Abstract
This review summarizes the recent advances of osteoimmunology, a new research field that investigates the interaction of the immune system with the skeleton. Osteoimmunology has contributed significantly to the understanding of joint destruction in rheumatoid arthritis and other forms of arthropathies. In particular, the molecular regulation of osteoclast formation and its control by proinflammatory cytokines have helped investigators to understand the mechanisms of bone erosion in rheumatic diseases. Osteoimmunology has also allowed an improvement in our knowledge of the structure-sparing effects of antirheumatic drug therapy. Moreover, recent advances in the understanding of the molecular regulation of osteophyte formation are based on the characterization of the regulation of bone formation by inflammation. This review highlights the key insights into the regulation of bone destruction and formation in arthritis. Moreover, concepts of how bone influences the immune system are discussed.
Introduction
Two major aspects determine the clinical picture of rheumatic diseases. The first one is that inflammation is considered a central component of many, especially the most severe, forms of rheumatic diseases. Based on the observation of auto-antibody formation and the accumulation of cells of the adaptive immune system at sites of inflammation, some rheumatic diseases, such as rheumatoid arthritis (RA), systemic lupus erythematosus, or Sjögren syndrome, are considered to be classic systemic autoimmune diseases. Chronic immune activation is regarded as a central triggering factor for inflammatory rheumatic diseases. The second key aspect is how the musculoskeletal tissue is affected, which is the common target organ of this disease group. Musculoskeletal tissue experiences progressive damage, which is the basis for a functional impairment and a high disease burden. The combination of chronic immune activation and musculoskeletal tissue damage is the hallmark of rheumatic diseases. A detailed understanding of the pathophysiological processes of rheumatic diseases thus requires an understanding of the mutual interactions between the immune system and musculoskeletal tissue.
Current concepts of osteoimmunology
Osteoimmunology is one of the areas that allow investigators to gain novel insights into the crosstalk between the immune and the musculoskeletal systems [1]. This field of research is particularly relevant to the understanding of rheumatic diseases, which are characterized by profound alterations of bone architecture aside from immune activation. The term osteoimmunology is a rather novel one. It was created in the late 1990s after landmark observations demonstrating that T lymphocytes triggered bone loss by inducing the differentiation of bone-resorbing cells termed osteoclasts [2-4]. This concept puts two, at first glance fundamentally different, organ systems – the immune system and the skeleton – in much closer relation to each other than one could ever expect.
Current concepts of osteoimmunology which are of relevance to rheumatology involve (a) the regulation of bone degradation by the immune system, (b) the interaction between inflammation and bone formation, and (c) the role of bone and bone marrow as a niche for immune cells, particularly plasma cells (PCs). The first concept, immune-mediated regulation of bone loss, has been studied intensively in recent years and has become a well-developed concept that is instrumental in the understanding of the different forms of bone loss in the course of rheumatic diseases. In contrast, the second concept, the molecular interactions between inflammation and bone formation, is still much less developed but is important in defining the mechanisms of repair of structural damage in the joint as well as in explaining the pathophysiology of bony ankylosis. Similarly, the third concept, the bone marrow niche, is still incompletely understood but is particularly relevant to the understanding of immune cell trafficking during inflammatory diseases (that is, the triggers for the recruitment of immune cells from the bone marrow into the inflammatory sites) and to explaining the formation of a stable microenvironment, which allows longevity and antibody production by long-lived PCs.
Osteoclasts as triggers of arthritic bone erosions
Erosion of periarticular bone is a central feature of RA and psoriatic arthritis [5,6]. Bone erosion mirrors a destructive process in joints affected by arthritis as it reflects damage triggered by chronic inflammation. Visualization of bone erosions by imaging techniques is important not only for diagnosing RA but also for defining severity of disease and response to antirheumatic therapy [7]. Bone erosions require the presence of osteoclasts in the joint as osteoclasts are the only cell type capable of removing calcium from bone and, therefore, of degrading bone matrix. Osteoclasts are part of the inflamed synovial tissue of human RA and psoriatic arthritis as well as of all major experimental models of arthritis. Bromley and Woolley [8] and Gravallese and colleagues [9] provided the first detailed description of osteoclasts in inflamed joints in the late 1990s, showing that mature osteoclasts are localized at the site of bone erosion in RA joints. Later, the essential function of osteoclasts in triggering inflammatory bone erosions was shown by blocking essential molecules for osteoclastogenesis or by using mice deficient in osteoclasts [10,11]. In all of these models, no bone erosions formed when osteoclasts were either effectively blocked or genetically depleted, despite the presence of synovial inflammation. These findings clearly showed that osteoclasts are essential to the formation of bone erosions and structural damage in inflamed joints.
Molecular and cellular mechanisms of inflammatory bone erosion
What are the mechanisms leading to enhanced osteoclast formation along joints? There are two key mechanisms that are essential to the formation of osteoclasts in joints: first, the accumulation of cells that serve as osteoclast precursors in the joint, and, second, stimulation of differentiation of these cells into the osteoclast lineage. Osteoclast precursors are mononuclear cells belonging to the monocyte/macrophage lineage [12]. Early monocytic precursor cells have the potential to differentiate into macrophages, dendritic cells, osteoclasts, and other more organ-specific cell lineage types such as Kupffer cells in the liver or microglia in the brain. It is not fully clear whether some monocytes entering an inflamed joint are already committed to the osteoclast linage or 'decide' locally within the synovium upon receiving the appropriate signals. Nonetheless, experimental evidence supports the view that the peripheral monocytic pool changes during inflammation. For instance, the fraction of CD11b+ cells that serve as osteoclast precursors increases, suggesting that an increased number of cells entering the joint can differentiate into osteoclasts [13]. Moreover, cytokines such as tumor necrosis factor (TNF) already induce the expression of receptors on the surface of monocytes, which are important for osteoclast differentiation. One of them is OSCAR (osteoclast-associated receptor), an important costimulation molecule for osteoclasts [14]. Much less is known about surface receptors on monocytes, which can negatively regulate their differentiation into osteoclasts. In fact, one such molecule is CD80/CD86, which effectively blocks osteoclast formation when bound to CTLA4, a negative regulator of T-cell costimulation by monocytes [15,16]. This could link regulatory T cells, which highly express CTLA4 on their surface, to bone homeostasis as these cells can suppress osteoclast formation independently of RANKL (receptor activator of nuclear factor-kappa B ligand).
The second mechanism is that monocytic osteoclast precursors which have already entered the inflamed joints are allowed to further differentiate into osteoclasts (Figure 1). This process requires intensive crosstalk with other cells, particularly with synovial fibroblast-like cells and activated T cells. Among T cells, both TH1 and TH17 subsets are of importance in this process. Both cell types inducibly express RANKL, which is an essential stimulating signal for osteoclastogenesis and is also involved in the activation of mature osteoclasts [3,17]. RANKL binds a surface receptor on the precursor cells termed RANK, which induces signaling via nuclear factor-kappa-B and the activation protein-1 transcription factor family, which are important for osteoclast differentiation [2,3]. This essential osteoclastogenic cytokine is expressed in the synovium of patients with RA, suggesting that it actively contributes to the formation of osteoclasts in the synovium [18,19]. A high level of RANKL expression is apparently not balanced by expression of regulatory molecules such as osteoprotegerin (OPG), a decoy receptor of RANKL which blocks osteoclast formation [20], suggesting that this imbalance appears to be of importance in yielding a negative net effect on local bone mass in the case of arthritis. This concept is supported not only by data obtained in animal models of arthritis showing effective protection from structural damage when blocking RANKL with OPG, but also by a recent clinical study showing that an antibody against RANKL (denosumab) provides protection from the progression of structural damage in RA patients [21].
Figure 1.
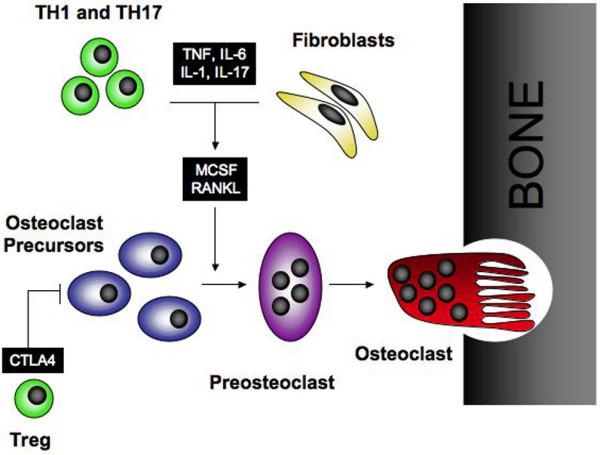
Osteoclast formation in the joint. Monocytic cells in the synovium serve as osteoclast precursors. Upon exposure to macrophage colony-stimulating factor (MCSF) and RANKL synthesized by T cells and synovial fibroblasts, osteoclasts fuse to polykaryons termed preosteoclasts, which then undergo further differentiation into mature osteoclasts, acquiring specific features such as the ruffled membrane. Inflammatory cytokines such as tumor necrosis factor (TNF) and interleukin (IL)-1, IL-6, and IL-17 increase the expression of RANKL and thus support osteoclastogenesis in the joint. In contrast, regulatory T (Treg) cells block osteoclast formation via CTLA4. RANKL, receptor activator of nuclear factor-kappa B ligand.
Apart from RANKL, the osteoclastogenic properties of the inflamed synovial membrane are further enhanced by the expression of macrophage colony-stimulating factor, which is essential for osteoclast formation as well [22]. Moreover, proinflammatory cytokines such as TNF and interleukin (IL)-1, IL-6, and IL-17 are all potent inducers of RANKL expression and thus enhance osteoclast differentiation as well. Some of these cytokines additionally exert direct effects on osteoclast precursors, and TNF, in particular, engages TNF-receptor type I on the surface of osteoclast precursors, stimulating their differentiation into osteoclasts [23]. This link between proinflammatory cytokines and osteoclast formation most likely explains why cytokine-targeted therapy, particularly blockade of TNF, is highly effective in retarding structural damage in RA. Thus, TNF-blocking agents virtually arrest radiographic damage in RA and are considered excellent agents for achieving structural protection of joints [24-29]. Although there are no data from randomized controlled trials which define the structure-sparing effect of tocilizumab in addition to its well-established anti-inflammatory effect [30,31], one can anticipate such an effect based on the observation that IL-6 drives RANKL expression and thus supports osteoclastogenesis [32].
Periarticular and systemic bone loss in rheumatic disease
Periarticular bone loss has long been known as a radiographic sign for RA and has been explained by paracrine effects of the inflammatory tissue on periarticular bone. Still, periarticular bone loss (also termed periarticular osteoporosis) has been poorly defined so far. Apparently, peri-articular bone loss is based on a substantial decrease in bone trabeculae along the metaphyses of bones close to inflamed joints, suggesting that the bone marrow cavity along inflamed joints is also part of the disease process of arthritis. This is supported by data from magnetic resonance imaging (MRI) studies in patients with RA which have unraveled a high frequency of signal alterations in the juxta-articular bone marrow in addition to synovitis outside the cortical bone barrier [33,34]. These lesions are water-rich lesions which have a low fat content, suggesting that bone marrow fat has been locally replaced by water-rich tissue. Histological examination of bone marrow lesions has been carried out in joints of advanced-stage RA patients undergoing joint replacement surgery. These studies have shown that bone marrow lesions visualized in MRI contain (water-rich) vascularized inflammatory infiltrates which replace bone marrow fat and harbor aggregates of B cells and T cells. Importantly, very similar, if not identical, MRI changes are found early in the disease process of RA and have been shown to be linked to subsequent bone erosions in the same joints [35]. Bone marrow lesions are often linked to a cortical penetration of inflammatory tissue either by means of bone erosions or by small cortical bone channels which connect the synovium with the juxta-articular bone marrow. Moreover, bone marrow lesions are associated with an endosteal bone response as they coincide with the accumulation of osteoblasts and the deposition of bone matrix in the endosteum [36]. These novel data have enhanced our view of arthritis as a disease that is not solely confined to the synovial membrane but that extends to bone marrow.
It has long been known that inflammatory diseases, including RA and ankylosing spondylitis (AS), lead to osteoporosis and increased fracture risk. Data obtained in recent years have supported these concepts and have shed more light on osteoporosis and fracture risk in RA patients. Osteopenia and osteoporosis are frequent concomitant diseases in patients with RA and are even observed in rather high frequency before any disease-modifying antirheumatic drug or glucocorticoid therapy is started. Roughly 25% of patients with RA show an osteopenic bone mineral density at the spine or hip before the onset of therapy in early RA patients, and 10% have osteoporosis [37]. This suggests that RA patients are at high risk to develop complications from systemic bone loss as the prevalence of low bone mass is already high at the onset of disease. The reasons for this appear to be based on the coincidence of standard risk factors for osteoporosis with the onset of RA such as higher age and female gender. Another explanation is the possibility that low-grade inflammation often long precedes the onset of clinical symptoms of RA. Indeed, as independent population-based studies have shown, even small elevations of C-reactive protein as a sign of low-grade inflammation in the normal healthy population dramatically increase fracture risk [38]. Fracture risk is indeed higher in RA patients as it has been confirmed by a recent meta-analysis of nine prospective population-based cohorts which showed that fracture risk doubles with the diagnosis of RA, regardless of whether glucocorticoids are used or not [39]. Similarly, a large case control study based on the British General Practice Research Database has shown that RA doubles the risk of hip and vertebral facture, clearly supporting the concept that inflammation is an independent risk factor for osteoporosis [40].
Osteoimmunological aspects of bone formation in rheumatic disease
To gain a balanced view of the interaction between the immune system and bone, it is important to better define how immune activation controls bone formation. Inflammatory arthritides show profound differences in joint architecture. These cover the whole spectrum; from an almost purely erosive disease like RA, to a mixed pattern with concurrent erosions and bone formation, and prominently bone-forming patterns of disease as observed in AS. Given this observation, the regulation of bone formation becomes an interesting aspect of rheumatic diseases. In RA, there is little sign of repair of bone erosions, which is astonishing considering that bone formation is usually coupled to bone resorption and increased rate of bone resorption should this entail increased bone formation. This, however, is by no means the case in RA, which is virtually a purely erosive disease. Recent data suggest that bone formation is actively suppressed by inflammation. Interestingly, TNF potently suppresses bone formation by enhancing the expression of dickkopf-1 (DKK1), a protein that negatively regulates the Wnt signaling pathway [41]. Wnt signals a key trigger for bone formation by enhancing the differentiation of osteoblasts from their mesenchymal cell precursors. Wnt proteins are also involved in the regulation of osteoclastogenesis since they enhance the expression of OPG and block osteoclast formation [42]. Thus, influencing the balance of Wnt proteins and their inhibitors is a very potent strategy to disturb bone homeostasis: Low levels of Wnt activity yield low bone formation and high bone resorption, whereas high levels of Wnt activity increase bone formation and simultaneously block bone resorption. In RA, the former scenarios appear to be relevant since bone resorption is increased and bone formation is decreased. Inhibitors of Wnt, like DKK1, are expressed in the synovial tissue of RA patients, suggesting suppression of bone formation. This concept is further supported by the paucity of fully differentiated osteoblasts within arthritic bone erosions, which indicates that there is indeed no major bone formation taking place in these lesions.
Pure degradation of bone during arthritis is rather the exception than the rule in joint disease. Psoriatic arthritis, AS, but also osteoarthritis and metabolic arthropathies such as hemochromatosis arthropathy are partly or even predominantly characterized by bony spurs along joints and intervertebral spaces. These lesions are based on new bone formation. We have recently observed that osteophyte formation cannot easily be compared with erosive structural damage observed in RA and that therapies blocking bone erosions such as TNF blockade do not influence the formation of osteophytes [43]. Areas that are prone to osteophyte formation are (a) periarticular sites of the periosteum in the vicinity of the articular cartilage, (b) edges of vertebral bodies, and (c) the insertion sites of tendons. These sites are particularly rich with fibro cartilage, which is considered a tissue from which osteophyte formation emerges given that certain triggering factors interact [44]. Triggers are certainly mechanical factors since osteophytes often emerge at the entheses along the insertion sites of the tendons. Usually, osteophytes are based on endochondral ossification, which first leads to differentiation of hypertrophic chondrocytes from mesenchymal cells and abundant deposition of extracellular matrix before rebuilding into bone occurs, which requires differentiation of osteoblasts and deposition of bone. Molecular signals involved in osteophyte formation have recently been defined: Transforming growth factor-beta as well as bone morphogenic proteins (BMPs) facilitate osteophyte formation, and active BMP signaling through Smad3 proteins has been demonstrated in human osteophyte formation [45]. Moreover, noggin, an inhibitor of BMPs, effectively blocks osteophyte formation, suggesting that this protein family plays a key role in the formation of bony spurs by facilitating osteoblast differentiation [45]. Another essential protein family involved in osteophyte formation is the Wnt protein family. These proteins bind to surface receptors like LRP5/6 and frizzled proteins on the surface of mesenchymal cells, leading to signaling through β-catenin, which translocates to the nucleus and activated genes involved in bone formation. Nuclear translocation of β-catenin is observed at sites of bony spurs, suggesting its activation by Wnt proteins. There appears to be tight crosstalk between Wnt protein and BMP proteins as these two protein families act synergistically on bone formation. Moreover, there are crosstalks to the RANKL-OPG system, and Wnt proteins induce the expression of OPG, which shuts down bone resorption [46]. It thus appears that the balance between bone-forming factors such as Wnt and BMP proteins and bone-resorbing factors such as RANKL and TNF is crucial to how a joint remodels during arthritis.
Bone marrow as a niche for B-cell differentiation and autoantibody formation
Osteoimmunology research in recent years has been dominated by mechanisms that explain the influence of the immune system on bone, but there are other areas in which bone-immune interactions play an important role. Hematopoiesis in the bone marrow is thought to depend on special microenvironments, known as niches, that maintain blood cells. Although the identity of niches and the interaction of blood cells are still poorly understood, they appear to be important in early B-cell differentiation as well as survival of long-lived B cells and PCs [47]. Both the earliest precursors, pre-pro-B cells and end-stage B cells, PCs require CXC chemokine ligand (CXCL) 12 to home to the bone marrow (Figure 2). CXCL12-expressing cells are a small population of bone marrow stromal cells that are scattered throughout bone marrow and that are distinct from the cells expressing IL-7 adjoining more mature pro-B cells [48]. These cells not only allow homing of memory B cells and PCs to the bone marrow but also provide survival signals that allow the longevity of these cells and prevent apoptosis. Thus, long-lived memory B cells and PCs are dependent not only on affinity maturation but also on an acquired ability to survive. Successful competition for survival niches thus appears to be a key factor explaining the longevity of these cells. Apparently, by means of CXCL12-induced chemotaxis, PCs traffic into these survival niches in the bone marrow, where they produce antibodies and persist. If bone marrow homing of PCs is disturbed (which is seen in murine lupus models, where PCs are unresponsive to CXCL12), a marked accumulation of PCs in the spleen is observed [47]. Also, circulating B cells might only become memory B cells if they find appropriate survival conditions outside of restimulating secondary lymphoid organs.
Figure 2.
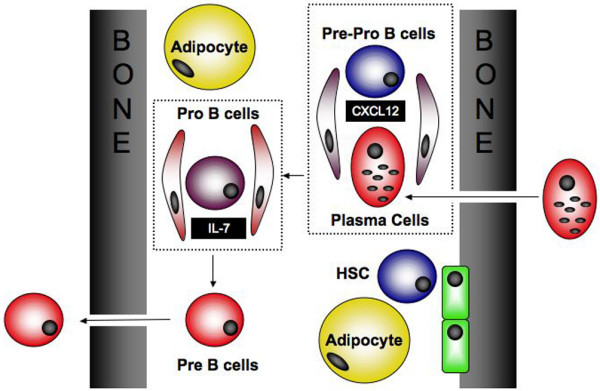
Bone marrow niche. Pre-pro-B cells share a common niche with plasma cells based on the expression of CXC chemokine ligand-12 (CXCL12) by bone marrow stromal cells. Upon further differentiation into pro-B cells, cells switch to a different niche, which is based on interleukin-7 (IL-7)-expressing bone marrow stromal cells. Further differentiation of B cells into pre-B cells makes them independent from bone marrow niches before leaving bone marrow to secondary lymphatic organs. Plasma cells re-entering the bone marrow share the CXCL12-triggered bone marrow niche with pre-pro B cells, as described above. Hematopoietic stem cells (HSCs) are linked to bone marrow niches created by osteoblasts.
Conclusion
Osteoimmunology has considerably refined our insights into the pathogenesis of rheumatic diseases, particularly arthritis. We have begun to understand the molecular interactions between immune activation and the skeletal system which link inflammatory diseases with bone loss. Knowledge of these pathways will allow us to tailor drug therapies to target skeletal damage more specifically and thus more effectively. In addition, further insights into the role of bone and bone marrow in shaping immune responses, particularly in maintaining PCs in the bone marrow niche, will open a new perspective in autoimmune diseases.
Abbreviations
AS: ankylosing spondylitis; BMP: bone morphogenic protein; CXCL: CXC chemokine ligand; DKK1: dickkopf-1; IL: interleukin; MRI: magnetic resonance imaging; OPG: osteoprotegerin; PC: plasma cell; RA: rheumatoid arthritis; RANKL: receptor activator of nuclear factor-kappa B ligand; TNF: tumor necrosis factor.
Competing interests
The author declares that he has no competing interests.
Note
The Scientific Basis of Rheumatology: A Decade of Progress
This article is part of a special collection of reviews, The Scientific Basis of Rheumatology: A Decade of Progress, published to mark Arthritis Research & Therapy's 10th anniversary.
Other articles in this series can be found at: http://arthritis-research.com/sbr
References
- Takayanagi H. Osteoimmunology: shared mechanisms and crosstalk between the immune and bone systems. Nat Rev Immunol. 2007;7:292–304. doi: 10.1038/nri2062. [DOI] [PubMed] [Google Scholar]
- Lacey DL, Timms E, Tan HL, Kelley MJ, Dunstan CR, Burgess T, Elliott R, Colombero A, Elliott G, Scully S, Hsu H, Sullivan J, Hawkins N, Davy E, Capparelli C, Eli A, Qian YX, Kaufman S, Sarosi I, Shalhoub V, Senaldi G, Guo J, Delaney J, Boyle WJ. Osteoprotegerin ligand is a cytokine that regulates osteoclast differentiation and activation. Cell. 1998;93:165–176. doi: 10.1016/S0092-8674(00)81569-X. [DOI] [PubMed] [Google Scholar]
- Kong YY, Yoshida H, Sarosi I, Tan HL, Timms E, Capparelli C, Morony S, Oliveirados-Santos AJ, Van G, Itie A, Khoo W, Wakeham A, Dunstan CR, Lacey DL, Mak TW, Boyle WJ, Penninger JM. OPGL is a key regulator of osteoclastogenesis, lymphocyte development and lymph-node organogenesis. Nature. 1999;397:315–323. doi: 10.1038/16852. [DOI] [PubMed] [Google Scholar]
- Horwood NJ, Kartsogiannis V, Quinn JM, Romas E, Martin TJ, Gillespie MT. Activated T lymphocytes support osteoclast formation in vitro. Biochem Biophys Res Commun. 1999;265:144–150. doi: 10.1006/bbrc.1999.1623. [DOI] [PubMed] [Google Scholar]
- McInnes I, Schett G. Cytokines in the pathogenesis of rheumatoid arthritis. Nat Immunol. 2007;7:429–442. doi: 10.1038/nri2094. [DOI] [PubMed] [Google Scholar]
- Firestein GS. Evolving concepts of rheumatoid arthritis. Nature. 2003;423:356–361. doi: 10.1038/nature01661. [DOI] [PubMed] [Google Scholar]
- Heijde DM Van der. Joint erosions and patients with early rheumatoid arthritis. Br J Rheumatol. 1995;34:74–78. [PubMed] [Google Scholar]
- Bromley M, Woolley DE. Chondroclasts and osteoclasts at subchondral sites of erosion in the rheumatoid joint. Arthritis Rheum. 1984;27:968–975. doi: 10.1002/art.1780270902. [DOI] [PubMed] [Google Scholar]
- Gravallese EM, Harada Y, Wang JT, Gorn AH, Thornhill TS, Goldring SR. Identification of cell types responsible for bone resorption in rheumatoid arthritis and juvenile rheumatoid arthritis. Am J Pathol. 1998;152:943–951. [PMC free article] [PubMed] [Google Scholar]
- Pettit AR, Ji H, von Stechow D, Müller R, Goldring SR, Choi Y, Benoist C, Gravallese EM. TRANCE/RANKL knockout mice are protected from bone erosion in a serum transfer model of arthritis. Am J Pathol. 2001;159:1689–1699. doi: 10.1016/S0002-9440(10)63016-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Redlich K, Hayer S, Ricci R, David JP, Tohidast-Akrad M, Kollias G, Steiner G, Smolen JS, Wagner EF, Schett G. Osteoclasts are essential for TNF-alpha-mediated joint destruction. J Clin Invest. 2002;110:1419–1427. doi: 10.1172/JCI15582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teitelbaum SL. Bone resorption by osteoclasts. Science. 2000;289:1504–1508. doi: 10.1126/science.289.5484.1504. [DOI] [PubMed] [Google Scholar]
- Ritchlin CT, Haas-Smith SA, Li P, Hicks DG, Schwarz EM. Mechanisms of TNF-alpha- and RANKL-mediated osteoclastogenesis and bone resorption in psoriatic arthritis. J Clin Invest. 2003;111:821–831. doi: 10.1172/JCI16069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herman S, Mueller R, Kronke G, Zwerina J, Redlich K, Hueber A, Gelse H, Neumann E, Mueller-Ladner , Schett G. OSCAR, a key co-stimulation molecule for osteoclasts, is induced in patients with rheumatoid arthritis. Arthritis Rheum. 2009 doi: 10.1002/art.23943. [DOI] [PubMed] [Google Scholar]
- Zaiss MM, Axmann R, Zwerina J, Polzer K, Gückel E, Skapenko A, Schulze-Koops H, Horwood N, Cope A, Schett G. Treg cells suppress osteoclast formation: a new link between the immune system and bone. Arthritis Rheum. 2007;56:4104–4112. doi: 10.1002/art.23138. [DOI] [PubMed] [Google Scholar]
- Axmann R, Herman S, Zaiss M, Franz S, Polzer K, Zwerina J, Herrmann M, Smolen J, Schett G. CTLA-4 directly inhibits osteoclast formation. Ann Rheum Dis. 2008;67:1603–1609. doi: 10.1136/ard.2007.080713. [DOI] [PubMed] [Google Scholar]
- Sato K, Suematsu A, Okamoto K, Yamaguchi A, Morishita Y, Kadono Y, Tanaka S, Kodama T, Akira S, Iwakura Y, Cua DJ, Takayanagi H. Th17 functions as an osteoclastogenic helper T cell subset that links T cell activation and bone destruction. J Exp Med. 2006;203:2673–2682. doi: 10.1084/jem.20061775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gravallese EM, Manning C, Tsay A, Naito A, Pan C, Amento E, Goldring SR. Synovial tissue in rheumatoid arthritis is a source of osteoclast differentiation factor. Arthritis Rheum. 2000;43:250–258. doi: 10.1002/1529-0131(200002)43:2<250::AID-ANR3>3.0.CO;2-P. [DOI] [PubMed] [Google Scholar]
- Shigeyama Y, Pap T, Kunzler P, Simmen BR, Gay RE, Gay S. Expression of osteoclast differentiation factor in rheumatoid arthritis. Arthritis Rheum. 2000;43:2523–2530. doi: 10.1002/1529-0131(200011)43:11<2523::AID-ANR20>3.0.CO;2-Z. [DOI] [PubMed] [Google Scholar]
- Stolina M, Adamu S, Ominsky M, Dwyer D, Asuncion F, Geng Z, Middleton S, Brown H, Pretorius J, Schett G, Bolon B, Feige U, Zack D, Kostenuik PJ. RANKL is a marker and mediator of local and systemic bone loss in two rat models of inflammatory arthritis. J Bone Miner Res. 2005;20:1756–1765. doi: 10.1359/JBMR.050601. [DOI] [PubMed] [Google Scholar]
- Cohen SB, Dore RK, Lane NE, Ory PA, Peterfy CG, Sharp JT, Heijde D van der, Zhou L, Tsuji W, Newmark R, Denosumab Rheumatoid Arthritis Study Group Denosumab treatment effects on structural damage, bone mineral density and bone turover in rheumatoid arthritis. Arthritis Rheum. 2008;58:1299–1309. doi: 10.1002/art.23417. [DOI] [PubMed] [Google Scholar]
- Seitz M, Loetscher P, Fey MF, Tobler A. Constitutive mRNA and protein production of macrophage colony-stimulating factor but not of other cytokines by synovial fibroblasts from rheumatoid arthritis and osteoarthritis patients. Br J Rheumatol. 1994;33:613–619. doi: 10.1093/rheumatology/33.7.613. [DOI] [PubMed] [Google Scholar]
- Lam J, Takeshita S, Barker JE, Kanagawa O, Ross FP, Teitelbaum SL. TNF-alpha induces osteoclastogenesis by direct stimulation of macrophages exposed to permissive levels of RANK ligand. J Clin Invest. 2000;106:1481–1488. doi: 10.1172/JCI11176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klareskog L, Heijde D van der, de Jager JP, Gough A, Kalden J, Malaise M, Martín Mola E, Pavelka K, Sany J, Settas L, Wajdula J, Pedersen R, Fatenejad S, Sanda M, TEMPO (Trial of Etanercept and Methotrexate with Radiographic Patient Outcomes) study investigators Therapeutic effect of the combination of etanercept and methotrexate compared with each treatment alone in patients with rheumatoid arthritis: double-blind randomised controlled trial. Lancet. 2004;363:675–681. doi: 10.1016/S0140-6736(04)15640-7. [DOI] [PubMed] [Google Scholar]
- Smolen JS, Heijde DM Van Der, St Clair EW, Emery P, Bathon JM, Keystone E. Predictors of joint damage in patients with early rheumatoid arthritis treated with high-dose methotrexate with or without concomitant infliximab: results from the ASPIRE trial. Arthritis Rheum. 2006;54:702–710. doi: 10.1002/art.21678. [DOI] [PubMed] [Google Scholar]
- Keystone EC, Kavanaugh AF, Sharp JT, Tannenbaum H, Hua Y, Teoh LS, Fischkoff SA, Chartash EK. Radiographic, clinical and functional outcomes of treatment with adalimumab (a human anti-tumor necrosis factor monoclonal antibody) in patients with active rheumatoid arthritis receiving concomitant methotrexate therapy: a randomized placebo-controlled 52-week trial. Arthritis Rheum. 2004;50:1400–1411. doi: 10.1002/art.20217. [DOI] [PubMed] [Google Scholar]
- Lipsky PE, Heijde DM van der, St Clair EW, Furst DE, Breedveld FC, Kalden JR, Smolen JS, Weisman M, Emery P, Feldmann M, Harriman GR, Maini RN, Anti-Tumor Necrosis Factor Trial in Rheumatoid Arthritis with Concomitant Therapy Study Group Infliximab and methotrexate in the treatment of rheumatoid arthritis. Anti-Tumor Necrosis Factor Trial in Rheumatoid Arthritis with Concomitant Therapy Study Group. N Engl J Med. 2000;343:1594–1602. doi: 10.1056/NEJM200011303432202. [DOI] [PubMed] [Google Scholar]
- Weinblatt ME, Keystone EC, Furst DE, Moreland LW, Weisman MH, Birbara CA, Teoh LA, Fischkoff SA, Chartash EK. Adalimumab, a fully human anti-tumor necrosis factor alpha monoclonal antibody, for the treatment of rheumatoid arthritis in patients taking concomitant methotrexate: the ARMADA trial. Arthritis Rheum. 2003;48:35–45. doi: 10.1002/art.10697. [DOI] [PubMed] [Google Scholar]
- Maini R, St Clair EW, Breedveld F, Furst D, Kalden J, Weisman M, Smolen J, Emery P, Harriman G, Feldmann M, Lipsky P. Infliximab (chimeric anti-tumour necrosis factor alpha monoclonal antibody) versus placebo in rheumatoid arthritis patients receiving concomitant methotrexate: a randomised phase III trial. ATTRACT Study Group. Lancet. 1999;354:1932–1939. doi: 10.1016/S0140-6736(99)05246-0. [DOI] [PubMed] [Google Scholar]
- Maini RN, Taylor PC, Szechinski J, Pavelka K, Bröll J, Balint G, Emery P, Raemen F, Petersen J, Smolen J, Thomson D, Kishimoto T, CHARISMA Study Group Double-blind randomized controlled clinical trial of the interleukin-6 receptor antagonist, tocilizumab, in European patients with rheumatoid arthritis who had an incomplete response to methotrexate. Arthritis Rheum. 2006;54:2817–2829. doi: 10.1002/art.22033. [DOI] [PubMed] [Google Scholar]
- Smolen JS, Beaulieu A, Rubbert-Roth A, Ramos-Remus C, Rovensky J, Alecock E, Woodworth T, Alten R, OPTION Investigators Effect of interleukin-6 receptor inhibition with tocilizumab in patients with rheumatoid arthritis (OPTION study): a double-blind, placebo-controlled, randomised trial. Lancet. 2008;371:987–997. doi: 10.1016/S0140-6736(08)60453-5. [DOI] [PubMed] [Google Scholar]
- Wong PK, Quinn JM, Sims NA, van Nieuwenhuijze A, Campbell IK, Wicks IP. Interleukin-6 modulates production of T lymphocyte-derived cytokines in antigen-induced arthritis and drives inflammation-induced osteoclastogenesis. Arthritis Rheum. 2006;54:158–168. doi: 10.1002/art.21537. [DOI] [PubMed] [Google Scholar]
- McQueen FM, Gao A, Østergaard M, King A, Shalley G, Robinson E, Doyle A, Clark B, Dalbeth N. High-grade MRI bone oedema is common within the surgical field in rheumatoid arthritis patients undergoing joint replacement and is associated with osteitis in subchondral bone. Ann Rheum Dis. 2007;66:1581–1587. doi: 10.1136/ard.2007.070326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conaghan P, Bird P, Ejbjerg B, O'Connor P, Peterfy C, McQueen F, Lassere M, Emery P, Shnier R, Edmonds J, Østergaard M. The EULAR–OMERACT rheumatoid arthritis MRI reference image atlas: the metacarpophalangeal joints. Ann Rheum Dis. 2005;64:i11–i21. doi: 10.1136/ard.2004.031815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McQueen FM, Benton N, Perry D, Crabbe J, Robinson E, Yeoman S, McLean L, Stewart N. Bone edema scored on magnetic resonance imaging scans of the dominant carpus at presentation predicts radiographic joint damage of the hands and feet six years later in patients with rheumatoid arthritis. Arthritis Rheum. 2003;48:1814–1827. doi: 10.1002/art.11162. [DOI] [PubMed] [Google Scholar]
- Jimenez-Boj E, Redlich K, Turk B, Hanslik-Schnabel B, Wanivenhaus A, Chott A, Smolen JS, Schett G. Interaction between synovial inflammatory tissue and bone marrow in rheumatoid arthritis. J Immunol. 2005;175:2579–2588. doi: 10.4049/jimmunol.175.4.2579. [DOI] [PubMed] [Google Scholar]
- Güler-Yüksel M, Bijsterbosch J, Goekoop-Ruiterman YP, de Vries-Bouwstra JK, Ronday HK, Peeters AJ, de Jonge-Bok JM, Breedveld FC, Dijkmans BA, Allaart CF, Lems WF. Bone mineral density in patients with recently diagnosed, active rheumatoid arthritis. Ann Rheum Dis. 2007;66:1508–1512. doi: 10.1136/ard.2007.070839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schett G, Kiechl S, Weger S, Pederiva A, Mayr A, Petrangeli M, Oberhollenzer F, Lorenzini R, Redlich K, Axmann R, Zwerina J, Willeit J. High-sensitivity C-reactive protein and risk of non-traumatic fractures in the Bruneck study. Arch Intern Med. 2006;166:2495–2501. doi: 10.1001/archinte.166.22.2495. [DOI] [PubMed] [Google Scholar]
- Kanis JA, Johnell O, Oden A, Johansson H, McCloskey E. FRAX and the assessment of fracture probability in men and women from the UK. Osteoporos Int. 2008;19:385–397. doi: 10.1007/s00198-007-0543-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Staa TP, Geusens P, Bijlsma JW, Leufkens HG, Cooper C. Clinical assessment of the long-term risk of fracture in patients with rheumatoid arthritis. Arthritis Rheum. 2006;54:3104–3101. doi: 10.1002/art.22117. [DOI] [PubMed] [Google Scholar]
- Diarra D, Stolina M, Polzer K, Zwerina J, Ominsky MS, Dwyer D, Korb A, Smolen J, Hoffmann M, Scheinecker C, Heijde D van der, Landewe R, Lacey D, Richards WG, Schett G. Dickkopf-1 is a master regulator of joint remodeling. Nat Med. 2007;13:156–163. doi: 10.1038/nm1538. [DOI] [PubMed] [Google Scholar]
- Glass DA, Bialek P, Ahn JD, Starbuck M, Patel MS, Clevers H, Taketo MM, Long F, McMahon AP, Lang RA, Karsenty G. Canonical Wnt signaling in differentiated osteoblasts controls osteoclast differentiation. Dev Cell. 2005;8:751–764. doi: 10.1016/j.devcel.2005.02.017. [DOI] [PubMed] [Google Scholar]
- Sieper J, Appel H, Braun J, Rudwaleit M. Critical appraisal of assessment of structural damage in ankylosing spondylitis: implications for treatment outcomes. Arthritis Rheum. 2008;58:649–656. doi: 10.1002/art.23260. [DOI] [PubMed] [Google Scholar]
- Benjamin M, McGonagle D. The anatomical basis for disease localization in seronegative spondylarthropathy at entheses and related sites. J Anat. 2001;199:503–526. doi: 10.1046/j.1469-7580.2001.19950503.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lories RJ, Derese I, Luyten FP. Modulation of bone morphogenetic protein signaling inhibits the onset and progression of ankylosing enthesitis. J Clin Invest. 2005;115:1571–1579. doi: 10.1172/JCI23738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manz RA, Arce S, Cassese G, Hauser AE, Hiepe F, Radbruch A. Humoral immunity and long-lived plasma cells. Curr Opin Immunol. 2002;14:517–521. doi: 10.1016/S0952-7915(02)00356-4. [DOI] [PubMed] [Google Scholar]
- Tokoyoda K, Egawa T, Sugiyama T, Choi BI, Nagasawa T. Cellular niches controlling B lymphocyte behavior within bone marrow during development. Immunity. 2004;20:707–718. doi: 10.1016/j.immuni.2004.05.001. [DOI] [PubMed] [Google Scholar]
- Erickson LD, Lin LL, Duan B, Morel L, Noelle RJ. A genetic lesion that arrests plasma cell homing to the bone marrow. Proc Natl Acad Sci USA. 2003;100:12905–12910. doi: 10.1073/pnas.2131686100. [DOI] [PMC free article] [PubMed] [Google Scholar]


