Abstract
Although high resolution ultrasonography (US) is helpful in the differentiation of suture granulomas from recurrent thyroid cancer in most cases, a definite diagnosis cannot always be made. We report a case that mimicked recurrent thyroid cancer on US and 2-[fluorine-18] fluoro-2-deoxy-D-glucose (FDG) positron emission tomography (PET), but diagnosis of a suture granuloma was confirmed by a US-guided fine needle aspiration biopsy (FNAB). In order to avoid unnecessary operations, the differential diagnosis between postoperative suture granulomas and recurrent cancer is important.
Keywords: Thyroid, ultrasonography, foreign bodies, granuloma
INTRODUCTION
High resolution ultrasonography (US) is widely used in the evaluation of the local recurrence of thyroid cancer in the thyroid bed and regional lymph nodes.1,2 Specifically, US is commonly used in patients who underwent a partial thyroidectomy because thyroglobulin level alone is not helpful in detecting tumor recurrence due to the presence of the other thyroid. Although the typical US findings of suture granulomas (a complication of thyroid surgery) are well known,3 benign lymph nodes and suture granulomas may mimic tumor recurrence on US. We report a case that was considered to be a local tumor recurrence by both US and 2-[fluorine-18] fluoro-2-deoxy-D-glucose (FDG) positron emission tomography (PET) images, but was confirmed to be a suture granuloma on a US-guided fine needle aspiration biopsy (FNAB).
CASE REPORT
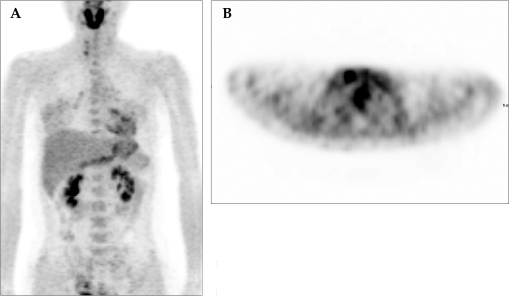
A 39-year-old woman visited our department for a follow-up US after undergoing a right thyroidectomy six months prior due to a papillary carcinoma. The preoperative thyroid US showed an ill-defined hypoechoic mass, measuring 1.5 cm, in the right thyroid (Fig. 1). It was confirmed to be a papillary carcinoma by FNAB. However, there was no evidence of nodal metastasis in the imaging study. A right lobectomy was performed, but iodine 131 therapy was not done because the left thyroid remained. The routine postoperative follow-up US, performed six months after surgery, showed a hypoechoic nodule with an irregular shape, measuring about 0.6 cm, in the right thyroidectomy bed (Fig. 2). Hyperechogenic lines, which are highly suggestive of suture granulomas,3 were not detected on the US. Upon physical examination, abnormal masses were not palpated nor was there any tenderness around the neck. Because only a right thyroidectomy had been done, the thyroglobulin level was not helpful in the diagnosis. A PET scan was performed to obtain additional information about the nodule in the operation bed. A few foci of mildly increased FDG uptake in the region of the right thyroidectomy bed were seen (Fig. 3). A region of interest was placed over this area and the average standard uptake value (SUV) was taken (SUV = 2.91). Because we could not rule out tumor recurrence in the operation bed, a US-guided fine needle aspiration was performed. The cytologic diagnosis was a suture granuloma, without evidence of tumor recurrence (Fig. 4). During the two-year follow-up period, the lesion shrunk.
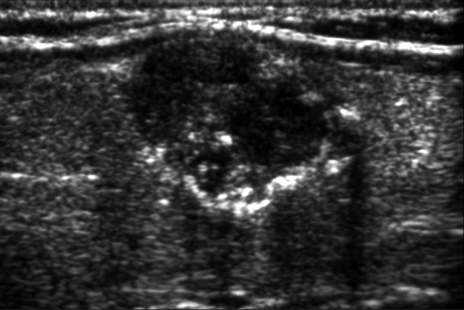
Fig. 1.
Longitudinal US shows a 1.4 × 1.5 cm-sized ill-defined hypoechic nodule with microcalcification at the right thyroid gland. It was confirmed to be a papillary carcinoma by surgery.
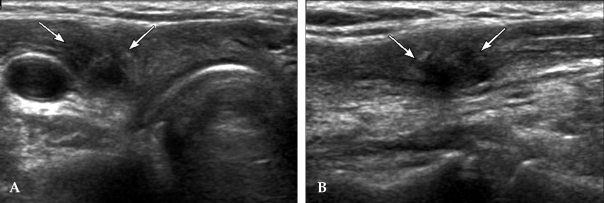
Fig. 2.
A, B. Transverse (A) and longitudinal (B) US shows an irregular shaped hypoechic nodule (arrows) in the right thyroidectomy bed.
Fig. 3.
A, B. Coronal (A) and Axial view (B). A few foci of mildly increased FDG uptake are seen in the right thyroidectomy area.
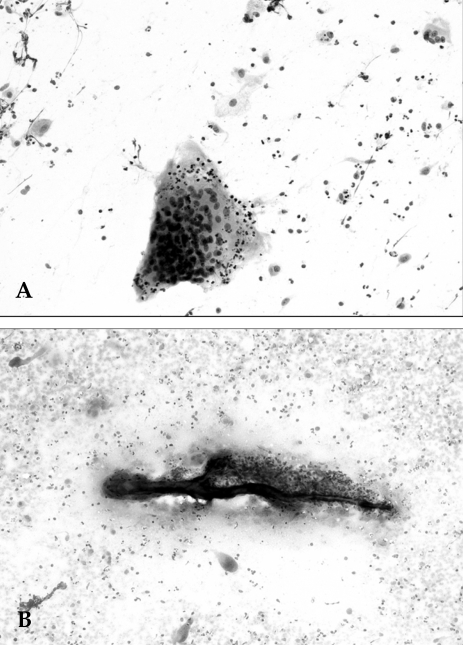
Fig. 4.
(A) A multinucleated giant cell engulfs several acute inflammatory cells in the background of the fibrohistiocytic and neutrophilic cells (Papanicolaou × 400). (B) A large central irregular foreign material is surrounded by granulomatous inflammatory aggregates in the background of variable inflammatory cells and frequent scattered giant cells (Diff-Quick stain × 100).
DISCUSSION
Suture granuloma is a rare complication of thyroid surgery and is known to occur after the use of non-absorbable suture materials deep within the skin. The pathogenesis of suture granulomas involves two steps.4 The first step is the initial reaction of the tissue, which reflects the amount of injury inflicted by the passage of the needle. After the initial reaction subsides, the second step occurs. In this step, the suture material causes specific inflammatory reactions.
Suture granuloma can occur anywhere in the body after a variety of operations.3,5 Eldridge et al.6 reported that the time lag between the operation and the formation of a suture granuloma was helpful in for differential diagnosis. They reported that almost all suture granulomas developed within two years of the operations, but others3 reported that the time interval varied from several months to years. Therefore, time interval was not a reliable diagnostic tool in differentiating between recurrent cancer and suture granulomas.
Suture granuloma is clinically important in cancer patients because it can mimic tumor recurrence. Several authors reported that high resolution US was helpful in differential diagnosis,3,5 but their cases mainly involved of suture granulomas after abdominal surgery. In a study by Rettenbacher et al.,3 the characteristic US finding of suture granulomas was a well-defined, hypoechoic lesion with hyperechoic double lines (rail-like lines) and/or a single line. In our case, there were no characteristic US findings of suture granulomas. Recently, Titton et al.2 reported that lesions developing in the operation bed after thyroidectomy with features suspicious of malignancy should be confirmed by FNAB. The characteristic malignant sonographic features include a marked hypoechoic echogenecity, microcalcification, taller than wide in shape, blurred margin, irregular shape, and intranodular blood flow in Doppler sonography. In our case, sonographic findings were more similar to recurrent cancer (Fig. 2) than to a suture granuloma. Therefore, FNAB was done for confirmation.
Khan et al.7 reported that PET was useful in detecting recurrent differentiated thyroid cancer. They indicated that the specificity was relatively less than sensitivity because inflammatory lesions could show hot uptake in FDG PET. Although false positive findings in PET were reported in other malignancies,8 only one case of suture granuloma was reported in a PET study that investigated the effectiveness of PET for the detection of melanoma metastases.9 This study reported that the false positive result was present due to a suture granuloma.
In summary, although US and PET are useful in differentiation of suture granuloma from local tumor recurrence in cases when the characteristic feature can be found. However, because suture granulomas may mimic recurrent thyroid cancer on US and PET, cautious interpretation is required. Therefore, a US-guided FNAB may be mandatory for confirmation of the diagnosis.
References
- 1.Hegedüs L. Thyroid ultrasound. Endocrinol Metab Clin North Am. 2001;30:339–360. doi: 10.1016/s0889-8529(05)70190-0. [DOI] [PubMed] [Google Scholar]
- 2.Titton RL, Gervais DA, Boland GW, Maher MM, Mueller PR. Sonography and sonographically guided fine-needle aspiration biopsy of the thyroid gland: indications and techniques, pearls and pitfalls. AJR Am J Roentgenol. 2003;181:267–271. doi: 10.2214/ajr.181.1.1810267. [DOI] [PubMed] [Google Scholar]
- 3.Rettenbacher T, Macheiner P, Hollerweger A, Gritzmann N, Weismann C, Todoroff B. Suture granulomas: sonography enables a correct preoperative diagnosis. Ultrasound Med Biol. 2001;27:343–350. doi: 10.1016/s0301-5629(00)00364-1. [DOI] [PubMed] [Google Scholar]
- 4.Postlethwait RW, Willigan DA, Ulin AW. Human tissue reaction to sutures. Ann Surg. 1975;181:144–150. doi: 10.1097/00000658-197502000-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Nagar H, Kessler A, Graif M. The role of ultrasound in the diagnosis of stitch granulomas following paediatric herniotomy. Pediatr Radiol. 1999;29:803–806. doi: 10.1007/s002470050699. [DOI] [PubMed] [Google Scholar]
- 6.Eldridge PR, Wheeler MH. Stitch granulomata after thyroid surgery. Br J Surg. 1987;74:62. doi: 10.1002/bjs.1800740119. [DOI] [PubMed] [Google Scholar]
- 7.Khan N, Oriuchi N, Higuchi T, Zhang H, Endo K. PET in the follow-up of differentiated thyroid cancer. Br J Radiol. 2003;76:690–695. doi: 10.1259/bjr/31538331. [DOI] [PubMed] [Google Scholar]
- 8.Liu SH, Chang JT, Ng SH, Chan SC, Yen TC. False positive fluorine-18 fluorodeoxy-D-glucose positron emission tomography finding caused by osteoradionecrosis in a nasopharyngeal carcinoma patient. Br J Radiol. 2004;77:257–260. doi: 10.1259/bjr/69516821. [DOI] [PubMed] [Google Scholar]
- 9.Holder WD, Jr, White RL, Jr, Zuger JH, Easton EJ, Jr, Greene FL. Effectiveness of positron emission tomography for the detection of melanoma metastases. Ann Surg. 1998;227:764–771. doi: 10.1097/00000658-199805000-00017. [DOI] [PMC free article] [PubMed] [Google Scholar]