Abstract
The use of non-absorbable suture materials for cystic duct ligation after cholecystectomy can expose patients to the risk of recurrent stone formation in the common bile duct (CBD). However, in Korea suture materials have rarely been found to act as a nidus for common bile duct calculus formation. Recently, we experienced a case in which suture material, that had migrated from a previous cholecystectomy site into the CBD, probably served as a nidus for common bile duct stone formation. The stone was confirmed by endoscopic retrograde cholangiopancreatography (ERCP) and removed successfully using a basket. The authors report a case of surgical suture migration and discuss its subsequent role as a stone forming nucleus within the CBD in a patient who underwent open cholecystectomy; and include a review of the literature.
Keywords: Suture material, Common bile duct stone, Cholecystectomy
INTRODUCTION
Since Homan first described silk suture material acting as a nidus for the development of subsequent CBD stones after cholecystectomy in 1897, several authors have reported that suture materials may cause choledocholithiasis1). Silk, chromic catgut, parasites, and other foreign bodies are known to form occasionally such niduses in the CBD2-7). In addition, with the advent of laparoscopic cholecystectomy, several authors have reported cases of choledocholithiasis induced by migrated surgical clips8-11). After cholecystectomy for gallstone associated cholecystitis, we infrequently encounter bile duct stones that cause symptoms, such as epigastric pain, cholangitis or right upper quadrant pain.
During the past two decades, many studies have been conducted on the pathogenesis of bile duct stones, but nevertheless, their exact pathogenesis remains unknown. However, it has been proposed that gradual erosion with subsequent inflammation induced by suture material, at a cystic duct ligature, might be a leading cause of stone formation within the CBD.
In the described case, the core of a biliary calculus in the CBD was found to contain filament-like threads. As a result, we suggest that the careful selection of suture materials, such as synthetic and absorbable threads, could prevent subsequent migration and stone formation in the CBD after hepatobiliary surgery.
CASE REPORT
A 74-year-old man was admitted to our hospital with a two-month history of intermittent episodes of right upper quadrant abdominal pain without jaundice. Open cholecystectomy had been performed for symptomatic gallstone-associated cholecystitis approximately 15 years earlier. At that time, multiple stones were found in a distended and inflamed gallbladder. Operative cholangiography showed a filling defect in the CBD. Upon exploration the distal CBD had been dissected and subsequently repaired with a proline suture after T-tube insertion. Over the intervening years the patient had remained asymptomatic until 2 months prior to this presentation. On admission, a physical examination revealed the patient to be relatively weak with an area of pain and mild tenderness to palpation in the right upper quadrant, and a post-operative scar on the abdomen. His vital signs were within normal ranges, i.e., body temperature 37.5℃, blood pressure 120/80 mmHg, heart rate 82/min, respiratory rate 20/min, and biochemical laboratory studies were normal, i.e., aspartate transaminase 23 IU/L (normal 10-35 IU/L), alanine transaminase 28 IU/L (normal 0-40 IU/L), total bilirubin 0.56 mg/dL (normal 0.1-1.2 IU/L), alkaline phosphatase 139 IU/L (normal 80-270 IU/L), and gamma glutamyl transferase 72 IU/L (normal 0-50 IU/L). Initial plain abdominal radiographs demonstrated two surgical clips in the right upper quadrant of the abdomen (Figure 1), and the following abdomen-pelvic computerized tomography (CT) scan revealed a small stone in the CBD and some sandy stones in the dependent portion of the CBD without significant biliary dilatation (Figure 2).
Figure 1.
Plain abdominal radiograph demonstrating two surgical clips in the right upper quadrant.
Figure 2.
The abdominal CT scan showing a small stone (arrow) in the common bile duct and some sand-like stones in the dependent portion of the common bile duct without significant biliary dilatation.
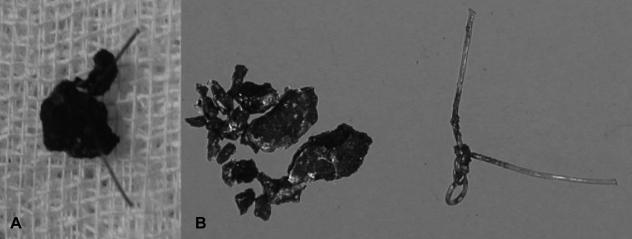
Endoscopic retrograde cholangiopancreatography (ERCP) was performed 2 days after admission, and clearly demonstrated a large freely movable filling defect suggestive of a CBD stone at a mildly dilated distal CBD, and a mild stricture at the mid-common bile duct. During ERCP, two surgical clips were seen adjacent to the cystic duct or artery area. After endoscopic sphincterotomy, a large stone was successfully removed using a retrieval balloon catheter and a Dormia basket. On gross examination, the removed stone was dark brown to black in color. This irregularly shaped CBD stone, measured 1.0×0.9×1.0 cm, had filament-like threads projecting from it (Figure 3). The patient was discharged after his symptomatic improvement and is currently doing well.
Figure 3.
Gross findings of the extracted black-colored stone. This photograph demonstrates filament-like threads projecting from the stone, which measured 1.0×0.9×1.0 cm (A). Crushed bile duct stone and a surgical knot with stone granules attached to its strands (B).
DISCUSSION
Retained stones are the cause of choledocholithiasis after cholecystectomy, and these either arise due to primary formation (arising de novo) or as a consequence of biliary surgery. Bile duct stones are usually classified into two categories based on sites of formation, i.e., as primary or secondary stones. While primary or stasis stones are formed de novo and originate in the bile duct, secondary stones are formed primarily in the gallbladder and subsequently migrate to the bile duct, where they are retained12). Brown pigment stones are generally regarded as primary stones with bacterial overgrowth that are formed secondary to biliary stasis. Several species of bacteria produce β-glucuronidase, which deconjugates bilirubin diglucuronide and frees bilirubin complexes, allowing them to complex with calcium and form an insoluble precipitate of calcium bilirubinate12, 13).
Various factors predispose stone formation in the biliary tract, such as malignancy, benign stricture, bacterial infection, ascaris (round worm) infestation (especially in East Asia), and a broad spectrum of foreign bodies6, 13), the latter of which include metallic hemoclips, retained tubes, ingested foods, and suture materials2-5, 8, 9, 14-19). It is presumed that these factors play an important role in bile stasis by blocking normal bile flow in the biliary tract. Moreover, bile flow blockage could be an initiating factor of nucleus formation in biliary calculi in the CBD.
Surgical clip migration is well-known to occur8-10). Walker et al.19) first reported surgical clip migration into the bile duct in 1979. Moreover, since the introduction of laparoscopic cholecystectomy in 1987, it has become a preferred procedure for the surgical removal of gallbladder stones, and is rapidly replacing open cholecystectomy. However, the mechanism of surgical clip migration into the bile duct is poorly understood. It has been reported that up to one-third of recurrent post-cholecystectomy stones may be due to migrated surgical clips7), and the increasing use of surgical clips and frequency of laparoscopic cholecystectomies has resulted in many reported cases of surgical clip-related stone formation. Nevertheless, some cases might have gone unnoticed due to the spontaneous passage of stones caused either by surgical clips or suture materials.
Non-absorbable sutures, particularly silk, have been found to be responsible for the majority of reported cases of stone formation resulting from a suture material nidus following biliary surgery. The first case of a silk suture serving as a nidus for stone formation after cholecystectomy was reported in 18971). Ban et al.5) reported that irritating operative residuals, such as non-absorbable suture materials, account for 82% of stones that form around a foreign body. Surgical sutures, especially those composed of non-absorbable materials, appear to function as a nidus for crystallization; bile salts gradually deposit around such nuclei, finally develop into large stones.
The role of silk sutures in this context in the biliary tract has been debated by authors. Mackie et al.17) reported three cases of suture material-related stone formation in the CBD, and suggested the use of an absorbable suture material, such as chromic catgut, for ligating the cystic duct or artery. In our case, the suture material was identified as proline, which was used to repair CBD dissection caused by CBD exploration. These proline sutures, which are non-absorbable synthetic monofilament sutures, are still commonly used in neurosurgery because they induce little tissue reaction and are easily placed.
During our review of previous cases, a report was found of a patient in whom chromic catgut had formed a CBD stone nidus, which suggests that absorbable sutures can also cause calculus formation3). The origins of specific causative postoperative sutures have been postulated to be either from cystic duct ligatures or subsequent choledochotomy stitches, which then migrate into the CBD and form biliary calculi. Moreover, since laparoscopic cholecystectomy has largely replaced open biliary surgery, the frequency of suture material-induced calculus formation decreased substantially.
It has been postulated that the chain of events that causes the migration of suture material into the bile duct, may be the same as that of surgical clip migration11). Presumably, repetitive erosion and ulceration of the bile duct by suture material due to an ongoing localized inflammatory process play a primary role in stone formation. When a fragment of suture material is introduced into the CBD, it serves as a nucleus for stone crystallization. Over time the nucleus increases in size and moves slowly toward the bile duct as a consequence of biliary duct activity, and eventually forms a sizable calculus. In addition, if any other cause of bile stasis is present as mentioned above, stone formation may be accelerated.
Endoscopic stone removal with a retrieval balloon catheter and a Dormia basket after sphincterotomy has been recommended as the procedure of choice for the majority of patients who have undergone previous cholecystectomy, since it requires a shorter hospital stay than surgical manipulation20). Bile duct stones can also be extracted endoscopically in patients with biliary pancreatitis or acute obstructive cholangitis. For those patients who have undergone either open cholecystectomy or laparoscopic cholecystectomy, clip migration or suture knot migration should be considered as a cause of recurrent painful symptoms in the right upper quadrant. The described case gives us the opportunity to remind surgeons and endoscopists that biliary stones can be formed by the surgery-related materials in patients that have undergone previous biliary surgery. Thus, here, we report a case in which a surgical suture migrated into the CBD and formed the core of a stone in a patient who had previously undergone open cholecystectomy, and provide a review of the literature.
In conclusion, any exogenous biliary tract foreign bodies, including non-absorbable suture materials, can infrequently function as niduses for stone formation in the common bile duct. We emphasize that synthetic, absorbable sutures or other suture materials with low inflammatory reaction potentials, should be used for biliary surgery, and that they be carefully applied to reduce the risk of recurrent stone formation in the biliary tract.
References
- 1.Homans J. Gall-stones formed around silk sutures, twenty months after recovery from cholecystectomy. Ann Surg. 1897;26:114–116. [PMC free article] [PubMed] [Google Scholar]
- 2.Sigler L, Sahler CO. Silk: the nidus of a common bile duct calculus. Surgery. 1969;65:276–279. [PubMed] [Google Scholar]
- 3.Fink DL, Budd DC. Chromic suture material as a nidus for common duct stone formation. Int Surg. 1983;68:151–152. [PubMed] [Google Scholar]
- 4.Lewis JW, Urdaneta LF. Stone formation on silk suture after cholecochoduodenostomy. South Med J. 1981;74:1280–1281. doi: 10.1097/00007611-198110000-00039. [DOI] [PubMed] [Google Scholar]
- 5.Ban JL, Hirose FM, Benfield JR. Foreign bodies of the biliary tract: report of two patients and a review of the literature. Ann Surg. 1972;176:102–107. doi: 10.1097/00000658-197207000-00018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Schulman A. Non-western patterns of biliary stones and the role of ascariasis. Radiology. 1987;162:425–430. doi: 10.1148/radiology.162.2.3541030. [DOI] [PubMed] [Google Scholar]
- 7.Wosiewitz U, Schenk J, Sabinski F, Schmack B. Investigations on common bile duct stones. Digestion. 1983;26:43–52. doi: 10.1159/000198867. [DOI] [PubMed] [Google Scholar]
- 8.Lee KW, Lee JW, Jeong S, Jung BJ, Lee DH, Kim PS, Kim HG, Kim YS, Choi SK. A case of common bile duct stone formed around a surgical clip after laparoscopic cholecystectomy. Korean J Gastroenterol. 2003;42:347–350. [PubMed] [Google Scholar]
- 9.Oh HJ, Jung HJ, Chai JI, Choi WY, Kim KM, Kim JH, Bae YM, Heo JH. A case of common bile duct stone developed due to a surgical clip as a nidus: an experience of successful management by endoscopy. Korean J Gastroenterol. 2003;42:351–353. [PubMed] [Google Scholar]
- 10.Ahn SI, Lee KY, Kim SJ, Cho EH, Choi SK, Hur YS, Cho YU, Hong KC, Shin SH, Kim KR, Woo ZH, Jeong S. Surgical clips found at the hepatic duct after laparoscopic cholecystectomy. Surg Laparosc Endosc Percutan Tech. 2005;15:279–282. doi: 10.1097/01.sle.0000183257.27303.4e. [DOI] [PubMed] [Google Scholar]
- 11.Chong VH, Yim HB, Lim CC. Clip-induced biliary stone. Singapore Med J. 2004;45:533–535. [PubMed] [Google Scholar]
- 12.Thistle JL. Pathophysiology of bile duct stones. World J Surg. 1998;22:1114–1118. doi: 10.1007/s002689900529. [DOI] [PubMed] [Google Scholar]
- 13.Stewart LS, Oesterle AL, Erdan I, Griffiss FM, Way LW. Pathogenesis of pigment gallstones in Western societies: the central role of bacteria. J Gastrointest Surg. 2002;6:891–903. doi: 10.1016/s1091-255x(02)00035-5. [DOI] [PubMed] [Google Scholar]
- 14.Son JM, Kim DI, Lee HJ, Mjung SJ, Kim HJ, Park ET, Lim BC, Yoo KS, Seo DW, Lee SK, Kim MH, Min YI. Suture material as a nidus of a common bile duct stone. Korean J Gastrointest Endosc. 1999;19:S98–S102. [Google Scholar]
- 15.Smoczynski M, Mittlener S. Suture material as a nidus of common bile duct calculi. Endoscopy. 1995;27:279. doi: 10.1055/s-2007-1005687. [DOI] [PubMed] [Google Scholar]
- 16.Ormann W. A thread as a nidus of a common bile duct calculus: findings during endoscopic lithotripsy. Endoscopy. 1989;21:191–192. doi: 10.1055/s-2007-1012940. [DOI] [PubMed] [Google Scholar]
- 17.Mackie DB, Haynes S, May RE. Unabsorbable suture material: a rare cause of recurrent stones in the common bile-duct. Br J Surg. 1973;60:23–24. doi: 10.1002/bjs.1800600105. [DOI] [PubMed] [Google Scholar]
- 18.Orr KB. Suture material as a nidus for formation of common bile duct stones. Aust N Z J Surg. 1980;50:493–494. doi: 10.1111/j.1445-2197.1980.tb04177.x. [DOI] [PubMed] [Google Scholar]
- 19.Walker WE, Avant GR, Reynolds VH. Cholangitis with a silver lining. Arch Surg. 1979;114:214–215. doi: 10.1001/archsurg.1979.01370260104019. [DOI] [PubMed] [Google Scholar]
- 20.Sivak MV., Jr Endoscopic management of bile duct stones. Am J Surg. 1989;158:228–240. doi: 10.1016/0002-9610(89)90256-0. [DOI] [PubMed] [Google Scholar]