2869.2005.00451.x. [DOI] [PubMed] [Google Scholar]
- Walters AS, Mandelbaum DE, Lewin DS, Kugler S, England SJ, Miller M. Dopaminergic therapy in children with restless legs/periodic limb movements in sleep and ADHD. Dopaminergic Therapy Study Group. Pediatric Neurology. 2000;22(3):182–186. doi: 10.1016/s0887-8994(99)00152-6. [DOI] [PubMed] [Google Scholar]
- Wei JL, Mayo MS, Smith HJ, Reese M, Weatherly RA. Improved behavior and sleep after adenotonsillectomy in children with sleep-disordered breathing. Archives of Otolaryngology and Head and Neck Surgery. 2007;133(10):974–9. doi: 10.1001/archotol.133.10.974. [DOI] [PubMed] [Google Scholar]
- Weiss MD, Wasdell MB, Bomben MM, Rea KJ, Freeman RD. Sleep hygiene and melatonin treatment for children and adolescents with ADHD and initial insomnia. Journal of the American Academy of Child and Adolescent Psychiatry. 2006;45(5):512–519. [PubMed] [Google Scholar]