Abstract
Background
Bone repair alteration is hypothesized for nonunion fracture pathogenesis. Since it is involved in osteoclast regulation, the RANK/RANKL/OPG system (receptor activator of nuclear factor kB/its ligand/osteoprotegerin) may play a role.
Materials and methods
Serum OPG, free RANKL, bone alkaline phosphatase (BAP), osteocalcin (OC), and urinary deoxypyridinoline (DPD) were determined in 16 male patients (20–39 years) with long bone atrophic nonunion fractures. Serum markers were also measured in 18 age-matched male controls who healed from the same type of fractures within six months, and in 14 age-matched male controls who were healing from the same fractures one month after injury. One-way ANOVA and Bonferroni’s test were used for statistical analysis.
Results
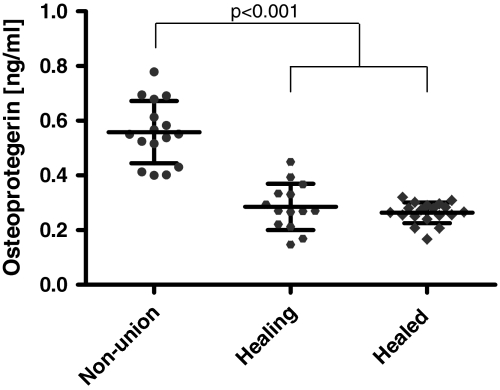
Only OPG was significantly higher (0.56 sd 0.11 ng/ml) in the patients compared to healed (0.26 sd 0.04 ng/ml; P < 0.001) and healing (0.29 sd 0.09 ng/ml; P < 0.001) controls. The patients’ DPD levels were normal. No correlations were found between bone markers and the characteristics of the subjects in all groups.
Conclusions
A normal steady state of bone metabolism seems to be present in patients with atrophic nonunion fractures, despite the high serum OPG. The reason for the inability of the patients’ OPG to inhibit osteoclastic activity is unknown. Osteoblast activity also appears normal, so another cellular source of OPG can be hypothesized.
Keywords: Bone turnover markers, Nonunion, Osteoprotegerin, Shaft fractures
Introduction
Shaft fracture nonunion is an unpredictable complication of orthopedic surgery that occurs in 5–10% of all fractures [1]. Nonunions are usually classifed into two subsets according to callus development, hypotrophic–atrophic and hypertrophic, which are radiologically distinguishable. Some recent studies on animal models and on human bioptic specimens showed that there are no vascularization differences between both atrophic and hypertrophic non-nion fractures and normal healing fractures [2, 3]. Furthermore, an ex vivo study on bioptic samples of nonunion neighboring tissue has evidenced that endothelial growth factor in nonunion fractures can activate vascular repair processes [4]. Therefore, if in nonunion fracture vascularization persists, as well as the ability to promote vascular repair, it is conceivable that nonunion development may result from abnormal biochemical activity during bone repair.
Bone callus formation depends on osteoblastic new bone apposition and low osteoclastic resorption activity at the edge of the fractured bone. During the subsequent remodeling phase, osteoclasts are very active. A major paradigm of osteoclast biology has emerged with the discovery of the receptor activator nuclear factor kB (RANK), its ligand (RANKL), and osteoprotegerin (OPG), which are heavily involved in bone resorption, regulating osteoclast activity. RANK is a membrane receptor on osteoclasts and immune system cells, and binding with RANKL is necessary to promote differentiation, survival and activation of osteoclastic cells. OPG acts as a decoy receptor for RANKL and prevents RANK–RANKL binding. In contrast to RANKL and RANK, which are produced in small amounts and the expression of which is mainly restricted to the skeletal and immune system, OPG is produced in high concentrations by cells of the osteoblast lineage and by many different tissues and cell types, such as smooth muscle, endothelial and epithelial cells [5, 6]. It is known that OPG serum level increases with age [5], and that the RANK/RANKL/OPG system is involved in many diseases with bone mineral metabolism derangement, such as rheumatoid arthritis, Paget’s disease, osteopetrosis, and atherosclerosis [7, 8]
To our knowledge no data are available in the literature about the OPG/RANK/RANKL system and fracture nonunion of long bones. The aim of this study was to investigate the relation between the OPG/RANK/RANKL system and this type of fracture in a case–control model.
Materials and methods
Sixteen male patients with an atrophic nonunion shaft fracture, 20–39 years old, were included in the study (“nonunion”). No patient developed a local or systemic infection. The first control group (“healed”) consisted of 18 age-matched male subjects who healed from the same type of fracture and from whom blood samples were taken within six months after the healing of the fracture. The second control group (“healing”) consisted of 14 age-matched male subjects who healed from a shaft fracture, and from whom blood samples had been collected and stored during fracture healing within one month from the injury. The study conforms to the Declaration of Helsinki, was approved by the local ethics committee, and written informed consent was obtained from patients and controls.
Fractured patients undergoing treatment with drugs that interfere with bone metabolism, with local or systemic severe diseases, with previous same limb segment fractures, or with previous nonunion fractures were excluded.
A 12 h fasting blood sample was taken from each patient and control; a 12 h fasting urinary sample was also collected from each patient.
Osteocalcin (OC), bone alkaline phosphatase (BAP), OPG, free RANKL and urinary deoxypyridinoline (DPD) were measured in the patients. The same tests were performed in controls with the exception of urinary DPD. Free RANKL expresses as a soluble unbound fraction, which is free to interact with its receptors (RANK, OPG).
OPG was measured using the Human Osteoprotegerin ELISA kit (BioVendor Laboratory Medicine, Inc. Brno, Czech Republic, Labogen-srl). The intra-assay (within-run) coefficient of variation was 5% and the interassay (run-to-run) coefficient of variation was 4.7%. The limit of detection was better than 0.024 ng/ml of sample; specificity was less than 0.06%. For RANKL measurement, the Human Serum RANKL Free ELISA kit was used (Biomedica Medizinprodukte GmbH & Co. KG, Wien, Austria, Pantec), with an intra-assay coefficient of variation of 4% and an interassay coefficient of variation of 7.5%; the limit of detection was better than 0.08 pmol/l. To measure BAP, OC and DPD, the Metra ELISA kit (Quidel; San Diego, CA, USA) was used; here, the intra-assay and interassay coefficients of variation (CV) for each marker were, respectively, 4.96 and 5.93%, 7.83 and 6.96%, 6.06 and 4.16%.
Statistical analysis
Comparisons of the values for the three groups (nonunion patients, healed and healing controls) were performed by one-way ANOVA and Bonferroni multiple comparison tests, with the level of significance (P) being <0.05. Data are expressed as mean values and SDs.
Results
Table 1 shows the characteristics of both the patients and the controls, the distribution of the fracture site in each group, and the values of the serum bone markers. The only statistically significant difference was found for the OPG values of nonunion patients compared with both control groups (P < 0.001). The distributions and standard deviations of the OGP values in the three groups are shown in Fig. 1.
Table 1.
Characteristics of patients and controls, and results of bone markers measurements; values are shown as mean (SD)
| Characteristic | Nonunion | Healing controls | Healed controls |
|---|---|---|---|
| 16 | 14 | 18 | |
| Site of fractures | |||
| Tibia | 7 | 8 | 9 |
| Radius | 1 | 0 | 2 |
| Radius + ulna | 3 | 2 | 4 |
| Humerus | 2 | 2 | 1 |
| Femur | 3 | 2 | 2 |
| Age (years) | 28.1 (5.9) | 31.4 (7.1) | 32.2 (5.7) |
| Time after injury (months) | 6–11 | 0.5 (0.5) | 8.5 (3.4) |
| OPG (ng/ml) | 0.56 (0.11) | 0.29 (0.09)* | 0.26 (0.04)* |
| Free RANKL (pmol/l) | 0.08 (0.09) | 0.16 (0.07) | 0.10 (0.07) |
| BAP (UI/l) | 24.46 (5.99) | 31.56 (17.67) | 24.21 (7.13) |
| OC (ng/ml) | 7.27 (3.95) | 8.60 (4.47) | 8.45 (2.94) |
* P < 0.001 versus nonunion
Fig. 1.
OPG serum levels in nonunion patients and in healing and healed controls
The mean urinary DPD measured in the patients, normalized with respect to urinary creatinine, was 7.04 (SD 1.45) nmol DPD/mmol U-Cre, which is within the normal laboratory reference range (2.07–11.80 nmol DPD/mmol U-Cre).
No significant correlations were found between OC, BAP, DPD, OPG, free RANKL and the characteristics of the nonunion patients and the controls.
Discussion
In our patients with atrophic nonunion shaft fractures, the mean serum OPG level was significantly increased with respect to healed and healing controls, whereas the values of the other serum bone markers did not differ between the three cohorts.
The significantly higher serum OPG level in the patients may suggest an imbalance in the RANK/RANKL/OPG system, with osteoclast downregulation promoting a net apposition of new bone tissue. However, the patients’ radiographic images did not show callus bridges or calcification between or around the fracture stumps. Moreover, the osteoclast resorption activity marker, namely urinary DPD, was within the laboratory reference range for the normal population, not lower, suggesting that there was no inhibition of osteoclastic activity in atrophic nonunion fractures. This assessment was also confirmed by the fact that, in spite of the higher serum OPG, free RANKL levels in patient serum were comparable to those of all of the controls, whereas free RANKL would be expected to be lower for increased binding associated with the high serum OPG.
The osteoblast activity of the patients also appeared to be normal. Indeed, the markers of osteoblast viability and mineralization, BAP and OC respectively, were comparable in the three groups and within the normal range of laboratory values. In this bone metabolic situation, it would be questionable to ascribe the source of the high OPG to osteoblasts. It appears reasonable to suppose that there could be another unknown source of OPG, such as endothelial cells from the vessels surrounding the fracture.
Some studies have investigated some biochemical markers of bone metabolism in animals and patients, and have found that nonunion and normal fracture healing exhibit different behaviors [9, 10]. A study showed a relation between human fracture healing at the 16th week and a decline in serum osteocalcin (OC) and alkaline phosphatase (AP) [11]. Recently, another author found that measurements of OC, bone alkaline phosphatase (BAP) and deoxypyridinoline (DPD) could be useful for early diagnosis of nonunion fractures in rabbits [10].
A study showed that transforming growth factor β (TGFβ), platelet-derived growth factor, basic fibroblast growth factor, and bone morphogenetic protein 2/4 (BMP) were not significantly different in rabbits with nonunion with respect to rabbits with normal healed fractures [2]. A study found that the TGFβ supergene family and BMP can induce bone formation [12]. So far, it has not been demonstrated that a metabolic derangement could be the cause of the failed formation of bone callus in man. Interpreting our data, a persistent steady state situation of apparently normal bone metabolism leading to missed fracture healing seems to be a possible explanation for nonunion fractures.
Also, the high OPG serum levels in nonunion patients do not seem to be bound to the reparatory process, considering that OPG is not elevated in the healing controls; therefore, it may be an indicator of metabolic derangement of bone repair.
In our study, no correlations between any bone marker and the characteristics of the patients and controls were found. In the literature, a positive correlation between serum OPG levels and the ages of normal subjects was described [13], but it was not confirmed in our cohorts, probably due to the short population age range in this study.
The relatively small population in this study and the lack of measurements of bone reabsorption markers for the control groups may have limited the interpretation of possible bone metabolism differences between patients and controls.
Nevertheless, our observations may have a practical consequence. Even today, clinical and imaging evaluation is the cornerstone of the diagnosis of nonunion fractures, which is established only after six months post-injury; an earlier diagnosis is still not achievable. OPG measurement may provide a tool that facilitates the early identification of nonunion fractures, so a longitudinal study could be useful for checking this assumption.
Acknowledgments
Conflict of interest statement The authors declare that they have no conflict of interest related to the publication of this manuscript.
References
- 1.Brumback RJ, Ellison TS, Poka A et al (1992) Intramedullary nailing of femoral fractures. Part III: long-term effects of static interlocking fixation. J Bone Joint Surg 74A:106–112 [PubMed]
- 2.Brownlow HC, Reed A, Simpson AH (2001) Growth factor during the development of atrophic non-union. Injury 32(7):519–524 [DOI] [PubMed]
- 3.Reed A, Joyner CJ, Brownlow HC et al (2002) Human atrophic fracture non-unions are not avascular. J Orthop Res 20:593–599 [DOI] [PubMed]
- 4.Brownlow HC, Reed A, Simpson AH (2002) The vascularity of atrophic non-unions. Injury 33:145–150 [DOI] [PubMed]
- 5.Oh ES, Rhee E-J, Oh KW et al (2005) Circulating osteoprotegerin levels are associated with age, waist-to-hip ratio, serum total cholesterol, and low-density lipoprotein cholesterol levels in healthy Korean women. Metabolism 54:49–54 [DOI] [PubMed]
- 6.Hofbauer LC, Heufelder AE (2000) The role of receptor activator of nuclear factor-kB ligand and osteoprotegerin in the pathogenesis and treatment of metabolic bone diseases. J Clin Endocrinol Metab 85(7):2355–2363 [DOI] [PubMed]
- 7.Hofbauer LC, Schoppet M (2001) Serum measurement of osteoprotegerin—clinical relevance and potential applications. Eur J Endocrinol 145:681–683 [DOI] [PubMed]
- 8.Theoleyre S, Wittrant Y, Tat SK et al (2004) The molecular triad OPG/RANK/RANKL: involvement in the orchestration of pathophysiological bone remodelling. Cytokine Growth Factor Rev 15:457–475 [DOI] [PubMed]
- 9.Nyman MT, Paavolainen P, Forsius S et al (1991) Clinical evaluation of fracture healing by serum osteocalcin and alkaline phosphatase. Ann Chir Gynaecol 80(3):289–293 [PubMed]
- 10.Southwood LL, Frisbie DD, Kawcak CE et al (2003) Evaluation of serum biochemical markers of bone metabolism for early diagnosis of non-union and infected non-union fracture in rabbits. J Am Vet Med Assoc 64(6):727–735 [DOI] [PubMed]
- 11.Simonet WS, Lacey DL, Dunstan CR et al (1997) Osteoprotegerin: a novel secreted protein involved in the regulation of bone density. Cell 89:309–319 [DOI] [PubMed]
- 12.Ripamonti U (2006) Soluble osteogenic molecular signals and the induction of bone formation. Biomaterials 27:807–822 [DOI] [PubMed]
- 13.Szulc P, Hofbauer LC, Heufelder AE et al (2001) Osteoprotegerin serum levels in men: correlation with age, estrogen and testosterone status. J Clin Endocrinol Metab 86(7):3162–3165 [DOI] [PubMed]