Abstract
This study was performed to evaluate the efficiency of simplified EM grid vitrification, skipping the step of removing the cryoprotectant (5.5 M EG + 1.0 M sucrose) droplet on the grid after loading oocytes, compared to conventional cryopreservation protocols for mouse mature oocytes. Firstly, the recovery, survival, fertilization and hatching rates of simplified EM grid vitrification were compared with those of the slow freezing method using 1.5 M DMSO. Then, conventional EM grid vitrification was compared with simplified EM grid vitrification. Simplified EM grid vitrification showed higher survival, fertilization and hatching rates than those of the slow freezing method (85.6% vs. 63.2%; 51.0% vs. 22.3%; 38.7% vs. 12.5%, p < 0.01, respectively). Moreover, simplified EM grid vitrification showed higher recovery, survival and fertilization rates than those of conventional EM grid vitrification (100% vs. 95.0%, p = 0.024; 90.0% vs. 78.9%, p = 0.033; 56.7% vs. 38.7%, p = 0.021, respectively). Hatching rate tended to be higher for simplified EM grid vitrification compared to conventional EM grid vitrification (41.1% vs. 24.1%). In conclusion, simplified EM grid vitrification is a convenient and efficient method for cryopreservation of mouse mature oocytes, compared to conventional EM grid vitrification and slow freezing methods.
Keywords: EM grid vitrification, cryopreservation, mouse oocyte
INTRODUCTION
Cryopreservation of oocytes is becoming an essential part of assisted reproductive technology (ART), including in vitro fertilization and embryo transfer (IVF-ET). Human oocyte cryopreservation has a relatively short history and was first introduced in 1986.1 At present, various protocols are used for freezing human oocytes. However, clinical efficiency remains low, which indicates that current freezing protocols still need to be improved.
Mouse oocyte cryopreservation is important since it provides preliminary data that may be applied to human oocyte cryopreservation. As in the case of human gametes, mammalian oocytes and spermatozoa can be effectively stored by cryopreservation in liquid nitrogen.1-3 Although relatively acceptable results have been obtained for mice,4-7 the storage of unfertilized oocytes is still unsatisfactory.
Frequently used protocols include slow freezing-ultrarapid thawing, ultrarapid freezing-ultrarapid thawing, and vitrification.8 In conventional EM grid vitrification, the cryoprotectant solution is removed from the EM grid along with the underlying sterilized filter paper after oocytes have been mounted.9 In this study, we simplified the EM grid vitrification method by skipping the process of removing the cryoprotectant, and compared the outcomes with those of conventional protocols. If simplified EM grid vitrification shows equivalent or better outcomes, then we can save time and enhance the convenience and efficiency of oocyte cryopreservation. We performed this investigation to compare the efficiency of simplified EM grid vitrification with slow freezing, ultrarapid freezing and conventional EM grid vitrification in terms of the recovery, survival, fertilization and hatching rates of mouse mature oocytes.
MATERIALS AND METHODS
Collection and preparation of oocytes
F1 hybrid mice (C57BL female × DBA male) were maintained under 14-hour light/10-hour dark cycles and were fed ad libitum. After 1 week of adaptation, 5 to 6-week old mice were used for the experiments. Mice were sacrificed by cervical dislocation and bilateral oviducts were resected. Mature oocytes were retrieved after intraperitoneal injection using 30-gauge tuberculin syringe needles to inject 5 IU pregnant mare serum gonadotropin (PMSG, Sigma, St. Louis, MO, USA) followed by 5 IU human chorionic gonadotropin (hCG, Sigma, USA) 48 hours later, in M16 media supplemented with 0.4% bovine serum albumin (BSA) under a dissecting microscope. Cumulus cells were removed by treatment with 0.1% hyaluronidase for 1 min.
Slow and ultrarapid freezing
Two milliliters of synthetic serum substitute (SSS) were diluted with 8 ml of D-PBS, and each of the cryoprotectants listed in Table 1. Ten to fifteen oocytes were placed in each culture dish containing cryoprotectant, and transferred into straws using negative pressure. For slow freezing, the straws were placed into automatic cell freezer (KRYO-10, Planer) within 10 min after immersing the oocytes into cryoprotectants. Temperature was lowered from 10℃ to -7℃ at -2℃/min. Seeding was done at -7℃ while waiting for 1 min to prevent hypercooling. Again, the temperature was lowered from -7℃ to -30℃ at -0.3℃/min. Straws were transferred into containers and plunged into liquid nitrogen. For ultrarapid freezing, oocytes were directly plunged into liquid nitrogen immediately after exposure to cryoprotectant solutions.
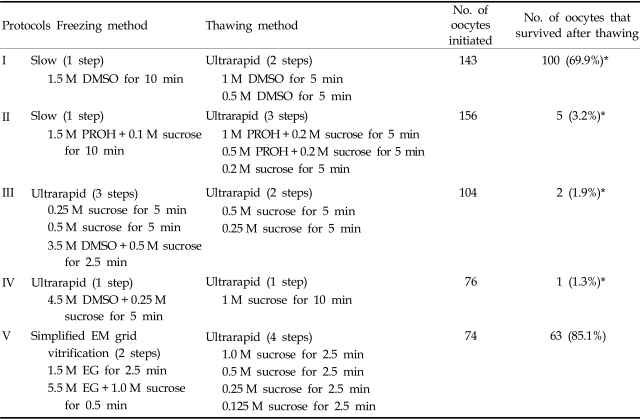
Table 1.
Preliminary Experiments: Post-thaw Survival Rates of Mouse Mature Oocytes for Various Cryopreservation Protocols
DMSO, dimethylsulfoxide; PROH, 1,2-propanediol; EG, ethylene glycol.
*p < 0.05 when compared with protocol V (simplified EM grid vitrification method).
For ultrarapid thawing, cryopreserved straws were exposed to room air for 20 sec, and oocytes in cryoprotectant were placed in culture dishes. The number of oocytes was counted under a dissecting microscope and transferred into thawing solution (D-PBS containing 20% SSS). Thawing was performed at graduated concentrations and for various durations as described in Table 1.
Vitrification: conventional and simplified
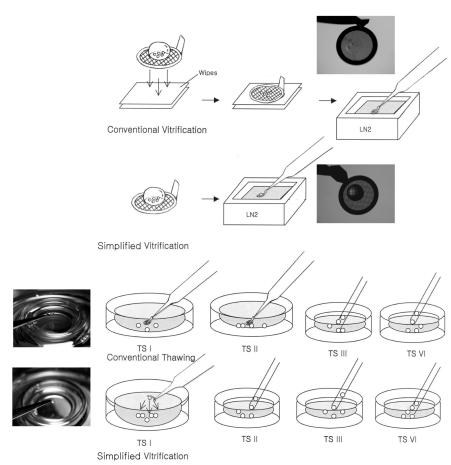
Oocytes were equilibrated in 1.5 M ethylene glycol (EG) (Sigma, USA) for 2 min 30 sec, and then in 5.5 M EG and 1.0 M sucrose. Within 30 sec, 5 oocytes were placed on each EM grid (Ted Pella, G600TT) and plunged into liquid nitrogen. For thawing, EM grids were taken out and exposed to 1.0 M, 0.5 M, 0.25 M and 0.125 M sucrose solutions for 2 min 30 sec each. Oocytes were rinsed with M16 containing 0.4% BSA. For the simplified EM grid vitrification method, the cryoprotectant solution droplet on the grid was not removed using the underlying sterilized filter paper as it was for the conventional EM grid vitrification (Fig. 1).9
Fig. 1.
Conventional and simplified vitrification methods. Top panel: In the simplified vitrification method, the cryoprotectant solution on the grid is not removed with the underlying sterilized filter paper (Wipes) as in conventional EM grid vitrification. Bottom panel: Most cryopreserved-thawed oocytes were retrieved at step I (TS I) following the simplified EM grid vitrification method, enabling the oocytes to avoid exposure to room air. In contrast, following conventional EM grid vitrification, it was necessary to move the grid to step II (TS II). Note the exemplary numbers of oocytes retrieved from both methods after 5 oocytes were loaded on each grid. TS: thawing solution, TS I: 1.0 M sucrose for 2.5 min, TS II: 0.5 M sucrose for 2.5 min, TS III: 0.25 M sucrose for 2.5 min, TS IV: 0.125 M sucrose for 2.5 min.
Post-thaw fertilization and culture
Sperm were collected from 8-week-old male mice after cervical dislocation. The tail of the epididymis was dissected with a 26-gauge needle and incubated in M16 media at 37℃ for 10 min. Supernatant was collected and capacitation was induced in M16 containing 0.4% BSA by incubating for 10 min.
The insemination concentration was 2 × 106/ml. Two-cell embryos after 24 hours were regarded as fertilized embryos. They were transferred to 2 ml of M16 media containing 0.4% BSA, and incubated at 37℃, 5% CO2 in air. Embryonic development was observed every 24 hours.
An oocyte was considered to have survived if it had clear and intact cytoplasm and zona pellucida. Oocyte survival rate was compared among the five cryopreservation methods (Table 1). Then, the slow or ultrarapid freezing protocol with the highest survival rate was compared with simplified EM grid vitrification in terms of recovery, survival, fertilization and hatching rates. Finally, conventional and simplified EM grid vitrification methods were compared in terms of recovery, survival, fertilization and hatching rates.
Statistical analysis
Data analysis was performed using SPSS 7.10 for Windows. Chi square and Fisher's exact tests were applied as appropriate. A p value of less than 0.05 was considered statistically significant.
RESULTS
The simplified EM grid vitrification group showed the highest survival rate of the five cryopreservation protocols, followed by slow-freezing and ultrarapid thawing using 1.5 M DMSO (Table 1).
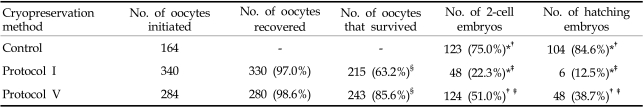
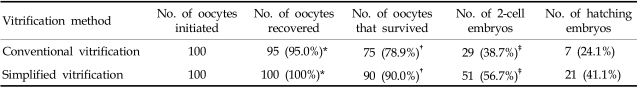
The simplified EM grid vitrification method resulted in higher survival, fertilization and hatching rates than the slow freezing-ultrarapid thawing method (85.6% vs. 63.2%; 51.0% vs. 22.3%; 38.7% vs. 12.5%, p < 0.01, respectively) (Table 2). Compared to conventional EM grid vitrification, the simplified method led to higher recovery, survival and fertilization rates (100% vs. 95.0%, p = 0.024; 90.0% vs. 78.9%, p = 0.033; 56.7% vs. 38.7%, p = 0.021, respectively). Hatching rate also tended to be higher following simplified EM grid vitrification compared to conventional EM grid vitrification (41.1% vs. 24.1%) (Table 3).
Table 2.
Comparison of Slow Freezing-Ultrarapid Thawing and Simplified EM Grid Vitrification Methods for Mouse Mature Oocyte Cryopreservation
Control: fresh oocytes.
Protocol I: slow freezing-ultrarapid thawing method using 1.5 M DMSO.
Protocol V: simplified vitrification method using 1.5 M EG and 5.5 M EG + 1.0 M sucrose.
*p < 0.001 when compared with protocol V.
†p < 0.001 when compared with protocol I.
‡p < 0.001 when compared with control.
§p < 0.001 when compared with each other.
Table 3.
Comparison of Conventional and Simplified EM Grid Vitrification Methods for Mouse Mature Oocyte Cryopreservation
*p = 0.024.
†p = 0.033.
‡p = 0.021.
DISCUSSION
Cryopreservation of oocytes is advantageous in that it allows for long-term storage of supernumerary oocytes produced by IVF and it can also be used for sperm function testing, for oocyte donation programs and for women receiving radio- or chemotherapy. There have been a few reports on the success of vitrification of human oocytes, however, the best oocyte cryopreservation protocol has yet to be determined.8,10
Mouse oocyte cryopreservation is important since it provides preliminary data that may indirectly be applicable to human oocyte cryopreservation. Cryopreserved-thawed mouse oocytes can be used for other experiments since mice are frequently used at many IVF centers for quality control. Finally, studies on mouse oocyte cryopreservation can provide basic cryobiological data.
Conventional EM grid vitrification is known to be superior to slow freezing for mouse mature oocyte cryopreservation.9 We wondered what the outcomes would be like if we skipped the step of removing the cryoprotectant from the EM grid after loading the oocytes. We wondered whether simplified EM grid vitrification would be as superior to slow or ultrarapid freezing as conventional EM grid vitrification and whether the simplified EM grid vitrification would be as efficient as conventional EM grid vitrification.
This study revealed that simplified EM grid vitrification showed better outcomes compared with either slow freezing or conventional EM grid vitrification. The simplified EM grid vitrification method resulted in higher survival, fertilization and hatching rates than the slow freezing method (Table 2). This means that simplifying the EM vitrification procedure did not negate the advantages of conventional EM grid vitrification. Compared to the conventional method, the simplified method led to higher recovery, survival and fertilization rates. The hatching rate tended to be higher for simplified EM grid vitrification compared to conventional EM grid vitrification, however, this difference was only significant when larger groups were compared (Table 3).
Compared to conventional EM grid vitrification, the simplified protocol was more convenient, as it was not necessary to remove the cryoprotectant using filter paper or wipes. As for post-thaw recovery, simplified EM grid vitrification samples had a higher recovery rate than the conventional method (Table 3), and most oocytes were recovered at the first step. For conventional EM grid vitrification samples, around 55%, 40% and 5% of oocytes were recovered at the first, second and third steps, respectively (Fig. 1). Oocytes on the EM grid were exposed to room air in between the second or third steps of the thawing procedure. The difference in the recovery rate was thought to be due to the presence of oocytes in the cryoprotectant droplet and the low probability of oocytes' sticking to the EM grid. At the first thawing step, we observed intact thawed droplets containing oocytes gliding from the grid of the simplified vitrification samples.
The first success with oocyte freezing was achieved in the mouse in 1977.11 Live offspring were obtained after IVF of mouse oocytes previously frozen with DMSO and stored under liquid nitrogen at -196℃. Despite this success, several problems with oocyte freezing were discovered. Freeze-thaw induced hardening of the zona pellucida and fertilization rates decreased in frozen-thawed mouse oocytes.12,13 Mouse embryos fertilized from frozen-thawed oocytes showed an increased incidence of polyploidy,14 while increased aneuploidy after vitrification was reported in mouse oocytes.15 Cytoplasmic disturbance in the post-thaw immature oocyte results in defective blastocyst development, which seems to be due to the loss of association between oocyte and cumulus cells induced by cryopreservation.16 Our investigation will extend into microscopic defects that may be caused by various cryoprotectants and protocols.
Research in oocyte cryobiology has been focused on optimizing mouse oocyte freezing protocols. Researchers have studied the temperature dependence of mature mouse oocyte membrane permeabilities in the presence of cryoprotectant.17 Other researchers have studied various freezing media with cryoprotective agents. For ultrarapid freezing and vitrification protocols, several cryoprotectants have been evaluated but the outcomes remain highly variable.18,19 Recently introduced, vitrification is now considered to be a promising technical innovation.20,21 We also found that vitrification had a superior efficiency for mouse mature oocyte cryopreservation.
In this study, we sought to evaluate and compare between simplified EM grid vitrification and slow freezing or conventional EM grid vitrification for mouse mature oocytes. Compared to slow freezing using 1.5 M DMSO, simplified EM grid vitrification using 5.5 M EG + 1.0 M sucrose was superior in terms of survival, fertilization and hatching rates. Moreover, simplified EM grid vitrification resulted in higher recovery, survival and fertilization rates. Hatching rate tended to be higher for simplified EM grid vitrification than the conventional method. In conclusion, this simplified EM grid vitrification is a convenient and efficient method for cryopreservation of mouse mature oocytes. Further studies are necessary to search for better cryoprotectants and to optimize their concentrations in terms of post-thaw survival rate and in vitro development. Microscopic defects that may be caused by various cryoprotectants also need further research.
Footnotes
This study was supported by grant No. 03-1999-090 from the SNUH Research Fund.
References
- 1.Chen C. Pregnancy after human oocyte cryopreservation. Lancet. 1986;1:884–886. doi: 10.1016/s0140-6736(86)90989-x. [DOI] [PubMed] [Google Scholar]
- 2.Van Uem JF, Siebzehnrubl ER, Schuh B, Koch R, Trotnow S, Lang N. Birth after cryopreservation of unfertilized oocytes. Lancet. 1987;1:752–753. doi: 10.1016/s0140-6736(87)90398-9. [DOI] [PubMed] [Google Scholar]
- 3.Porcu E, Fabbri R, Seracchioli R, Ciotti PM, Magrini O, Flamigni C. Birth of a healthy female after intracytoplasmic sperm injection of cryopreserved human oocytes. Fertil Steril. 1997;68:724–726. doi: 10.1016/s0015-0282(97)00268-9. [DOI] [PubMed] [Google Scholar]
- 4.Gook DA, Osbom SM, Bourne H, Johnston WI. Fertilization of human oocytes following cryopreservation: normal karyotypes and absence of stary chromosomes. Hum Reprod. 1994;9:684–691. doi: 10.1093/oxfordjournals.humrep.a138572. [DOI] [PubMed] [Google Scholar]
- 5.Tucker M, Wright G, Morton P, Shanguo L, Massey J, Kort H. Preliminary experience with human oocyte cryopreservation using 1,2-propanediol and sucrose. Hum Reprod. 1996;11:1513–1515. doi: 10.1093/oxfordjournals.humrep.a019428. [DOI] [PubMed] [Google Scholar]
- 6.Matson PL, Graefling J, Junk SM, Yovich JL, Edirisinghe WR. Cryopreservation of oocytes and embryos: use of a mouse model to investigate effects upon zona hardness and formulate treatment strategies in an in-vitro fertilization programme. Hum Reprod. 1997;12:1550–1553. doi: 10.1093/humrep/12.7.1550. [DOI] [PubMed] [Google Scholar]
- 7.Mandelbaum J, Belaisch-Allart J, Junca AM, Antoine JM, Plachot M, Alvarez S, et al. Cryopreservation in human assisted reproduction is now routine for embryos but remains a research procedure for oocytes. Hum Reprod. 1998;13(Suppl 3):161–177. doi: 10.1093/humrep/13.suppl_3.161. [DOI] [PubMed] [Google Scholar]
- 8.Fabbri R, Porcu E, Marsella T, Primavera MR, Rocchetta G, Ciotti PM, et al. Technical aspects of oocyte cryopreservation. Mol Cell Endocrinol. 2000;169:39–42. doi: 10.1016/s0303-7207(00)00349-x. [DOI] [PubMed] [Google Scholar]
- 9.Park SE, Chung HM, Cha KY, Hwang WS, Lee ES, Lim JM. Cryopreservation of ICR mouse oocytes: improved post-thawed preimplantation development after vitrification using Taxol, a cytoskeleton stabilizer. Fertil Steril. 2001;75:1177–1184. doi: 10.1016/s0015-0282(01)01809-x. [DOI] [PubMed] [Google Scholar]
- 10.Van der Elst J. Oocyte freezing: here to stay? Hum Reprod Update. 2003;9:463–470. doi: 10.1093/humupd/dmg032. [DOI] [PubMed] [Google Scholar]
- 11.Whittingham DG. Fertilization in vitro and development to term of unfertilized mouse oocytes previously stored at -196 degrees C. J Reprod Fertil. 1977;49:89–94. doi: 10.1530/jrf.0.0490089. [DOI] [PubMed] [Google Scholar]
- 12.Vincent C, Pickering SJ, Johnson MH. The hardening effect of dimethylsulphoxide on the mouse zona pellucida requires the presence of an oocyte and is associated with a reduction in the number of cortical granules present. J Reprod Fertil. 1990;89:253–259. doi: 10.1530/jrf.0.0890253. [DOI] [PubMed] [Google Scholar]
- 13.Wood MJ, Whittingham DG, Lee SH. Fertilization failure of frozen mouse oocytes is not due to premature cortical granule release. Biol Reprod. 1992;46:1187–1195. doi: 10.1095/biolreprod46.6.1187. [DOI] [PubMed] [Google Scholar]
- 14.Bouquet M, Selva J, Auroux M. Effects of cooling and equilibration in DMSO, and cryopreservation of mouse oocytes, on the rates of in vitro fertilization, development, and chromosomal abnormalities. Mol Reprod Dev. 1995;40:110–115. doi: 10.1002/mrd.1080400114. [DOI] [PubMed] [Google Scholar]
- 15.Kola I, Kirby C, Shaw J, Davey A, Trounson A. Vitrification of mouse oocytes results in aneuploid zygotes and malformed fetuses. Teratology. 1988;38:467–474. doi: 10.1002/tera.1420380510. [DOI] [PubMed] [Google Scholar]
- 16.Ruppert-Lingham CJ, Paynter SJ, Godfrey J, Fuller BJ, Shaw RW. Developmental potential of murine germinal vesicle stage cumulus-oocyte complexes following exposure to dimethylsulphoxide or cryopreservation: loss of membrane integrity of cumulus cells after thawing. Hum Reprod. 2003;18:392–398. doi: 10.1093/humrep/deg071. [DOI] [PubMed] [Google Scholar]
- 17.Paynter SJ, Fuller BJ, Shaw RW. Temperature dependence of mature mouse oocyte membrane permeabilities in the presence of cryoprotectant. Cryobiology. 1997;34:122–130. doi: 10.1006/cryo.1996.1990. [DOI] [PubMed] [Google Scholar]
- 18.Rayos AA, Takahashi Y, Hishinuma M, Kanagawa H. Quick freezing of unfertilized mouse oocytes using ethylene glycol with sucrose or trehalose. J Reprod Fertil. 1994;100:123–129. doi: 10.1530/jrf.0.1000123. [DOI] [PubMed] [Google Scholar]
- 19.O'Neil L, Paynter SJ, Fuller BJ, Shaw RW, DeVries AL. Vitrification of mature mouse oocytes in a 6 M Me2SO solution supplemented with antifreeze glycoproteins: the effect of temperature. Cryobiology. 1998;37:59–66. doi: 10.1006/cryo.1998.2098. [DOI] [PubMed] [Google Scholar]
- 20.Lane M, Gardner DK. Vitrification of mouse oocytes using a nylon loop. Mol Reprod Dev. 2001;58:342–347. doi: 10.1002/1098-2795(200103)58:3<342::AID-MRD13>3.0.CO;2-X. [DOI] [PubMed] [Google Scholar]
- 21.Mavrides A, Morroll D. Cryopreservation of bovine oocytes: is cryoloop vitrification the future to preserving the female gamete? Reprod Nutr Dev. 2002;42:73–80. doi: 10.1051/rnd:20020008. [DOI] [PubMed] [Google Scholar]