Abstract
Bezoars are concretions or hard masses of foreign matter that are found in the gastrointestinal tract. Recent reports have demonstrated the efficacy of Coca-Cola administration for the dissolution of phytobezors. Here we report on a 73-year-old man with a very large gastric persimmon diospyrobezoar, and this caused small intestinal obstruction after partial dissolution with oral and injected Coca-Cola.
Keywords: Coca-Cola, Bezoar, Intestinal obstruction, Small intestine, Gastrointestinal endoscopy
INTRODUCTION
Bezoars are concretions or hard masses of foreign matter that are found in the gastrointestinal tract. They usually occur in patients who have undergone gastric surgery and have delayed gastric emptying1). Diospyrobezoar is a type of phytobezoar that is caused by persimmons and it is considered to be harder than other types of phytobezoars. Phytobezoars are often resistant to drug treatment and hence, they are usually removed endoscopically or surgically2, 3). The efficacy of administering Coca-Cola for the dissolution of phytobezoars was recently reported4-8). This nonsurgical approach has been considered safe and effective with minimal complications. However, we report here on the first case of phytobezoars that resulted in small intestinal obstruction after partial dissolution with oral and injected Coca-Cola. This case illustrates a potential danger with using Coca-Cola to digest a gastric phytobezoar and it emphasizes the need for careful patient follow-up.
CASE REPORT
A 73-year-old man was referred to our hospital with epigastric pain. He had a history of the hypereosinophilic syndrome for 8 months. His routine blood test 8 months previously showed a white blood cell count of 25,060/mm3 (eosinophils: 61.2%). After taking prednisolone 40 mg on alternative days, the white blood cell count was much improved to 11,400/mm3 (eosinophils: 15%). However, the patient developed epigastric pain. Esophagogastroduodenoscopy (EGD) revealed a very large round hard bezoar with an irregular surface in the stomach (Figure 1). An initial attempt at endoscopic extraction failed to remove the mass due to the size and hardness of the bezoar. We decided to attempt administering two cans (500 mL) of 'Coca-Cola' (Coca-Cola Co., Seoul, South Korea) every 6 hours according to the method described elsewhere6). Four days later, EGD demonstrated that the bezoar was much softened and it was smaller than previously noted. We performed direct endoscopic injection of Coca-Cola into the bezoar. Eight days passed, but bezoar was still in the stomach. Endoscopic injection of Coca-Cola was tried again, and finally the bezoar broke into three pieces. Fifteen days later, the bezoar dissolved (Figure 2) and the epigastric pain resolved. The patient was then lost to follow up. However, 1 month later, he visited the emergency room for abdominal pain with vomiting. On physical examination, a vague abdominal mass just to the right of the umbilicus was noted. The abdomen was tender to direct palpation and it was without rebound tenderness. The bowel sounds were increased. The plain abdominal radiograph showed dilated loops of small intestine with multiple air-fluid levels, which was compatible with obstruction of the small intestine (Figure 3). The subsequent abdominal ultrasound exam showed about a 3.7 cm sized echogenic intraluminal lesion with posterior acoustic shadowing in a dilated small bowel loop with fluid filled dilatation at the right paraumbilical area (Figure 4). The patient was taken to surgery.
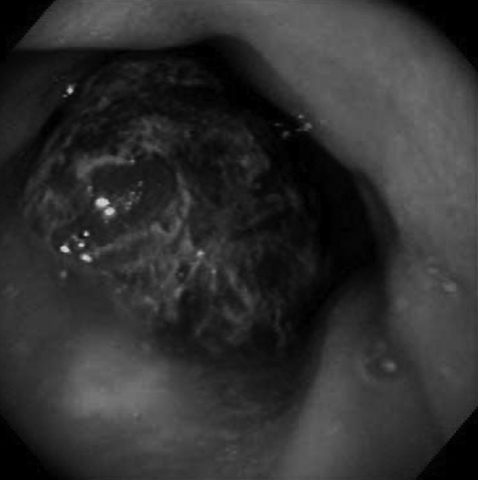
Figure 1.
Esophagogastroduodenoscopy reveals a very large round hard bezoar with an irregular surface in the stomach.
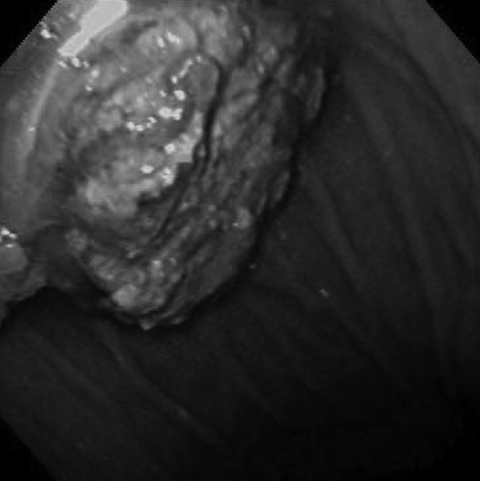
Figure 2.
Esophagogastroduodenoscopy shows that the phytobezoars were broken up into loose fragments in the stomach, 15 days later.
Figure 3.
The plain abdominal radiograph shows dilated loops of small intestine with multiple air-fluid levels.
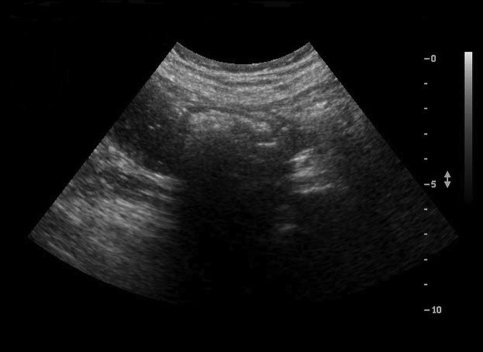
Figure 4.
The abdominal ultrasound shows about a 3.7 cm sized echogenic intraluminal lesion with posterior acoustic shadowing in a dilated loop of small bowel with fluid filled dilatation.
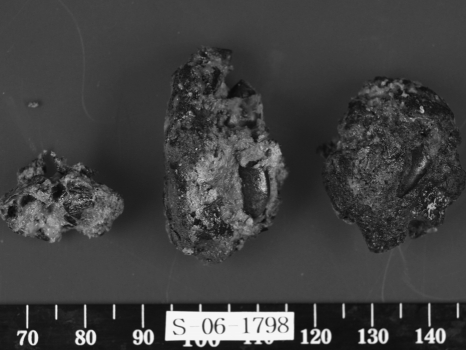
The intraoperative findings revealed small bowel obstruction that was caused by the bezoar. The patient underwent enterotomy and removal of the bezoar; this was followed by primary closure. Three pieces of bezoars were identified and they were composed of persimmons (Figure 5).
Figure 5.
Three pieces of phytobezoar composed of persimmons were the cause of the small bowel obstruction.
DISCUSSION
Several non-surgical methods have been proposed for the treatment of bezoars, and these include a liquid diet, sodium bicarbonate powder, enzymatic digestion with various agents and endoscopic fragmentation. A number of endoscopic techniques for the management of phytobezoars have been described, including fragmentation with biopsy forceps, polypectomy snares, electrosurgical knives and electrohydraulic lithotripsy.
The efficacy of an oral intake and/or endoscopic injection of Coca-Cola and nasogastric lavage with Coca-Cola for the dissolution of diospyrobezoar have been reported5, 6). Ladas et al.4) reported on five consecutive patients with large gastric bezoars. They were treated with 3 L of Coca-Cola nasogastric lavage over a 12 hour period. Kato et al.5) reported on a 52-year-old woman who received oral antidepressants. She was treated with 3 L of 'Coca-Cola light' through a 16 F nasogastric tube over a 12 hour period. Chung et al.6) suggested that drinking two cans (500 mL) of 'Coca-Cola light' every 6 hours and endoscopic injection of Coca-Cola were safe and effective. In addition, Lee et al.7) treated two patients with phytobezoars by having them drink 700~800 mL of 'Coca-Cola' daily. In all the above cases, complete phytobezoar dissolution was achieved by dissolution therapy with Coca-Cola. The mechanism by which Coca-Cola causes dissolution is still unknown. It has been suggested that the NaHCO3 contained in Coca-Cola has a mucolytic effect9). Furthermore, penetration of CO2 bubbles into the surface of the bezoars is thought to digest the fibers of concretion4). The combined action of NaHCO3 and CO2, as well as other unidentified agents in the Coca-Cola, can dissolve bezoars. There have been no side effects reported with this procedure or with using the sugar-free product. Because Coca-Cola is easy to obtain and use, as well as being inexpensive and convenient, it has been accepted as a new method for the management of gastric bezoars.
The occurrence of small intestinal obstruction with a bezoar is usually due to migration of a gastric bezoar10, 11). However, obstruction in the small bowel caused by primary bezoars might be associated with underlying diseases such as diverticulum, stricture or tumor12-14). In one report, partial enzymatic dissolution of a gastric bezoar caused subsequent small bowel obstruction in a 59-yr-old man. The patient underwent 80% gastrectomy with a Billroth II procedure without vagotomy15). In another case, a 66-year-old woman had a sudden onset of small-bowel obstruction during enzymatic treatment for a gastric persimmon bezoar16).
In summary, we reported here on a case of small intestinal obstruction after partial dissolution of a bezoar with performing oral and injected Coca-Cola therapy. While it is apparent from the previous reports that Coca-Cola was safe and effective for the dissolution of phytobezoars, the possibility of subsequent partial or complete small bowel obstruction must be kept in mind so that this potentially catastrophic complication can be more expeditiously managed.
Footnotes
The authors have no commercial association that might be a conflict of interest in relation to this article.
References
- 1.Cifuentes Tebar J, Robles Campos R, Parrilla Paricio P, Lujan Mompean JA, Escamilla C, Liron Ruiz R, Pellicer Franco EM. Gastric surgery and bezoars. Dig Dis Sci. 1992;37:1694–1696. doi: 10.1007/BF01299861. [DOI] [PubMed] [Google Scholar]
- 2.Rozen P, Gilat T. Enzymatic softening and endoscopic destruction of a phytobezoar in an unoperated stomach. Am J Gastroenterol. 1975;64:397–399. [PubMed] [Google Scholar]
- 3.Walker-Renard P. Update on the medicinal management of phytobezoars. Am J Gastroenterol. 1993;88:1663–1666. [PubMed] [Google Scholar]
- 4.Ladas SD, Triantafyllou K, Tzathas C, Tassios P, Rokkas T, Raptis SA. Gastric phytobezoars may be treated by nasogastric Coca-Cola lavage. Eur J Gastroenterol Hepatol. 2002;14:801–803. doi: 10.1097/00042737-200207000-00017. [DOI] [PubMed] [Google Scholar]
- 5.Kato H, Nakamura M, Orito E, Ueda R, Mizokami M. The first report of successful nasogastric Coca-Cola lavage treatment for bitter persimmon phytobezoars in Japan. Am J Gastroenterol. 2003;98:1662–1663. doi: 10.1111/j.1572-0241.2003.07563.x. [DOI] [PubMed] [Google Scholar]
- 6.Chung YW, Han DS, Park YK, Son BK, Paik CH, Jeon YC, Sohn JH. Huge gastric diospyrobezoars successfully treated by oral intake and endoscopic injection of Coca-Cola. Dig Liver Dis. 2006;38:515–517. doi: 10.1016/j.dld.2005.10.024. [DOI] [PubMed] [Google Scholar]
- 7.Lee HJ, Kang HG, Park SY, Yi CY, Na GJ, Lee TY, Kim SH, Song CS. Two cases of phytobezoars treated by adminsitration of Coca-Cola by oral route. Korean J Gastroenterol. 2006;48:431–433. [PubMed] [Google Scholar]
- 8.Martinez de Juan F, Martinez-Lapiedra C, Picazo V. Phytobezoar dissolution with Coca-Cola. Gastroenterol Hepatol. 2006;29:291–293. doi: 10.1157/13087468. [DOI] [PubMed] [Google Scholar]
- 9.Sanderson I, Ibberson O, Fish EB. Gastric phytobezoar following gastrectomy. Can Med Assoc J. 1971;104:1115. [PMC free article] [PubMed] [Google Scholar]
- 10.Krausz MM, Moriel EZ, Ayalon A, Pode D, Durst AL. Surgical aspects of gastrointestinal persimmon phytobezoar treatment. Am J Surg. 1986;152:526–530. doi: 10.1016/0002-9610(86)90221-7. [DOI] [PubMed] [Google Scholar]
- 11.Escamilla C, Robles-Campos R, Parrilla-Paricio P, Lujan-Mompean J, Liron-Ruiz R, Torralba-Martinez JA. Intestinal obstruction and bezoars. J Am Coll Surg. 1994;179:285–288. [PubMed] [Google Scholar]
- 12.Frazzini VI, Jr, English WJ, Bashist B, Moore E. Small bowel obstruction due to phytobezoar formation within Meckel diverticulum: CT findings. J Comput Assist Tomogr. 1996;20:390–392. doi: 10.1097/00004728-199605000-00012. [DOI] [PubMed] [Google Scholar]
- 13.Herbetko J, Brunton FJ. Enteroliths of small bowel diverticula. Clin Radiol. 1991;43:311–313. doi: 10.1016/s0009-9260(05)80536-7. [DOI] [PubMed] [Google Scholar]
- 14.Lorimer JW, Allen MW, Tao H, Burns B. Small-bowel carcinoid presenting in association with a phytobezoar. Can J Surg. 1991;34:331–333. [PubMed] [Google Scholar]
- 15.Rumley TO, Hocking MP, King CE. Small bowel obstruction secondary to enzymatic digestion of a gastric bezoar. Gastroenterology. 1983;84:627–629. [PubMed] [Google Scholar]
- 16.Nomura H, Kitamura T, Takahashi Y, Mai M. Small-bowel obstruction during enzymatic treatment of gastric bezoar. Endoscopy. 1997;29:424–426. doi: 10.1055/s-2007-1004229. [DOI] [PubMed] [Google Scholar]