Abstract
Introduction
This study replicated prior observations of racial differences in smoking cessation in which Black smokers have demonstrated lower smoking cessation rates than White smokers.
Methods
The study used data from a smoking cessation intervention and compared White and Black female prisoners (N = 233) on a 10-week intervention of group psychotherapy and nicotine replacement (patch). Generalized estimating equations were used to model smoking cessation across the 12-month follow-up.
Results
Compared with an untreated control group, both Black and White smokers benefited from the cessation treatment. However, after controlling for potential confounds, White smokers had significantly higher overall smoking cessation rates across time compared with Black smokers (e.g., 30% vs. 24% abstinent at 6 weeks; 13% vs. 10% abstinent at 12 months). Smoking mentholated cigarettes was not associated with these differences in quit rates.
Discussion
Understanding differential treatment responses can lead to the development of more tailored and efficacious smoking cessation interventions that may reduce the morbidity and mortality associated with smoking in prison populations.
Introduction
Smoking is the leading cause of preventable death in the United States, and about one in five adults is a current cigarette smoker (Centers for Disease Control and Prevention [CDC], 2007). Historically, Whites were more likely to smoke cigarettes than Blacks; however, in recent years, the prevalence rates between the groups has narrowed, with Whites (21.9%) now smoking at slightly lower prevalence rates than Blacks (23%; CDC, 2007). The number of current smokers is a dynamic composite of initiation and quit rates. One factor that may contribute to higher smoking rates among Blacks is that Black smokers appear to have lower smoking cessation success rates compared with White smokers (Covey et al., 2008; U.S. Department of Health and Human Services [USDHHS], 1998).
Differences between Whites and Blacks on other kinds of smoking behavior have been noted, and these may account in part for differences in cessation success. For example, Black smokers are more likely to smoke mentholated cigarettes (Foulds, Gandhi, et al., 2006; Muscat, Richie, & Stellman, 2002; USDHHS, 1998), smoke fewer cigarettes (Foulds, Gandhi, et al., 2006; Muscat et al., 2002), and take fewer puffs per cigarette (Clark, Gautam, & Gerson, 1996; Jarvik, Tashkin, Caskey, McCarthy, & Rosenblatt, 1994; McCarthy et al., 1995) but have higher carbon monoxide (CO) levels (Ahijevych & Parsley, 1999; Ahijevych, Weed, & Clark, 2004; Clark et al., 1996; Melikian et al., 2007). This pattern suggests that the puffs taken are larger and that the cigarettes are smoked more intensively.
Mentholated cigarettes have been suggested as a possible agent in poor cessation rates by allowing smokers to inhale cigarette smoke more deeply into the lungs and increase exposure to nicotine and other chemicals (Foulds, Williams, & Gandhi, 2006). However, findings are mixed. Muscat et al. (2002) investigated spontaneous quit rates in a large cross-sectional study of Black and White smokers and did not find any differences between quit rates, even when accounting for smoking mentholated cigarettes. Similar results were found in the Community Intervention Trial for Smoking Cessation; mentholated smoking was not associated with cessation rates (Hyland, Garten, Giovino, & Cummings, 2002). Okuyemi et al. (2003) found that mentholated smoking was associated with difficulty with early cessation (6 weeks) but not with long-term quitting (6 month) in Black smokers. Fu et al. (2008) found no racial differences or impact of smoking mentholated cigarettes in smoking cessation among older veterans.
Prisoners are a special population with a high prevalence of smoking. Approximately 70%–80% of prisoners have been identified as current smokers (Belcher, Butler, Richmond, Wodak, & Wilhelm, 2006; Colsher, Wallace, Loeffelholz, & Sales, 1992; Conklin, Lincoln, & Tuthill, 2000; Cropsey, Eldridge, & Ladner, 2004; Cropsey, Eldridge, Weaver, Villalobos, & Stitzer, 2006; Cropsey & Kristeller, 2003, 2005; Sieminska, Jassem, & Konopa, 2006). Consistent with previous population data, one study with female prisoners found prevalence rates of smoking to be higher for Whites than Blacks (79.5% vs. 71.3%; Cropsey et al., 2004) and found that Black female prisoners smoked fewer cigarettes per day than did White prisoners (11.1% vs. 19.2%; Cropsey et al., 2006).
Cropsey et al. (2008) recently conducted a randomized controlled trial of a smoking cessation intervention (10-week group therapy combined with nicotine replacement) with female prisoners. Although participants who dropped out during treatment were significantly more likely to be single and to initiate smoking at a younger age compared with treatment completers, overall study results demonstrated that female prisoners can successfully quit smoking when offered access to standard treatment for smoking cessation (Cropsey et al., 2008). Data from this study provided an opportunity to determine if racial differences existed in response to the smoking cessation intervention among the sample of female prisoners and also to determine whether use of mentholated cigarettes was a factor in any racial differences identified. We expected that Blacks would have lower smoking cessation rates compared with White smokers and that smoking mentholated cigarettes would not be related to lower cessation rates.
Methods
Participants
Demographic characteristics were compared between racial groups (Table 1). Overall, White participants were older, had higher levels of educational attainment, and reported a higher rate of lifetime mental health treatment compared with Black participants.
Table 1.
Demographic characteristics (N = 233)
| Variable |
White (n = 109) | Black (n = 124) | Chi-square or F test | p value | |
| Age (years) | M | 35.3 | 32.7 | 4.7 | .03 |
| SD | 9.6 | 8.3 | |||
| Marital status | Married | 16.5% | 13.7% | 0.6 | .59 |
| Other | 83.5% | 86.3% | |||
| Education level | <HS | 17.4% | 37.9% | 12.0 | .002 |
| HS/GED | 46.8% | 34.7% | |||
| >HS | 35.8% | 27.4% | |||
| Received mental health treatment | Yes | 78.7% | 56.1% | 13.2 | .001 |
| No | 21.3% | 43.9% | |||
| Received substance abuse treatment | Yes | 57.8% | 60.2% | 0.7 | .79 |
| No | 42.2% | 39.8% | |||
Note. HS, high school; GED, General Educational Development.
The study used the following inclusion criteria: females aged 18 years or older, smoking at least 5 cigarettes/day, maintained in general population (e.g., not held in segregation), and desiring smoking cessation treatment. Exclusion criteria included severe, acute mental illness (e.g., current suicidal ideation/intent, actively psychotic), or mental retardation such that they could not provide informed consent or participate in group therapy, known allergy to nicotine replacement patches, less than 1 year to serve on their sentence, or not English speaking. Participants with other disabilities such as nonreaders or legally blind participants were admitted into the study and were assisted in completing their survey instruments.
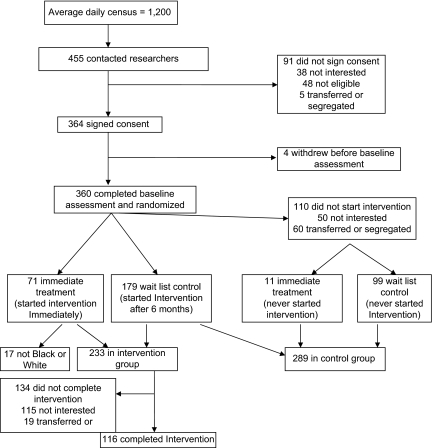
A total of 364 participants signed informed consent, 360 participants completed the baseline assessment, and 250 participants started the intervention either immediately after the baseline assessment (n = 71) or after a 6-month wait-list period (n = 179). Since we were interested in comparing White to Black women, 17 participants were excluded because they did not fall into one of these racial groups, leaving a final sample of 233 who entered the intervention and were included in this analysis (Figure 1). A total of 289 participants comprised the control sample, with 179 of these participants crossing over to the active intervention after 6 months (see Figure 1).
Figure 1.
Study flowchart.
Procedures
Study procedures have been described previously (Cropsey et al., 2008). Briefly, all participants were recruited though announcements and study fliers in prison housing units from June 2004 through June 2006. They were followed through 12 months at a medium–maximum security female prison. This study received institutional review board approval from Virginia Commonwealth University, the Virginia Department of Corrections, and the University of Alabama at Birmingham. A certificate of confidentiality was obtained by the federal government to further protect confidentiality of research data.
The original study was a randomized controlled trial using a wait-list control group (6-month wait-list). Participants completed a baseline assessment of smoking history and demographic information. After entering the group intervention, weekly measures of daily smoking, concentration of expired CO (Vitalograph BreathCO), type of cigarette smoked, and height and weight were collected. An expired-CO reading of 3 ppm or higher was used to indicate current smoking, which was the optimal cutoff indicated in a previous investigation with smoking and nonsmoking female prisoners (Cropsey et al., 2006).
Intervention description
The behavioral intervention used for this study was Mood Management Training to Prevent Smoking Relapse (Hall, Muñoz, & Reus, 1994). This intervention was chosen because it focused on mood management skills, as well as standard behavioral interventions for smoking cessation. This 10-session group intervention was modified for the unique environment encountered by female prisoners and included examples of smoking triggers encountered in prison and acceptable coping strategies that could be used in the prison environment. A full description of how this intervention was modified was reported previously (Cropsey et al., in press).
In addition to the group intervention, all participants received NicoDerm CQ patches following the manufacturer's suggested dosing regimen. Participants started nicotine replacement and were asked to make a quit attempt between weeks 3 and 4 of the intervention. Participants completed assessments at end of treatment (EOT) and at 3-, 6-, and 12-month follow-ups. Participants who started on 21-mg nicotine patches had an additional medication check-in the week after the EOT assessment to refill medication and assess for side effects. All study outcomes through the 12-month follow-up are presented here.
Data analyses
Comparison of baseline characteristics between White and Black participants was done using chi-square and analysis of variance procedures where appropriate. The outcome variable, smoking abstinence, was obtained by asking participants if they smoked in the past 7 days and was confirmed by expired CO, with participants coded as abstinent if they denied any smoking in the past week and had a CO level of 2 ppm or less. Each timepoint abstinence was based on 7-day abstinence.
We used a generalized estimating equation (GEE) method to examine the long-term impact of the intervention on smoking rates among racial groups. GEE is a robust procedure used with longitudinal, dichotomous outcomes data to provide the best estimation of the relationships of the variables of interest across time. In this analysis, the model included treatment (group/nicotine replacement vs. wait-list control), race (White vs. Black), time (15 timepoints: baseline; weeks 1–10 of group treatment; a medication check 1 week after group termination; and 3-, 6-, and 12-month follow-ups), treatment by time interaction, and treatment by race interaction terms. The outcome variable of interest was 7-day smoking cessation at each timepoint (smoking vs. quit). Participants who dropped out of the intervention were coded as smoking, whereas participants who were transferred to another facility or released after the intervention ended had their last value (e.g., quit or smoking) carried forward for subsequent follow-up points. All other missing data (e.g., return to court, segregation) during follow-up were coded as smoking.
For this sample, we used a GEE model with the following explanatory variables: treatment (wait-list control = 0, group/nicotine replacement = 1), race (Black = 0, White = 1), and time (more than 15 timepoints). We also were interested in the effect of treatment over time and how treatment effects varied by race. Age, education, average number of cigarettes per day, change in smoking behavior since coming to prison, and prior mental health treatment were added as covariates. As a secondary analysis, we examined the impact of smoking mentholated cigarettes on treatment outcomes and controlled for baseline age, education, average number of cigarettes per day, change in smoking behavior since coming to prison, and prior mental health treatment and differences between White and Black smokers. Thus, the second model only examined individuals who received treatment (N = 233). Both models were fit with an exchangeable working correlation. A p value less than .05 was used for all analyses to indicate significance.
Results
Racial differences on smoking history and behavior
Table 2 compares baseline smoking characteristics across racial groups. Compared with Black smokers, White smokers were younger when they initiated smoking and when they began daily smoking and therefore had smoked for a greater number of years. Whites smoked more cigarettes per day, had a higher maximum lifetime number of cigarettes smoked, and had higher expired-CO levels. No differences were found between White and Black smokers on time since last cigarette, number of past quit attempts, longest period of time quit, last time they made a quit attempt, difficulty of their last quit attempt, or likelihood that they would continue to smoke after their release from prison.
Table 2.
Baseline smoking characteristics (N = 233)
| Variable |
White (n = 109) | Black (n = 124) | F test | p value | |
| Age first tried smoking | M | 12.8 | 14.4 | 6.1 | .014 |
| SD | 4.8 | 4.7 | |||
| Age at daily smoking | M | 15.4 | 16.7 | 3.8 | .05 |
| SD | 5.2 | 4.5 | |||
| Average cigarettes per day | M | 19.8 | 13.6 | 32.0 | <.001 |
| SD | 7.2 | 8.9 | |||
| Highest cigarettes per day | M | 31.7 | 17.4 | 39.6 | <.001 |
| SD | 19.4 | 12.0 | |||
| Number smoked today | M | 7.4 | 5.2 | 11.6 | .001 |
| SD | 4.8 | 5.1 | |||
| Number smoked yesterday | M | 17.7 | 11.9 | 29.2 | <.001 |
| SD | 7.4 | 8.7 | |||
| Time since last cigarette (min) | M | 46.7 | 46.9 | 2.7 | .10 |
| SD | 65.5 | 108.2 | |||
| Carbon monoxide level | M | 16.2 | 12.9 | 8.4 | .004 |
| SD | 8.9 | 7.7 | |||
| Total number of years smoking | M | 20.6 | 16.9 | 8.9 | .003 |
| SD | 9.8 | 8.9 | |||
| Number of past quit attempts | M | 2.6 | 2.1 | 0.9 | .35 |
| SD | 3.0 | 2.4 | |||
| Longest quit (months) | M | 14.6 | 11.4 | 0.8 | .37 |
| SD | 19.3 | 13.2 | |||
| Last time quit (months) | M | 35.4 | 22.4 | 1.2 | .27 |
| SD | 67.7 | 30.1 | |||
| Difficulty of last quit attempt | M | 5.5 | 5.0 | 2.9 | .09 |
| SD | 2.0 | 2.0 | |||
| Percentage of family members who smoke | M | 56.7 | 42.7 | 8.7 | .004 |
| SD | 35.7 | 35.5 | |||
| Percentage of friends who smoke | M | 80.1 | 75.2 | 1.9 | .17 |
| SD | 22.3 | 29.8 | |||
| Average amount spent on cigarettes (weekly) | M | $17.2 | $21.5 | 5.8 | .02 |
| SD | $10.2 | $14.5 | |||
| Likelihood of continuing to smoke after release | M | 3.8 | 3.7 | 0.1 | .82 |
| SD | 2.2 | 2.2 | |||
| Variable | White (n = 109) (%) | Black (n = 124) (%) | Chi-square | p value | |
| Thinking about quitting smoking | Within 30 days | 44.4 | 50.8 | 10.7 | .005 |
| Within 6 months | 47.2 | 49.2 | |||
| No, not considering quitting | 8.3 | — | |||
| Family members with medical problems related to smoking | Yes | 52.3 | 28.2 | 21.7 | <.001 |
| No | 19.3 | 4.86 | |||
| Do not know | 28.4 | 25.0 | |||
| Family members died from smoking | Yes | 48.6 | 25.0 | 18.4 | <.001 |
| No | 25.7 | 50.8 | |||
| Do not know | 25.7 | 24.2 | |||
| Personal medical problems from smoking | Yes | 37.6 | 26.6 | 6.4 | .042 |
| No | 37.6 | 54.0 | |||
| Do not know | 24.8 | 19.4 | |||
| Type of cigarette smoked before coming to prison | Regular | 38.8 | 4.4 | 67.7 | <.001 |
| Light | 11.7 | — | |||
| Menthol | 48.5 | 94.7 | |||
| Unfiltered/rolled | 1.0 | 0.9 | |||
| Type of cigarette smoked since coming to prison | Regular | 30.5 | 2.5 | 50.6 | <.001 |
| Menthol | 38.1 | 81.3 | |||
| Unfiltered/rolled | 31.4 | 16.1 | |||
| Change in smoking behavior since coming to prison | Started to smoke | 10.3 | 16.3 | 14.3 | .006 |
| Increased | 43.9 | 58.5 | |||
| Decreased | 24.3 | 8.9 | |||
| Stayed same | 21.5 | 15.4 | |||
| Quit | — | 0.8 | |||
White smokers reported a higher percentage of family members who smoked cigarettes. They also reported more family members with a smoking-related illness or death, but we found no differences between the two racial groups on personal medical problems related to their smoking. Black participants spent more money on cigarettes and were more likely to state that they wanted to quit smoking within the next 30 days. Significant differences were found between the racial groups on the type of cigarettes smoked, with Black smokers favoring menthol cigarettes before coming to prison and since coming to prison. Less than 1% of smokers smoked unfiltered or rolled cigarettes outside the prison, but both White (31.1%) and Black (15.9%) smokers reported that unfiltered or rolled cigarettes were the type smoked most often in prison. Black smokers were more likely to report starting smoking for the first time since coming to prison and to report increasing the amount they smoked during incarceration.
Racial differences on smoking cessation outcomes
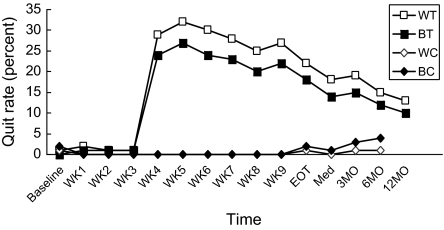
The results of the GEE analysis comparing racial groups on smoking cessation showed that the treatment by race interaction was significant. White smokers who received the intervention had overall higher quit rates than did Black participants (e.g., 30% vs. 24% abstinent at 6 weeks; 13% vs. 10% abstinent at 12 months; see Table 3 and Figure 2).
Table 3.
GEE test of model effects with smoking cessation as outcome variable and treatment group, race, and time as explanatory variables (N = 471)
| Variable | Wald chi-square | df | p value |
| Intercept | 3743.5 | 1 | <.001 |
| Treatment | 3236.2 | 1 | <.001 |
| Race | 2.1 | 1 | .147 |
| Time | 33350.4 | 14 | <.001 |
| Treatment × time | 5084.7 | 4 | <.001 |
| Treatment × race | 4.8 | 1 | .029 |
Note. GEE, generalized estimating equation; age, education, average cigarettes per day, change in smoking behavior since coming to prison, and prior mental health treatment were added as covariates.
Figure 2.
Quit rates by race across time and treatment condition (N = 471). WT, white treatment; BT, black treatment; WC, white control; BC, black control; WK, week; EOT, end of treatment; MO, month. Age, education, average number of cigarettes per day, change in smoking behavior since coming to prison, and prior mental health treatment were added as covariates.
A second GEE model was calculated to determine if differences in baseline characteristics between White and Black smokers could account for the relationship between race and smoking cessation treatment outcomes. Based on previous findings that suggest that race may be a proxy for other differences in smoking characteristics (e.g., menthol smoking; Gardiner, 2004) and differences in baseline characteristics between White and Black participants in this sample (e.g., younger Black smokers), mentholated smoking (yes/no) was entered into the model and age, education, average number of cigarettes per day, change in smoking behavior since coming to prison, and prior mental health treatment were added as covariates. Only participants who entered the active treatment arm of the study were examined in the model.
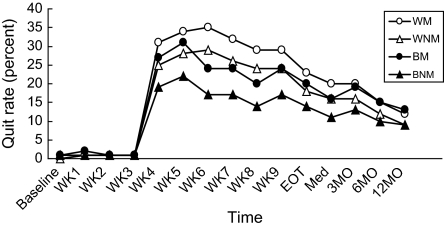
Overall, the results were similar to the original model and supported the differences in response to treatment between racial groups across time. The interaction between race and smoking menthol cigarettes was not significant, nor was there a main effect for smoking menthol cigarettes (Table 4), even when controlling for covariates. White smokers, on average, had higher quit rates, regardless of menthol cigarette preference, compared with Black smokers (Figure 3).
Table 4.
GEE test of model effects with smoking cessation as the outcome variable and race, menthol smoking, and time as explanatory variables (N = 233)
| Variable | Wald chi-square | df | p value |
| Intercept | 295.6 | 1 | <.001 |
| Race | 28.2 | 1 | <.001 |
| Time | 495.8 | 14 | <.001 |
| Menthol | 1.2 | 1 | .272 |
| Race × time | 9897.6 | 14 | <.001 |
| Race × menthol | 0.1 | 1 | .827 |
Note. GEE, generalized estimating equation; age, education, average cigarettes per day, change in smoking behavior since coming to prison, and prior mental health treatment were added as covariates.
Figure 3.
Quit rates among treated smokers by race across time and menthol use, controlling for age and average number of cigarettes per day (N = 233). WM, white menthol; WNM, white non menthol; BM, black menthol; BNM, black non menthol; WK, week; EOT, end of treatment; MO, month. Age, education, average number of cigarettes per day, change in smoking behavior since coming to prison, and prior mental health treatment were added as covariates.
Discussion
Consistent with findings from previous studies (Covey et al., 2008; USDHHS, 1998), White smokers had higher rates of smoking cessation with treatment compared with Black smokers in the present sample of incarcerated female smokers. This outcome is important, given literature that suggests that Black smokers are more susceptible to serious health consequences from smoking. Further, in our study, Black smokers were twice as likely as White smokers to smoke mentholated cigarettes during incarceration (80.2% vs. 38.7%). However, menthol preference did not account for racial differences in smoking cessation outcomes, even when controlling for important covariates. In fact, White smokers, regardless of cigarette preference, had higher quit rates, on average, than Black smokers, despite factors such as higher smoking rates and longer smoking histories that may have conveyed a poorer prognosis for quitting. Interestingly, although Black smokers smoked fewer cigarettes per day than did Whites, they also reported spending more money on cigarettes (about $21 vs. $17 per week). We believe this difference is due to menthol preference and buying name brand cigarettes (e.g., Newports), compared with buying rolling tobacco, which was cheaper and preferred by White smokers. Also, Black smokers may have bought more cigarettes from the commissary and bartered them away more frequently than did White smokers. We can only speculate about these differences because our study was not designed to explore this issue in any greater depth.
Alternative explanations for racial disparities in smoking cessation have been suggested and include slower metabolism of nicotine among Black smokers (Benowitz, O. F. Pomerleau, C. S. Pomerleau, & Jacob, 2003; Kandel, Hu, Schaffran, Udry, & Benowitz, 2007; Pérez-Stable, Herrera, Jacob, & Benowitz, 1998) and higher exposure to CO and other smoke constituents (Ahijevych & Parsley, 1999; Ahijevych et al., 2004; Melikian et al., 2007). In the present study, we can only speculate that these factors may have contributed to the differential smoking cessation rates demonstrated between White and Black smokers. More research is needed to understand the role of these variables in smoking cessation outcomes.
Our study had several limitations. First, it involved a female prisoner population, and it is not clear how these results would apply to male prisoners or nonprisoner populations. Further, prison is a unique environment of long-term confinement, and it is not clear if our results would apply to other correctional settings (e.g., jails, community corrections). Although White and Black smokers were fairly equally represented, other racial or ethnic groups were not represented. Another limitation was the high attrition out of the study, with only about half of participants who started the intervention completing the entire program. Although many individuals who left the intervention expressed frustration at their inability to quit smoking, most still allowed us to conduct long-term follow-up. Thus, given the unique aspects of the prison system, even though about half of the participants stopped attending group, we were able to determine smoking status for the majority of participants. Finally, other smoking differences between the two groups that we were not able to capture (e.g., puff volume) may have accounted for our findings.
Institutional responses to smoking generally have been to ban smoking completely within facilities or to severely restrict smoking to a few designated areas (Kauffman, Ferketich, & Wewers, 2008). However, banning smoking does not ensure complete absence of tobacco within facilities. The only study to investigate the impact of a smoking ban noted that up to 76% of inmates were still smoking 1 month after a smoking ban (Cropsey & Kristeller, 2005). Most facilities will likely ban smoking completely over the next 5–10 years, but this study is still relevant for demonstrating the feasibility of providing smoking cessation interventions within the prison system. The optimal strategy for ensuring compliance with smoking cessation bans would be to provide treatment in conjunction with such restrictions or bans.
This paper is one of the first to examine racial differences in response to a standard smoking cessation intervention that included both behavioral and pharmacotherapies and the first to extend previous observations to an incarcerated female population. Prisons are unique settings with individuals who have high rates of both smoking prevalence (70%–80%; Cropsey & Kristeller, 2003, 2005; Cropsey et al., 2004) and smoking-related health problems (Maruschak & Beck, 2001). These individuals also are unlikely to access community-based smoking cessation treatment; therefore, prison can serve as a unique point of contact for smoking cessation interventions for these individuals (Cropsey et al., 2004). Finally, minority populations, particularly Blacks, are over-represented in prisons and other correctional settings (Bureau of Justice Statistics, 1997), and understanding differential treatment responses between White and Black smokers in this environment can lead to the development of more tailored and efficacious smoking cessation interventions to reduce the morbidity and mortality associated with smoking.
Funding
National Institute on Drug Abuse (grant K23DA15774).
Declaration of Interests
None declared.
Supplementary Material
Acknowledgments
The views expressed in this paper are solely the responsibility of the authors and do not necessarily reflect the views of the National Institutes of Health or National Institute on Drug Abuse. Product support was provided by GlaxoSmithKline.
References
- Ahijevych K, Parsley LA. Smoke constituent exposure and stage of change in Black and White women cigarette smokers. Addictive Behaviors. 1999;24:115–120. doi: 10.1016/s0306-4603(98)00031-8. [DOI] [PubMed] [Google Scholar]
- Ahijevych K, Weed H, Clark J. Levels of cigarette availability and exposure in Black and White women and efficient smokers. Pharmacology Biochemistry, and Behavior. 2004;77:685–693. doi: 10.1016/j.pbb.2004.01.016. [DOI] [PubMed] [Google Scholar]
- Belcher JM, Butler T, Richmond RL, Wodak AD, Wilhelm K. Smoking and its correlates in an Australian prisoner population. Drug and Alcohol Review. 2006;25:343–348. doi: 10.1080/09595230600741198. [DOI] [PubMed] [Google Scholar]
- Benowitz NL, Pomerleau OF, Pomerleau CS, Jacob P., III Nicotine metabolite ratio as a predictor of cigarette consumption. Nicotine & Tobacco Research. 2003;5:621–624. doi: 10.1080/1462220031000158717. [DOI] [PubMed] [Google Scholar]
- Bureau of Justice Statistics. National Probation Data Survey, National Prisoner Statistics, Survey of Jails, and National Parole Data Survey. Correctional Populations in the United States. 1997 Retrieved April 9, 2009, from http://www.ojp.usdoj.gov/bjs/abstract/cpusst.htm. [Google Scholar]
- Centers for Disease Control and Prevention. Adult cigarette smoking in the United States: Current estimates. 2007 Retrieved April 9, 2009, from http://www.cdc.gov/tobacco/data_statistics/Factsheets. [Google Scholar]
- Clark PI, Gautam S, Gerson LW. Effects of menthol cigarettes on biochemical markers of smoke exposure among Black and White smokers. Chest. 1996;110:1194–1198. doi: 10.1378/chest.110.5.1194. [DOI] [PubMed] [Google Scholar]
- Colsher PL, Wallace RB, Loeffelholz PL, Sales M. Health status of older male prisoners: A comprehensive review. American Journal of Public Health. 1992;82:881–884. doi: 10.2105/ajph.82.6.881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conklin TJ, Lincoln T, Tuthill RW. Self-reported health and prior health behaviors of newly admitted correctional inmates. American Journal of Public Health. 2000;90:1939–1941. doi: 10.2105/ajph.90.12.1939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Covey LS, Botello-Harbaum M, Glassman AH, Masmela J, LoDuca C, Salzman V, et al. Smokers’ response to combination bupropion, nicotine patch and counseling treatment by race/ethnicity. Ethnicity and Disease. 2008;18:59–64. [PubMed] [Google Scholar]
- Cropsey KL, Eldridge GD, Ladner T. Smoking among female prisoners: An ignored public health epidemic. Addictive Behaviors. 2004;29:425–431. doi: 10.1016/j.addbeh.2003.08.014. [DOI] [PubMed] [Google Scholar]
- Cropsey KL, Eldridge GD, Weaver MF, Villalobos GC, Stitzer ML. Expired carbon monoxide levels in self-reported smokers and non-smokers in prison. Nicotine & Tobacco Research. 2006;8:653–659. doi: 10.1080/14622200600789684. [DOI] [PubMed] [Google Scholar]
- Cropsey KL, Eldridge GD, Weaver MF, Villalobos GC, Stitzer ML, Best AM. Smoking cessation intervention for female prisoners: Addressing an urgent public health need. American Journal of Public Health. 2008;98:1894–1901. doi: 10.2105/AJPH.2007.128207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cropsey KL, Kristeller JL. Motivational factors related to quitting smoking among prisoners during a smoking ban. Addictive Behaviors. 2003;28:1081–1093. doi: 10.1016/s0306-4603(02)00230-7. [DOI] [PubMed] [Google Scholar]
- Cropsey KL, Kristeller JL. The effects of a prison smoking ban on smoking behavior and withdrawal symptoms. Addictive Behaviors. 2005;30:589–594. doi: 10.1016/j.addbeh.2004.07.003. [DOI] [PubMed] [Google Scholar]
- Foulds J, Gandhi KK, Steinberg MB, Richardson D, Williams J, Burke M, et al. Factors associated with quitting smoking at a tobacco dependence treatment clinic. American Journal of Health Behavior. 2006;30:400–412. doi: 10.5555/ajhb.2006.30.4.400. [DOI] [PubMed] [Google Scholar]
- Foulds J, Williams JM, Gandhi KK. Racial differences in lung cancer. Letter to the editor. The New England Journal of Medicine. 2006;354:1952. [PubMed] [Google Scholar]
- Fu SS, Okuyemi KS, Partin MR, Ahluwalia JS, Nelson DB, Clothier BA, et al. Menthol cigarettes and smoking cessation during an aided quit attempt. Nicotine & Tobacco Research. 2008;10:457–462. doi: 10.1080/14622200801901914. [DOI] [PubMed] [Google Scholar]
- Gardiner PS. The African Americanization of menthol cigarette use in the United States. Nicotine & Tobacco Research. 2004;6(Suppl. 1):S55–S65. doi: 10.1080/14622200310001649478. [DOI] [PubMed] [Google Scholar]
- Hall SM, Muñoz R, Reus VI. Cognitive-behavioral intervention increases abstinence rates for depressive-history smokers. Journal of Consulting and Clinical Psychology. 1994;62:141–146. doi: 10.1037//0022-006x.62.1.141. [DOI] [PubMed] [Google Scholar]
- Hyland A, Garten S, Giovino GA, Cummings KM. Mentholated cigarettes and smoking cessation: Findings from COMMIT. Tobacco Control. 2002;11:135–139. doi: 10.1136/tc.11.2.135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jarvik ME, Tashkin DP, Caskey NH, McCarthy WJ, Rosenblatt MR. Mentholated cigarettes decrease puff volume of smoke and increase carbon monoxide absorption. Physiological Behavior. 1994;56:563–570. doi: 10.1016/0031-9384(94)90302-6. [DOI] [PubMed] [Google Scholar]
- Kandel DB, Hu M, Schaffran C, Udry JR, Benowitz NL. Urine nicotine metabolites and smoking behavior in a multiracial/multiethnic national sample of young adults. American Journal of Epidemiology. 2007;165:901–910. doi: 10.1093/aje/kwm010. [DOI] [PubMed] [Google Scholar]
- Kauffman RM, Ferketich AK, Wewers ME. Tobacco policy in American prisons, 2007. Tobacco Control. 2008;17:357–360. doi: 10.1136/tc.2007.024448. [DOI] [PubMed] [Google Scholar]
- Maruschak LM, Beck AL. Medical problems of inmates, 1997. U.S. Department of Justice, Bureau of Justice Statistics (NCJ 181644); 2001. [Google Scholar]
- Melikian AA, Djordjevic MV, Hosey J, Zhang J, Chen S, Zang E, et al. Gender differences relative to smoking behavior and emissions of toxins from mainstream tobacco smoke. Nicotine & Tobacco Research. 2007;9:377–387. doi: 10.1080/14622200701188836. [DOI] [PubMed] [Google Scholar]
- McCarthy WJ, Caskey NH, Jarvik ME, Gross TM, Rosenblatt MR, Carpenter C. Menthol vs. nonmenthol cigarettes: Effects on smoking behavior. American Journal of Public Health. 1995;85:67–72. doi: 10.2105/ajph.85.1.67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muscat JE, Richie JP, Stellman SD. Mentholated cigarettes and smoking habits in Whites and Blacks. Tobacco Control. 2002;11:368–371. doi: 10.1136/tc.11.4.368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Okuyemi KS, Ahluwalia JS, Ebersole-Robinson M, Catley D, Mayo MS, Resnicow K. Does menthol attenuate the effect of bupropion among African American smokers? Addiction. 2003;98:1387–1393. doi: 10.1046/j.1360-0443.2003.00443.x. [DOI] [PubMed] [Google Scholar]
- Pérez-Stable EJ, Herrera B, Jacob P, Benowitz NL. Nicotine metabolism and intake in Black and White smokers. The Journal of the American Medical Association. 1998;280:152–156. doi: 10.1001/jama.280.2.152. [DOI] [PubMed] [Google Scholar]
- Sieminska A, Jassem E, Konopa K. Prisoners’ attitudes towards cigarette smoking and smoking cessation: A questionnaire study in Poland. BMC Public Health. 2006;6:181–190. doi: 10.1186/1471-2458-6-181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services. Tobacco use among U.S. racial/ethnic groups—African Americans, American Indian and Alaska Natives, Asian Americans and Pacific Islanders, and Hispanics: A report of the surgeon general. Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention; 1998. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.