Abstract
The purpose of the present study was to evaluate the efficacy and safety of bipolar transurethral prostatectomy (TURP) using the Gyrus™ PlasmaKinetic System compared with conventional monopolar TURP. This study included 102 patients with benign prostatic hyperplasia (BPH) who underwent TURP from January 2003 to March 2005. In all, 49 consecutive patients had bipolar and 53 had monopolar TURP. All patients were assessed by preoperative and postoperative International Prostate Symptom Score (IPSS), uroflowmetry, transrectal ultrasonography, operative time, weight of resected tissue, change in serum sodium and hemoglobin, duration of catheter use, length of hospital stay, and complication rates. Significant improvement was seen postoperatively in both groups, and no difference was observed in the resection time, weight of resected tissue, change in serum sodium and hemoglobin, improvement of IPSS and peak flow rate (Qmax), or complication rates over the 12-month follow-up in both groups. There was, however, a significant difference in duration of catheter use and hospital stay. Duration of catheter use (2.28 days vs. 3.12 days) and hospital stay (3.52 days vs. 4.27 days) were shorter in the bipolar group (p = 0.012 vs. p = 0.034, respectively). Our results demonstrate that bipolar TURP using the Gyrus™ Plasma Kinetic System is as effective as conventional monopolar TURP with the additional advantage of reduced length of catheter use and hospital stay. Bipolar TURP is a promising new technique that may prove to be a good alternative to conventional TURP in the future.
Keywords: Prostatic hyperplasia, transurethral resection of prostate
INTRODUCTION
There are numerous treatment alternatives available for patients with bladder outlet obstruction (BOO) secondary to benign prostatic hyperplasia (BPH), including watchful waiting, pharmacological therapy, minimally invasive therapy, transurethral resection (TURP), and open prostatectomy. Despite the widespread use of medical treatment, a significant proportion of patients require surgical intervention.1 TURP remains the most frequently performed operation for men with BPH,2 despite the availability of numerous minimally invasive alternatives, because these fail to equal TURP and require costly instruments, a steep learning curve, and long-term follow-up to establish their efficacy and safety.3-5
At the same time, TURP often requires extended Foley catheterization and hospital stays, and is associated with various complications, including bleeding, TUR syndrome, incontinence, impotence, and urethral stricture. In conventional TURP, most morbidities are related to the use of nonelectrolyte irrigation fluid, monopolar current, poor visibility due to bleeding, and mechanical factors.
Recently, transurethral resection with bipolar energy was introduced to overcome some of these complications. Bipolar TURP results in less thermal damage and better visibility, and most importantly, the ability to use physiologic saline for irrigation.
The purpose of this study was to compare the efficacy and safety of this newer bipolar TURP using the Gyrus™ PlasmaKinetic Tissue Management System (Gyrus Medical Ltd., Bucks, UK) with conventional monopolar TURP over a follow-up period of 12 months.
MATERIALS AND METHODS
This study included a total of 102 patients with BPH who underwent TURP using the Gyrus™ PlasmaKinetic Tissue Management System (Gyrus Medical Ltd., Bucks, UK) or conventional monopolar resectoscope between January 2003 and March 2005. Forty-nine consecutive patients underwent bipolar TURP using the Gyrus™ system and fifty-three consecutive patients underwent monopolar TURP using the conventional monopolar resectoscope. For inclusion, patients were required to be older than 50 years with symptomatic BPH requiring surgical intervention. Patients were excluded if they had an abnormal digital rectal examination (DRE), increased serum prostate specific antigen (PSA), evidence of neurogenic bladder, urethral stricture, bladder stone or tumor, or a history of prostate surgery.
All patients were preoperatively evaluated in detail by medical history, physical examination with DRE, multiple serum analyses including PSA, uroflowmetry, and transrectal ultrasound (TRUS).
One expert surgeon performed all operations. Bipolar TURP was performed with a 24 Fr. Karl Storz® (Tuttlingen, Germany) continuous flow resectoscope using saline irrigation and the Gyrus™ PlasmaKinetic Tissue Management System. The PlasmaKinetic device had a maximum power of 200 W and delivered a radio frequency wavelength of 320-450 kHz and a voltage range of 254-350 V. The TUR loop consisted of an 80/20 platinum/iridium alloy electrode with the active and return electrode on the same axis (axipolar) separated by a ceramic insulator.
Conventional monopolar TURP was performed with an ACMI® (Southborough, MA, USA) 24 Fr. resectoscope using Urion® (Hwaseong, Korea) irrigation.
At the end of the procedure, a 22 Fr. 3-way Foley catheter was inserted. Saline irrigation was continued at a rate sufficient to maintain a clear returning fluid and the catheter was removed if the urine was clear in the absence of irrigation. The patient was subsequently given a voiding trial and discharged from the hospital if voiding spontaneously.
Serum electrolytes and hemoglobin were measured after TURP. Resection time, weight of resected tissue, duration of catheter use and hospital stay, and presence of any complications were documented in detail. Patients were observed at 1, 6 and 12 months after TURP to allow for the detection of early and late complications, International Prostate Symptom Score (IPSS) assessment, and uroflowmetry.
Statistical analysis was carried out using Student's t-test, Mann-Whitney test and Chi-square test. A p-value < 0.05 was considered to be statistically significant. Statistical data are presented as mean ± SD.
RESULTS
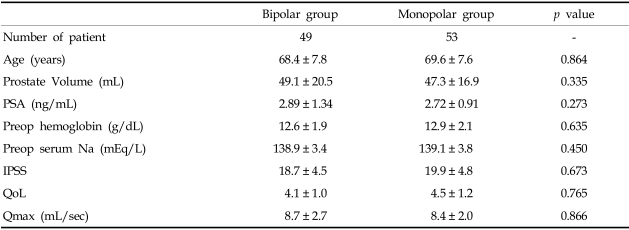
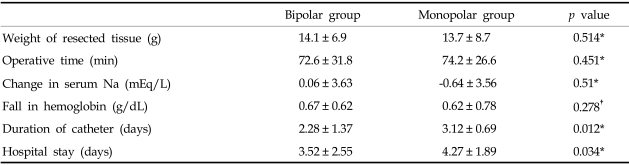
Table 1 shows the characteristics of the 102 patients. The mean operative time was 72.6 ± 31.8 minutes in the bipolar group and 74.2 ± 26.6 minutes in the monopolar group (p = 0.451). With bipolar resection, 14.1 ± 6.9g of prostatic tissue was resected versus 13.7 ± 8.7g in the monopolar group (p = 0.514). Postoperatively, there was no statistical difference in the mean changes of hemoglobin (Hb) and serum sodium between the two groups (p = 0.278 and p = 0.51, respectively) (Table 2).
Table 1.
Patient Characteristic
Values are presented as mean ± SD.
IPSS, international prostate symptom score; QoL, quality of life; Qmax, peak flow rate.
Table 2.
Perioperative Data
Values are presented as mean ± SD.
*p value by Mann-Whitney test.
†p value by t-test.
Mean catheter duration was 2.28 ± 1.37 days in the bipolar group and 3.12 ± 0.69 days in the monopolar group (p = 0.012). The hospital stay was also shorter in the bipolar group (3.52 ± 2.55 days vs. 4.27 ± 1.89 days) (p = 0.034) (Table 2).
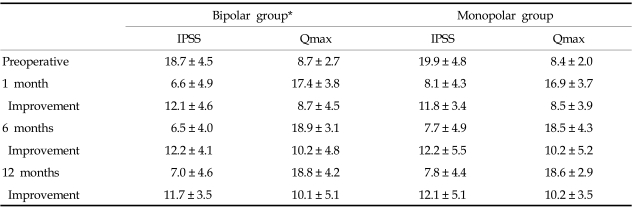
IPSS and peak flow rate (Qmax) improvements at 1, 6 and 12 months were equal in the two groups (Table 3).
Table 3.
Preoperative and Postoperative Improvement of IPSS and Qmax (mL/s) at 1, 6 and 12 Months
Values are presented as mean ± SD.
IPSS, international prostate symptom score; Qmax, peak flow rate.
*p > 0.05 by Mann-Whitney test.
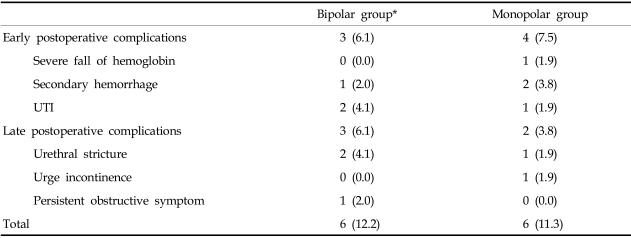
In the early postoperative period, complications were noted in three cases (6.1%) in the bipolar group and four cases (7.5%) in the monopolar group. One patient required blood transfusion due to severe reduction in Hb (1.9%) and two patients required a second operation for TUR fulguration due to bleeding in the monopolar group (3.8%). In the bipolar group, no patient required blood transfusion and one patient required a second operation for TUR fulguration due to bleeding (2.0%). Urinary tract infection (UTI) was observed in two (4.1%) and one (1.9%) patients in the bipolar and monopolar groups, respectively (Table 4).
Table 4.
Complications
Values are presented as number (%).
*p > 0.05 by Chi-square test.
At 12 months, late postoperative complications were noted in three cases (6.1%) in the bipolar group and two (3.8%) cases in the monopolar group. Urethral stricture was observed in two (4.1%) and one (1.9%) patients in the biopolar and monopolar groups, respectively. Urge incontinence was observed in one (1.9%) patient in monopolar group, and persistent obstructive symptom was observed in one (2.0%) patient in the bipolar group (Table 4).
DISCUSSION
BPH is a common problem that affects aging men. Treatment of this condition includes medical and surgical approaches. Despite the availability of medical treatment, about twenty percent of patients with symptomatic BPH require surgical intervention.1 Even with new advances in minimally invasive techniques, TURP remains the standard surgical therapy.2 The large amount of data currently available allows adequate assessment of the efficacy of TURP compared with these new minimally invasive techniques.3-5
Conventional monopolar TURP is considered safe with a low associated mortality rate. High perioperative morbidity rates largely due to intraoperative and postoperative hemorrhage or perforation, however, have been reported. Moreover, TUR syndrome, caused by absorption of irrigation fluid, has been known to occur.6-8 Typically, TURP is performed using a monopolar electric current whose direction flows from the active electrode to a ground. To avoid conduction of this electrical energy to surrounding tissues, a nonconductive irrigating solution is used which, when absorbed in excess, may cause TUR syndrome. The reported rates range from 0.18% to 10.9%, with Mebust and his colleagues reporting an incidence of 2% in conventional monopolar TURP.9-11 The risk of TUR syndrome increases with a larger prostate (> 45 g) or longer resection time (> 90 min).
Recently, transurethral resection and vaporization with bipolar energy has been introduced as a technical modification of TURP.12-14 The biggest advantage of bipolar current in TURP is the use of saline for irrigation, which may reduce the morbidity associated with the absorption of fluid. Performing TURP with saline eliminates the risk of TUR syndrome, thereby enabling the removal of a large bulk of prostate tissue by resection or vaporization.
In our results, the change in serum sodium concentration was not significantly greater in the monopolar resection group when compared to the bipolar group (p = 0.51). In bipolar TURP, the change in serum sodium was 0.06 mEq/L, whereas in the monopolar group, the mean change was -0.64 mEq/L. Two patients of the monopolar groups were found to have serum sodium levels of less than 135 mEq/L (125 mEq/L and 130 mEq/L respectively). Although these patients did not develop symptoms, they were at risk for TUR syndrome.
In conventional monopolar TURP, radiofrequency energy is directed into the tissue where electrical resistance creates temperatures as high as 400℃. In bipolar TURP, however, radiofrequency energy converts a conductive medium (saline irrigant) into a plasma field of highly ionized particles that disrupt the organic molecular bonds between the tissues. By directing the radiofrequency current from an active electrode to an adjacent return electrode, tissue temperature is reduced to 40-70℃. The low temperatures of bipolar TURP allow for minimal tissue damage.15
The absence of a return current in bipolar surgery also removes the risks of burns and cardiac pacemaker problems.
Moreover, bipolar electrocautery seems to be more efficient for removing tissue and simultaneously controlling bleeding when compared to the monopolar procedure. Coagulation is also accurate and effective, which decreases the time for control of bleeding and improves intraoperative vision. Wendt-Nordahl and co-workers reported that bleeding rate was significantly reduced using the bipolar resectoscope in their ex-vivo experiments, compared to the monopolar resection device.14
Our results show that bipolar TURP was equivalent to conventional monopolar TURP in improvement of IPSS and urinary flow rates at 1, 6 and 12 months of follow-up. In addition to the aforementioned advantages, bipolar TURP allows more rapid catheter removal and a shorter hospital stay. Botto and co-workers12 reported a mean hospital stay of only 2.2 days, and all patients were discharged without a catheter, while Eaton and Francis13 reported that 85% of patients were able to return home on the day of surgery and have their catheters removed at 48 hours in the bipolar TURP group. In another study, the patients treated by Gyrus TURP had their catheter removed a mean of 1.4 days earlier than the standard group, improving patient comfort, length of hospital stay, and costs.16
Our results also show that both duration of catheter use and hospital stay were significantly shorter in the bipolar group (p = 0.012 and p = 0.034, respectively).
Other studies with bipolar TURP have reported high rates of recatheterization and that irritative symptoms were more common in the bipolar group, probably as a result of edema secondary to higher current with lower frequency exerted on the tissue.17 Urethral stricture formation was also more commonly observed in the bipolar group. Several risk factors, such as the use of higher ablative energy or larger resectoscope diameter, may account for increased urethral stricture formation. Higher recatheterization rates with the bipolar device were also described in a randomized study by Dunsmuir and collegues.15 Singh and his collegues,18 however, reported that postoperative dysuria was less with bipolar TURP than with monopolar TURP. This difference could be attributed to the greater thermal damage and formation of granulation tissue with monopolar current. In our results, there was no difference in the incidence of recatheterization, irritative symptoms, or postoperative dysuria between the two groups.
We encountered six complications (12.2%) in the monopolar and six (11.3%) in the bipolar group. Only one patient in the monopolar group required transfusion for secondary hemorrhage. With regards to overall complication rates, there was no significant difference between the two groups.
In conclusion, the bipolar transurethral prostatectomy (TURP) using the Gyrus™ Plasma Kinetic System is as effective as conventional monopolar TURP with the additional advantage of decreased duration of catheter use and hospital stay. Therefore, bipolar TURP is a promising new technique that may prove to be a good alternative to conventional TURP in the future.
References
- 1.Barba M, Leyh H, Hartung R. New technologies in transurethral resection of the prostate. Curr Opin Urol. 2000;10:9–14. doi: 10.1097/00042307-200001000-00003. [DOI] [PubMed] [Google Scholar]
- 2.Wasson JH, Reda DJ, Bruskewitz RC, Elinson J, Keller AM, Henderson WG. A comparison of transurethral surgery with watchful waiting for moderate symptoms of benign prostatic hyperplasia. The Veterans Affairs Cooperative Study Group on Transurethral Resection of the Prostate. N Engl J Med. 1995;332:75–79. doi: 10.1056/NEJM199501123320202. [DOI] [PubMed] [Google Scholar]
- 3.Madersbacher S, Schatzl G, Djavan B, Stulnig T, Marberger M. Long-term outcome of transrectal high-intensity focused ultrasound therapy for benign prostatic hyperplasia. Eur Urol. 2000;37:687–694. doi: 10.1159/000020219. [DOI] [PubMed] [Google Scholar]
- 4.Kaplan SA. Minimally invasive alternative therapeutic options for lower urinary tract symptoms. Urology. 1998;51(4A) Suppl:32–37. doi: 10.1016/s0090-4295(98)00053-3. [DOI] [PubMed] [Google Scholar]
- 5.Larson TR. Rationale and assessment of minimally invasive approaches to benign prostatic hyperplasia therapy. Urology. 2002;59(2) Suppl 1:12–16. doi: 10.1016/s0090-4295(01)01557-6. [DOI] [PubMed] [Google Scholar]
- 6.Doll HA, Black NA, McPherson K, Flood AB, Williams GB, Smith JC. Mortality, morbidity and complications following transurethral resection of the prostate for benign prostatic hypertrophy. J Urol. 1992;147:1566–1573. doi: 10.1016/s0022-5347(17)37628-0. [DOI] [PubMed] [Google Scholar]
- 7.Horninger W, Unterlechner H, Strasser H, Bartsch G. Transurethral prostatectomy: mortality and morbidity. Prostate. 1996;28:195–200. doi: 10.1002/(SICI)1097-0045(199603)28:3<195::AID-PROS6>3.0.CO;2-E. [DOI] [PubMed] [Google Scholar]
- 8.Uchida T, Ohori M, Soh S, Sato T, Iwamura M, Ao T, et al. Factors influencing morbidity in patients undergoing transurethral resection of the prostate. Urology. 1999;53:98–105. doi: 10.1016/s0090-4295(98)00524-x. [DOI] [PubMed] [Google Scholar]
- 9.Kolmert T, Norlen H. Transurethral resection of the prostate. A review of 1111 cases. Int Urol Nephrol. 1989;21:47–55. doi: 10.1007/BF02549901. [DOI] [PubMed] [Google Scholar]
- 10.Koshiba K, Egawa S, Ohori M, Uchida T, Yokoyama E, Shoji K. Does transurethral resection of the prostate pose a risk to life? 22-year outcome. J Urol. 1995;153:1506–1509. [PubMed] [Google Scholar]
- 11.Mebust WK, Holtgrewe HL, Cockett AT, Peters PC. Transurethral prostatectomy: immediate and postoperative complications. A cooperative study of 13 participating institutions evaluating 3,885 patients. J Urol. 1989;141:243–247. doi: 10.1016/s0022-5347(17)40731-2. [DOI] [PubMed] [Google Scholar]
- 12.Botto H, Lebret T, Barre P, Orsoni JL, Herve JM, Lugagne PM. Electrovaporization of the prostate with the Gyrus device. J Endourol. 2001;15:313–316. doi: 10.1089/089277901750161917. [DOI] [PubMed] [Google Scholar]
- 13.Eaton AC, Francis RN. The provision of transurethral prostatectomy on a day-case basis using bipolar plasma kinetic technology. BJU Int. 2002;89:534–537. doi: 10.1046/j.1464-410x.2002.02673.x. [DOI] [PubMed] [Google Scholar]
- 14.Wendt-Nordahl G, Hacker A, Reich O, Djavan B, Alken P, Michel MS. The Vista system: a new bipolar resection device for endourological procedures: comparison with conventional resectoscope. Eur Urol. 2004;46:586–590. doi: 10.1016/j.eururo.2004.07.018. [DOI] [PubMed] [Google Scholar]
- 15.Dunsmuir WD, McFarlane JP, Tan A, Dowling C, Downie J, Kourambas J, et al. Gyrus bipolar electrovaporization vs transurethral resection of the prostate: a randomized prospective single-blind trial with 1 y follow-up. Prostate Cancer Prostatic Dis. 2003;6:182–186. doi: 10.1038/sj.pcan.4500631. [DOI] [PubMed] [Google Scholar]
- 16.Starkman JS, Santucci RA. Comparison of bipolar transurethral resection of the prostate with standard transurethral prostatectomy: shorter stay, earlier catheter removal and fewer complications. BJU Int. 2005;95:69–71. doi: 10.1111/j.1464-410X.2005.05253.x. [DOI] [PubMed] [Google Scholar]
- 17.Tefekli A, Muslumanoglu AY, Baykal M, Binbay M, Tas A, Altunrende F. A hybrid technique using bipolar energy in transurethral prostate surgery: a prospective, randomized comparison. J Urol. 2005;174:1339–1343. doi: 10.1097/01.ju.0000173075.62504.73. [DOI] [PubMed] [Google Scholar]
- 18.Singh H, Desai MR, Shrivastav P, Vani K. Bipolar versus monopolar transurethral resection of prostate: randomized controlled study. J Endourol. 2005;19:333–338. doi: 10.1089/end.2005.19.333. [DOI] [PubMed] [Google Scholar]