Abstract
Behçet's disease (BD) is a chronic relapsing multisystem disease characterized by oral ulceration, genital ulceration and ocular lesions. Gastrointestinal involvement is rare, often difficult to treat and associated with a high mortality rate. We treated a 47-year-old Korean man with BD who had a recurrent intestinal ulcer with tumor necrosis factor α antibody (infliximab); he initially underwent right hemicolectomy due to uncontrolled intestinal bleeding. For patients with intestinal BD who fail to respond to conventional treatment, infliximab may be a safe and effective new therapeutic option.
Keywords: Behcet syndrome, Tumor necrosis factor-alpha, Infliximab
INTRODUCTION
Behçet's disease (BD) was first described by Behçet in 1937 as a chronic recurrent disease characterized by recurrent oral ulceration, genital ulceration and ocular involvement1), additional involvement of many other organs has been reported including: joints, skin, blood vessels, the nervous system and gastrointestinal tract2). Reports on invasion into the gastrointestinal tract vary depending on country, however, it has been reported to be present in three to 60% of BD patients3). For these patients, medical treatment is the primary approach to therapy, however, additional surgical treatment is necessary for cases with complications such as, perforation, intractable pain and hemorrhage. However, lesions frequently recur after surgical treatment and the incidence of more than one surgical procedure is high; such cases may be untreatable and lead to death. Recently, cases of BD with gastrointestinal involvement have been treated with tumor necrosis factor alpha (TNF-α) antibody (Infliximab)4, 5), however, there is no prior case of such treatment reported in Korea. We treated a patient with recurrent intestinal ulcer who underwent right hemicolectomy due to uncontrolled intestinal bleeding with infliximab. The case is described in this report and the medical literature reviewed.
CASE REPORT
A 47 years old male patient was admitted to the hospital due to severe abdominal pain for five days. The past medical history was significant for recurrent oral and genital ulceration over the past 20 years. He underwent right hemicolectomy due to uncontrolled intestinal bleeding caused by intestinal Behçet's ulceration 10 years previously. Subsequently, he was treated by conventional medical therapy including corticosteroids, sulfasalazine and azathioprine. However, intestinal Behçet's ulceration recurred at the anastomosis site and the patient required several subsequent hospitalizations due to repeated abdominal pain and intestinal bleeding. The physical examination showed an acutely ill patient with a blood pressure of 120/70 mmHg, a pulse rate of 94 times/min, a respiratory rate of 24 times/min and a temperature of 38.5℃. The abdomen was flat with mild tenderness; the bowel sounds were normal.
The laboratory test results showed a white blood cell count, 540/mm3; hemoglobin, 7.2 g/dL; hematocrit, 28%; platelet count, 47,000/mm3; total protein, 5.7 g/dL; and erythrocyte sedimentation rate (ESR) was increased to 60 mm/H and C-reactive protein (CRP) was increased to 70 mg/L. The Crohn's Disease Activity Index (CDAI)6) at the time of admission was 183 and the Harvey-Bradshaw Index (HBI)7) was 10. The computed tomography showed a suspicious large deep ulcer with bowel wall thickening at the right hemicolectomy site but no obstruction or fistula was observed (Figure 1). A colonoscopy showed the right hemicolectomy and a well demarcated large deep ulcer with a clear ulcer bed at the stomal site (Figure 2). Colonic biopsies showed ulceration with necrotic fibrin debris, an inflammatory infiltrate with neutrophils predominating but no granuloma (Figure 3). The azathioprine was discontinued due to hematological side effects. Because of the uncontrolled continuous abdominal pain, infliximab (5 mg/kg) was started. There were no observed side effects from the infliximab; two weeks after the treatment was started, the symptoms improved dramatically. After one month, the laboratory testing showed a white blood cell count, 4,470/mm3; hemoglobin, 12.3 g/dL; hematocrit, 36.8% and a platelet count, 168,000/mm3. The ESR and CRP were decreased to 11 mm/H and 6.7 mg/L, respectively and the CDAI and HBI were decreased to 88 and 2, respectively. Follow up colonoscopy showed a well demarcated marginal ulcer with granulation tissue at the stomal site, however, the ulcer size was decreased compared to the prior study (Figure 4). A second infliximab (5 mg/kg) treatment was administered one month after the first. The symptoms continued to improve and the abdominal pain resolved completely four months after the second injection of infliximab. The CRP and ESR were maintained in the normal range and the value of CDAI and HBI continued to decrease. The patient was entirely asymptomatic at the 12 month follow up.
Figure 1.
CT scan shows a suspicious large deep ulcer with gastrointestinal wall thickening at the right hemicolectomy site but no obstruction or fistula.
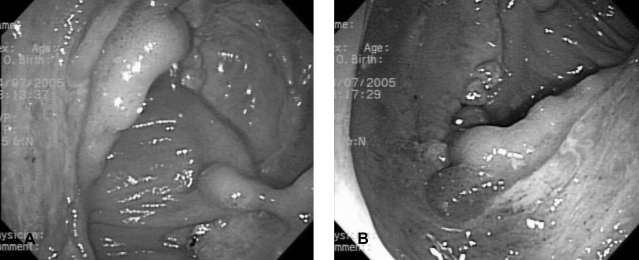
Figure 2.
(A, B) Colonoscopy shows the right hemicolectomy and a well demarcated single large ulcer with a clear ulcer bed at the stomal site.
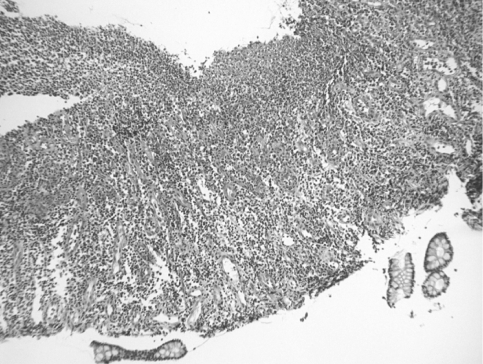
Figure 3.
The colonic biopsies show ulceration with necrotic fibrin debris, inflammatory infiltrate with predominant neutrophils and granulation tissue infiltrated into mononuclear leukocytes (Hematoxylin and eosion stain, original magnification ×40).
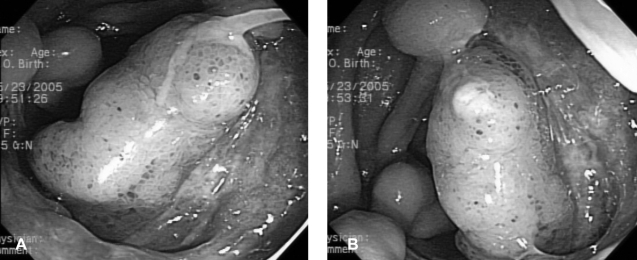
Figure 4.
(A, B) Follow up colonoscopy shows decreased size of the punched out ulcer with granulation tissue at the anastomosis site compared to the prior study.
DISCUSSION
When intestinal ulceration occurs in patients with BD it is found predominately in the ileocecal region, however, ulcers may be found throughout the entire colon. Colonoscopy findings usually show deep punched out ulcerations with nodular margins and converging folds; the histological findings show a non specific inflammation. Intestinal BD may be associated with a significant morbidity and mortality which results from the high complication rate8, 9).
Although the exact pathogenesis of BD is not completely understood, it has been suggested that the disease is due to an abnormal immune response to environmental factors such as microbial agents in genetically susceptible individuals10). The presence of autoantibodies, a decrease in the T4/T8 ratio and an increased number of circulating natural killer cells and γδ+ T cells also suggest an autoimmune etiology of disease10, 11). In patients with active BD an increase of TNF in the blood and an increase of γδ+ T cells producing TNF have been observed12). Improvement of symptoms has been reported after the administration of TNF blockers in patients unresponsive to conventional therapy13). Therefore, TNF has been considered to play an important role in the inflammation observed in BD patients and this may account for the response to infliximab. Treatment for patients with intestinal BD consists of medical and surgical therapy. Conventional medical therapeutic options include: corticosteroids, mesalamine, thalidomide, bowel rest, total parenteral nutrition and immunosuppressive agents such as azathioprine2). However, surgery is generally required due to resistance to medications, frequent recurrence of lesions and complications such as intestinal perforation and fistula formation. According to Cha et al.14), the rate of surgery over five years has been reported to be approximately 47%. Recurrent ulcers after surgery are commonly found near the anastomosis site, as in this case; the ulcers appear as deep multiple aphthous ulcers or as cutaneous intestinal fistula. When these ulcers are present, the recurrence rate has been reported to be as high as 40~80%15).
In our case, 10 years prior to the admission, the patient meet the criteria for the diagnosis of BD recommended by International Study Group for Behçet's disease16). Based on repeated oral and genital ulceration as well as a positive pathergy test, severe abdominal pain and uncontrolled intestinal bleeding, the patient was diagnosed with intestinal BD and underwent a right hemicolectomy. Despite conventional medical treatment, he had recurrent intestinal ulceration and intractable abdominal pain, therefore, another treatment modality was required. Infliximab has been effective for induction and maintenance treatment in patients with BD and has been particularly successful for treatment of cases with severe mucocutaneous17), gastrointestinal4, 5) and ocular18) manifestations of BD. For patients with intestinal BD, in cases treated with infliximab, the standard dose of infliximab has not yet been established, however, treatment according to the dose and protocol used for Crohn's disease5) or based on the symptoms of the patient4, 19) have been reported.
The disease activity of the patient was evaluated before and after treatment, the CDAI and HBI were used for Behçet's disease because there is no activity index established to date. In our case, infliximab (5 mg/kg) was administered at 0 and 4 weeks and symptomatic complete remission was observed at the 12 month follow up, in addition, endoscopic improvement was also observed. A third infusion of infliximab will be considered for future symptoms or endoscopic findings. This case illustrates that for patients with BD who fail to respond to conventional treatment, infliximab may be a safe and effective new therapeutic option. The long term safety and efficacy of infliximab therapy requires further study.
References
- 1.Behet H. Ueber rezidivierende aphtese durch ein virus verusachte Geswuere am Mund, am Auge und an den Genitalien. Dermatol Wochenschr. 1937;105:1152–1157. [Google Scholar]
- 2.Sakane T, Takeno M, Suzuki N, Inaba G. Behet's disease. N Engl J Med. 1999;341:1284–1291. doi: 10.1056/NEJM199910213411707. [DOI] [PubMed] [Google Scholar]
- 3.Bayraktar Y, Ozaslan E, van Thiel DH. Gastrointestinal manifestations of Behcet's disease. J Clin Gastroenterol. 2000;30:144–154. doi: 10.1097/00004836-200003000-00006. [DOI] [PubMed] [Google Scholar]
- 4.Travis SP, Czajkowski M, McGovern DP, Watson RG, Bell AL. Treatment of intestinal Behet's syndrome with chimeric tumour necrosis factor alpha antibody. Gut. 2001;49:725–728. doi: 10.1136/gut.49.5.725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kram MT, May LD, Goodman S, Molinas S. Behcet's ileocolitis: successful treatment with tumor necrosis factor-alpha antibody (infliximab) therapy: report of a case. Dis Colon Rectum. 2003;46:118–121. doi: 10.1007/s10350-004-6506-4. [DOI] [PubMed] [Google Scholar]
- 6.Best WR, Becktel JM, Singleton JW. Rederived values of the eight coefficients of the Crohn's Disease Activity Index (CDAI) Gastroenterology. 1979;77:843–846. [PubMed] [Google Scholar]
- 7.Harvey RF, Bradshaw JM. A simple index of Crohn's disease activity. Lancet. 1980;1:514. doi: 10.1016/s0140-6736(80)92767-1. [DOI] [PubMed] [Google Scholar]
- 8.Masugi J, Matsui T, Fujimori T, Maeda S. A case of Behcet's disease with multiple longitudinal ulcers all over the colon. Am J Gastroenterol. 1994;89:778–780. [PubMed] [Google Scholar]
- 9.Choi IJ, Kim JS, Cha SD, Jung HC, Park JG, Song IS, Kim CY. Long-term clinical course and prognostic factors in intestinal Behcet's disease. Dis Colon Rectum. 2000;43:692–700. doi: 10.1007/BF02235590. [DOI] [PubMed] [Google Scholar]
- 10.Gul A. Behet's disease: an update on the pathogenesis. Clin Exp Rheumatol. 2001;19:S6–S12. [PubMed] [Google Scholar]
- 11.Suzuki Y, Hoshi K, Matsuda T, Mizushima Y. Increased peripheral blood gamma delta+ T cells and natural killer cells in Behcet's disease. J Rheumatol. 1992;19:588–592. [PubMed] [Google Scholar]
- 12.Yamashita N, Kaneoka H, Kaneko S, Takeno M, Oneda K, Koizumi H, Kongure M, Inaba G, Sakane T. Role of gammadelta T lymphocytes in the development of Behcet's disease. Clin Exp Immunol. 1997;107:241–247. doi: 10.1111/j.1365-2249.1997.274-ce1159.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sfikakis PP. Behcet's disease: a new target for anti-tumour necrosis factor treatment. Ann Rheum Dis. 2002;61:ii51–ii53. doi: 10.1136/ard.61.suppl_2.ii51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cha SD, Lim YS, Kim JW, Kim CG, Kim JS, Chang DK, Jung HC, Song IS, Choi KW, Kim CY. Response to medical therapy, course and recurrence of colonic lesions in Behcet's colitis. Korean J Gastroenterol. 1997;30:472–480. [Google Scholar]
- 15.Kasahara Y, Tanaka S, Nishino M, Umemura H, Shiraha S, Kuyama T. Intestinal involvement in Behcet's disease: review of 136 surgical cases in the Japanease literature. Dis Colon Rectum. 1981;24:103–106. doi: 10.1007/BF02604297. [DOI] [PubMed] [Google Scholar]
- 16.International Study Group for Behcet's Disease. Criteria for diagnosis of Behcet's disease. Lancet. 1990;335:1078–1080. [PubMed] [Google Scholar]
- 17.Robertson LP, Hickling P. Treatment of recalcitrant orogenital ulceration of Behcet's syndrome with Infliximab. Rheumatology. 2001;40:473–474. doi: 10.1093/rheumatology/40.4.473. [DOI] [PubMed] [Google Scholar]
- 18.Munoz-Fernandez S, Hidalgo V, Fernandez-Melon J, Schlincker A, Martin-Mola E. Effect of infliximab on threatening panuveitis in Behcet's disease. Lancet. 2001;358:1644. doi: 10.1016/S0140-6736(01)06677-6. [DOI] [PubMed] [Google Scholar]
- 19.Hassard PV, Binder SW, Nelson V, Vasiliauskas EA. Anti-tumor necrosis factor monoclonal antibody therapy for gastrointestinal Behcet's disease: a case report. Gastroenterology. 2001;120:995–999. doi: 10.1053/gast.2001.22556. [DOI] [PubMed] [Google Scholar]