Abstract
This study sought to determine the outcomes of posterior lumbar interbody fusion (PLIF), via a unilateral approach, in selected patients who presented with unilateral leg pain and segmental instability of the lumbar spine. Patients with a single level of a herniated disc disease in the lumbar spine, unilateral leg pain, chronic disabling lower back pain (LBP), and a failed conservative treatment, were considered for the procedure. A total of 41 patients underwent a single-level PLIF using two PEEK™ (Poly-Ether-Ether-Ketone) cages filled with iliac bone, via a unilateral approach. The patients comprised 21 women and 20 men with a mean age of 41 years (range: 22 to 63 years). Two cages were inserted using a unilateral medial facetectomy and a partial hemilaminectomy. At follow-up, the outcomes were assessed using the Prolo Scale. The success of the fusion was determined by dynamic lumbar radiography and/or computerized tomography scanning. All the patients safely underwent surgery without severe complications. During a mean follow-up period of 26 months, 1 patient underwent percutaneous pedicle screw fixation due to persistent LBP. A posterior displacement of the cage was found in one patient. At the last follow up, 90% of the patients demonstrated satisfactory results. An osseous fusion was present in 85% of the patients. A PLIF, via a unilateral approach, enables a solid union with satisfactory clinical results. This preserves part of the posterior elements of the lumbar spine in selected patients with single level instability and unilateral leg pain.
Keywords: Posterior lumbar interbody fusion (PLIF), unilateral approach, instability
INTRODUCTION
A lumbar fusion through an available surgical technique, can reduce pain and decrease disability in patients with chronic lower back pain (LBP). Posterior lumbar interbody fusion (PLIF) has the advantages of restoring the disc height, immobilizing the unstable degenerated intervertebral disc area, decompressing the nerve roots, and restoring load bearing to anterior structures.1 The use of two cages has recently become routinely as a standard PLIF technique.2,3 However, it is very difficult to insert two cages of an appropriate size without surgical destruction of the posterior element of the spine. Extensive laminectomy and bilateral facetectomy cause iatrogenic instability of the posterior elements, which may cause postoperative back pain syndrome.4 Therefore, most clinical reports recommend that PLIF should be combined with pedicle screw fixation for a good clinical and radiological outcome.5,6 However, the wide exposure required for a circumferential fusion can cause unnecessary trauma to the lumbar musculoligamentous complex, which is one of the causes of a poor postoperative outcome.4,7 Most patients with a chronic disc herniation of the lumbar spine suffer from long standing LBP with instability. This is sometimes combined with a unilateral radiating leg pain, relative to the location of the disc herniation. We performed a PLIF, using two PEEK™ (Poly-Ether-Ether-Ketone) O.I.C. cages, with a unilateral medial facetectomy and hemilaminectomy, to avoid extensive iatrogenic destabilization of the posterior elements of the lumbar spine. Forty-one patients with unilateral leg pain accompanied by instability were treated with this unilateral approach. In this report we present our surgical experience, results of an average follow-up of 26-months, and a review of the literature regarding PLIF.
MATERIALS AND METHODS
Patient population
Forty-one patients underwent a single-level PLIF with a unilateral approach in our hospital between March 1999 and March 2001. The subjects comprised 20 men and 21 women with a mean age of 41 years (range: 22 to 63 years) at the time of surgery. The mean postoperative follow-up was 26 months (range: 18 months to 3 years). All the patients had significant unilateral leg pain and mechanical LBP. The LBP in all the patients had been unresponsive to conservative treatment for more than 6 months. Plain radiographies, including dynamic view and magnetic resonance imaging (MRI), were performed in all the patients. A computed tomography (CT) scan and discogram were performed when needed. All the patients were found to have a unilateral disc herniation from the MRI with radiographic instability in the dynamic lateral X-ray, which was compatible with the clinical features. All except two had definite disc space narrowing compared to the adjacent normal disc space. Six patients had previously undergone a discectomy at the same level. Patients with LBP only, or a multilevel degenerative disc disease, were excluded.
Surgical technique
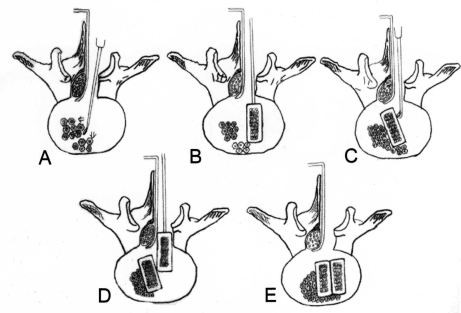
The patients were placed in the prone position under general anesthesia. A posterior midline incision was performed, the symptomatic side of the paravertebral muscle was split and retracted laterally, and the lamina and facet joints were exposed. The partial hemilaminectomy was performed first, followed by the unilateral medial facetectomy. Adequate decompression of the foraminal stenosis was accomplished simultaneously, and the facet joints were preserved as much as possible. The thecal sac and traversing nerve root were mobilized and retracted to the midline. The disc material and the endplates were removed as much as possible using a pituitary rongeurs, a rotate-cutter, an endplate scraping device, and down-biting curved curettes. The disc material and endplates in the contralateral side should be denuded as much as possible with the down-biting curettes and the specially designed curved rotate-cutter. The disc spreaders were inserted and manipulated in the disc space to provide disc space distraction. All patients underwent autogenous, cortical and cancellous, bone harvesting from the iliac crest. We used paired PEEK cages as a hollow ramp; a rectangular implant with round edges and variable sizes (13 mm, 11 mm, and 9 mm height), which enables easy insertion; and radiolucency, which enables the complete inspection of the radiological fusion. The chamber of the PEEK cages was filled with cancellous bone from the iliac crest. Before cage insertion, the lamina and cortical bone from the iliac crest were grafted into the contralateral and anterior sides of the intervertebral space as much as possible. The first cage was introduced to the intervertebral space. This was followed by careful pushing to the contralateral side with the down-biting curettes and impactor. The second cage was impacted to the ipsilateral side in the same manner (Fig. 1). Since the PEEK cage has a round edge in the posterior wall, the first cage was usually moved to the contralateral side without any trouble. After complete hemostasis, the wound was closed in layers in the usual fashion. On the first postoperative day, all patients were allowed to ambulate with a lumbar orthosis, which was usually worn for 1-2 months.
Fig. 1.
Diagrams depicting the steps of the PLIF via a unilateral approach. (A) After the retraction of the thecal sac and traversing nerve root to the midline, disc material and endplates are removed as much as possible in both the contralateral and ipsilateral sides. Before the cage insertion, the lamina and cortical bone from the iliac crest are grafted as much as possible into the contralateral and anterior sides of the intervertebral space. (B) The first cage filled with cancellous bone from the iliac crest is introduced to the intervertebral space. (C) The cage is carefully pushed to the contralateral side with the down-biting curettes and impactor. (D) The second cage was impacted to the ipsilateral side in the same manner. (E) Lastly, adequate impaction and complete hemostasis are performed.
Outcome assessment
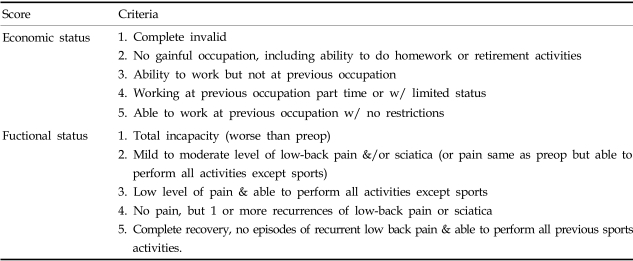
The follow-up evaluations consisted of a re-examination of the patients at the out-patient clinic, mailed questionnaires, and radiographic workup. The patients' clinical symptoms were assessed before surgery and re-assessed at 1, 6, 12, and 24 months postoperative. The clinical outcomes were evaluated using the Prolo economic and functional rating scale (Table 1), based on the results of the follow-up physical examinations and interview.8 Good and excellent outcomes were considered a clinical success, and fair or poor outcomes were considered unsatisfactory results. Finally, the patients were asked to rate their condition as: improved, unchanged, or worse. They were also questioned as to whether they would undergo the same procedure again under the same circumstances. The radiological evaluation of the fusion state was checked, primarily with the use of plain radiographs at follow-up. In some cases, a CT scan was performed to supplement the plain radiographic findings. All x-ray films were interpreted by a spine radiologist, who was not involved in the evaluation of the clinical outcome. Fusion was defined as radiographic evidence of bone bridging, the absence of lucency around the implant, and no motion during flexion and extension in dynamic lateral films. The disc height was measured before and immediately after surgery, as well as at the last follow up. The method for measuring disc height was based on the corners of adjacent vertebral contour and by averaging the ventral and dorsal disc heights.
Table 1.
Prolo Functional Economic Outcome Rating Scale
RESULTS
All patients underwent a one-level fusion. The vertebral levels at which the implants were inserted were as follows: L2-3 (one patient), L4-5 (25 patients), and L5-S1 (15 patients). With regard to the complications, there was one case of transient weakness of the foot. A re-operation was required in 1 patient due to implant migration. No implant fractures or deformities occurred.
At the time of the last follow-up visit, 37 patients (90%) were satisfied with the results of the surgery. No patients, with the exception of one, felt they were worse after the surgery. Twenty-five patients (61%) experienced excellent results, 12 (29%) had good results, three (7%) had fair results, and one (2%) had a poor clinical result. The radicular symptoms were resolved in all patients, with the exception of three, who still suffer from mild discomfort of the leg.
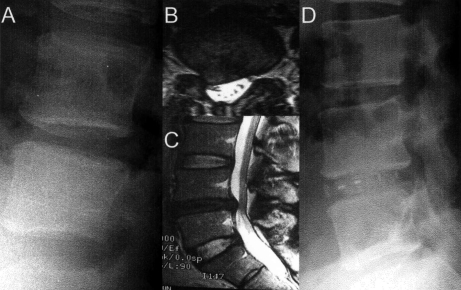
One patient, with worsened LBP 1 year after surgery, underwent a percutaneous pedicle screw fixation using the Sextant system. A good outcome was achieved 6 months after the second operation. A successful radiographic fusion was achieved at the time of the last follow-up in 35 patients (85%). Fig. 2 demonstrates a case of solid fusion after PLIF via a unilateral approach.
Fig. 2.
A 53-year-old woman presented with a 1-year history of LBP and radiating right leg pain. (A) Plain dynamogram revealing flexion instability at L4-5. (B-C) Spinal MRI showing a severe disc protrusion with degenerative disease at the same level. The patient underwent L4-5 PLIF using PEEK cage. (D) Plain radiograph obtained one and a half years after the surgery demonstrates a solid fusion. At the last follow-up visit, she has returned to daily activities without any symptoms.
The fusion status was not associated with the clinical outcome (p = 0.15). The majority of patients felt they had improved postoperatively and would opt for the same surgery again. The average disc height before surgery was 8.1 mm, which was restored to an average of 11.7 mm immediate after surgery. At the last follow-up, the average disc height had decrease to 10.1 mm. The disc height after the PLIF procedure was increased significantly. However, there was no corelation between the change of disc height and the Prolo scale.
DISCUSSION
Over the last few decades, surgical fusion of the lumbar spine has been increasingly performed on patients with chronic LBP. A variety of different surgical techniques can be used to achieve lumbar fusion.9 Posterolateral fusion has been one of the standards for surgical treatment of lumbar spinal instability, and with the use of spinal instrumentation, it has been widely used for lumbar degenerative pathology.1 However, posterolateral fusion may not restore the disc space height or sagittal segmental alignment, even when spinal instrumentation is used.
The origin of chronic LBP remains unclear and controversial. In degenerative disc disease with instability, the major source of the pain is thought to be a result of the degenerative disc itself and/or the facet joints. If the source of pain is believed to be a degenerative disc, it seems reasonable to remove this structure and replace it with a bone transplant, using either PLIF or anterior lumbar interbody fusion (ALIF).2,3 PLIF, pioneered by Cloward, has the advantage of allowing the restoration of the disc space height, sagittal plane alignment, and weight bearing through the anterior column.3-5 Since the introduction of various cages for PLIF, the surgical technique and its outcomes have been greatly improved. An interbody fusion with a cage alone has been increasingly accepted for the treatment of a lumbar degenerative change.6,7
However, PLIF with a stand-alone cage has been criticized by many spine surgeons due to the need for removing a significant amount of the posterior supporting spinal structures. This can be achieved by a bilateral facetectomy or a wide laminectomy, for the bilateral placement of the cage into the disc space. Therefore, most surgeons recommend that PLIF should be supplemented by posterior instrumentation.5,8,9 However, a greater exposure and disruption of the posterior elements would be needed to perform a circumferential fusion of the unstable segment.
There are several reports that an iatrogenic soft-tissue injury correlates with negative long-term clinical outcomes.10 Excessive intra-operative dissection and retraction of the paraspinal musculature can lead to denervation and atrophy. The damaged muscle tissue acts as a pain generator, which results in an increased risk of"failed back syndrome".11 Extensive bilateral facetectomy is also associated with postoperative pain and prolonged disability. Therefore, in patients with chronic LBP with a unilateral disc herniation, wide exposure and circumferential fusion may produce iatrogenic flat back syndrome or contralateral leg discomfort, despite the improvement in ipsilateral leg pain. Transforaminal lumbar interbody fusion is another surgical method to achieve successful fusion with no risk of nerve root injury.12,13 With this approach, the intervertebral disc can be accessed, unilaterally, through the neural foramen for the introduction of the bone graft material or a fusion cage. Many surgeons favor this approach over PLIF for the treatment of spondylolisthesis.
However, this approach also has the disadvantage of a wide exposure of the lumbar spine in patients with a single level instability without spondylolisthesis. In 1985, Blume14 reported that unilateral PLIF with a bone dowel and cancellous bone chip had the advantage of preserving the posterior ligament structure. Conversely, a bone graft without cages may cause disc space collapse in the long-term. Zhao et al. recently reported on the use of a single threaded interbody fusion cage, placed obliquely, for degenerative spondylolisthesis.15 They found that a unilateral facetectomy enabled sufficient decompression for the safe placement of the cage device, while maintaining the important posterior supporting spinal structures. They reported that PLIF using a single long threaded cage inserted obliquely through a unilateral facetectomy and hemilaminectomy, was significantly stiffer than that achieved with two posterior cages inserted through a bilateral facetectomy and laminectomy.16 Abumi et al.17 found that a bilateral facetectomy produced a marked increases in the motions of flexion and axial rotation, whereas a unilateral facetectomy produced less increases in motion, especially in rotation. Therefore, by avoiding bilateral facet disruption, surgeons can achieve solid fusion with PLIF.
With our surgical approach, we can save most portions of the posterior elements, including the spinous process and all the structures on the contralateral side. A total facetectomy on the ipsilateral side is not required. In contrast to the single cage technique, we used two cages with a unilateral approach. It was possible to insert two appropriately sized cages using this unilateral approach with the decompression of unilateral stenosis, with no major complications. A unilateral partial hemi-laminectomy and medial facetectomy, which is the most common procedure for a simple disc herniation, is enough for a PLIF with two cages to be achieved. Since the remaining posterior elements can maintain their physiological range of motion in flexion and rotation, we think that supplemental posterior instrumentation is not necessary as long as the facet joints are preserved.
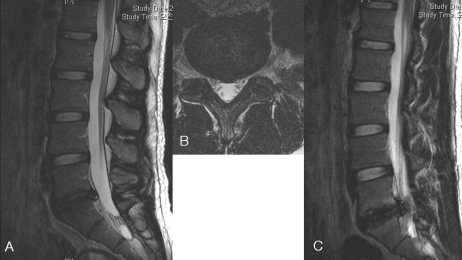
To increase the solid fusion rate, it is essential to increase the area of the bone fusion and the total amount of graft bone. Another advantage of our approach is that an additional bone graft could be implanted before the insertion of the cage into the contralateral intervertebral space, with no risk of bone graft retropulsion or collapse. Compared to the cylindrical cage, a rectangular PEEK cage is smaller, which eliminates the need for extensive retraction of the neural tissue or the total removal of the facet joints, for its insertion. We had one case of cage retropulsion that required re-operation. There is a risk of posterior migration when rounded, stand-alone cages are used. This can be prevented by the surgeon using an appropriate cage.
PLIF in revision surgery is a technically demanding procedure. Chitnavis et al., reported excellent results following a PLIF using a carbon cage in patients with recurrent disc herniations.18 They proposed that the cage offered structural support while biological fusion occurred. However, most patients with recurrent disc herniations usually have unilateral leg pain. A bilateral approach may cause pain or sensory disturbance to the contralateral leg. We performed our surgical method in 6 patients with recurrent disc herniations accompanied by segmental instability. Of these patients, 4 had excellent clinical outcomes, and the other 2 had good outcomes. No patient felt their condition was worse after the surgery. At the time of the last follow-up visit, 4 patients were not satisfied with the results of the surgery. Of these, two patients had a normal disc space but with flexion instability. A facet fracture occurred during the insertion of larger cages into the intervertebral space, and the cages and grafted bone were unable to fully fill the intervertebral space. We had difficulty moving the first cages to the contralateral side and inserting the two large cages through the unilateral route. One of them underwent percutaneous pedicle screw fixation with the Sextant system.10 This produced a good outcome 6 months after the second operation. Two other patients had a mild to moderate degree of LBP despite a radiological solid fusion at the time of the last follow-up.
In our series, the radiological fusion rate was slightly lower than that with other PLIF techniques. A sound fusion is thought to be a parameter for clinical success in patients with mechanical LBP. However, the fusion rates did not correlate with the clinical outcomes in our patients. In previous studies, the clinical outcome did not always parallel the radiographically solid fusion.19 Agazzi et al. have reported that a PLIF with a cage may restore and maintain the disc height and the sagittal balance. This may improve the clinical results despite the lack of solid fusion.7 The primary indication from our operative method was a chronic degenerative disc disease with unilateral leg pain combined with radiological instability, but without spondylolisthesis. This technique can manage both problems successfully, without the need for a circumferential operation. The limitations of this unilateral approach for bilateral PLIF include, instability with a normal disc height, spondylolisthesis, and bilateral foraminal stenosis, requiring bilateral decompression. Further study and long-term follow-up will be necessary. A posterior lumbar interbody fusion with two cages, via a unilateral approach, enables sufficient decompression and solid interbody fusion to be achieved, while the majority of the posterior elements are maintained. It is an ideal procedure in a patient with severe symptomatic axial LBP with radiculopathy from disc herniation or stenosis.
Fig. 3.
This case showed retropulsion of the inserted cage at 6 months postoperative. (A, B) Preoperative MRI showed degenerative disc herniation at L5/S1 segments. (C) At 6 months after PLIF, the cage migrated posteriorly and compressed the dural sac.
Footnotes
This work was supported by a grant (03-PJ1-PG1-CH07-0004) of the 2003 Good Health R&D Project, Ministry of Health and Welfare, Korea.
References
- 1.Axelsson P, Johnsson R, Stromqvist B, Arvidsson M, Herrlin K. Posterolateral lumbar fusion. Outcome of 71 consecutive operations after 4 (2-7) years. Acta Orthop Scand. 1994;65:309–314. doi: 10.3109/17453679408995459. [DOI] [PubMed] [Google Scholar]
- 2.Fritzell P, Hagg O, Wessberg P, Nordwall A. Chronic low back pain and fusion: a comparison of three surgical techniques: a prospective multicenter randomized study from the Swedish lumbar spine study group. Spine. 2002;27:1131–1141. doi: 10.1097/00007632-200206010-00002. [DOI] [PubMed] [Google Scholar]
- 3.Brislin B, Vaccaro AR. Advances in posterior lumbar interbody fusion. Orthop Clin North Am. 2002;33:367–374. doi: 10.1016/s0030-5898(01)00013-x. [DOI] [PubMed] [Google Scholar]
- 4.Lin PM, Cautilli RA, Joyce MF. Posterior lumbar interbody fusion. Clin Orthop Relat Res. 1983;180:154–168. [PubMed] [Google Scholar]
- 5.Lin PM. Posterior lumbar interbody fusion (PLIF): past, present, and future. Clin Neurosurg. 2000;47:470–482. [PubMed] [Google Scholar]
- 6.Hacker RJ. Comparison of interbody fusion approaches for disabling low back pain. Spine. 1997;22:660–665. doi: 10.1097/00007632-199703150-00017. discussion 665-6. [DOI] [PubMed] [Google Scholar]
- 7.Agazzi S, Reverdin A, May D. Posterior lumbar interbody fusion with cages: an independent review of 71 cases. J Neurosurg. 1999;91(2) Suppl:186–192. doi: 10.3171/spi.1999.91.2.0186. [DOI] [PubMed] [Google Scholar]
- 8.Suk SI, Lee CK, Kim WJ, Lee JH, Cho KJ, Kim HG. Adding posterior lumbar interbody fusion to pedicle screw fixation and posterolateral fusion after decompression in spondylolytic spondylolisthesis. Spine. 1997;22:210–219. doi: 10.1097/00007632-199701150-00016. discussion 219-20. [DOI] [PubMed] [Google Scholar]
- 9.Brantigan JW, Steffee AD, Geiger JM. A carbon fiber implant to aid interbody lumbar fusion. Mechanical testing. Spine. 1991;16(6) Suppl:S277–S282. doi: 10.1097/00007632-199106001-00020. [DOI] [PubMed] [Google Scholar]
- 10.Foley KT, Gupta SK. Percutaneous pedicle screw fixation of the lumbar spine: preliminary clinical results. J Neurosurg. 2002;97(1) Suppl:7–12. doi: 10.3171/spi.2002.97.1.0007. [DOI] [PubMed] [Google Scholar]
- 11.Sihvonen T, Herno A, Paljarvi L, Airaksinen O, Partanen J, Tapaninaho A. Local denervation atrophy of paraspinal muscles in postoperative failed back syndrome. Spine. 1993;18:575–581. doi: 10.1097/00007632-199304000-00009. [DOI] [PubMed] [Google Scholar]
- 12.Lowe TG, Tahernia AD. Unilateral transforaminal posterior lumbar interbody fusion. Clin Orthop Relat Res. 2002;394:64–72. doi: 10.1097/00003086-200201000-00008. [DOI] [PubMed] [Google Scholar]
- 13.Moskowitz A. Transforaminal lumbar interbody fusion. Orthop Clin North Am. 2002;33:359–366. doi: 10.1016/s0030-5898(01)00008-6. [DOI] [PubMed] [Google Scholar]
- 14.Blume HG. Unilateral posterior lumbar interbody fusion: simplified dowel technique. Clin Orthop Relat Res. 1985;193:75–84. [PubMed] [Google Scholar]
- 15.Zhao J, Hai Y, Ordway NR, Park CK, Yuan HA. Posterior lumbar interbody fusion using posterolateral placement of a single cylindrical threaded cage. Spine. 2000;25:425–430. doi: 10.1097/00007632-200002150-00006. [DOI] [PubMed] [Google Scholar]
- 16.Zhao J, Wang X, Hou T, He S. One versus two BAK fusion cages in posterior lumbar interbody fusion to L4-L5 degenerative spondylolisthesis: a randomized, controlled prospective study in 25 patients with minimum two-year follow-up. Spine. 2002;27:2753–2757. doi: 10.1097/00007632-200212150-00003. [DOI] [PubMed] [Google Scholar]
- 17.Abumi K, Panjabi MM, Kramer KM, Duranceau J, Oxland T, Crisco JJ. Biomechanical evaluation of lumbar spinal stability after graded facetectomies. Spine. 1990;15:1142–1147. doi: 10.1097/00007632-199011010-00011. [DOI] [PubMed] [Google Scholar]
- 18.Chitnavis B, Barbagallo G, Selway R, Dardis R, Hussain A, Gullan R. Posterior lumbar interbody fusion for revision disc surgery: review of 50 cases in which carbon fiber cages were implanted. J Neurosurg. 2001;95(2) Suppl:190–195. doi: 10.3171/spi.2001.95.2.0190. [DOI] [PubMed] [Google Scholar]
- 19.Turner JA, Ersek M, Herron L, Haselkorn J, Kent D, Ciol MA, et al. Patient outcomes after lumbar spinal fusions. JAMA. 1992;268:907–911. [PubMed] [Google Scholar]