Abstract
Introduction
The present study examined indoor air quality in a global sample of smoke-free and smoking-permitted Irish pubs. We hypothesized that levels of respirable suspended particles, an important marker of secondhand smoke, would be significantly lower in smoke-free Irish pubs than in pubs that allowed smoking.
Methods
Indoor air quality was assessed in 128 Irish pubs in 15 countries between 21 January 2004 and 10 March 2006. Air quality was evaluated using an aerosol monitor, which measures the level of fine particle (PM2.5) pollution in the air. A standard measurement protocol was used by data collectors across study sites.
Results
Overall, the level of air pollution inside smoke-free Irish pubs was 93% lower than the level found in pubs where smoking was permitted.
Discussion
Levels of indoor air pollution can be massively reduced by enacting and enforcing smoke-free policies.
Introduction
In recent years, many U.S. states and cities have passed laws prohibiting smoking in workplaces, including pubs and restaurants (American Nonsmokers’ Rights Foundation, 2007). Several countries also have enacted comprehensive indoor smoking bans, including Bhutan, Malta, Norway, Sweden, Italy, New Zealand, Uruguay, Scotland, Northern Ireland, and, most recently, England. In March 2004, the government of Ireland banned smoking in all work-sites, including public houses (pubs), making Ireland the first country to implement a nationwide policy. Given the smoking rates in Ireland and the association between smoking and visiting a pub, this was an historic event.
Secondhand smoke (SHS) exposure remains a major global public health concern, and it is entirely preventable (U.S. Department of Health and Human Services [USDHHS], 2000). SHS is a human carcinogen that contains at least 250 chemicals known to be toxic or carcinogenic (National Toxicology Program, 2000). Each year in the United States, SHS is responsible for an estimated 3,000 lung cancer deaths in never-smokers and more than 35,000 deaths from coronary heart disease in never-smokers. Further, SHS causes respiratory infections, asthma, sudden infant death syndrome, and other illnesses in children (Centers for Disease Control and Prevention, 2002; National Toxicology Program, 2000; USDHHS, 2000). SHS exposure in the workplace was responsible for more than 2,800 deaths in nonsmokers in 2002 across the 25 countries of the European Union (Smoke Free Partnership, 2006). The dangers of SHS exposure are highest among restaurant and bar workers, who typically receive little protection from smoking regulations (Eisner, Smith, & Blanc, 1998; Mulcahy & Repace, 2002; Siegel, 1993; Siegel & Skeer, 2003; Skeer & Siegel, 2003; USDHHS, 2000; U.S. Environmental Protection Agency [U.S. EPA], 1992).
SHS is a major source of respirable suspended particles (RSPs) or PM2.5 (i.e., particulate matter less than 2.5 microns in diameter). These fine particles are especially dangerous since they can easily be inhaled deep into the lungs and lead to a variety of adverse health effects, including cardiovascular disease, respiratory morbidity, and even death. To protect the public health, the U.S. EPA has set limits of 15 μg/m3, for the average annual level of PM2.5 exposure, and 35 μg/m3, for 24-hr exposure (U.S. EPA Technology Transfer Network, 2006). The 24-hr PM2.5 standard was lowered in 2006 (from 65 to 35 μg/m3) because mounting evidence established that short-term exposure to PM2.5 can result in numerous health effects, including increased mortality (U.S. EPA Technology Transfer Network, 2006). Studies in the United States have evaluated the impact of smoke-free air legislation by measuring the difference in RSP levels between smoke-free venues and those that permit smoking (Hyland, Travers, & Repace, 2004; Ott, Switzer, & Robinson, 1996; Repace, 2004; Travers et al., 2004).
In the Republic of Ireland, an air quality assessment conducted in Irish pubs showed a dramatic reduction in the presence of RSPs (PM10 and PM2.5) shortly after implementation of the smoke-free law, with no apparent adverse effects on business (Mulcahy, Byrne, & Ruprecht, 2005; Office of Tobacco Control, 2005). Despite claims that the law would not be adhered to and that it would have a negative impact on pub business, these claims have not been realized. Fong et al. (2006) reported high compliance with the Irish law.
Irish pubs can be found in nearly every city in the world. Some are smoke-free, while others remain smoke-filled. Given the smoke-free legislation in the Republic of Ireland, a study of air pollution in Irish pubs globally provides an opportunity to assess the effectiveness of comprehensive smoke-free laws and policies. The present study examined indoor air quality in a global sample of smoke-free and smoking-permitted Irish pubs. We hypothesized that RSP levels, an important marker of SHS, would be significantly lower in smoke-free Irish pubs than in pubs that allowed smoking.
Methods
Testing sites
Between 21 January 2004 and 10 March 2006, air quality was assessed in 128 Irish pubs in 15 countries. The pubs were located in the Republic of Ireland, the United States, Canada, Australia, Northern Ireland, France, Lebanon, Belgium, Poland, Greece, Germany, China, England, Romania, and Armenia. Testing sites were selected by tobacco control professionals in their respective cities (i.e., a convenience sample). Irish pubs were defined as those that served Irish beer on tap and had an Irish name (e.g., Murphy’s, O’Donnell’s) or a visible statement that the venue was an Irish pub (e.g., exterior or interior sign with terms such as “Irish pub”). Testing was completed in smoking-permitted and smoke-free pubs on all the days of the week from afternoon onward. Some pubs were individually owned establishments, and some were part of local or national chains.
The smoke-free Irish pubs were located in three cities and one town in the Republic of Ireland (Cork, Dublin, Ennis, and Galway), in two cities in Canada (Toronto and Waterloo), and in nine U.S. cities (Appleton, WI; Austin, TX; Bethesda, MD; Bloomington, IN; Boston, MA; Buffalo, NY; Hartford, CT; Providence, RI; and New York City). Smoking-permitted pubs were located in 13 countries and 38 cities, including Armenia (Yerevan), Australia (Sydney), Northern Ireland (Belfast and Newry), Germany (Berlin), Greece (Athens), Lebanon (Beirut), France (Lyon and Paris), Belgium (Brussels, Charleroi, and Liege), Poland (Torun and Warsaw), China (Beijing), Romania (Bucharest), the United States (Arlington, VA; Atlanta, GA; Baltimore, MD; Chapel Hill, NC; Charleston, SC; Chicago, IL; Denver, CO; Durham, NC; Galveston, TX; Hoboken, NJ; Houston, TX; Indianapolis, IN; Lakewood, OH; Louisville, KY; Manchester, NH; Santa Fe, NM; St. Paul, MN; Philadelphia, PA; Phoenix, AZ; and Washington, DC), and England (London and Manchester).
The average size of the pubs was 961 m3 (n = 124) with the smoke-free pubs being on average smaller than smoking-permitted pubs (724 vs. 1,069 m3). The average number of patrons present during sampling was 59 (n = 126) and consistent with their smaller size, the smoke-free pubs had fewer people on average than the smoking-permitted pubs 51 vs. 65.
Measurement protocol
A standard measurement protocol was used by data collectors across study sites. In each establishment, RSPs were measured using a TSI SIDEPAK AM510 Personal Aerosol Monitor (TSI, Inc., St. Paul, MN), an aerosol monitor fitted with a 2.5-μm impactor so that it could measure the concentration of particulate matter with a mass median aerodynamic diameter of less than or equal to 2.5 μm or PM2.5. The SIDEPAK was used with a calibration factor setting of 0.32. This factor was determined by calibrating the SIDEPAK with another laser photometer that had been calibrated for SHS and used in previous studies (Repace, 2004). Light scattering photometer devices have proven to be effective air monitoring devices in similar studies (Repace, 2004).
The equipment was set to a 1-min log interval, which averages the previous 60 1-s measurements. Sampling was discreet so that the occupants’ normal behavior would not be disrupted. For each pub, the first and last minute of logged data were removed because they are averaged with outdoors and entryway air. The remaining datapoints were averaged to provide an average PM2.5 concentration within the venue.
Establishments were tested for a minimum of 30 min. The number of people inside the venue and the number of burning cigarettes were recorded upon entry into the venue and every 15 min during sampling until the venue was exited. Thus, at least three observations were averaged over the time inside the venue to determine the average number of people on the premises and the average number of burning cigarettes. For most establishments, a sonic measure (Zircon Corporation, Campbell, CA) was used to measure room dimensions and, hence, the volume of each of the venues. Room dimensions were estimated when the sonic measure could not be used.
Data analyses
We used the Mann–Whitney U test to assess the difference in average PM2.5 levels in a cross-sectional sample of smoke-free and smoking-permitted Irish pubs. Descriptive statistics including venue volume, number of patrons, and average smoker density (i.e., number of burning cigarettes per 100 m3) also are reported for each pub and averaged for all pubs. The active smoker density was calculated by dividing the average number of burning cigarettes by the volume of the room in cubic meters. For smoking-permitted pubs, the bivariate association between active smoker density and PM2.5 level was assessed using a Pearson's correlation.
Results
The average PM2.5 level in the 41 smoke-free pubs was 23 μg/m3 (SD = 18.0; range = 3–96 μg/m3). The average PM2.5 level in the 87 smoking pubs was 329 μg/m3 (SD = 269.7; range = 33–1,320 μg/m3) (Table 1). Although some overlap in measured exposure was found between smoking-permitted pubs and smoke-free pubs, the average level in all the smoking-permitted pubs was more than 14 times higher than in smoke-free pubs. The level of indoor air pollution was 93% lower in the smoke-free pubs than in those where smoking was permitted. The difference in indoor air quality between smoking-permitted and smoke-free pubs was statistically significant according to the Mann–Whitney U test (p < .001).
Table 1.
Summary of smoke-free and smoking-permitted pubs by country
| Country | State/region | City | Policy | Sample size | Mean PM2.5 level (μg/m3) |
| U.S. smoke-free pubs | 8 | 9 | 14 | 14 | |
| Connecticut | Hartford | Yes | 2 | 18 | |
| Indiana | Bloomington | Yes | 1 | 10 | |
| Maryland | Bethesda | Yes | 1 | 8 | |
| Massachusetts | Boston | Yes | 2 | 13 | |
| New York | Buffalo | Yes | 2 | 15 | |
| New York City | Yes | 2 | 17 | ||
| Rhode Island | Providence | Yes | 1 | 3 | |
| Texas | Austin | Yes | 1 | 22 | |
| Wisconsin | Appleton | Yes | 2 | 17 | |
| U.S. smoking pubs | 18 | 20 | 48 | 263 | |
| Arizona | Phoenix | No | 3 | 142 | |
| Colorado | Denver | No | 4 | 90 | |
| Georgia | Atlanta | No | 2 | 267 | |
| Illinois | Chicago | No | 2 | 235 | |
| Indiana | Indianapolis | No | 3 | 337 | |
| Kentucky | Louisville | No | 5 | 284 | |
| Maryland | Baltimore | No | 1 | 87 | |
| Minnesota | St. Paul | No | 4 | 276 | |
| New Hampshire | Manchester | No | 3 | 394 | |
| New Jersey | Hoboken | No | 2 | 709 | |
| New Mexico | Santa Fe | No | 1 | 57 | |
| North Carolina | Raleigh–Durham–Chapel Hill | No | 2 | 170 | |
| Ohio | Lakewood | No | 3 | 425 | |
| Pennsylvania | Philadelphia | No | 2 | 293 | |
| South Carolina | Charleston | No | 3 | 236 | |
| Texas | Galveston | No | 2 | 363 | |
| Houston | No | 1 | 125 | ||
| Virginia | Arlington | No | 3 | 145 | |
| Washington, DC | Washington, DC | No | 2 | 184 | |
| Ireland | 4 | 25 | 29 | ||
| Dublin | Yes | 7 | 30 | ||
| Cork | Yes | 6 | 32 | ||
| Ennis | Yes | 4 | 32 | ||
| Galway | Yes | 8 | 23 | ||
| Canada | 2 | 2 | 12 | ||
| Ontario | Toronto | Yes | 1 | 19 | |
| Waterloo | Yes | 1 | 4 | ||
| Other nations | 18 | 39 | 411 | ||
| Armenia | Yerevan | No | 1 | 498 | |
| Australia | New South Wales | Sydney | No | 4 | 132 |
| Belgium | Brussels | No | 1 | 273 | |
| Charleroi | No | 1 | 876 | ||
| Liege | No | 2 | 423 | ||
| China | Beijing | No | 1 | 145 | |
| England | London | No | 3 | 296 | |
| Manchester | No | 3 | 415 | ||
| France | Paris | No | 2 | 363 | |
| Lyon | No | 1 | 1,051 | ||
| Germany | Berlin | No | 1 | 278 | |
| Greece | Athens | No | 1 | 748 | |
| Lebanon | Beirut | No | 2 | 730 | |
| Northern Ireland | Belfast | No | 7 | 353 | |
| Newry | No | 6 | 400 | ||
| Poland | Torun | No | 1 | 695 | |
| Warsaw | No | 1 | 272 | ||
| Bucharest | No | 1 | 623 | ||
| Romania |
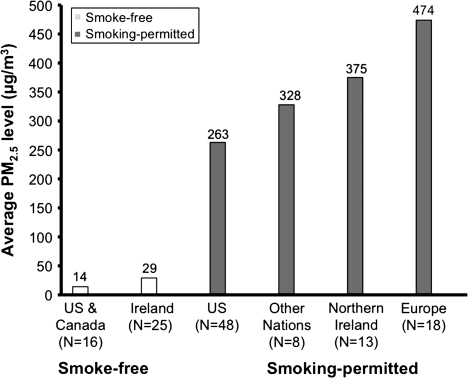
Figure 1 shows the average air pollution levels found in Irish pubs across world regions. The average PM2.5 levels in smoke-free Irish pubs in the United States and Canada (14 μg/m3) and the Republic of Ireland (29 μg/m3) were significantly lower than levels in smoking-permitted pubs in the United States (263 μg/m3), other nations (China, Australia, Armenia, and Lebanon; 328 μg/m3), Northern Ireland (375 μg/m3), and Europe (474 μg/m3).
Figure 1.
Average level of indoor air pollution in Irish pubs by world region.
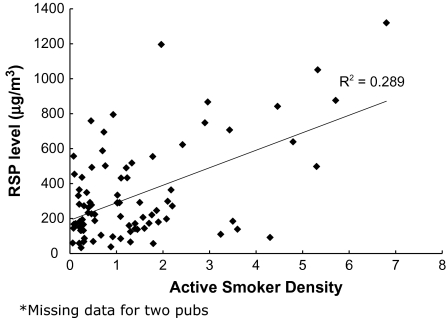
The average smoker density in the smoking permitted pubs (n = 85) was 1.40 burning cigarettes/100 m3. No smoking was observed in any of the pubs with smoke-free policies. As shown in Figure 2, average PM2.5 levels were significantly positively correlated (r = .538, p < .01, R2 = .289) with smoker density.
Figure 2.
RSP level versus smoker density for smoking pubs.
Discussion
Levels of indoor air pollution can be massively reduced by enacting and enforcing smoke-free policies. Indoor air quality testing revealed that, on average, PM2.5 levels in smoke-free Irish pubs were 93% lower than in smoking-permitted Irish pubs (23 vs. 340 μg/m3). The absence of smokers in the Irish pubs tested also indicates that workplace owners and patrons are complying with these laws.
Some study limitations need to be noted. First, because the sample of pubs tested was a convenience sample, we cannot specifically make inferences to all Irish pubs, although our findings are consistent with other studies that have examined changes in indoor air quality to evaluate the impact of smoking restriction legislation (Hyland et al., 2004; Mulcahy, Evans, Hammond, Repace, & Byrne, 2005; Mulcahy, Byrne, & Ruprecht, 2005; Repace, 2004; Travers et al., 2004). Second, SHS is not the only source of indoor PM2.5. Other sources, such as ambient particle concentrations, cooking, and migration of particles from outside, also could contribute to overall levels of indoor air pollution. We would expect, however, that these other sources of air pollution would likely be present in both smoke-free and smoking-permitted pubs; thus, the differences in average PM2.5 found are most likely attributable to SHS. Third, testing did not control for ventilation or for smoke that might have migrated from outdoors, where smokers tend to smoke when complying with smoking bans (Mulcahy, Evans, et al., 2005). However, previous research has shown that the ventilation effect is likely to be small and unlikely to account for the large differences observed in smoke-free and smoking-permitted pubs (Repace, 2004).
Despite these limitations, the present study provides evidence that the most effective method for reducing SHS exposure in public places is implementation of policies requiring smoke-free environments (Hopkins et al., 2001). The World Health Organization (WHO) (2006) Framework Convention on Tobacco Control calls on governments to “protect all persons from exposure to tobacco smoke,” rather than just specific populations such as children or pregnant women (Guiding Principle 4.1). This protection should be extended, according to Article 8.2, “in indoor workplaces, public transport, indoor public places and … other public places” (WHO, 2006). Since the Republic of Ireland banned indoor smoking in all public spaces, including restaurants and pubs, many countries and U.S. states have implemented policies for smoke-free workplaces, including restaurants and pubs.
Reducing the level of indoor air pollution from SHS should translate into improved health for both workers and patrons. One study found improvements in respiratory health among bartenders after implementation of a statewide smoking ban (Eisner et al., 1998), and another study reported reductions in acute myocardial infarctions in patients admitted to a hospital after implementation of a local smoking ban (Sargent, Shepard, & Glantz, 2004). An examination of SHS exposure among workers following Ireland's comprehensive ban showed significant reductions in air nicotine and salivary cotinine (Mulcahy, Evans, et al., 2005). Respiratory health studies in Ireland have shown results similar to those found in California as well as dramatic reductions in exhaled carbon monoxide and ambient benzene levels after the smoking ban (Goodman, Agnew, McCaffrey, Paul, & Clancy, 2007). According to Repace, Al-Delaimy, and Bernert (2006), RSPs are correlated with biological markers for exposure (e.g., nicotine and cotinine) that can be used to predict adverse health outcomes. These results further confirm that these laws, when implemented properly, will reduce SHS exposure and can provide health benefits worldwide.
Funding
Flight Attendant Medical Research Institute and the U.S. National Cancer Institute (TTURC-P50 CA111236); Health Service Executive-West, Primary Community Continuing Care, Galway, and RIFTFS Dublin, Republic of Ireland.
Declaration of Interests
None declared.
Supplementary Material
Acknowledgments
The authors thank Carolyn Dresler, of the International Agency for Research on Cancer, who organized and coordinated air monitoring data collection in many countries internally with the collaboration of investigators at Roswell Park Cancer Institute. The authors also acknowledge the following individuals for their contributions: Adrian Watson, Christian Hassleholdt, Amy Barkley, Cheryl Ferguson, Cheryl Higbee, Chris Tholkes, Barbara Schillo, Cindy L. Carter, Connie Olson, Dan Carrigan, Geoffrey T. Fong, Taryn Sendzik, Matthew Sendzik, Heather Giles, Ioana Munteanu, Florin Mihaltan, Isabelle Convié, Jennifer Witten, Jiang Yuan, Kang Ji Ming, Li Zhu, Jon Macy, Julea Steiner, Julia Valdez, Justin Turner, Krzysztof Przewozniak, Jakub Gumkowski, Witold Zatonski, Martina Pötschke-Langer, Susanne Schunk, Bjoern Seibold, Elmar Jentsch, Matthew J. Carpenter, Meg Gallogly, Ben Needham, Erika Schlachter, Danny McGoldrick, Mike Kuntz, Miranda Spitznagle, Missy Lewis, Shelley O’Connell, Patrice Adams, Tim Filler, Nan Savage, Frances Gannon, Richard Fitzgerald, Tony Christie, Catherine Dunne, Marie McCaffrey, Narine Movsisyan, Natalie Linos, Stephanie Meredith Chace, Stephanie Weiss, Paul Mowery, Philip Huang, Eric Miller, Rhea Staniszewski, Robyn Wiesman, Shawn Boogaard, Stephannie Thacker, Stephanie Uliana, Paul Kiser, Steve Houston, Sylviane Ratte, Christelle Nieraad, and Wendy Oakes.
References
- American Nonsmokers’ Rights Foundation. Smoke-free lists and maps. 2007. Retrieved July 19, 2007, from http://www.no-smoke.org/pdf/percentstatepops.pdf. [Google Scholar]
- Centers for Disease Control and Prevention. Annual smoking-attributable mortality, years of potential life lost, and economic costs—United States, 1995–1999. MMWR Morbidity and Mortality Weekly Report. 2002;51:300–320. [PubMed] [Google Scholar]
- Eisner MD, Smith AK, Blanc PD. Bartenders’ respiratory health after establishment of smoke-free bars and taverns. The Journal of the American Medical Association. 1998;280:1909–1914. doi: 10.1001/jama.280.22.1909. [DOI] [PubMed] [Google Scholar]
- Fong GT, Hyland A, Borland R, Hammond D, Hastings G, McNeill A, et al. Changes in exposure to tobacco smoke pollution and support for smoke-free public places following the implementation of comprehensive smoke-free workplace legislation in the Republic of Ireland: Findings from the ITC Ireland/UK Survey. Tobacco Control. 2006;15(Suppl. 3):iii51–iii58. doi: 10.1136/tc.2005.013649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goodman P, Agnew M, McCaffrey M, Paul G, Clancy L. Effects of the Irish smoking ban on respiratory health of bar workers and air quality in Dublin pubs. 2007. Retrieved July 19, 2007, from http://www.tri.ie/ [DOI] [PubMed] [Google Scholar]
- Hopkins DP, Briss PA, Ricard CJ, Husten CG, Carande-Kulis VG, Fielding JE, et al. Reviews of evidence regarding interventions to reduce tobacco use and exposure to environmental tobacco smoke. American Journal of Preventive Medicine. 2001;20(Suppl. 2):16–66. doi: 10.1016/s0749-3797(00)00297-x. [DOI] [PubMed] [Google Scholar]
- Hyland A, Travers MJ, Repace JL. 7 City Air Monitoring Study, March–April 2004. 2004, May. Retrieved July 16, 2007, from http://tobaccofreekids.org/pressoffice/7camreport.pdf. [Google Scholar]
- Mulcahy M, Repace J. Proceeedings of Indoor Air 2002, the Ninth International Conference on Indoor Air Quality and Climate. Volume II. Monterey, California: 2002. Passive smoking exposure and risk for Irish bar staff; pp. 144–149. [Google Scholar]
- Mulcahy M, Byrne MA, Ruprecht A. How does the Irish smoking ban measure up? A before and after study of particle concentrations in Irish pubs. Indoor Air. 2005;15(Suppl. 11):86. [Google Scholar]
- Mulcahy M, Evans DS, Hammond SK, Repace JL, Byrne M. Secondhand smoke exposure and risk following the Irish smoking ban: An assessment of salivary cotinine concentrations in hotel workers and air nicotine levels in bars. Tobacco Control. 2005;14:384–388. doi: 10.1136/tc.2005.011635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Toxicology Program. Ninth Report on Carcinogens 2000. Research Triangle Park, NC: U.S. Department of Health and Human Services, National Institute of Environmental Health Sciences; 2000. [Google Scholar]
- Office of Tobacco Control. Smoke-free workplaces in Ireland: A one-year review. Dublin, Ireland: Office of Tobacco Control; 2005. [Google Scholar]
- Ott W, Switzer P, Robinson J. Particle concentrations inside a tavern before and after prohibition of smoking: Evaluating the performance of an indoor air quality model. Journal of the Air & Waste Management Association. 1996;46:1120–1134. doi: 10.1080/10473289.1996.10467548. [DOI] [PubMed] [Google Scholar]
- Repace J. Respirable particles and carcinogens in the air of Delaware hospitality venues before and after a smoking ban. Journal of Occupational and Environmental Medicine. 2004;46:887–905. doi: 10.1097/01.jom.0000141644.69355.52. [DOI] [PubMed] [Google Scholar]
- Repace J, Al-Delaimy WK, Bernert JT. Correlating atmospheric and biological markers in studies of secondhand tobacco smoke exposure and dose in children and adults. Journal of Occupational and Environmental Medicine. 2006;48:181–194. doi: 10.1097/01.jom.0000184883.72902.d4. [DOI] [PubMed] [Google Scholar]
- Sargent RP, Shepard RM, Glantz SA. Reduced incidence of admissions for myocardial infarction associated with public smoking ban: Before and after study. British Medical Journal. 2004;328:977–980. doi: 10.1136/bmj.38055.715683.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Siegel M. Involuntary smoking in the restaurant workplace: A review of employee exposure and health effects. The Journal of the American Medical Association. 1993;270:490–493. [PubMed] [Google Scholar]
- Siegel M, Skeer M. Exposure to secondhand smoke and excess lung cancer mortality risk among workers in the 5 B's bars, bowling alleys, billiard halls, betting establishments and bingo parlours. Tobacco Control. 2003;12:333–338. doi: 10.1136/tc.12.3.333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skeer M, Siegel M. The descriptive epidemiology of local restaurant smoking regulations in Massachusetts: An analysis of the protection of restaurant customers and workers. Tobacco Control. 2003;12:221–226. doi: 10.1136/tc.12.2.221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smoke Free Partnership. Lifting the smokescreen. 10 reasons for a smoke free Europe. 2006, February. Retrieved July 19, 2007, from http://www.ersnet.org/ers/show/default.aspx?id_attach=13509. [Google Scholar]
- Travers MJ, Cummings MJ, Hyland A, Repace J, Babb S, Pechacek T, et al. Indoor air quality in hospitality venues before and after implementation of a clean indoor air law—Western New York. MMWR Morbidity and Mortality Weekly Report. 2004;53:1038–1041. [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services. Reducing tobacco use: A report of the Surgeon General. Washington, DC: U.S. Government Printing Office; 2000. [Google Scholar]
- U.S. Environmental Protection Agency. Respiratory health effects of passive smoking: Lung cancer and other disorders. Washington, DC: U.S. Environmental Protection Agency, Office of Research and Development, Office of Air and Radiation; 1992. [Google Scholar]
- U.S. Environmental Protection Agency Technology Transfer Network. National ambient air quality standards (NAAQS). Area designations for 2006 24-hour PM2.5 NAAQS—Technical information. 2006. Retrieved June 19, 2008, from http://www.epa.gov/ttn/naaqs/pm/pm25_2006_techinfo.html#A. [Google Scholar]
- World Health Organization. Framework Convention Alliance for Tobacco Control. 2006. Retrieved July 19, 2007, from http://www.who.int/tobacco/framework/WHO_FCTC_english.pdf. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.