Abstract
Background
Delays in accessing care for young people with a first episode of psychosis are significantly associated with poorer treatment response and higher relapse rates.
Aim
To assess the effect of an educational intervention for GPs on referral rates to early-intervention services and the duration of untreated psychosis for young people with first-episode psychosis.
Design of study
Stratified cluster randomised controlled trial, clustered at practice level.
Setting
Birmingham, England.
Method
Practices with access to the three early-intervention services in three inner-city primary care trusts in Birmingham were eligible for inclusion. Intervention practices received an educational intervention addressing GP knowledge, skills, and attitudes about first-episode psychosis. The primary outcome was the difference in the number of referrals to early-intervention services between practices. Secondary outcomes were duration of untreated psychosis, time to recovery, use of the Mental Health Act, and GP consultation rate during the developing illness.
Results
A total of 110 of 135 eligible practices (81%) were recruited; 179 young people were referred, 97 from intervention and 82 from control practices. The relative risk of referral was not significant: 1.20 (95% confidence interval [CI] = 0.74 to 1.95; P = 0.48). No effect was observed on secondary outcomes except for ‘delay in reaching early-intervention services’, which was statistically significantly shorter in patients registered in intervention practices (95% CI = 83.5 to 360.5; P = 0.002).
Conclusion
GP training on first-episode psychosis is insufficient to alter referral rates to early-intervention services or reduce the duration of untreated psychosis; however, there is a suggestion that training facilitates access to the new specialist teams for early psychosis.
Keywords: education, primary health care, psychosis
INTRODUCTION
During the last two decades, the importance of intervening as early as possible when a young person develops a first episode of psychosis has become accepted internationally. This has been underpinned by studies demonstrating that young people with first-episode psychosis experience lengthy delays between the onset of psychotic symptoms and receipt of treatment (duration of untreated psychosis) of up to 2 years,1–3 and that delays in accessing care are significantly associated with poorer treatment response.4
There is a limited evidence base in this area of primary care, but GPs may be key to the identification and management of first-episode psychosis, as they are usually the first point of patient contact,5 their involvement in the management of psychosis is associated with a reduction of the use of the Mental Health Act,6 and they are the most common final referral agent to early-intervention services.7 However, early detection presents challenges as psychosis can take several months to emerge,8 and may be difficult to distinguish from normal adolescent behaviour and substance misuse.9,10 There can be changes in presentation during the early phase,11 which may lead to diagnostic caution among GPs.
The perceived and actual stigma of mental illness may also impede help seeking and lead to a form of ‘collusion’ between the patient, carer/family member, and GP, so that the diagnosis is not openly raised, or other less-stigmatising diagnoses considered. There is also evidence that a majority of GPs have no postgraduate mental health training; that they often have negative opinions about providing care for people with schizophrenia;12 that they believe they contribute little to the care of people with serious mental illness in general; and that the incidence of first-episode psychosis is too low to warrant more active involvement.13 A training-needs analysis devised and distributed by the current study team to GPs across Birmingham also identified knowledge uncertainties around diagnosing first-episode psychosis and worries on how to phrase questions about hallucinations.14 Together, these data suggest reasons why the duration of untreated psychosis is so long and the potential importance of training GPs to improve the early detection of first-episode psychosis. GPs also need swift access to specialist services if they are going to play a role in reducing the duration of untreated psychosis.
An evidence-based intervention that addressed knowledge, skills, and attitudes of GPs about a first episode of psychosis was therefore developed. The intervention was evaluated in a stratified-cluster randomised controlled trial, clustered at practice level. It was hypothesised that although incidence would not change, the intervention would sensitise GPs to the diagnosis, and therefore potentially increase referral rates of young people to early-intervention services from this sector of the health and welfare system. It was also hypothesised that GPs in the intervention group would prospectively diagnose young people with first-episode psychosis at an earlier stage in the illness and, therefore, in the longer term decrease the duration of untreated psychosis. There was a possibility that, due to detection bias (that is, GPs in the intervention group identifying young people, some of whom had had the diagnosis for some time15), cases in the control group might have a shorter duration of untreated psychosis during this trial. For these reasons, the number of people referred was chosen as a primary outcome, and the duration of untreated psychosis as one of the secondary outcomes.
METHOD
Participants
The REDIRECT trial (BiRmingham Early Detection In untREated psyChosis Trial) was conducted in practices in three inner-city primary care trusts (PCTs) in Birmingham, England. Practices were eligible if they had access to early-intervention services. Consecutive patients with first-episode psychosis referred to early-intervention services with a diagnosis of psychosis over a 3-year period from April 2004 to February 2007 were eligible for inclusion. Patients were aged between 14 and 30 years, in line with policy guidance,16 and had an International Classification of Diseases (ICD-1017) chart diagnosis of schizophrenia or related disorders, such as a persistent delusional disorder. Exclusion criteria were patients with a primary diagnosis of substance use disorder, mood disorder, or organic mental disorder, current criminal proceedings, serious concurrent physical illness, institutional residence, learning disability, or inability to provide informed consent.
How this fits in
Young people with a first episode of psychosis experience delays of up to 2 years between the onset of psychotic symptoms and receipt of treatment, even though delays in accessing care are significantly associated with poorer treatment response and higher relapse rates. GPs are usually the first point of patient contact on the illness pathway. GP training on first-episode psychosis alone is not sufficient to alter referral rates to early-intervention services or reduce the duration of untreated psychosis; however, delay in reaching early-intervention services was shorter in patients registered with intervention practices (95% confidence interval 83.5 to 360.5; P = 0.002). GP training may be an important component of a broader community approach to the treatment of young people with psychosis.
Practice recruitment occurred in three waves, as new early-intervention services opened across the city and therefore more practices became eligible to participate. Practices were randomised to receive either the intervention on detecting first-episode psychosis or to be part of the control group.
Intervention
In developing the intervention, the study team followed the framework proposed by the Medical Research Council,18,19 and also incorporated evidence from systematic reviews and guidelines on changing professional practice.20 The framework provides guidance on using a stepped approach to the development and evaluation of complex interventions in health care. This phased approach separates the different questions being asked and helps researchers to establish the probable active components of an intervention. The educational intervention was ‘complex’, in that it comprises a number of interconnected components that are likely to interact with one another. In the context of this study, in phase 0 (the theoretical phase) a formal literature review of the format, content, and effectiveness of previous educational programmes in primary care was undertaken; and the psychological literature on attitude formation and change and the relationship between attitudes and behaviour was reviewed. Phase 1 included qualitative and quantitative evaluations through focus groups and a training-needs analysis questionnaire to identify GP attitudes and behaviours towards people with first-episode psychosis, and organisational factors that might help tailor the educational intervention to the primary care setting. The outcome of the theoretical and modelling work suggested that the educational intervention needed to impart knowledge about important symptoms and signs evident in first-episode psychosis, teach core questioning skills, and encourage more positive attitudes towards young people with the condition.
A 17-minute video made specifically for the study, depicting role-played primary care consultations with young people with first-episode psychosis, was shown to GPs in intervention practices. The video included specific messages, for example about links between substance misuse and psychosis, the importance of listening to parental concerns and, above all, to refer early to early-intervention services if there were concerns. The study team then led a 15-minute question and answer session including referral guidelines to early-intervention services. GPs in the first wave of practices viewed the video between November 2003 and January 2004, in the second wave between April and May 2005, and in the third wave between April and May 2006.
Two refresher educational sessions were conducted in small groups for the first-wave intervention practices between June and July 2004 and then between July and November 2005. Second-wave intervention practices had one refresher session between July and November 2005. Third-wave practices did not have a refresher session, as the study closed within 8 months of their recruitment. The first refresher training consisted of personal testimonies from two service users, one of whom also made a video of her experience. The second refresher session was led by a GP and carer, and stressed the importance of family support.
Outcome measures
The primary outcome was the difference in number of referrals to early-intervention services of young people with first-episode psychosis between intervention and control practices. This was chosen because, as described earlier, it was hypothesised that education would sensitise GPs to the diagnosis, and therefore more people with the diagnosis, some of whom may have been unwell and untreated for some time, would be referred to early-intervention services in the intervention group. Secondary outcomes were duration of untreated psychosis, time to recovery, use of the Mental Health Act, and GP consultation rate during the time between the intervention and point of referral to a mental health team.21
Eligible patients were interviewed by the research team at baseline and at 4 months' follow-up. At baseline, data were collected on sociodemographic factors and psychosis symptoms during the first episode using the Schedules for Clinical Assessment in Neuropsychiatry (SCAN) version 2.0.22 Insight (a patient's awareness of an illness, of a need for treatment, and attribution of symptoms) was measured at baseline and at 4 months, as part of the assessment of recovery, with the Insight Scale.23 The Early Signs Scale24 was used at baseline and at 4 months to assess at-risk mental states and provide a measure of clinical recovery; the scale has been used to measure both the build up to and recovery from, an acute psychotic episode. Psychotic symptoms were measured at baseline and at 4 months with the Positive and Negative Syndrome Scale (PANSS).25 The scale was also used as part of the assessment of recovery. Duration of untreated psychosis was assessed at baseline with a semi-structured interview following the model of Beiser et al.26 It was defined as the time interval between the onset of psychotic symptoms and the initiation of treatment with neuroleptic medication, and calculated according to a stringent protocol adapted from criteria developed by Larsen et al.27 Premorbid functioning was assessed at baseline with the Premorbid Adjustment Scale.28 Pathways to care (routes of contact with and through health services) were measured at baseline with the Encounter form.29 This instrument was also used to determine GP consultation and referral rates.
Inter-rater reliability maintenance checks of PANSS and SCAN were conducted on one occasion during the study to avoid drift in scoring over time.
Sample size
As the practices, rather than their patients, were the subjects of the study, the statistical analysis and power calculation accounted for this. Assuming the standard critical value for α (two-sided P = 0.05), and that, on average, two referrals would be made in control practices in the study period, and that the variance for between-practice variability is one, the study had 80% power (1–β) to detect a mean difference of 1.2 referrals between intervention and control practices (relative risk 1.6), and 90% power (1–β) to detect a mean difference of 1.4 referrals (relative risk 1.7), which was felt to be clinically important by the clinicians involved in the trial. This meant that 160 individuals with first-episode psychosis needed to be recruited for the study to be fully powered. Minimal attrition was accounted for, based on the relatively short follow-up period.
Once practices had been recruited, they were randomly allocated using a computer-based algorithm to either intervention or control groups by one of the investigators who was blind to practice identity. Practices were stratified by list size (more or fewer than 3500 patients) and PCT (Heart of Birmingham or not), to ensure balance on the number of practices where no referrals of first-episode psychosis might occur, and to account for the differential prevalence of first-episode psychosis across the study area.
All study personnel with patient contact, and participants, were blind to treatment assignment for the duration of the study.
Analysis
The effect of the intervention on the primary outcome was estimated using a non-linear mixed model, where the number of referrals per practice was modelled using Poisson error. Overdispersion (extra-Poissonian variability) was accounted for by defining the practice as a random effect.30 Analyses were conducted using Proc Nlmixed in the SAS statistical programme (version 9.1). Secondary outcomes were analysed using a mixed modelling strategy, accounting for between-practice variability by defining practices as random effects. As the subject of the experiment was the practice, the denominator degrees of freedom for the analysis were derived from that stratum. No subgroup analyses were prespecified.
RESULTS
Patients were recruited from April 2004 until February 2007, with a 4-month follow-up. During the study lifetime, 135 general practices within three PCTs able to refer to early-intervention services were eligible for inclusion in the trial. Practices were recruited over three time periods, as further early-intervention services opened and therefore more practices became eligible to enter the study.31 Characteristics of participating practices are summarised in Table 1.
Table 1.
Characteristics of study practices.
| Characteristics | Intervention practices (n = 55) | Control practices (n = 55) |
|---|---|---|
| Number of partners | ||
| 1 | 23 | 26 |
| 2–3 | 22 | 24 |
| 4–6 | 9 | 2 |
| ≥7 | 1 | 1 |
| List size | ||
| <3000 | 21 | 17 |
| 3000–5999 | 24 | 31 |
| 6000–8999 | 8 | 5 |
| ≥9000 | 2 | 2 |
Sixty-two of a possible 93 GPs working in each of the first wave of 39 intervention practices participated in the initial educational session between November 2003 and January 2004. At least one GP in each participating practice attended the session. Forty-three GPs in 27 (69%) practices participated in the booster educational sessions in June and July 2004, and 21 practices (50%) in July and November 2005.
Although GPs had direct access to early-intervention services, as part of the study protocol, all referral letters to the 14 mental health teams in Birmingham who could have acted as conduits on the referral path to early-intervention services were audited. This process, which was included to identify ‘false-positive’ referrals as a possible adverse consequence of the educational sessions, began in January 2004 and reviewed referrals for the previous 6 months, to gain a baseline value prior to patient recruitment, and continued until May 2006 when figures had been stable for 12 months. As part of the process, it was noted that a number of young people referred with probable first-episode psychosis, and subsequently diagnosed as such, were never transferred on to an early-intervention service. However, these individuals were patients in participating practices and had been referred with the diagnosis of probable first-episode psychosis; therefore, they were eligible to form part of the primary outcome. After discussion with the data monitoring committee, a pragmatic decision was made to include them in the study. These patients had not consented to participate in the trial and so no secondary outcome data were available. Routinely collected demographic details were available from the mental health team databases.
A total of 179 patients were referred and therefore eligible to form part of the primary outcome from 110 practices; 97 patients were registered in intervention and 82 in control practices. Of the 179 referred patients, 125 were recruited from the early-intervention services, and 54 were found to be eligible for inclusion during the mental health team notes audit. Eighty-three patients provided secondary outcome data, and 68 of these were followed up at 4 months (Figure 1). Basic demographic data from early-intervention and community mental health team notes were available on 123 participants, with detailed data on 83 patients (Table 2).
Figure 1.
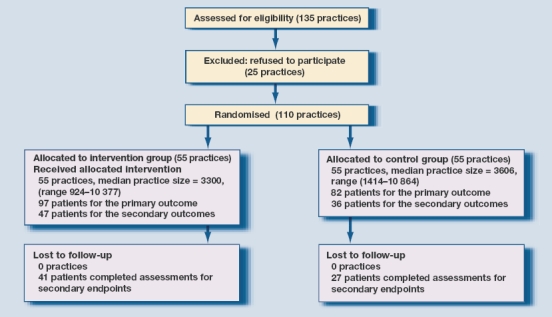
Trial flow diagram
Table 2.
Baseline characteristics of participants
| Intervention (n = 65) | Control (n = 58a) | |
|---|---|---|
| Mean age, years (SD)b | 21.6 (3.7) | 22.7 (3.8) |
| Sex, n (%)c | ||
| Female | 22 (18.7) | 20 (17.0) |
| Male | 39 (33.1) | 37 (31.4) |
| Employment status, n (%)d | ||
| In employment | 9 (11.0) | 3(3.7) |
| Student | 12 (14.6) | 5 (6.1) |
| Unemployed | 25 (30.5) | 28 (34.2) |
| Living arrangements, n (%)e | ||
| Living with parents | 32 (39.0) | 26 (31.7) |
| Living alone | 7(8.5) | 7 (8.5) |
| Marital status, n (%)f | ||
| Married | 4 (4.9) | 5 (6.1) |
| Single | 40 (48.9) | 30 (36.6) |
| Ethnicity, n (%)g | ||
| Asian | 33 (28.7) | 29 (25.2) |
| White | 7 (6.1) | 6 (5.2) |
| Black | 20 (17.4) | 16 (13.9) |
| Other | 1(0.9) | 3 (2.6) |
| Primary ICD-10 diagnosis, n (%)h | ||
| Schizophrenia F20 | 21 (25.3) | 16 (19.3) |
| Other non-organic psychotic, n (%)h | ||
| Disorder F28 (other non-organic psychotic disorders) | 21 (25.3) | 16 (19.3) |
| Simple schizophrenia F22 | 2 (2.4) | 0 (0) |
| Other | 4 (4.8) | 3 (3.6) |
Missing demographic data for two patients.
Denominator = 114 for age.
Denominator = 118 for sex.
Denominator = 82 for employment status.
Denominator = 82 for living arrangements.
Denominator = 82 for marital status.
Denominator = 115 for ethnicity.
Denominator = 83 for diagnosis. ICD = International Classification of Diseases.
Primary outcome
Ninety-seven people with a first episode of psychosis were referred by intervention practices, and 82 people from control practices during the study: relative risk of referral 1.20 (95% confidence interval [CI] 0.74 to 1.95; P = 0.48).
Secondary outcomes
No effect was observed on any secondary outcome except for one component of duration of untreated psychosis (Table 3). Eight people were detained under the Mental Health Act in the control group of 71 patients (11.3%), and 13 in the intervention group of 87 people (14.9%; P = 0.79). Recovery was initially analysed using the scores on the positive subscale of the PANSS. Remission was defined as a score below 10. Twenty-two of the 36 patients (64.4%) in the control group, and 26 of the 47 patients (55.3%) in the intervention group met these criteria for recovery (P = 0.66). In view of the lack of difference, further analysis was not undertaken.
Table 3.
Results of secondary outcomes.
| Comparison | Difference | 95% CI | P-value |
|---|---|---|---|
| Delay in help seeking | −105.97 | −267.49 to 55.56 | 0.19 |
| Delay in help-seeking pathway | 4.07 | −51.51 to 59.65 | 0.88 |
| Delay in reaching early-intervention service | 222.03 | 83.54 to 360.52 | 0.002 |
| Delay within mental health services | 87.34 | −22.45 to 197.14 | 0.13 |
| Duration of prodromal period | 59.34 | −290.21 to 408.89 | 0.74 |
| Duration of untreated illness | 187.23 | −106.26 to 480.73 | 0.21 |
| Duration of untreated psychosis | −13.78 | −199.12 to 171.57 | 0.88 |
| Early Signs Scale24 | |||
| T1 | −2.62 | −13.17 to 7.93 | 0.62 |
| T2 | 0.68 | −5.85 to 7.21 | 0.84 |
| Insight Scale23 | |||
| T1 | 1.01 | −1.29 to 3.31 | 0.38 |
| T2 | 0.84 | −1.41 to 3.08 | 0.45 |
| Premorbid Adjustment Scale (PAS)28 | −4.99 | −18.90 to 8.93 | 0.46 |
| Child PAS | −1.16 | −2.92 to 0.61 | 0.19 |
| Early adolescent PAS | −1.25 | −3.45 to 0.95 | 0.26 |
| Late adolescent PAS | −1.31 | −4.16 to 1.55 | 0.36 |
| Adulthood PAS | −0.60 | −3.30 to 2.10 | 0.65 |
| General PAS | −1.99 | −6.92 to 2.95 | 0.41 |
| Positive and Negative Syndrome Scale (PANSS)25 | |||
| Total PANSS T1 | −3.34 | −11.42 to 4.74 | 0.41 |
| General PANSS T1 | −1.74 | −6.10 to 2.62 | 0.42 |
| Negative PANSS T1 | −0.12 | −3.49 to 3.25 | 0.94 |
| Positive PANSS T1 | −1.37 | −4.11 to 1.36 | 0.32 |
| Total PANSS T2 | −11.89 | −22.98 to −0.80 | 0.04 |
| General PANSS T2 | −6.23 | −11.84 to −0.61 | 0.03 |
| Negative PANSS T2 | −3.79 | −7.40 to −0.18 | 0.04 |
| Positive PANSS T2 | −1.88 | −4.54 to 0.79 | 0.16 |
T1 = time 1 data collection point. T2 = time 2 data collection point.
The number of consultations in primary care following the intervention was assessed from the pathways to care protocol. Data were available for 68 participants. Twenty-eight patients in the control group had 21 visits to their GP after the training sessions date, and 40 in the treatment group had a total of 39 visits. The relative risk between the groups was 0.77 (95% CI = 0.45 to 1.33; P = 0.34).
Mean duration of untreated psychosis was 247.1 days (median 56.5 days, standard deviation [SD] = 454.2) for patients registered in intervention practices, and 234.2 days (median 71.0 days, SD = 290.0) in the control group. However, delay in reaching early-intervention services, defined as the time from the first decision to seek care to the point of referral to an early-intervention service, was much shorter in patients registered in intervention practices, with a mean of 143.1 days (median 61.0 days, SD = 192.8) compared to 366.9 days (median 181.5 days, SD = 388.8) for patients registered in control practices (95% CI = 83.5 to 360.5; P = 0.002). It is interesting to note that the mean delay within mental health services was shorter in people registered in intervention practices, although this did not achieve statistical significance (P = 0.12).
Analysis of pathways to care data also found that GPs were the most frequent first and final point of contact into services (Table 4).
Table 4.
Pathways to care.
| Care pathway | Intervention (n = 40) | Control (n = 28) | Total (n = 68) |
|---|---|---|---|
| First point of contact, n (% total first contacts) | |||
| GP | 27 (39.7) | 13 (19.1) | 40 (58.8) |
| Accident and emergency | 5 (7.3) | 6 (8.8) | 11 (16.2) |
| Police | 3 (4.4) | 4 (5.9) | 7 (10.3) |
| Religious leader | 2 (2.9) | 0 (0) | 2 (2.9) |
| Psychiatrist | 1 (1.5) | 1 (1.5) | 2 (2.9) |
| Psychiatric hospital | 1 (1.5) | 0 (0) | 1 (1.5) |
| Primary care liaison mental health team | 0 (0) | 1 (1.5) | 1 (1.5) |
| Other | 1 (1.5) | 3 (4.4) | 4 (5.9) |
| Total | 40 (58.8) | 28 (41.2) | 68 (100) |
| Last point of contact before referral to early-intervention service, n (% total last contacts) | |||
| GP | 15 (22.1) | 14 (20.6) | 29 (42.7) |
| Accident and emergency | 3 (4.4) | 2 (2.9) | 5 (7.3) |
| Social services | 2 (2.9) | 1(1.5) | 3 (4.4) |
| Prison | 1 (1.5) | 1 (1.5) | 2 (2.9) |
| Psychiatrist | 2 (2.9) | 0 (0) | 2 (2.9) |
| Psychiatric hospital | 0 (0) | 1 (1.5) | 1 (1.5) |
| Community mental health team | 6 (8.8) | 4 (5.9) | 10 (14.7) |
| Home treatment team | 7 (10.3) | 4 (5.9) | 11 (16.2) |
| Other | 4 (5.9) | 1 (1.5) | 5 (7.4) |
| Total | 40 (58.8) | 28 (41.2) | 68 (100) |
There were no adverse events reported as a result of the trial, and no increase in false-positive referrals from primary care, which remained between 12.7% and 13.4% before and during the study.
DISCUSSION
Summary of main findings
This trial suggests that GPs' training in identification of first-episode psychosis does not alter referral rates to early-intervention services or reduce the duration of untreated psychosis.
The finding on the secondary outcome of much faster access to early-intervention services for patients registered with intervention practices, suggests that these cases were clearly flagged by GPs as requiring specialist care for a first episode of psychosis and that interfaces within secondary care became more permeable. As there is now strong evidence that treatment by an early-intervention service improves outcomes,32 this is an important although exploratory finding, given the overall neutral results from the trial. The long delays within secondary care itself, and the fact that so many young people with a first episode of psychosis appeared to become ‘stuck’ within community mental health teams and were not referred on to early-intervention services, also suggest the educational messages around diagnosis and timely referral could be useful within secondary care.
Strengths and limitations of the study
The main strength of this study lies in its unique position as the first fully powered and tailored trial of the effect of GP education on referral patterns and the duration of untreated psychosis. The practice recruitment and level of commitment to the education sessions was excellent. The intervention was theoretically driven using a combination of strategies,33 and was personalised and delivered in a way that had relevance to those receiving it.34 The video-based nature of the education also makes it easy to disseminate.
Study limitations include the fact that secondary outcome data and some demographic data were not available to the study team. Eighty-three of 179 (46.4%) people completed the study schedules, and 68 of those (81.9%) repeated them at 4 months. Although patients were representative of the wider group of young people with first-episode psychosis in terms of age and sex, there was an over-representation of young people from black and ethnic minority communities, reflecting the study setting and the known epidemiological gradients of psychosis.35 In retrospect, it may also have been better to have used the duration of untreated psychosis as the primary outcome measure, as the trial aimed to facilitate earlier detection and referral of young people with a first episode of psychosis.
Comparison with existing literature
This study supports previous findings that GPs have a key role in the care pathway as young people develop a first episode of psychosis.5 GPs in the current study were by far the most common first and final point of contact in the care pathway, emphasising the need to ensure they are aware of the condition and its treatment.
There have been four published evaluations of early-detection programmes aimed at reducing the duration of untreated psychosis, three of which have included elements of GP training. The Treatment and Intervention in Psychosis study in Norway reported a reduction in duration of untreated psychosis from a mean of 114.2 weeks to 25.3 weeks after the introduction of an intensive community education campaign and access to an early-detection team.36 A community-wide education programme in Canada reported no difference in duration of untreated psychosis as a result of the intervention.37 In Melbourne, Australia a community development campaign that included GP education reported shorter duration of untreated psychosis in the intervention sector once nine patients with a very long duration of untreated psychosis had been excluded from the analysis.38 In London, England, the Lambeth Early Onset Crisis Assessment Team study included a single short training session for 17 of 23 intervention practices who also had direct access to early-intervention services, and found intervention group GPs were more likely to refer their patients to mental health services than control group GPs who had no training and no direct access; but no difference was found in the duration of untreated psychosis between practices.39 This study, the first to focus solely on GP education as a mechanism for increasing referrals and decreasing the duration of untreated psychosis, suggests that education alone is insufficient to make a marked difference to the rate of referral or the duration of untreated psychosis. However, training of GPs did have a significant impact on speed of access to early-intervention services.
Implications for future research and clinical practice
Primary care would appear to be just one part of the solution in terms of reducing the duration of untreated psychosis for young people with first-episode psychosis. This trial and the wider evidence base suggest that a whole-systems approach is required, consisting of a combination of primary care and secondary care education and training, with clear protocols determining fast access to early-intervention services, community awareness campaigns, and clear protocols for the recognition and management of psychosis in mental health services. Collectively, these may reduce the duration of untreated psychosis and improve outcomes for young people with first-episode psychosis.
Acknowledgments
We would like to acknowledge the hard work of field researchers, Chris John and Kate Harris, the cooperation of the primary care trust education and learning staff, the case workers and team leads in the Birmingham EIS, and GPs and staff in the participating practices.
Funding body
This study was funded by the Birmingham and Solihull Mental Health NHS Trust. REDIRECT is registered with the Current Controlled Trial: ISRCTN87898421 and the National Research Register: N0222140891
Ethical approval
Ethical approval was granted by the Sandwell & West Birmingham, South Birmingham and East Birmingham Research Ethics Committees
Competing interests
The authors have stated that there are none; all authors are independent from the funding body and the views expressed in this paper have not been influenced by the funding source
Discuss this article
Contribute and read comments about this article on the Discussion Forum: http://www.rcgp.org.uk/bjgp-discuss
REFERENCES
- 1.Drake RJ, Haley CJ, Akhtar S, Lewis SW. Causes and consequences of duration of untreated psychosis in schizophrenia. Br J Psychiatr. 2000;177:511–515. doi: 10.1192/bjp.177.6.511. [DOI] [PubMed] [Google Scholar]
- 2.Lincoln C, McGorry P. Who cares? Pathways to psychiatric care for young people experiencing a first episode of psychosis. Psychiatr Serv. 1995;46(11):1166–1171. doi: 10.1176/ps.46.11.1166. [DOI] [PubMed] [Google Scholar]
- 3.Larsen T, Friis S, Haahr U, et al. Early detection and intervention in first-episode schizophrenia: a critical review. Acta Psychiatr Scand. 2001;103(5):323–334. doi: 10.1034/j.1600-0447.2001.00131.x. [DOI] [PubMed] [Google Scholar]
- 4.Marshall M, Lewis S, Lockwood A. Association between duration of untreated psychosis and outcome in cohorts of first episode psychosis. Arch Gen Psychiatry. 2005;62(9):975–983. doi: 10.1001/archpsyc.62.9.975. [DOI] [PubMed] [Google Scholar]
- 5.Cole E, Leavey G, King M, et al. Pathways to care for patients with a first episode of psychosis: a comparison of ethnic groups. Br J Psychiatr. 1995;167(6):770–776. doi: 10.1192/bjp.167.6.770. [DOI] [PubMed] [Google Scholar]
- 6.Burnett R, Mallett R, Bhugra D, et al. The first contact of patients with schizophrenia with psychiatric services: social factors and pathways to care in a multi-ethnic population. Psychol Med. 1999;29(2):475–483. doi: 10.1017/s0033291798008125. [DOI] [PubMed] [Google Scholar]
- 7.Skeate A, Jackson C, Birchwood M, et al. Duration of untreated psychosis and pathways to care in first episode psychosis. Br J Psychiatry. 2002;181:73–77. doi: 10.1192/bjp.181.43.s73. [DOI] [PubMed] [Google Scholar]
- 8.Shiers D, Lester H. Early intervention for first episode psychosis needs greater involvement of primary care professionals for its success. BMJ. 2004;328:1451–1452. doi: 10.1136/bmj.328.7454.1451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Etheridge K, Yarrow L, Peet M. Pathways to care in first episode psychosis. J Psychiatr Ment Health Nurs. 2004;11(2):125–128. doi: 10.1111/j.1365-2850.2003.00673.x. [DOI] [PubMed] [Google Scholar]
- 10.Falloon IRH. General practice recruitment for people at risk of schizophrenia: the Buckingham experience. Aust NZ J Psychiatry. 2000;34:S131–S136. doi: 10.1080/000486700233. [DOI] [PubMed] [Google Scholar]
- 11.Fenning S, Kovasznay B, Rich C, et al. Six month stability of psychiatric diagnosis in first admission patients with psychosis. Am J Psychiatr. 1995;151(8):1200–1205. doi: 10.1176/ajp.151.8.1200. [DOI] [PubMed] [Google Scholar]
- 12.Lawrie SM, Martin K, McNeill G, et al. General practitioners' attitudes to psychiatric and medical illness. Psychol Med. 1998;28(6):1463–1467. doi: 10.1017/s0033291798007004. [DOI] [PubMed] [Google Scholar]
- 13.Bindman J, Johnson S, Wright S, Szmukler G, et al. Integration between primary and secondary services in the care of the severely mentally ill: patients' and general practitioners' views. Br J Psychiatry. 1997;171:169–174. doi: 10.1192/bjp.171.2.169. [DOI] [PubMed] [Google Scholar]
- 14.Lester HE, Tait L, Khera A, Birchwood M. The development and evaluation of an educational intervention on first episode psychosis for primary care. Med Educ. 2005;39(10):1006–1014. doi: 10.1111/j.1365-2929.2005.02273.x. [DOI] [PubMed] [Google Scholar]
- 15.Brunet K, Birchwood M, Lester H, Thornhill K. Delays in mental health services and duration of untreated psychosis. Psychiatr Bull. 2007;31:408–410. [Google Scholar]
- 16.Department of Health. The mental health policy implementation guide. London: Department of Health; 2001. [Google Scholar]
- 17.World Health Organization. The ICD-10 International Classification of Diseases and Related Health Problems. 10th rev edn. Geneva: World Health Organization; 2004. [Google Scholar]
- 18.Campbell M, Fitzpatrick R, Haines A, et al. Framework for design and evaluation of complex interventions to improve health. BMJ. 2000;321(7262):694–696. doi: 10.1136/bmj.321.7262.694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Medical Research Council. A framework for development and evaluation of RCTs for complex interventions to improve health. London: Medical Research Council; 2000. [Google Scholar]
- 20.Oxman AD, Thomson MA, Haynes RB, Davies DA. No magic bullets: a systematic review of 102 trials of interventions to improve professional practice. CMAJ. 1995;153(10):1423–1431. [PMC free article] [PubMed] [Google Scholar]
- 21.Tait L, Lester HE, Birchwood M, et al. Design of the BiRmingham Early Detection In untREated psyChosis Trial (REDIRECT): cluster randomised controlled trial of general practitioner education in detection of first episode psychosis. BMC Health Serv Res. 2005;5(1):19. doi: 10.1186/1472-6963-5-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.World Health Organization. SCAN: Schedules for Clinical Assessment in Neuropsychiatry. Geneva: World Health Organization; 1999. [Google Scholar]
- 23.Birchwood M, Smith J, Drury V, et al. A self report Insight Scale for psychosis: reliability, validity and sensitivity to change. Acta Psychiatr Scand. 1994;89(1):62–67. doi: 10.1111/j.1600-0447.1994.tb01487.x. [DOI] [PubMed] [Google Scholar]
- 24.Birchwood M, Smith J, Macmillan F, et al. Predicting relapse in schizophrenia: the development and implementation of an early signs monitoring system using patients and families as observers, a preliminary investigation. Psychol Med. 1989;19(3):649–656. doi: 10.1017/s0033291700024247. [DOI] [PubMed] [Google Scholar]
- 25.Kay S, Fiszbein A, Opler LA. The positive and negative syndrome scale (PANSS) for schizophrenia. Schizophr Bull. 1987;13(2):261–276. doi: 10.1093/schbul/13.2.261. [DOI] [PubMed] [Google Scholar]
- 26.Beiser M, Erickson D, Fleming JAE, Iacono WG. Establishing the onset of psychotic illness. Am J Psychiatry. 1993;150(9):1349–1354. doi: 10.1176/ajp.150.9.1349. [DOI] [PubMed] [Google Scholar]
- 27.Larsen TK, Johannessen JO, Opjordsmoen S. First-episode schizophrenia with long duration of untreated psychosis. Br J Psychiatr. 1998;172(Suppl 33):45–52. [PubMed] [Google Scholar]
- 28.Cannon-Spoor HE, Potkin SG, Wyatt RJ. Measurement of premorbid adjustment in chronic schizophrenia. Schizophr Bull. 1982;8(3):470–484. doi: 10.1093/schbul/8.3.470. [DOI] [PubMed] [Google Scholar]
- 29.Gater R, Sousa BD, Barrientos G, et al. The pathways to psychiatric care — a cross-cultural study. Psychol Med. 1991;21(3):761–774. doi: 10.1017/s003329170002239x. [DOI] [PubMed] [Google Scholar]
- 30.McCulloch CE, Searle SR. Generalized, linear, and mixed models. New York: John Wiley & Sons; 2001. [Google Scholar]
- 31.Altman DG, Schulz KF, Moher D, et al. The revised CONSORT statement for reporting randomized trials: explanation and elaboration. Ann Intern Med. 2001;134(8):663–694. doi: 10.7326/0003-4819-134-8-200104170-00012. [DOI] [PubMed] [Google Scholar]
- 32.Craig T, Garety P, Power P, et al. The Lambeth Early Onset (LEO) Team: randomised controlled trial of the effectiveness of specialised care for early psychosis. BMJ. 2004;329(7474):1067–1071. doi: 10.1136/bmj.38246.594873.7C. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Gilbody S, Whitty P, Grimshaw J, Thomas R. Educational and organizational interventions to improve the management of depression in primary care: a systematic review. JAMA. 2003;289(23):3145–3151. doi: 10.1001/jama.289.23.3145. [DOI] [PubMed] [Google Scholar]
- 34.Thompson C, Kinmonth AL, Stevens A, et al. Effects of a clinical-practice guideline and practice-based education on detection and outcome of depression in primary care: Hampshire Depression Project randomised controlled trial. Lancet. 2000;355(9199):185–191. doi: 10.1016/s0140-6736(99)03171-2. [DOI] [PubMed] [Google Scholar]
- 35.McGrath JJ. The surprisingly rich contours of schizophrenia epidemiology. Arch Gen Psychiatry. 2007;64(1):14–16. doi: 10.1001/archpsyc.64.1.14. [DOI] [PubMed] [Google Scholar]
- 36.Larsen TK, McGlashen T, Johannessen JO. Shortened duration of untreated first episode psychosis: changes in patients; characteristics at treatment. Am J Psychiatry. 2001;158(11):1917–1919. doi: 10.1176/appi.ajp.158.11.1917. [DOI] [PubMed] [Google Scholar]
- 37.Malla A, Norman R, Scholten D, et al. A community intervention for early identification of first episode psychosis: impact on duration of untreated psychosis (DUP) and patient characteristics. Soc Psychiatry Psychiatr Epidemiol. 2005;40(5):337–344. doi: 10.1007/s00127-005-0901-6. [DOI] [PubMed] [Google Scholar]
- 38.Krstev H, Carbonne S, Harrigan S, et al. Early intervention in first episode psychosis — the impact of community development campaign. Soc Psychiatry Psychiatr Epidemiol. 2004;39(9):711–719. doi: 10.1007/s00127-004-0798-5. [DOI] [PubMed] [Google Scholar]
- 39.Power P, Iacoponi E, Reynolds N, et al. The Lambeth Early Onset Crisis Assessment Team Study: general practitioner education and access to an early detection team in first-episode psychosis. Br J Psychiatr. 2007;191(s51):s133–s139. doi: 10.1192/bjp.191.51.s133. [DOI] [PubMed] [Google Scholar]


