Abstract
Autologous transfusion has been used to overcome adverse effects of homologous transfusion. Clinical studies evaluating general orthopaedic postoperative results have been designed to compare these transfusion methods. However, few studies have evaluated postoperative results in spinal fusion surgeries, which have larger blood loss volumes. The purpose of this study is to determine if there are differences in postoperative infection and clinical results of spinal fusion with autologous, as compared to homologous, blood transfusion. A total of 62 patients who underwent instrumented spinal fusion and received autologous (n = 30) or homologous (n = 32) transfusions were reviewed. Information on gender, age, preoperative and 3-day postoperative hematologic features, total transfused units, segmental estimated blood loss, transfused units, and surgery time were collected. In addition, postoperative infection data on wound infection, pneumonia, urinary tract infection, cellulitis, and viral disease, incidence and duration of fever, as well as clinical results, fusion rates, and patient feedback were collected. No differences in postoperative infection and clinical results were found between the two types of transfusions; however, homologous transfusion was associated with an increased number of total units transfused, longer duration of fever, and decreased patient satisfaction regarding the transfusion.
Keywords: Spinal fusion, autologous transfusion
INTRODUCTION
Major orthopedic surgical procedures, including hip arthroplasty, may result in significant blood loss.1,2 Certain procedures, especially spinal fusions, require relatively large amounts of transfusion due to long operative duration, bleeding from the bone graft bed, and spinal instrumentation.3,4
In spite of developments in transfusion medicine, several complications are directly related to homologous blood transfusion. Although infectious contamination has declined substantially, the most common risk remains viral hepatitis, with a transmission rate of approximately 1 per 100,000 units transfused.5
Autologous transfusion (preoperative blood deposit and retransfusion) has been proposed to overcome adverse effects of homologous transfusion. Advantages include elimination of viral infection, transfusion-related lung injury, anaphylaxis, graft-versus-host disease, alloimmunization, and Rh sensitization.6 Autologous transfusions have been used in major orthopaedic procedures, including hip and knee arthroplasties, and, since the introduction of spinal surgery in the 1970s, it continues to be used.3,7-12,14-18
Previous clinical studies have evaluated autologous transfusion combined with hypotensive anesthesia,19 hemodilution,20 replacement time,21 and efficacy.14,22 Several studies have also examined differences in postoperative results, compared to homologous transfusion, in hysterectomies,23 general orthopedic surgeries,24 and hip arthroplasties.25 Surprisingly, few studies have evaluated postoperative infection and clinical results in spinal fusions, which tend to have the largest volumes of blood loss.
The purpose of this study is to determine whether postoperative infection and clinical results differ between patients receiving autologous or homologous blood in instrumented spinal fusion.
MATERIALS AND METHODS
We reviewed medical records of patients who underwent transfusion and instrumented spinal fusion for spinal stenosis or spondylolisthesis between January 1, 1999, and December 31, 2000. Spinal stenosis without spondylolisthesis and spondylolisthesis alone occurred in 41 (66%) and 21 (34%) patients, respectively. Operations were performed by the same surgeons and anesthesiologist. All patients provided informed consent.
Autologous or homologous blood transfusion only, occurred in 30 and 32 procedures, respectively. Twenty five patients who received both autologous and homologous blood were excluded from the study. Patients with high infection risk, including steroid therapy, malnutrition, obesity, diabetes mellitus, and immunosuppression, were not included.
Criteria for autologous donation included a preparticipation screening hemoglobin value; at least 110 grams per liter. Phlebotomy was performed weekly and completed at least five days prior to surgery. Donation was delayed if hemoglobin was less than 110 grams per liter at any time during the blood-acquisition process. Oral iron administration was initiated prior to donation and continued for approximately two months.
In accordance with recently established red blood-cell transfusion guidelines,26 absolute indication for transfusion included intra- or postoperative hemoglobin less than 70 grams per liter. However, most patients received transfusion for clinically based signs and laboratory findings consistent with symptomatic anemia; defined as hemoglobin less than 100 grams per liter, and associated with persistent tachycardia refractory to intravenous fluids, orthostatic hypotension, dyspnea on exertion, or profound fatigability that precluded physical therapy.
We collected information on gender, age, hemoglobin, hematocrit, preoperative and 3-day postoperative platelet count, segmental estimated blood loss, transfused units, surgery time, total transfused units, and duration of prophylactic systemic antibiotic therapy. Segmental estimated blood loss, time, and transfused units in surgery are defined as total blood loss, time, and transfused units divided by number of fused vertebrae, respectively.
Information on postoperative infections, such as wound infection, pneumonia, urinary tract infection, cellulitis, and viral transmitted disease, and incidence and duration of fever without identified infection, was collected. Additional collected information included postoperative clinical results, fusion rates, and satisfaction for the transfusion.
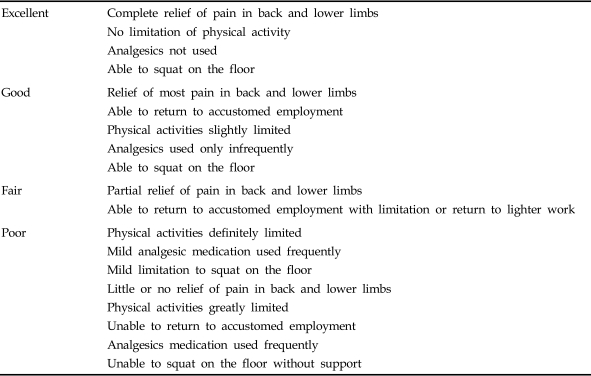
Criteria used for postoperative infection were those used by Tartter et al.27,28 Purulent exudate and positive cultures were adequate evidence of postoperative wound infection. Urinary tract infection was diagnosed when more than 105 colonies grew from culture. Fever, leukocytosis, and chest infiltrate indicated pneumonia. Fever was defined by temperature more than 38.3℃ (101°F). Duration of fever was calculated in days.25 Clinical results were analyzed by Kim's criteria, according to clinical improvement variables (Table 1).29 Solid fusion is defined by continuous trabecular bridge traversing the grafted segment between the transverse processes by flexion and extension dynamogram.30,31 Patient satisfaction was classified as "satisfied," "unsatisfied," and "not judged," by asking patient discomfort during and after transfusion, compared to before transfusion.
Table 1.
Criteria for Measuring Improvement of Clinical Results
Statistical analysis was performed using SPSS 10. The independent-samples t test, chi-square test, and Pearson correlation analysis were used to compare variables. P value less than 0.05 was considered significant.
RESULTS
Autologous and homologous recipients were similar in gender, age, segmental time in surgery, estimated blood loss, number of transfused units, number of fused vertebrae, duration of antibiotic therapy, and mean hospital stay. Homologous transfusion was associated with an increased total number of units transfused (Table 2). Usually the recommended duration for prophylactic antibiotic administration upon spinal surgery is two days;32 however, longer durations are common practice at our institution.
Table 2.
Clinical Features of Patients with Autologous and Homologous Transfusion
The values shown are mean ± SD unless otherwise noted.
The p values were determined by independent-samples t test, level 5%.
*Not significant.
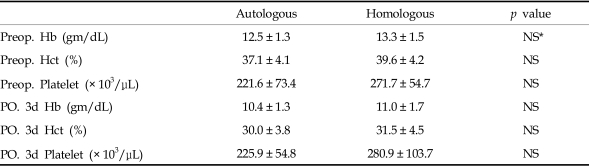
The autologous and homologous recipients were similar in hemoglobin, hematocrit, and platelet count preoperatively and at the 3rd postoperative day (Table 3).
Table 3.
Laboratory Features of Patients with Autologous and Homologous Transfusion
The values shown are mean ± SD.
The p values were determined by independent-samples t test, level 5%.
*Not significant.
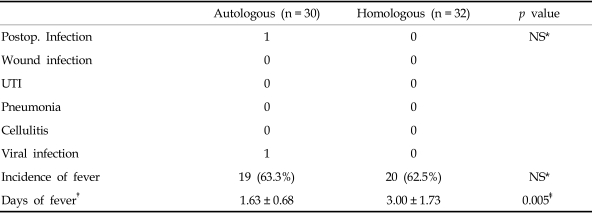
No statistical differences were found in postoperative infections including wound infection, pneumonia, urinary tract infection, or cellulites, although one patient in the autologous group developed postoperative wound infection, and one developed viral infection (the common cold) (Table 4).
Table 4.
Postoperative Complications of Patients with Autologous and Homologous Transfusion
*Not significant.
†The values shown are mean ± SD.
‡The p values were determined by independent-samples t test, level 5%.
No differences were found in incidence of fever without identified infection; however, homologous transfusion was associated with longer fever duration (Table 4), which, in turn, was associated with an increased total number of units transfused (Pearson correlation 0.448, p-value 0.015).
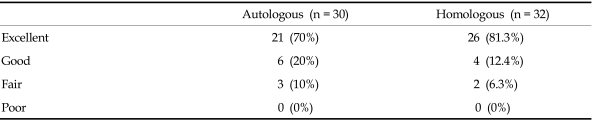
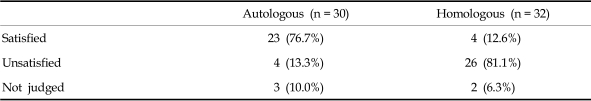
No differences were found in improvement of postoperative clinical results or fusion rates, but autologous transfusion was associated with increased satisfaction (Table 5, 6).
Table 5.
Postoperative Clinical Results of Patients with Autologous and Homologous Transfusion
Chi-Square test, p value = 0.710.
Table 6.
Overall Satisfaction for Transfusion in the Autologous and Homologous Transfused Groups
Chi-square test, p value = 0.001.
DISCUSSION
The purpose of this study is to determine whether differences in postoperative infection and clinical results occurred between those receiving autologous or homologous transfusion during spinal fusion.
Most large series evaluating postoperative wound infection in spinal surgery report an overall rate of less than 1%.33-35 The incidence of postoperative wound infections depends on operative methods, times, and preoperative conditions; it decreases with simple procedures, good vascularity, and prophylactic systemic antibiotics, and increases with more fusions. Instrumented spinal fusion procedures involve more extensive soft tissue dissection, longer operative times, greater blood loss, greater dead space, and increased soft tissue damage from poor vascularity.35 We targeted patients with instrumented procedures because of the greater possibility of postoperative infection.
Triulzi et al.36 reported that patients who received both types of transfusions had a significantly greater rate of postoperative bacterial infection, compared to those with autologous blood only, 20.8% vs. 3.3%, respectively. Among patients with postoperative bacterial infections, surgery to address scoliosis was the most common surgical procedure (6/8) used in this study.36 Usually, the scoliosis surgical procedure results in larger blood loss volumes than in spinal stenosis and spondylolisthesis surgical procedures. In these cases, autologous transfusion is usually not sufficient for replacement, and additional homologous blood is usually required.37 Therefore, we targeted spinal fusion for spinal stenosis or spondylolisthesis, as homologous transfusion after autologous transfusion is usually not needed in such cases.
As postoperative wound infection in spinal surgery is less than 1%, we evaluated postoperative infection, including wound infection, pneumonia, urinary tract infection, cellulitis, and viral disease.
There has been reported increase risk of postoperative infection in patients receiving homologous blood, compared to those receiving autologous blood, in orthopaedic24 and hip arthroplastic surgeries.25 Triulzi et al.36 reported an increased rate of postoperative bacterial infection in patients who received homologous blood, compared to those who received no blood (20.8 vs. 4.0%). Increased postoperative infection during homologous transfusion was correlated with a higher level of plasma immunosuppressive factor,38 drop in natural killer cells,36 decrease in the number of auxiliary CD4 lymphocytes,39 increase in the number of CD8 suppressor lymphocytes, 39 and suppressed cell-mediated immunity.40
However, in our report, no differences were found among cases of postoperative infections, including wound infection, pneumonia, urinary tract infection, and cellulites. Recipients of homologous blood were not at increased risk of infection, compared to autologous blood recipients in a study evaluating hysterectomies.23 In cases of suppressed immunity, such as burn incidents, sepsis, or trauma, it was found that homologous transfusions were immunosuppressive.41-43 However, it has been demonstrated that homologous transfusions produced mild immunostimulation in cases of normal immunity in an untraumatized, nonseptic rodent model.44 It is also reported that postoperative wound infection is affected mainly by systemic immunosuppression, such as occurs in trauma and sepsis.44 Many studies report that postoperative wound infection is common in immunosuppressed patients.27,41-43,45
No differences in incidence of fever without source was found, but homologous transfusion was associated with longer fever duration. Non-hemolytic febrile transfusion reactions and febrile allergic reactions are more common with homologous than autologous transfusion but do not generally result in serious morbidity.46 Murphy et al.25 reported that patients who received homologous blood and those who received autologous blood did not differ in total number of transfused units and fever duration (1.1 vs. 1.3 days). Differences in our report may be because the total number of transfused units was greater in patients with homologous than autologous transfusion.
The common outcome predictors of surgery for spinal stenosis are preoperative walking ability, co-morbidity, such as cardiovascular disease, and increased dural sac cross-sectional area by decompression.47,48 No differences were found in postoperative clinical results, because autologous transfusion likely did not improve walking ability and cardiovascular function. However, autologous transfusion was associated with increased satisfaction since it decreased total number of units transfused and fever duration.
Limitations of this retrospective and comparative study include a non-randomized design, as patients were not allowed to donate at low hemoglobin values.
Our finding suggests that autologous transfusion does not result in decreased incidence of postoperative infection. However, its use may enhance recovery to the level of average daily living activity by increasing satisfaction due to fewer total units transfused and shorter fever duration.
Footnotes
This work was supported in part by Brain Korea 21 Project, Yonsei University College of Medicine.
References
- 1.Tobias JD. Strategies for minimizing blood loss in orthopedic surgery. Semin Hematol. 2004;41(1) Suppl 1:145–156. doi: 10.1053/j.seminhematol.2003.11.025. [DOI] [PubMed] [Google Scholar]
- 2.Pouliquen JC, Jean N, Noat M, Boyer JM, Yannoutsos H. Blood saving in pediatric orthopedics. A study of 145 posterior vertebral arthrodesis. Chirurgie. 1990;116:303–311. [PubMed] [Google Scholar]
- 3.Johnson RG, Murphy M, Miller M. Fusions and transfusions. An analysis of blood loss and autologous replacement during lumbar fusions. Spine. 1989;14:358–362. [PubMed] [Google Scholar]
- 4.Guay J, Haig M, Lortie L, Guertin MC, Poitras B. Predicting blood loss in surgery for idiopathic scoliosis. Can J Anaesth. 1994;41:775–781. doi: 10.1007/BF03011583. [DOI] [PubMed] [Google Scholar]
- 5.Klein HG. Allogeneic transfusion risks in the surgical patient. Am J Surg. 1995;170(6A) Suppl:21S–26S. doi: 10.1016/s0002-9610(99)80054-3. [DOI] [PubMed] [Google Scholar]
- 6.Goodnough LT, Brecher ME, Kanter MH, AuBuchon JP. Transfusion medicine. Second of two parts--blood conservation. N Engl J Med. 1999;340:525–533. doi: 10.1056/NEJM199902183400706. [DOI] [PubMed] [Google Scholar]
- 7.Rubio Martinez A, Garcia Erce JA, Solano Bernad VM, Lallana Dupla JJ, Salvador Osuna C, Gimeno Lozano JJ. Transfusion and pre-deposit autotransfusion in orthopedic and traumatologic surgery. Sangre (Barc) 1999;44:335–341. [PubMed] [Google Scholar]
- 8.Gandini G, Franchini M, de Gironcoli M, Giuffrida A, Bertuzzo D, Zanolla L, et al. Preoperative autologous blood donation by elderly patients undergoing orthopaedic surgery. Vox Sang. 2001;80:95–100. doi: 10.1046/j.1423-0410.2001.00020.x. [DOI] [PubMed] [Google Scholar]
- 9.Bernstein LH, Coles M, Granata A. The Bridgeport Hospital experience with autologous transfusion in orthopedic surgery. Orthopedics. 1997;20:677–680. doi: 10.3928/0147-7447-19970801-05. [DOI] [PubMed] [Google Scholar]
- 10.Baghdadi H, Hemon Y, Aubaniac JM, Argenson JN, Gouin F. Transfusion strategy in programmed hemorrhagic orthopedic surgery. Presse Med. 1996;25:55–58. [PubMed] [Google Scholar]
- 11.Pinkerton PH. Use of autologous blood in support of orthopaedic surgery using a hospital-based autologous donor programme. Transfus Med. 1995;5:139–144. doi: 10.1111/j.1365-3148.1995.tb00202.x. [DOI] [PubMed] [Google Scholar]
- 12.Thomson JD, Callaghan JJ, Savory CG, Stanton RP, Pierce RN. Prior deposition of autologous blood in elective orthopaedic surgery. J Bone Joint Surg Am. 1987;69:320–324. [PubMed] [Google Scholar]
- 13.Dorang LA, Klebanoff G, Kemmerer WT. Autotransfusion in long-segment spinal fusion. An experimental model to demonstrate the efficacy of salvaging blood contaminated with bone fragments and marrow. Am J Surg. 1972;123:686–688. doi: 10.1016/0002-9610(72)90354-6. [DOI] [PubMed] [Google Scholar]
- 14.Siller TA, Dickson JH, Erwin WD. Efficacy and cost considerations of intraoperative autologous transfusion in spinal fusion for idiopathic scoliosis with predeposited blood. Spine. 1996;21:848–852. doi: 10.1097/00007632-199604010-00015. [DOI] [PubMed] [Google Scholar]
- 15.Park KS, Lim YJ, Do SH, Min SW, Kim CS, Lee JH, et al. Combined use of autologous transfusion techniques to avoid allogeneic transfusion in spinal fusion surgery with instrumentation. Int J Clin Pract. 2004;58:260–263. doi: 10.1111/j.1368-5031.2004.0029.x. [DOI] [PubMed] [Google Scholar]
- 16.Flynn JM, Nieves R. The use of intraoperative autotransfusion as a second stage of autologous blood use in pediatric orthopaedic surgery. P R Health Sci J. 1995;14:259–262. [PubMed] [Google Scholar]
- 17.Goodnough LT, Marcus RE. Effect of autologous blood donation in patients undergoing elective spine surgery. Spine. 1992;17:172–175. doi: 10.1097/00007632-199202000-00009. [DOI] [PubMed] [Google Scholar]
- 18.Oga M, Ikuta H, Sugioka Y. The use of autologous blood in the surgical treatment of spinal disorders. Spine. 1992;17:1381–1385. doi: 10.1097/00007632-199211000-00019. [DOI] [PubMed] [Google Scholar]
- 19.Mandel RJ, Brown MD, McCollough NC, 3rd, Pallares V, Varlotta R. Hypotensive anesthesia and autotransfusion in spinal surgery. Clin Orthop Relat Res. 1981;154:27–33. [PubMed] [Google Scholar]
- 20.Copley LA, Richards BS, Safavi FZ, Newton PO. Hemodilution as a method to reduce transfusion requirements in adolescent spine fusion surgery. Spine. 1999;24:219–224. doi: 10.1097/00007632-199902010-00005. [DOI] [PubMed] [Google Scholar]
- 21.Albert TJ, Desai D, McIntosh T, Lamb D, Balderston RA. Early versus late replacement of autotransfused blood in elective spinal surgery. A prospective randomized study. Spine. 1993;18:1071–1078. doi: 10.1097/00007632-199306150-00018. [DOI] [PubMed] [Google Scholar]
- 22.Blais RE, Hadjipavlou AG, Shulman G. Efficacy of autotransfusion in spine surgery: comparison of autotransfusion alone and with hemodilution and apheresis. Spine. 1996;21:2795–2800. doi: 10.1097/00007632-199612010-00016. [DOI] [PubMed] [Google Scholar]
- 23.Sauaia A, Alexander W, Moore EE, Stevens BR, Rosen H, Dunn TR. Autologous blood transfusion does not reduce postoperative infection rates in elective surgery. Am J Surg. 1999;178:549–555. doi: 10.1016/s0002-9610(99)00242-1. [DOI] [PubMed] [Google Scholar]
- 24.Fernandez MC, Gottlieb M, Menitove JE. Blood transfusion and postoperative infection in orthopedic patients. Transfusion. 1992;32:318–322. doi: 10.1046/j.1537-2995.1992.32492263444.x. [DOI] [PubMed] [Google Scholar]
- 25.Murphy P, Heal JM, Blumberg N. Infection or suspected infection after hip replacement surgery with autologous or homologous blood transfusions. Transfusion. 1991;31:212–217. doi: 10.1046/j.1537-2995.1991.31391165169.x. [DOI] [PubMed] [Google Scholar]
- 26.Practice Guidelines for blood component therapy: A report by the American Society of Anesthesiologists Task Force on Blood Component Therapy. Anesthesiology. 1996;84:732–747. [PubMed] [Google Scholar]
- 27.Tartter PI. Blood transfusion and infectious complications following colorectal cancer surgery. Br J Surg. 1988;75:789–792. doi: 10.1002/bjs.1800750822. [DOI] [PubMed] [Google Scholar]
- 28.Tartter PI, Driefuss RM, Malon AM, Heimann TM, Aufses AH. Relationship of postoperative septic complications and blood transfusions in patients with Crohn's disease. Am J Surg. 1988;155:43–48. doi: 10.1016/s0002-9610(88)80256-3. [DOI] [PubMed] [Google Scholar]
- 29.Kim NH, Lee JW. Anterior interbody fusion versus posterolateral fusion with transpedicular fixation for isthmic spondylolisthesis in adults. A comparison of clinical results. Spine. 1999;24:812–817. doi: 10.1097/00007632-199904150-00014. [DOI] [PubMed] [Google Scholar]
- 30.Christensen FB, Laursen M, Gelineck J, Eiskjaer SP, Thomsen K, Bunger CE. Interobserver and intraobserver agreement of radiograph interpretation with and without pedicle screw implants: the need for a detailed classification system in posterolateral spinal fusion. Spine. 2001;26:538–544. doi: 10.1097/00007632-200103010-00018. [DOI] [PubMed] [Google Scholar]
- 31.Stauffer RN, Coventry MB. Posterolateral lumbar-spine fusion. Analysis of Mayo Clinic series. J Bone Joint Surg Am. 1972;54:1195–1204. [PubMed] [Google Scholar]
- 32.Mader JT, Cierny G., 3rd The principles of the use of preventive antibiotics. Clin Orthop. 1984;190:75–82. [PubMed] [Google Scholar]
- 33.El-Gindi S, Aref S, Salama M, Andrew J. Infection of intervertebral discs after operation. J Bone Joint Surg Br. 1976;58:114–116. doi: 10.1302/0301-620X.58B1.1270487. [DOI] [PubMed] [Google Scholar]
- 34.Horwitz NH, Curtin JA. Prophylactic antibiotics and wound infections following laminectomy for lumber disc herniation. J Neurosurg. 1975;43:727–731. doi: 10.3171/jns.1975.43.6.0727. [DOI] [PubMed] [Google Scholar]
- 35.Heller JG, Levine MJ. Postoperative infections of spine. In: Rothman RH, Simone FA, editors. Spine. 4th ed. Vol. 2. Philadelphia: WB Saunders Co; 1999. pp. 1671–1686. [Google Scholar]
- 36.Triulzi DJ, Vanek K, Ryan DH, Blumberg N. A clinical and immunologic study of blood transfusion and postoperative bacterial infection in spinal surgery. Transfusion. 1992;32:517–524. doi: 10.1046/j.1537-2995.1992.32692367194.x. [DOI] [PubMed] [Google Scholar]
- 37.Murray DJ, Forbes RB, Titone MB, Weinstein SL. Transfusion management in pediatric and adolescent scoliosis surgery. Efficacy of autologous blood. Spine. 1997;22:2735–2740. doi: 10.1097/00007632-199712010-00007. [DOI] [PubMed] [Google Scholar]
- 38.Shenton BK, Proud G, Smith BM, Taylor RM. Identification of immunosuppressive factors in plasma following multiple blood transfusions. Transplant Proc. 1979;11:171–174. [PubMed] [Google Scholar]
- 39.Boileau S, Hoffmann S, Janot C, Grosdidier G, Laxenaire MC. Comparative study of immunologic consequences of autotransfusion and homologous transfusion in lung cancer surgery. Ann Fr Anesth Reanim. 1993;12:251–259. doi: 10.1016/s0750-7658(05)80650-1. [DOI] [PubMed] [Google Scholar]
- 40.Fischer E, Lenhard V, Seifert P, Kluge A, Johannsen R. Blood transfusion-induced suppression of cellular immunity in man. Hum Immunol. 1980;1:187–194. doi: 10.1016/0198-8859(80)90013-0. [DOI] [PubMed] [Google Scholar]
- 41.Waymack JP, Balakrishnan K, McNeal N, Gonce S, Miskell P, Warden GD, et al. Effect of blood transfusions on macrophage-lymphocyte interaction in an animal model. Ann Surg. 1986;204:681–685. doi: 10.1097/00000658-198612000-00011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Waymack JP, Gallon L, Barcelli U, Alexander JW. Effect of blood transfusions on macrophage function in a burned animal model. Curr Surg. 1986;43:305–307. [PubMed] [Google Scholar]
- 43.Waymack JP, Rapien J, Garnett D, Tweddell JS, Alexander JW. Effect of transfusion on immune function in a traumatized animal model. Arch Surg. 1986;121:50–55. doi: 10.1001/archsurg.1986.01400010056007. [DOI] [PubMed] [Google Scholar]
- 44.Brunson ME, Ing R, Tchervenkov JI, Alexander JW. Variable infection risk following allogeneic blood transfusions. J Surg Res. 1990;48:308–312. doi: 10.1016/0022-4804(90)90064-9. [DOI] [PubMed] [Google Scholar]
- 45.Graves TA, Cioffi WG, Mason AD, Jr, McManus WF, Pruitt BA., Jr Relationship of transfusion and infection in a burn population. J Trauma. 1989;29:948–952. doi: 10.1097/00005373-198907000-00007. [DOI] [PubMed] [Google Scholar]
- 46.Snyder EL. Transfusion reaction. In: Hoffman R, Benz EJ, Shattil SJ, Furie B, Cohen HJ, Silberstein LE, editors. Hematology. 2nd ed. New York: Churchill Livingstone Inc.; 1995. pp. 2045–2053. [Google Scholar]
- 47.Katz JN, Stucki G, Lipson SJ, Fossel AH, Grobler LJ, Weinstein JN. Predictors of surgical outcome in degenerative lumbar spinal stenosis. Spine. 1999;24:2229–2233. doi: 10.1097/00007632-199911010-00010. [DOI] [PubMed] [Google Scholar]
- 48.Mariconda M, Zanforlino G, Celestino GA, Brancaleone S, Fava R, Milano C. Factors influencing the outcome of degenerative lumbar spinal stenosis. J Spinal Disord. 2000;13:131–137. doi: 10.1097/00002517-200004000-00007. [DOI] [PubMed] [Google Scholar]