Abstract
BACKGROUND:
In recent years, there has been a rapid growth in diagnostic and therapeutic procedures performed by respirologists.
OBJECTIVES:
To assess the number and type of procedures performed in Canadian respirology training programs, for comparison with the American College of Chest Physicians minimum competency guidelines, and to assess fellow satisfaction with procedural training during their fellowships.
METHODS:
Internet-based surveys of Canadian respirology fellows and respirology fellowship program directors were conducted.
RESULTS:
Response rates for program director and respirology fellow surveys were 71% (10 of 14) and 62% (41 of 66), respectively. Thirty-eight per cent of respirology fellows reported the presence of an interventional pulmonologist at their institution. Flexible bronchoscopy was the only procedure reported by a large majority of respirology fellows (79.5%) to meet American College of Chest Physicians recommendations (100 procedures). As reported by respirology fellows, recommended numbers of procedures were met by 59.5% of fellows for tube thoracostomy, 21% for transbronchial needle aspiration and 5.4% for closed pleural biopsy. Respirology fellows in programs with an interventional pulmonologist were more likely to have completed some form of additional interventional bronchoscopy training (80% versus 32%; P=0.003), had increased exposure to and expressed improved satisfaction with training in advanced diagnostic and therapeutic procedures, but did not increase their likelihood of achieving recommended numbers for any procedures.
CONCLUSIONS:
Canadian respirology fellows perform lower numbers of basic respiratory procedures, other than flexible bronchoscopy, than that suggested by the American College of Chest Physicians guidelines. Exposure and training in advanced diagnostic and therapeutic procedures is minimal. A concerted effort to improve procedural training is required to improve these results.
Keywords: Bronchoscopy, Education, Needle biopsy, Pulmonary training, Respirology
Abstract
HISTORIQUE :
Ces dernières années, les interventions diagnostiques et thérapeutiques effectuées par les pneumologues ont connu une croissance rapide.
OBJECTIFS :
Évaluer le nombre et le type d’interventions exécutées dans les programmes canadiens de formation en pneumologie, les comparer avec les lignes directrices de compétence minimale de l’American College of Chest Physicians et évaluer la satisfaction des étudiants envers la formation sur les interventions pendant leur spécialité.
MÉTHODOLOGIE :
Les auteurs ont procédé à des sondages par Internet auprès des étudiants canadiens en pneumologie et des directeurs de ces programmes.
RÉSULTATS :
Le taux de réponse des directeurs de programmes et des étudiants en pneumologie était de 71 % (dix sur 14) et de 62 % (41 sur 66), respectivement. Trente-huit pour cent des étudiants en pneumologie ont déclaré la présence d’un pneumologue interventionniste à leur établissement. La bronchoscopie flexible était la seule intervention déclarée par une majorité des étudiants en pneumologie (79,5 %) à respecter les recommandations de l’American College of Chest Physicians (100 interventions). Tels que l’ont déclaré les étudiants en pneumologie, le nombre recommandé d’interventions était respecté par 59,5 % des étudiants pour la thoracostomie par drain, 21 % pour l’aspiration à l’aiguille transbronchiale et 5,4 % pour la biopsie pleurale fermée. Les étudiants aux programmes de pneumologie comptant un pneumologue interventionniste étaient plus susceptibles d’avoir terminé un type de formation en bronchoscopie interventionniste (80 % par rapport à 32 %; P=0,003), étaient davantage exposés à la formation sur les interventions diagnostiques et thérapeutiques avancées et en étaient plus satisfaits, mais la probabilité qu’ils effectuent le nombre recommandé d’une intervention donnée n’était pas plus élevée.
CONCLUSIONS :
Les étudiants canadiens en pneumologie effectuent moins d’interventions respiratoires de base que le nombre recommandé par les lignes directrices de l’American College of Chest Physicians, à part la bronchoscopie flexible. La formation sur les interventions diagnostiques et thérapeutiques avancées et l’exposition à ces interventions sont minimes. Un effort concerté pour améliorer ce type de formation s’impose.
In recent years, there has been rapid growth in the complexity and number of diagnostic and therapeutic procedures performed by respirologists. Many centres now have dedicated interventional pulmonary medicine (IPM) specialists or, at the least, respirologists with a particular interest in this area, while fellowship training programs in IPM are becoming more common. Other interventional subspecialties in internal medicine have subspecialty boards accredited through the American Board of Internal Medicine (cardiology, interventional cardiology, gastroenterology) that require threshold numbers of supervised procedures to achieve competence (1), although such subspecialties are not recognized by the Royal College of Physicians and Surgeons of Canada (RCPSC) (2). In respirology, controversy exists regarding the issue of requiring a minimum number of procedures for the certification of competence and whether an additional year of training in advanced IPM techniques should be offered (3,4). Both the European Respiratory Society (5) and the American College of Chest Physicians (ACCP) have published guidelines on interventional pulmonary procedures with recommendations on the number of procedures to be performed to achieve competence (6); however, there is little published information regarding current training in bronchoscopy and in other interventional pulmonary procedures. The RCPSC requires that candidates “perform and understand indications, contraindications, technical aspects and quality assurance issues and complications of bronchoscopy (including transbronchial biopsy), thoracentesis and pleurodesis and placement of chest tube” (7), but minimum procedure numbers are not considered.
In a large national survey (8) of practicing respirologists in the United States (US), only 26% currently perform all of the procedures that are required for board certification in respirology. In five of the 13 procedures that were in question, more than 20% of respondents stated that they had learned the procedures in practice and not in their training program. Several studies (9–11) have demonstrated a large variation in the spectrum of respirology procedures offered to trainees. Although programs with a dedicated interventional pulmonologist (IP) are more likely to offer training in advanced therapeutic procedures, fewer than 30% of these programs provide enough procedural numbers for their trainees to meet ACCP competency recommendations (9).
The current rapid evolution of respirology procedures has led to challenges in terms of both ensuring timely but safe introduction of new techniques in the armamentarium of practicing respirologists, and in allowing fellows in training programs the opportunity to receive formal, up-to-date procedural training. Currently, little is known about the availability and adequacy of training offered to Canadian fellows, especially for more advanced procedures. The present study aimed to assess the number and type of procedures offered and performed in Canadian respirology fellowship programs, to compare the number of procedures reported with those suggested in the ACCP guidelines, and to assess fellows’ satisfaction with procedural training during their fellowships.
METHODS
Study design
Internet-based surveys of Canadian respirology fellows (RFs) and respirology fellowship program directors (PDs) were conducted.
Survey design
Surveys used for both RFs and PDs were modified with permission from those developed at the Medical University of South Carolina (South Carolina, USA) (10,12). Minor modifications were made to make surveys applicable to Canadian respirology training programs. Both surveys were translated into French. The surveys were then uploaded to Web-based survey software (SurveyMonkey, USA). Each of the four survey versions were then pilot tested by five different physicians fluent in French or English according to the survey version. Minor modifications were made based on the feedback from the pilot tests.
Standard diagnostic procedures were defined as flexible bronchoscopy (FB), transbronchial biopsies and tube thoracostomy. Advanced diagnostic procedures were defined as endobronchial ultrasound, autofluorescence bronchoscopy, transthoracic needle aspiration and closed pleural biopsy. Advanced therapeutic procedures were defined as rigid bronchoscopy, electrocautery, laser, cryotherapy, stents, transtracheal oxygen therapy, percutaneous tracheostomy, medical thoracoscopy, photodynamic therapy and brachytherapy.
Mailing list
A list of PDs for all Canadian respirology training programs was tabulated. Each PD was contacted to confirm that they were the active PD for their program and to request a complete e-mail list of RFs currently in second or third year or having graduated the year before.
Invitations to fill out the survey were sent via e-mail in February 2006 and a reminder e-mail was sent in March 2006. A limited mail-out was sent in June 2006 after several incorrect e-mail addresses were identified in the original list.
Data analysis
Survey results were downloaded anonymously from the Web site, and the English and French replies collated into statistical analysis software (SPSS version 12.0, USA). Data are presented in descriptive format. The presence of an IP was ascertained and procedural offerings, volume and RF satisfaction were compared with programs that did not have an IP, using χ2 tests and Fisher’s exact tests, as appropriate.
RESULTS
The response rates for PDs and RF surveys were 71% (10 of 14) and 62% (41 of 66), respectively. Three of the RF respondents and two of the PD respondents did not complete every answer on the survey.
RFs
The RF respondents consisted of recent graduates (n=15; 36.6%) and second-year (n=16; 39.0%) or third-year (n=10; 24.4%) respirology or respirology/critical care fellows. Approximately 22% of RFs (nine of 41) were enrolled in or had completed fellowships in respirology and critical care, whereas 78% (32 of 41) were in respirology programs.
Approximately 38% of RFs (15 of 40) reported the presence of an IP at their institution. Fifty per cent of RFs (20 of 40) reported doing dedicated training in interventional bronchoscopy in the form of an elective month with an IP or an interventional bronchoscopy course. Forty-five per cent (18 of 40) of RFs stated that they would be interested in an extra year of IPM training.
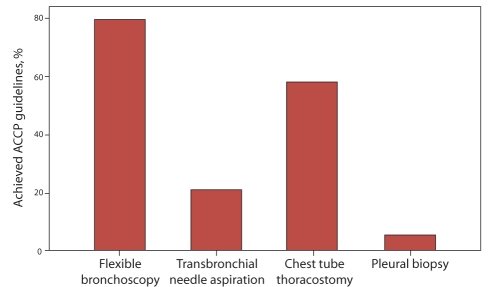
Of the standard diagnostic procedures (FB, tube thoracostomy and transbronchial biopsies), FB was the only procedure reported by a large majority of RFs (79.5%; 31 of 39) to meet ACCP recommendations (100 procedures). If second-year RFs were excluded from the present analysis, the number of RFs meeting ACCP recommendations for FB only increased to 83.3% (20 of 24). Recommended numbers for tube thoracostomy (10 procedures) were met by 59.5% of RFs (23 of 39), for transbronchial needle aspiration (TBNA) (25 procedures) by 20.5% (eight of 39), for transbronchial biopsies (using TBNA criteria of 25 because there are no ACCP recommended numbers for competency for transbronchial biopsy) by 51.3% (20 of 39) with 33.3% (13 of 39) reporting less than 15. Recommended numbers for closed pleural biopsy (five procedures) was met by 5.4% of RFs (two of 37) (Figure 1).
Figure 1).
Percentage of respirology fellows who report achieving recommended number of procedures according to American College of Chest Physicians (ACCP) guidelines
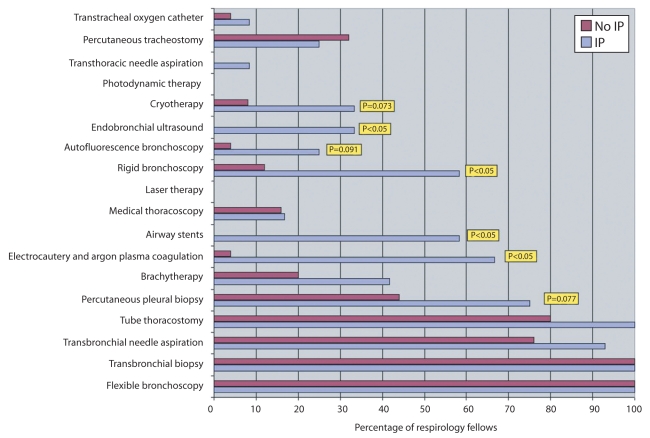
Programs with an IP offered exposure to a greater variety of advanced diagnostic and therapeutic procedures (Figure 2), although the presence of an IP did not increase the likelihood of RFs meeting the ACCP recommendations for any of the procedures. RFs in programs with an IP were more likely to have completed some form of additional interventional bronchoscopy training (80% versus 32%; P=0.003).
Figure 2).
Percentage of respirology fellows offered training for each procedure according to the presence or absence of an interventional pulmonologist (IP) on staff
The quality of training in standard diagnostic procedures was described as good or very good by 95.1% of RFs (39 of 41). Training was rated as barely acceptable, poor or very poor for TBNA, advanced diagnostic procedures and advanced therapeutic procedures in 46% (19 of 41), 82.8% (34 of 41) and 82.8% (34 of 41), respectively. RFs rated the quality of procedural training significantly (P<0.05) higher for all but standard diagnostic procedures in the presence of an IP (Table 1).
Table 1.
Respirology fellows’ (RFs) assessment of procedural training in programs with and without an interventional pulmonologist (IP)
| Procedure type | RFs quality ratings for procedural training in programs with an IP (% good or very good) | RFs quality ratings for procedural training in programs without an IP (% good or very good) | P |
|---|---|---|---|
| Standard diagnostic procedures | 100.0 | 92.0 | NS |
| TBNA | 73.3 | 34.8 | 0.02* |
| Advanced diagnostic procedures | 38.5 | 0 | 0.013* |
| Advanced therapeutic procedures | 40.0 | 0 | 0.005* |
P <0.05. NS Not significant; TBNA Transbronchial needle aspiration
PDs
Most PDs believed that RFs obtained adequate numbers for all standard diagnostic procedures. Approximately 87.5% of PDs (seven of eight) reported that their RFs achieved recommended numbers for FB, 62.5% (five of eight) for tube thoracostomy, 62.5% (five of eight) for TBNA and 37.5% (three of eight) for closed pleural biopsy.
Seventy-five per cent of PDs (six of eight) believe that it is reasonable to require performance of a minimal number of supervised procedures for certification. Seventy-five per cent of PDs (six of eight) also agreed that the minimal number of supervised procedures for certification suggested in the ACCP guidelines were appropriate, and six of eight PDs required that their fellows maintain procedure logbooks of some kind. Eighty-nine per cent of PDs believed that an extra year of training would be desirable for competency for some or most procedures.
DISCUSSION
Medical procedures performed by a subspecialty group represent an integral core component of that subspecialty’s overall expertise and skill set; indeed, they form a part of its identity. Specialists performing procedures within their subspecialty area are expertly positioned not only to perform the procedures themselves, but to intimately understand their indications, contraindications, risks and benefits, and to explain this information to their patients. As such, it becomes critical to ensure optimal procedural training for respirology trainees. These surveys were undertaken to determine the state of procedural training in Canadian respirology training programs.
The findings in the present study are worrisome. The only procedure for which a large majority of Canadian RFs reported reaching minimum recommended targets for competency as per ACCP guidelines was FB. Fewer than two-thirds of fellows achieved the minimum 10 chest tube placements during their fellowships and only 50% performed at least 25 transbronchial biopsies. Approximately 21% met the target number for TBNA and only 5% met the target for closed pleural biopsy. PDs appear to be aware of these problems given that three of the eight respondents did not believe that their programs allowed for adequate numbers of chest tube placements or TBNA, and five of eight PDs for closed pleural biopsy. While many studies have demonstrated the underuse of TBNA (11,13), it is harder to explain how basic skills such as chest tube placements and transbronchial biopsies are not being more frequently practiced by our fellows. At the time of survey preparation, it was believed that Canadian internal medicine residents would have received adequate thoracentesis training by the end of their three-year internal medicine residency (14) because this is a requirement of the RCPSC; however, given the findings in the present study, it may have been useful to include this procedure in the survey. Given that training in advanced diagnostic and therapeutic pulmonary procedures is not a requirement of the RCPSC, it is not surprising that this training is almost nonexistent, at least in terms of fellows achieving published recommendations.
Results for bronchoscopy and chest tube placement are similar to those reported in a survey of US fellows, although fellows in that survey reported significantly higher rates of achievements for both TBNA (58.5%) and closed pleural biopsy (37.7%) (9). As well, a small minority of these fellows received training in advanced therapeutic and diagnostic modalities. The higher rates found in this study may reflect a sample bias given that the questionnaire was administered at a ‘hands-on’ course, likely attended by fellows specifically interested in the procedural aspects of respirology.
The presence of an IP was associated with increased exposure to advanced techniques for fellows, and led to increased satisfaction in training for TBNA and advanced diagnostic and therapeutic procedures. These findings mirrored those from a US-based survey (9). The presence of an IP, however, did not increase the likelihood of RFs meeting the ACCP recommendations for any procedures.
While there remains an ongoing debate regarding the specific minimum numbers of procedures required for the certification of competence, or whether requiring specific numbers is an appropriate measure of competence (3,4), other interventional subspecialties in internal medicine (gastroenterology and cardiology in the US) require threshold numbers of supervised procedures to achieve competence (1). The RCPSC does not stipulate a minimum number of procedures for demonstrating competency and includes bronchoscopy (with bronchoalveolar lavage and transbronchial biopsy), thoracentesis, chest tube placement and pleurodesis in the list of procedures for which competency is required (7). The RCPSC procedural training requirements do not address training for TBNA, closed pleural biopsy, or any of the advanced diagnostic or therapeutic IPM procedures. Despite the lack of minimum procedure requirements by the RCPSC, 75% of PDs agreed that meeting a minimum number of supervised procedures is an important component of the certification of competence, that fellows should maintain procedure logs, and that the minimum numbers in the ACCP guidelines were appropriate.
The Interventional Chest/Diagnostic Procedures Network of the ACCP attempted to address the lack of guidelines for chest procedures in 2003 (6). These consensus guidelines were developed by a group of expert respirologists and thoracic surgeons residing in the US and abroad. The objectives of such guidelines are to ensure that the basic skills and competencies needed to safely perform standard respirology and interventional pulmonary procedures are acquired by the dedicated operators (ie, respirologists, thoracic surgeons). Similar guidelines were also published by the European Respiratory Society, but these only addressed advanced procedures (5). The guidelines are limited because the evidence available in the literature is often inadequate to make definitive statements on patient outcomes and number of procedures needed to achieve competency.
Why do Canadian respirology training programs appear to have difficulty providing enough experience for fellows in some of the most basic respirology procedures? It may be that given the lack of specific volume criteria required by the RCPSC, programs are not designed to achieve the numbers in the range recommended by the ACCP guidelines. One could argue that performing 80 bronchoscopies or 15 transbronchial biopsies is enough for many trainees to achieve competency, but when the benchmarks are relatively low such as for chest tube insertion (10 procedures), it becomes more difficult to argue that one becomes an expert after participating in only a handful of procedures.
The advent of image-guided procedures, usually performed by interventional radiologists, has certainly reduced the number of thoracenteses, chest tubes and even pleural biopsies performed by respirologists. While image guidance has undoubtedly improved the safety and accuracy of these procedures, relatively few respirologists have adapted by learning thoracic ultrasonography for these purposes.
Respirologists have also been particularly slow in adapting other new technologies. TBNA remains an underused technique by respirologists in North America (11,13), despite extensive evidence for its high yield, safety and cost savings (15–19). In Canada, the most significant advance in bronchoscopy since the invention of the flexible instrument is endobronchial ultrasonography, which may be more rapidly implemented into practice by thoracic surgeons given its role as an alternative procedure to mediastinoscopy. Respirologists will have to be more proactive in implementing new techniques if they are to remain experts in the field of bronchoscopy.
Currently, procedural training in most respirology training programs often consists of opportunistic procedures performed on patients seen in a clinic or while on inpatient services. As such, the type, volume and frequency of procedures performed is left to chance and will vary according to the fellow’s assigned rotations and preceptors. A more concerted effort at procedural training will be required to ensure that each fellow is exposed to appropriate numbers of at least the basic procedures. This may require specific elective time dedicated to procedural training in collaboration with our colleagues in interventional radiology and thoracic surgery. Bronchoscopy simulators and other procedural simulators, including animal models, have been developed and have shown significant success in establishing fundamental bronchoscopy skills and improving airway anatomical knowledge (20,21). Procedural simulators may improve trainee satisfaction and can be used for advanced procedures. It is possible that procedural simulators could facilitate sufficient skill development and thereby reduce the numbers of procedures that would be required to achieve competence.
Fellows demonstrated significant interest in IPM procedures, with 50% of them having completed elective time, courses or additional fellowship training in IPM. Similarly, a majority of PDs believed that an additional year of training was desirable for at least some of the procedures discussed, and 45% of RFs would be interested in such a program. Fellows having had increased exposure to the field of IPM through the presence of an IP in their centre were more likely to have completed and to consider additional training in the field.
Fellows graduating from Canadian respirology training programs have minimal exposure to advanced diagnostic and therapeutic IPM skills. The list of advanced techniques will only grow in the future with the addition of bronchoscopic guidance techniques, in vivo microscopic imaging, as well as bronchoscopic treatments for chronic obstructive pulmonary disease and even asthma. To expect that most RFs would be trained, or that the practicing respirologist would maintain proficiency in the majority of these procedures, is clearly unrealistic given the current findings. Additional training will be required by respirologists wishing to master these techniques. Unfortunately, additional fellowship training in IPM is currently available in only a small number of centres in North America, with the demand greatly outnumbering the number of available positions. However, the number of IPM programs is growing steadily, and with the support of academic centres, local IPM programs can flourish and the development of additional dedicated fellowship programs will follow to satisfy this demand.
The present study describes the number and type of procedures currently being offered and performed in Canadian respirology fellowship programs according to the reports of RFs and PDs. Our data suggest that programs are currently only meeting the ACCP minimum competency recommendations for FB and not for other standard diagnostic procedures, nor for advanced diagnostic or therapeutic pulmonary procedures. Prospective studies using logbooks of supervised procedures would help confirm our findings, because a limitation of the present study is that reported procedure numbers by the fellows may be based on fellow recollection even if we requested that logbook data be used. A concerted effort toward procedural training is required to improve the current state. The use of bronchoscopy and procedural simulation may assist in improving skill development and trainee satisfaction, and may eventually reduce the minimum number of procedures necessary for the certification of competence. The present study supports previous findings that the presence of a dedicated IPM specialist improves trainee satisfaction in their procedural training (12). As well, it is expected that the rapid growth in complexity of bronchoscopy and other respirology procedures will require additional formal training in IPM to acquire the necessary skills and competency in the field.
Acknowledgments
This work was performed out of the Division of Respiratory Medicine, University of Calgary; Southern Alberta Cancer Research Institute, Calgary, Alberta.
Footnotes
CONFLICT OF INTERESTS: The authors disclose that they have no actual or potential conflicts of interest with regard to the content of this manuscript.
REFERENCES
- 1.Feller-Kopman D. Is a dedicated 12-month training program required in interventional pulmonology. Con: Dedicated training. J Bronchol. 2004;11:62–4. [Google Scholar]
- 2.The Royal College of Physicians and Surgeons of Canada Accredited residency programs<http://rcpsc.medical.org/residency/accreditation/arps/arp_e.php> (Version current at May 22, 2008).
- 3.Torrington KG. Bronchoscopy training and competency: How many are enough? Chest. 2000;118:572–3. doi: 10.1378/chest.118.3.572. [DOI] [PubMed] [Google Scholar]
- 4.Wahidi MM, Herth FJ, Ernst A. State of the art: Interventional pulmonology. Chest. 2007;131:261–74. doi: 10.1378/chest.06-0975. [DOI] [PubMed] [Google Scholar]
- 5.Bolliger CT, Mathur PN. ERJ/ATS statement on interventional pulmonology. Eur Respir J. 2002;19:356–73. doi: 10.1183/09031936.02.00204602. [DOI] [PubMed] [Google Scholar]
- 6.Ernst A, Silvestri GA, Johnstone D. Interventional pulmonary procedures: Guidelines from the American College of Chest Physicians. Chest. 2003;123:1693–717. doi: 10.1378/chest.123.5.1693. [DOI] [PubMed] [Google Scholar]
- 7.The Royal College of Physicians and Surgeons of Canada Objectives of training and specialty training requirements in adult respirology<http://rcpsc.medical.org/information/index.php?specialty=472&submit=Select> (Version current at May 22, 2008).
- 8.Tape TG, Blank LL, Wigton RS. Procedural skills of practicing pulmonologists. A national survey of 1,000 members of the American College of Physicians. Am J Respir Crit Care Med. 1995;151:282–7. doi: 10.1164/ajrccm.151.2.7842180. [DOI] [PubMed] [Google Scholar]
- 9.Haponik EF, Russell GB, Beamis JF, Jr, et al. Bronchoscopy training: Current fellows’ experiences and some concerns for the future. Chest. 2000;118:625–30. doi: 10.1378/chest.118.3.625. [DOI] [PubMed] [Google Scholar]
- 10.Pastis NJ, Nietert PJ, Silvestri GA. Variation in training for interventional pulmonary procedures among US pulmonary/critical care fellowships: A survey of fellowship directors. Chest. 2005;127:1614–21. doi: 10.1378/chest.127.5.1614. [DOI] [PubMed] [Google Scholar]
- 11.Haponik EF, Shure D. Underutilization of transbronchial needle aspiration: Experiences of current pulmonary fellows. Chest. 1997;112:251–3. doi: 10.1378/chest.112.1.251. [DOI] [PubMed] [Google Scholar]
- 12.Pastis NJ, Nietert PJ, Silvestri GA. Fellow’s perspectives of their training in interventional pulmonary procedures. J Bronchol. 2007;12:88–95. [Google Scholar]
- 13.Prakash UB, Offord KP, Stubbs SE. Bronchoscopy in North America: The ACCP survey. Chest. 1991;100:1668–75. doi: 10.1378/chest.100.6.1668. [DOI] [PubMed] [Google Scholar]
- 14.The Royal College of Physicians and Surgeons of Canada Objectives of Training and Specialty Training Requirements in Internal Medicine<http://rcpsc.medical.org/information/index.php?specialty=136&submit=Select> (Version current at May 22, 2008).
- 15.Cetinkaya E, Yildiz P, Altin S, et al. Diagnostic value of transbronchial needle aspiration by Wang 22-gauge cytology needle in intrathoracic lymphadenopathy. Chest. 2004;125:527–31. doi: 10.1378/chest.125.2.527. [DOI] [PubMed] [Google Scholar]
- 16.Wang KP, Terry P, Marsh B. Bronchoscopic needle aspiration biopsy of paratracheal tumors. Am Rev Respir Dis. 1978;118:17–21. doi: 10.1164/arrd.1978.118.1.17. [DOI] [PubMed] [Google Scholar]
- 17.Wang KP, Terry PB. Transbronchial needle aspiration in the diagnosis and staging of bronchogenic carcinoma. Am Rev Respir Dis. 1983;127:344–7. doi: 10.1164/arrd.1983.127.3.344. [DOI] [PubMed] [Google Scholar]
- 18.Shure D. Transbronchial biopsy and needle aspiration. Chest. 1989;95:1130–8. doi: 10.1378/chest.95.5.1130. [DOI] [PubMed] [Google Scholar]
- 19.Mehta AC, Kavuru MS, Meeker DP, et al. Transbronchial needle aspiration for histology specimens. Chest. 1989;96:1228–32. doi: 10.1378/chest.96.6.1228. [DOI] [PubMed] [Google Scholar]
- 20.Blum MG, Powers TW, Sundaresan S. Bronchoscopy simulator effectively prepares junior residents to competently perform basic clinical bronchoscopy. Ann Thorac Surg. 2004;78:287–91. doi: 10.1016/j.athoracsur.2003.11.058. [DOI] [PubMed] [Google Scholar]
- 21.Colt HG, Crawford SW, Galbraith O., 3rd Virtual reality bronchoscopy simulation: A revolution in procedural training. Chest. 2001;120:1333–9. doi: 10.1378/chest.120.4.1333. [DOI] [PubMed] [Google Scholar]