Abstract
Although Skin Metastasis From A Malignant Tumor Of An Internal Organ Usually Occurs At An Advanced Disease Stage, There Has Been No Prior Report Of A Cutaneous Acral Metastasis From Ampullary Carcinoma To Date. We Report A 71-year Old Male Patient With Cutaneous Metastasis From An Ampullary Adenocarcinoma. The Patient Had A History Of Pylorus Preserving Pancreaticoduodenectomy For Carcinoma Of The Ampulla Of Vater Two Years Prior To Presentation. Physical Examination Revealed Ill-defined, Painful And Hard Erythematous Nodules At The Left Thumb And Distal Phalanx Of The Right Middle Finger. The Computed Tomography Scan Showed Low Density Masses In The Retroperitoneum; The Histological Examination Of A Nodule From The Right Middle Finger Showed A Metastatic Adenocarcinoma. This Case Illustrates That Cutaneous Metastasis From Ampullary Carcinoma Has A Poor Prognosis.
Keywords: Ampulla of Vater, Adenocarinoma, Metastasis
INTRODUCTION
Metastasis to the skin from an internal malignancy is rare. To date, most of the data regarding frequency has been obtained from autopsy series where the frequency of skin metastasis has ranged from 0.7% to 10.4%1-3). When cutaneous metastasis appears as the first sign of a primary cancer, the internal malignancy should be identified. However, most skin metastasis manifest at end stage disease of the primary cancer or during treatment. Therefore, metastatic carcinoma to the skin is generally a poor prognostic sign. We present a male patient with skin metastasis that originated from an ampullary carcinoma. Skin metastasis from ampullary cancer has not been reported in the English literature. Here we describe a case of acral metastasis from ampullary carcinoma and review the related literature.
CASE REPORT
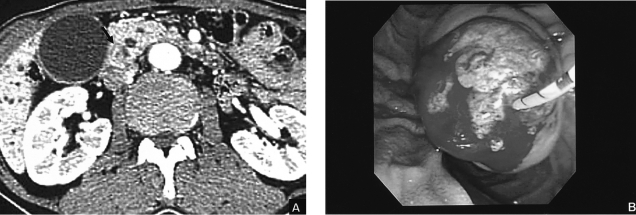
A 71-year-old Korean man was admitted to our hospital with epigastric pain and general weakness. The ocular conjunctiva was icteric. His abdomen was soft and no mass was palpable. The blood chemistry revealed Hgb 12.5 g/dL, bilirubin 1.3 mg/dL, ALP 1879 U/L and GGT 89 U/L. Tumor markers were CA19-9 8.5 U/mL, CEA 8.5 ng/mL and CA-125 7.46 U/mL which were within normal limits. The patient's abdominal computed tomography (CT) showed a mass, with contrast enhancement, at the ampulla of Vater and dilatation of the bile duct as well as the main pancreatic duct (Figure 1A). His duodenoscopy showed a reddish protruding tumor mass at the ampulla of Vater (Figure 1B). The endoscopic ultrasonography demonstrated a hypoechoic mass at the ampulla of Vater without any invasion into the duodenal muscularis propria layer, or pancreatic parenchyma; the mass measured 25×25 mm in size. The endoscopic biopsy of the tumor showed a well-differentiated adenocarcinoma (Figure 3A). The patient underwent pylorus preserving pancreatico-duodenectomy; the resection margins were intact histologically. The tumor size was 25×25×10 mm in diameter. The results of the microscopic examination along with dissection of six lymph nodes confirmed that the lymph nodes did not have any tumor cells. Invasion of the lymphatic and venous systems were not found histologically; however, focal invasion of the common bile duct was observed. Therefore, the tumor was stage I (T2N0M0). The patient recovered without any complication.
Figure 1.
(A) Abdominal computed tomography shows a mass 2.5 cm in diameter at the ampulla of Vater. (B) Endoscopic findings show a protruded mass into the ampulla of Vater.
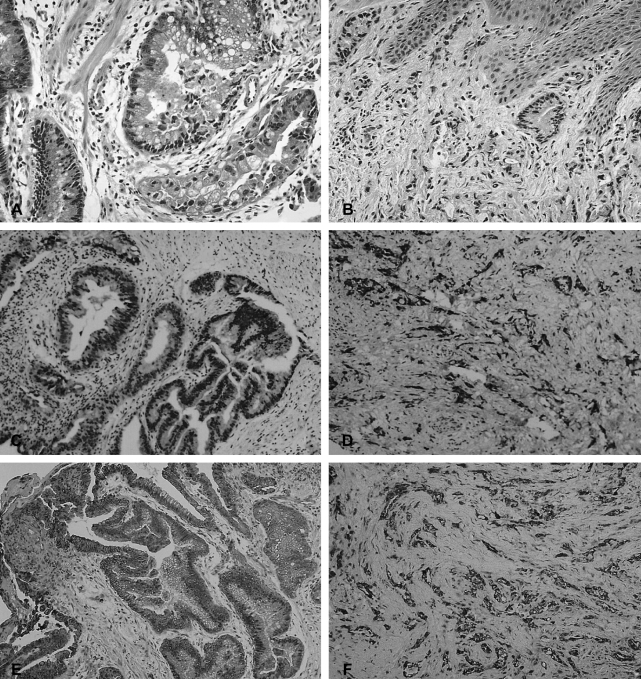
Figure 3.
(A) Histological findings of the mass at the ampulla shows a well differentiated adenocarcinoma (H&E, ×200). (B) Histological findings of the right middle finger shows a well-differentiated adenocacinoma in the dermis (H&E, ×200). (C-F) Immunohistochemical staining supports an acral metastasis; the ampulla carcinoma had a positive result for MUC 1 and CK 7; (C) MUC-1, finger; (D) MUC-1, ampulla; (E) CK7, finger; (F) CK7, ampulla.
Twenty-seven months after surgery, he revisited our hospital because of painful erythematous swelling of the left thumb and the distal phalanx of the right middle finger (Figure 2). Physical examination showed that the patient had a firm, hard, painful swelling that measured 3 cm in diameter on the affected fingers. Skin biopsy from the right middle finger revealed a well-differentiated adenocarcinoma (Figure 3B). In order to confirm that this lesion originated from the primary ampullary carcinoma. and to exclude that this lesion was from other primary sites, immunohistochemical staining was performed with cytokeratin 7 (CK 7), cytokeratin 20 (CK 20), mucin 1 (MUC 1), mucin 2 (MUC 2), thyroid transcription factor-1 (TTF-1), prostate specific antigen (PSA) against the ampullary tumor and skin biopsy specimen. Both tissues were not stained with the TTF-1, PSA, MUC 2, CK 20; however, they stained positive with MUC 1 and CK 7 (Figure 3C-F). The negative result for TTF-1 and PSA supported exclusion of other primary sites (eg lung, prostate). Therefore, our findings confirmed acral metastases from the ampullary carcinoma primary.
Figure 2.
Painful erythematous swelling on the left thumb and distal phalanx of the right middle finger.
Abdominal and pelvic CT at that time demonstrated new retroperitoneal and pelvic lymphadenopathy. The bone scan showed metastasis at the first, third and ninth thoracic spine and fifth left rib; however, no metastasis to the finger bones was observed. The patient was diagnosed with widespread metastatic adenocarcinoma of the ampulla of Vater. He refused to undergo further treatment, and died eight months after the diagnosis of cutaneous metastases.
DISCUSSION
The biological basis of tumor metastasis is complex and not completely understood. The incidence of cutaneous metastases is associated with the type of primary tumor and the patients' gender. In their report, Brownstein and Helwig4) found that the lung is the most common primary site of carcinoma in men while the breast is the most common primary site of carcinoma in women. Other common primary tumor sites are the large intestine and the skin5). Although both pancreatic and biliary adenocarcinoma usually metastasize to the lymph nodes, liver and peritoneum, cutaneous metastasis is rare.
Skin metastasis tends to occur in close proximity to the primary tumor4). Therefore, common sites of skin metastasis are the head, chest6), and abdomen, but metastasis to the fingers is rare7). Generally, cutaneous metastases are classified into three groups according to their appearance: nodular, inflammatory and sclerodermoid metastatic lesions4). They may appear as one or as a combination of the morphologic forms mentioned. Our case presented as an inflammatory type skin metastasis. Painful cutaneous metastasis like our case are rare7). They must be distinguished from acute suppurative inflammation, osteomyelitis, acute paronychia, foreign body granuloma, infectious hematoma, as well as tuberculosis. Based on the fact that this patient had problems with his fingers as a result of gardening work, initially his finger lesion was misdiagnosed as a foreign body granuloma caused by thorns. However, the biopsy of the inflammatory lesion revealed adenocarcinoma.
Ampullary carcinomas have two different types of histopathologic morphology; most tumors exhibit an intestinal morphology resembling primary adenocarcinomas of the colon and rectum, whereas a minority have pancreaticobiliary features similar to adenocarcinoma of pancreas or distal bile duct8). Periampullary tumors represent a spectrum of disease with intestinal-type tumors (duodenal and most ampullary) at the biologically favorable end and the pancreaticobiliary type tumors with an unfavorable prognosis9). Because the two subtypes have different outcomes, it is necessary to identify the appropriate classification. The positive results found for both CK 20 and MUC 2 classified the tumor in the case presented here as an intestinal type, while the positive results for both CK 7 and MUC 1 classified it as a pancreatobiliary type10-12). Because of the positive CK 7 and MUC 1, the ampullary tumor was thought to be classified as a pancreatobiliary type tumor with an unfavorable prognosis.
The recognition of metastatic disease to the skin is important for the following two reasons. First, a cutaneous metastasis may be present before there are clinical signs of an internal malignancy. Second, if a cutaneous metastasis is present, a skin biopsy may help confirm a suspected diagnosis of cancer suggested by findings from other organs which may be much more difficult to biopsy. The results of the skin biopsy may help clinicians focus on the likely location of the primary tumor.
The causes of skin metastasis are as follows: direct invasion from underlying structures, extension through the lymphatics, embolization by the lymphatics and blood vessels and accidental seeding at surgery13). Although the patient in our case had an early stage tumor, he manifested the cutaneous metastasis only twenty-seven months after complete surgical resection of the tumor. We suggest that the leading cause of the cutaneous metastasis might have been embolization through the lymphatics and blood vessels. However, further studies are needed for confirmation. Skin metastasis can occur at any stage of primary cancer. However, most cases have been reported to appear at the end stage14); therefore, it is generally associated with a poor prognosis. In addition, the majority of cancer patients who show skin metastasis are over 50 years of age and most die within a few months after the metastasis is identified1, 2). Our patient had extensive metastases including abdominal and bone metastases at the time the skin lesions were found. This distant spread illustrates that the cancer cells may reach many sites of the body via the blood stream and the lymphatic system.
Although a tumor with cutaneous metastases is unlikely to respond to systemic therapy, local radiotherapy may be indicated for relief of symptoms. On rare occasions, surgical excision of cutaneous metastases may be indicated. In this case, because the patient did not want to receive further treatment, he died eight months after the diagnosis of cutaneous metastasis.
This is the first documented case of the cutaneous finger metastasis from ampullary cancer. It is important to be alert to the possibility that skin metastasis, in distal parts of the extremities, may result from extensive metastasis. In addition, immunohistochemical staining for CK and MUC may be helpful for prediction of prognosis of ampullary carcinoma.
Footnotes
This paper was supported by a grant from Wonkwang University (2006).
References
- 1.Reingold IM. Cutaneous metastases from internal carcinoma. Cancer. 1966;19:162–168. doi: 10.1002/1097-0142(196602)19:2<162::aid-cncr2820190204>3.0.co;2-a. [DOI] [PubMed] [Google Scholar]
- 2.Spencer PS, Helm TN. Skin metastases in cancer patients. Cutis. 1987;39:119–121. [PubMed] [Google Scholar]
- 3.Lookingbill DP, Spangler N, Helm KF. Cutaneous metastases in patients with metastatic carcinoma: a retrospective study of 4020 patients. J Am Acad Dermatol. 1993;29:228–236. doi: 10.1016/0190-9622(93)70173-q. [DOI] [PubMed] [Google Scholar]
- 4.Brownstein MH, Helwig EB. Patterns of cutaneous metastasis. Arch Dermatol. 1972;105:862–868. [PubMed] [Google Scholar]
- 5.Takeuchi H, Kawano T, Toda T, Minamisono Y, Nagasaki S, Yao T, Sugimachi K. Cutaneous metastasis from pancreatic adenocarcinoma: a case report and a review of the literature. Hepatogastroenterology. 2003;50:275–277. [PubMed] [Google Scholar]
- 6.Saeed S, Keehn CA, Morgan MB. Cutaneous metastasis: a clinical, pathological, and immunohistochemical appraisal. J Cutan Pathol. 2004;31:419–430. doi: 10.1111/j.0303-6987.2004.00207.x. [DOI] [PubMed] [Google Scholar]
- 7.Stein RH, Spencer JM. Painful cutaneous metastases from esophageal carcinoma. Cutis. 2002;70:230–232. [PubMed] [Google Scholar]
- 8.Howe JR, Klimstra DS, Moccia RD, Conlon KC, Brennan MF. Factors predictive of survival in ampullary carcinoma. Ann Surg. 1998;228:87–94. doi: 10.1097/00000658-199807000-00013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Todoroki T, Koike N, Morishita Y, Kawamoto T, Ohkohchi N, Shoda J, Fukuda Y, Takahashi H. Patterns and predictors of failure after curative resections of carcinoma of the ampulla of Vater. Ann Surg Oncol. 2003;10:1176–1183. doi: 10.1245/aso.2003.07.512. [DOI] [PubMed] [Google Scholar]
- 10.Le Pessot F, Ranty ML, Hellot MF, Lemoine F, Teniere P, Testart J, Metayer J. Cytokeratins 7 and 20 immunohistochemistry in ampullary carcinomas. Ann Pathol. 2004;24:312–318. doi: 10.1016/s0242-6498(04)93977-6. [DOI] [PubMed] [Google Scholar]
- 11.Zhou H, Schaefer N, Wolff M, Fischer HP. Carcinoma of the ampulla of Vater: comparative histologic/immunohistochemical classification and follow-up. Am J Surg Pathol. 2004;28:875–882. doi: 10.1097/00000478-200407000-00005. [DOI] [PubMed] [Google Scholar]
- 12.Chu PG, Schwarz RE, Lau SK, Yen Y, Weiss LM. Immunohistochemical staining in the diagnosis of pancreatobiliary and ampulla of Vater adenocarcinoma: application of CDX2, CK17, MUC1, and MUC2. Am J Surg Pathol. 2005;29:359–367. doi: 10.1097/01.pas.0000149708.12335.6a. [DOI] [PubMed] [Google Scholar]
- 13.Braverman IM. Skin manifestations of internal malignancy. Clin Geriatr Med. 2002;18:1–19. doi: 10.1016/s0749-0690(03)00031-4. [DOI] [PubMed] [Google Scholar]
- 14.DiSpaltro FX, Bickley LK, Nissenblatt MJ, Devereux D. Cutaneous acral metastasis in a patient with primary gastric adenocarcinoma. J Am Acad Dermatol. 1992;27:117–118. doi: 10.1016/s0190-9622(08)80823-7. [DOI] [PubMed] [Google Scholar]