Abstract
Purpose
Human DNA topoisomerases I and II (topo-I and -II) are essential for vital cellular processes such as DNA replication, transcription, translation, recombination, and repair. In the present study, we correlate topo-I and -II expression and outcome after chemotherapy in primary and relapsed colorectal cancer.
Patients and methods
Patients with colorectal cancer that had recurred, following surgery and adjuvant chemotherapy and underwent a second operation were included in the present study. All had undergone surgical resection of the primary tumor and received post-operatively 5-FU-based (5FU + Leucovorin, Mayo Clinic regimen) adjuvant chemotherapy. Tumor tissue was collected at the initial operation from the primary tumor and at the time of recurrence (during the second operation following chemotherapy). All tissue samples were analyzed for levels of expression of both topo-I and topo-IIa using standard three-step immunohistochemistry on paraffin sections.
Results
Forty patients were included. Levels of expression of topo-I and topo-II were higher in malignant cells from tumor recurrences compared to primary tumors (P = 0.0001 for both). There was a statistically significant positive relationship between patients age and levels of topo-I (P = 0.011) and topo-II (P = 0.011) expression.
Conclusions
The study results reported here underscore the role of topoisomerase expression in colorectal cancer and suggest a potential role in tumor recurrence.
Keywords: Topoisomerase I, Topoisomerase IIα, Colorectal cancer, 5-FU, Chemotherapy
Introduction
The aim of the present study was to investigate whether chemotherapy with 5-FU alters the levels of topoisomerase I (topo-I) and II (topo-II) in neoplastic tissues from patients with colorectal cancer. To this end, we examined the relationship between clinical data and the expression of topo I and II in patients treated with 5-FU post-operatively and who underwent surgery at recurrence.
Human DNA topo-I is an essential nuclear enzyme for vital cellular processes such as DNA replication, transcription, translation, recombination and repair. Topo-I unwinds and uncoils the supercoiled DNA double helix by transiently cleaving one of the two strands and allowing its rotation over the other, following which topo-I reseals the cleaved strand [1–5]. Topo-II works in a similar manner, with the difference that it cleaves both DNA strands, allowing the passage of an intact double helix through the break. The entire reaction takes place at the expense of ATP hydrolysis [6]. In contrast to topo-I, which is monomeric, two homologous but distinct isoforms of type II human topoisomerases have been identified, DNA topo-IIα and IIβ [6, 7]. The α isoform is the type II topoisomerase that was originally described and characterized in mammalian species [6].
Several studies have shown topo-IIα to be a reliable marker of cell proliferation in tumors [8, 9]. In contrast to topo-II, topo-I levels are not cycle-specific and remain stable throughout the cell cycle [10]. Topo-IIα plays important roles in DNA synthesis and transcription, as well as chromosomal segregation during mitosis. Beyond its physiological functions, topo-IIα is reported to be a sensitive and specific marker of actively proliferating cells (in the late S, G2 and M-phases of the cell cycle) and has been used as a proliferation marker in studies of colorectal cancer [7, 8, 10]. In addition to the well described role of the three MDR-related proteins, topo-IIα has been implicated in drug resistance of tumor cells [9].
Topo-I catalytic activity has been evaluated in various studies and has been detected in all normal tissues at fairly constant levels [10]. Additional parameters were further investigated: topo-I immunoreactive protein levels were estimated by Western blot analysis, and topo-I gene expression (topo-I mRNA) was evaluated by Northern blot analysis. With regard to colorectal tumors, they were found to exhibit 5- to 35-fold increases in topo-I levels compared to the adjacent normal colonic mucosa [11].
Topo-I expression has also been evaluated by immunohistochemistry in paraffin-embedded human tissues [12], and its expression has been demonstrated in numerous neoplastic tissues. Increased topo-I has been shown in ovarian carcinomas (elevated topo-I expression in 43% of tumors) [12]; colorectal carcinomas (ranging from 43–86% in various studies) [13–15]; testicular tumors (30–38% in seminomas, 30% in embryonal carcinomas, and 100% in teratomas and yolk sac tumors) [16]; transitional carcinoma of the bladder (overexpression in 77%) [17], and renal cell carcinomas (ranging from 36–100% according to grade) [18]; malignant melanomas (overexpression in 41.6%) [19]; gastric carcinomas (overexpression in 68%) [20]; sarcomas (high levels of topo-I in 13%) [21]; breast carcinomas (overexpression in 41%) [22], oral dysplasias, and squamous cell carcinomas (overexpression in 79 and 92%, respectively) [23, 24]. In normal tissues, topo-I expression appeared to be higher in the germinal centers of the tonsil and in the mucosal lymphocytes of the colon, while topo I positivity was also detected in the glandular epithelium of the colon [12].
Patients and methods
Patients
Forty patients with colorectal cancer that had recurred following surgery and adjuvant chemotherapy who underwent a second operation were included in this study. All had undergone surgical resection for their primary tumor and received post-operatively 5-FU-based [5FU and Leucovorin (LV), Mayo Clinic regimen] adjuvant chemotherapy [25]. Patients characteristics are described in Table 1.
Table 1.
Patients characteristics
| Patients (n) | 40 |
| Gender | |
| Men | 25 |
| Women | 15 |
| Median age at diagnosis (years) | 58 (35–75) |
| Performance status (WHO), 0–1 | 40 |
| Location of primary tumor | |
| Right colon | 6 |
| Left colon | 28 |
| Rectum | 6 |
| Stage (Dukes’) | |
| B2 | 13 |
| C | 27 |
| Relapse | |
| Local | 17 |
| Distant | 23 |
| Differentiation | |
| Well | 2 |
| Moderate | 31 |
| Poor | 7 |
| Disease-free survival (months) | 18 (range, 6–79) |
Study plan
Tumor tissue was collected during the initial operation from the primary tumor, before the administration of any adjuvant chemotherapy and also at the time of recurrence (during the second operation following chemotherapy). All these tissues were analyzed for expression of both topo-I and topo-IIα.
Determination of topo-I and topo-IIα
The expression of topo-I and topo-IIα was studied on paraffin sections by a standard three-step immunohistochemistry. Topogen, an anti-topo-I monoclonal antibody (mAb) (2012-3) was applied. Topogen is a mouse mAb (IgG2b isotype); its epitope has not been mapped [26–28]. The primary mAb JH2.7 for topo-IIα (Biocare Medical, CA, USA) is a mouse mAb (IgG1 isotype) that recognizes a 170-kDa protein, the epitope of which maps between aminoacid 854–1447 of topo-IIα [27–29]. Counterstaining with hematoxylin was applied in the end of the classical immunohistochemistry procedure.
Positive and negative controls
For the expression of topo-I and –IIa, normal human tonsil tissues immunostaining served as positive controls. Non-specific, isotype-matched monoclonal Abs worked well as substitute negative controls [26–29].
Determination of topo-I and topo-IIα expression
First step Sections were examined for quantified immunoreactivity by two independent investigators blinded to any relevant patient clinical data. They evaluated more than 1,000 neoplastic cells in consecutive areas of neoplastic tissue. The numbers of positive cells were then expressed as a percentage of labeled tumor cells with respect to the total number of tumor cells that were evaluated. Immunostaining for topo-I and -IIα was graded according to the percentage of tumor cells staining positive (and ± for <5%, + for 5–50% and ++ for 50 to 75% of cells with positive staining) and intensity of staining (weakly positive, moderately positive, or strongly positive). To simplify the scoring, we graded them as 0 (negative cells), 1 (± and/or <5%), 2 (+ and/or 5–50%), 3 (++ and/or 50–75%). Then, the sections were evaluated classified in pairs (one section from the first surgery and one section from the second surgery for each patient).
Second step The percentages of immunoreactive malignant cells were calculated using an image analysis system with an appropriate software package [Sigma Scan Pro, Version 5.0 (SPSS Science, Erkrath, Germany)]. The ratio was calculated as a percentage of immunohistochemically positive neoplastic cells over the total number (stained and unstained) of neoplastic cells. The membrane, cytoplasmic or nuclear intensity of the specific immunohistochemical stain, was also assessed. All the positively stained cells were classified in two groups (weakly stained and strongly stained).
DNA ploidy of neoplastic cells was evaluated by image DNA cytometry performed on Feulgen-stained sections. Images were acquired using a Zeiss Axiolab microscope (Carl Zeiss Jena GmbH, Jena, Germany) with a mechanical stage, fitted with a SONY-iris CCD video camera (SONY Corporation, Tokyo, Japan). The latter was connected to a Pentium II personal computer which included the relevant software. Slides were examined at low power magnification (40×) to identify the areas with the highest cellularity. In each case, a total number of ≥200 Feulgen-stained nuclei was selected at high power magnification (400×) and stored as JPEG file [1,550 × 1,070 pixels, 16.7 million colors (24-bit)]. Then the images were converted to gray scale and the staining intensity of the Feulgen-stained nuclei was measured semi-automatically. A classification of the nuclei in pairs according to their staining intensity followed. Finally, the graphic presentation of the nuclei demonstrating their distribution according to their DNA content was also performed.
Statistical analysis
All analyses were performed with SPSS version 10.1 (Statistical Product and Service Solutions; SPSS Inc., Chicago, IL, USA). We used McNemar’s paired Chi-square test to assess the possible alteration of the levels of topoisomerases after chemotherapy with 5-FU. Fisher’s exact test was performed in order to assess the possible relationship of topoisomerase increase with gender, Dukes’ stage, tumor grade and localization. Mann–Whitney U Test was performed to assess a possible relationship between patient age and alteration in topoisomerases levels.
Results
Patients
Forty patients were included in the present study. Of these, 25 were men and 15 were women. The median age was 58 years (range, 35–75). All patients had a performance status (PS) of 0–1. Tumor localization at the time of diagnosis was: right colon 6, left colon 28, and rectum 6. According to pathological classification, 13 patients had Dukes B2 tumors, and the remaining 27 Dukes C. With regard to differentiation, 2 tumors were well differentiated, 31 moderately and, 7 were poorly differentiated. Of all these patients, 17 relapsed locally and 23 with distant metastases, with a median relapse-free interval of 18 (range, 6–79) months (Table 1). All patients who entered the trial were evaluable for analysis.
Ploidy
Out of 40 primary tumors, 12 were highly aneuploid and the remaining 28 were moderately aneuploid. There was no association between the degree of DNA aneuploidy and the expression of any of the analyzed markers.
Topoisomerase I
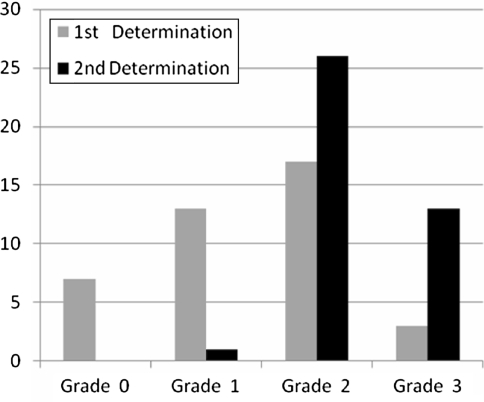
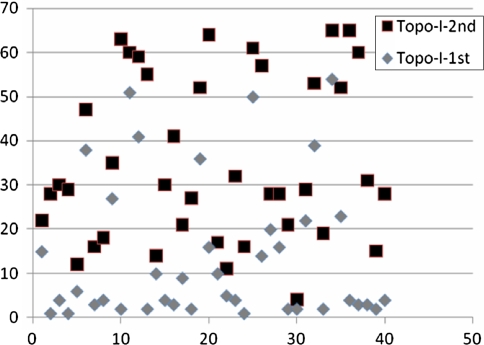
Immunohistochemical analysis revealed that levels of topo-I expression were higher in malignant cells from tumor recurrences compared to cells from the primary tumors (P = 0.0001) (Table 2; Fig. 1); decreased in grade 1 (P = 0.007) and increased in grade 3 (P = 0.003) (Table 2). In image analysis evaluation, there was a significant increase in malignant cells from the tumor recurrences (P = 0.0001) (Table 3); low expression was noticed in range 1–5 (P = 0.0001) and 26–30 (P = 0.0143) (Table 3; Fig. 3). The increase in topo-I levels was not significantly correlated with gender, performance status (WHO), location of the primary tumor, Dukes’ stage, grade of differentiation, and localization of relapse. There was a statistically significant relationship between the age of patients and the expression of topo-I (P = 0.011). Patients with an increased expression of topo-I levels were older in age (median = 62.5) than patients without increased expression (median = 50).
Table 2.
Photomicroscopic evaluation
| Examined parameters | Photo, microscopic evaluation | P | ||
|---|---|---|---|---|
| Grade | First evaluation | Second evaluation | ||
| Topoisomerase I | 0 | 7 | 0 | 0.0117 |
| 1 | 13 | 1 | 0.0007 | |
| 2 | 17 | 26 | 0.0722 | |
| 3 | 3 | 13 | 0.0103 | |
| Increased: 25, decreased: 0, no change: 15, P = 0.0001 | ||||
| Topoisomerase IIa | 0 | 0 | 0 | 1 |
| 1 | 10 | 2 | 0.0252 | |
| 2 | 30 | 28 | 0.8027 | |
| 3 | 0 | 10 | 0.0010 | |
| Increased: 18, decreased: 0, no change: 22, P = 0.0001 | ||||
Fig. 1.
Topoisomerase I (Topo-I) expression in relation to tumor grade according to immunohistochemical evaluation
Table 3.
Image analysis evaluation (%)
| Range | First sample (no.) | Second sample (no.) | P | Range | First sample (no.) | Second sample (no.) | P |
|---|---|---|---|---|---|---|---|
| Topoisomerase I | |||||||
| 0 | 0 | 0 | 1 | 36–40 | 3 | 0 | 0.2405 |
| 1–5 | 21 | 1 | 0.0001 | 41–45 | 1 | 1 | 1.000 |
| 6–10 | 4 | 0 | 0.1156 | 46–50 | 1 | 1 | 1.000 |
| 11–15 | 2 | 4 | 0.6752 | 51–55 | 2 | 4 | 0.6752 |
| 16–20 | 3 | 5 | 0.7119 | 56–60 | 0 | 4 | 0.1156 |
| 21–25 | 2 | 3 | 1 | 61–65 | 0 | 5 | 0.0547 |
| 26–30 | 1 | 9 | 0.0143 | 66–70 | 0 | 0 | |
| 31–35 | 0 | 3 | 0.2405 | 71–80 | 0 | 0 | |
| Topoisomerase IIa | |||||||
| 0 | 0 | 0 | 1 | 36–40 | 2 | 3 | 1 |
| 1–5 | 10 | 4 | 0.1395 | 41–45 | 5 | 1 | 0.2007 |
| 6–10 | 6 | 5 | 1 | 46–50 | 0 | 3 | 0.2405 |
| 11–15 | 5 | 2 | 0.4315 | 51–55 | 0 | 2 | 0.4937 |
| 16–20 | 9 | 1 | 0.0143 | 56–60 | 0 | 0 | 1 |
| 21–25 | 0 | 5 | 0.0547 | 61–65 | 0 | 1 | 1 |
| 26–30 | 3 | 3 | 1 | 66–70 | 0 | 2 | 0.4937 |
| 31–35 | 0 | 3 | 0.2405 | 71–80 | 0 | 5 | 0.0547 |
| Total | First determination | Second determination | P | ||||
|---|---|---|---|---|---|---|---|
| Mean | Median | Range | Mean | Median | Range | ||
| Topoisomerase I | 13.875 | 4.5 | 1–54 | 35.375 | 29.5 | 4–65 | 0.0001 |
| Topoisomerase IIa | 16.775 | 15 | 1–45 | 34.575 | 31 | 2–79 | 0.0001 |
Fig. 3.
Dispersion diagram of topoisomerase I (Topo-Ι) expression as assessed by immunohistochemistry
Topoisomerase IIα
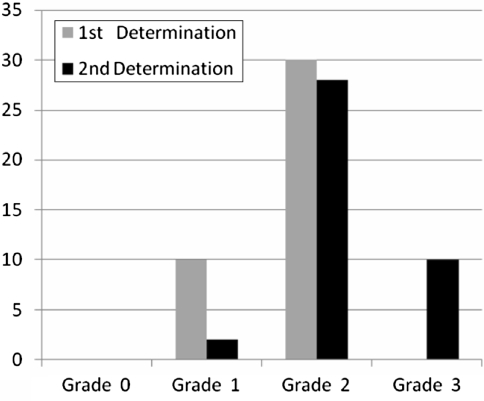
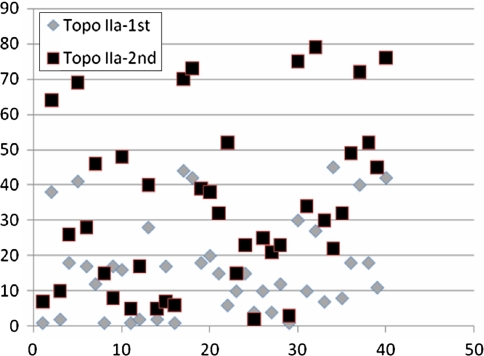
Malignant cells from tumor recurrences showed statistically significantly increased levels of topo-II, compared to those of the primary tumors (P = 0.0001) (Table 2; Fig. 2); while topo-II levels were decreased in grade 3 lesions (P = 0.0001) (Table 2; Fig. 4). In image analysis, there was a significant increase in malignant cells from tumor recurrences (P = 0.0001) (Table 3); low expression was noticed in the range of 16–20 (P = 0.0143) (Table 3). There was a statistically significant relationship between the age of patients and increased levels of expression of topo-IIα (P = 0.011). Levels of topo-IIα expression were higher in malignant cells from tumor recurrences compared to cells from primary tumors (P = 0.0001). There was a statistically significant positive correlation between the age of patients and increased levels of expression topo-IIα (P = 0.011). The increase in topo-IIα levels did not demonstrate any significant correlations with gender, age, PS (WHO), localization of primary tumor, Dukes’ stage, tumor grade, and location of relapse when compared to topo-IIα levels in the primary tumors (P = 0.0001).
Fig. 2.
Topoisomerase IIα (Topo-IIα) expression in relation to tumor grade according to immunohistochemical evaluation
Fig. 4.
Dispersion diagram of topoisomerase IΙα Topo-IIΑ expression as assessed by immunohistochemistry
Discussion
In our study, 33 out of 40 (83%) samples of colorectal cancer stained positive for topoisomerase (Table 2; Fig. 3). This finding is in close agreement with the results of Staley et al. [14], who reported 86% of positive staining in 29 samples, but in contrast with the results from Boonsong et al. [13], who demonstrated a lower percentage of cells expressing topo-I; 51% of the samples, including 24.4% with >50% positive tumor cells [13]. Topo-I immunoreactivity was confined to the nucleus in all samples, being consistent with the role of topo-I as a nuclear protein. For topo-IIα, 21 out of 40 (52%) samples of colorectal cancer stained positive (Table 2; Fig. 4), including 10/40 (25%) with weak positive staining (grade 1). This finding was confirmed by Image Analysis (Table 3). These data are consistent with those reported by Burden and Osheroff [6].
In this study, we present significantly increased topo-I and topo-IΙα expression in recurrent colorectal tumors, reinforcing the view that their expression is likely part of the malignant cells phenotype in recurrent colorectal carcinomas. This observation is in agreement with previous studies [15, 30], which demonstrated a direct correlation between thymidylate synthase (TS) and topo-I tumor expression and hypothesized, similar to TS [31], that high topo-I expression is related to a more aggressive biological phenotype. Of note, increased topo-IIα expression characterizes rapidly proliferating cells [6] and represents an accepted marker of aggressive tumor behavior [32].
Since the increase of topo-I and -IIα expression was demonstrated following 5-FU-based treatment, it is tempting to attribute this change to 5-FU. High levels of topo-I correlate with sensitivity to camptothecins (irinotecan and topotecan) [17], whereas high levels of topo-IIα correlate with sensitivity to etoposide, a known topo-IIα-targeting agent [32]. Thus, it is reasonable to consider applying these agents sequentially for the treatment of colorectal cancer; i.e. 5-FU → irinotecan and 5-FU → etoposide.
Irinotecan (CPT-11), a water soluble camptothecin derivative, is a specific potent inhibitor of topo-I [33]. In a European phase II study, irinotecan achieved response rates of 19% in chemotherapy-naive patients and 18% in pretreated patients with advanced disease [34].
Drugs that target topo-II, such as etoposide (VP-16), doxorubicin, and mitoxantrone, are among the most effective anticancer drugs in clinical use. Etoposide destroys cells by inhibiting the ability of topo-II to ligate nucleic acids cleaved during the double-stranded DNA passage reaction [35].
Irinotecan yielded response rates of 15–25% in 5-FU-refractory patients [36–44], not dissimilar to those observed in first-line treatment of colorectal cancer (18–32%) [45–47] and in contrast to the expected decreasing response rate from the application of irinotecan in second-line treatment. Treating patients with irinotecan upon progression to 5-FU/LV seems to be yielding more significant results compared to the opposite sequence, based in our previous experience, where the best results with sequential monotherapies were obtained when 5-FU/LV was followed by irinotecan (5-FU/LV → CPT11) at disease progression or relapse [41].
With regard to irinotecan efficacy, in vitro data suggest that topo-I expression could be regarded as an important cellular sensitivity determinant [16]. In particular, decreased DNA topo-I expression was correlated with camptothecin-resistant cell lines [27], while Jansen et al. [36] reported a positive correlation between irinotecan sensitivity and topo-I activity.
Topo-IIα is the primary cytotoxic target of some of the most effective chemotherapeutic drugs, such as the epipodophylotoxins, etoposide (VP-16) and teniposide (VM-26) [32]. Studies in previously untreated patients with advanced colorectal carcinoma evaluating the combination of etoposide with cisplatin or 5-FU demonstrated minimal activity in metastatic colorectal cancer [48–51]; there have been no clinical data supporting the in vitro synergy observed between these cytotoxic agents [52, 53]. Other studies failed to prove any benefit with the combination of etoposide with 5-FU or cisplatin/carboplatin [54]. However, the combination of etoposide with 5-FU + LV had demonstrated some activity when administered as second-line treatment after failure of weekly 5-FU + LV in patients with metastatic colorectal cancer [55, 56].
The results reported herein underscore the role of topoisomerase (topo-I and topo-IIα) expression in colorectal cancer. It is believed that translational studies of molecular targets for currently applied cytotoxic and biological agents (like bevacizumab and cetuximab) might form the basis of current and future drug combinations, in rationalizing the optimal chemotherapeutic drug schedule and sequence that, will eventually translate in improved tumor eradication and survival prolongation.
Acknowledgments
We thank Dimitris Boulamatsis for the statistical analysis of the manuscript and Madalena Zlovotska for collection of the data. This trial was supported by a grant from ELKE 80546 of the University of Athens School of Medicine.
Open Access This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Footnotes
An erratum to this article can be found at http://dx.doi.org/10.1007/s00280-009-0988-7
Contributor Information
Nicolas Tsavaris, Phone: +30-210-6463191, FAX: +30-210-6463191, Email: tsavari1@otenet.gr.
Christos Kosmas, Email: ckosm1@ath.forthnet.gr.
References
- 1.Gupta M, Fujimori A, Pommier Y (1995) Eukaryotic DNA topoisomerases I. Biochim Biophys Acta 1262:1–14 [DOI] [PubMed]
- 2.Pommier Y, Pourquier P, Fan Y, Strumberg D (1998) Mechanism of action of eukaryotic DNA topoisomerase I and drugs targeted to the enzyme. Biochim Biophys Acta 1400:83–105 [DOI] [PubMed]
- 3.Stewart L, Redinbo MR, Qiu X, Hol WG, Champoux JJ (1998) A model for the mechanism of human topoisomerase I. Science 279:1534–1541 [DOI] [PubMed]
- 4.Merino A, Madden KR, Lane WS, Champoux JJ, Reinberg D (1993) DNA topoisomerase I is involved in both repression and activation of transcription. Nature 365:227–232 [DOI] [PubMed]
- 5.Florell SR, Martinchick JF, Holden JA (1996) Purification of DNA topoisomerase I from the spleen of a patient with non-Hodgkin’s lymphoma. Anticancer Res 16:3467–3474 [PubMed]
- 6.Burden DA, Osheroff N (1998) Mechanism of action of eukaryotic topoisomerase II and drugs targeted to the enzyme. Biochim Biophys Acta 1400:139–154 [DOI] [PubMed]
- 7.Kellner U, Jacobsen A, Kellner A, Mantke R, Roessner A, Röcken C (2003) Comparative genomic hybridization. Synchronous occurrence of focal nodular hyperplasia and hepatocellular carcinoma in the same liver is not based on common chromosomal aberrations. Am J Clin Pathol 119:265–271 [DOI] [PubMed]
- 8.Nakopoulou L, Zervas A, Lazaris AC, Constantinides C, Stravodimos C, Davaris P, Dimopoulos C (2001) Predictive value of topoisomerase IIα immunostaining in urothelial bladder carcinoma. J Clin Pathol 54:309–313 [DOI] [PMC free article] [PubMed]
- 9.Gibbons D, Fogt F, Kasznica J, Holden J, Nikulasson S (1997) Comparison of topoisomerase II alpha and Ki-67 expression in uterine cervical squamous lesions. Mod Pathol 10:409–413 [PubMed]
- 10.Heck MM, Hittelman WN, Earnshaw WC (1988) Differential expression of DNA topoisomerases I and II during the eukaryotic cell cycle. Proc Natl Acad Sci USA 85:1086–1090 [DOI] [PMC free article] [PubMed]
- 11.Bronstein IB, Vorobyev S, Timofeev A, Jolles CJ, Alder SL, Holden JA (1996) Elevations of DNA topoisomerase I catalytic activity and immunoprotein in human malignancies. Oncol Res 8:17–25 [PubMed]
- 12.Holden JA, Rahn MP, Jolles CJ, Vorobyev SV, Bronstein IB (1997) Immunohistochemical detection of DNA topoisomerase I in formalin fixed, paraffin wax embedded normal tissues and in ovarian carcinoma. J Clin Pathol 50:247–253 [DOI] [PMC free article] [PubMed]
- 13.Boonsong A, Curran S, McKay JA, Cassidy J, Murray GI, McLeod HL (2002) Topoisomerase I protein expression in primary colorectal cancer and lymph node metastases. Hum Pathol 33:1114–1119 [DOI] [PubMed]
- 14.Staley BE, Samowitz WS, Bronstein IB, Holden JA (1999) Expression of DNA topoisomerase I and DNA topoisomerase II-alpha in carcinoma of the colon. Mod Pathol 12:356–361 [PubMed]
- 15.Paradiso A, Xu J, Mangia A, Chiriatti A, Simone G, Zito A, Montemurro S, Giuliani F, Maiello E, Colucci G (2004) Topoisomerase-I, thymidylate synthase primary tumour expression and clinical efficacy of 5-FU/CPT-11 chemotherapy in advanced colorectal cancer patients. Int J Cancer 111:252–258 [DOI] [PubMed]
- 16.Coleman LW, Perkins SL, Bronstein IB, Holden JA (2000) Expression of DNA toposiomerase I and DNA topoisomerase II-alpha in testicular seminomas. Hum Pathol 31:728–733 [DOI] [PubMed]
- 17.Monnin KA, Bronstein IB, Gaffney DK, Holden JA (1999) Elevations of DNA topoisomerase I in transitional cell carcinoma of the urinary bladder: correlation with DNA topoisomerase II-alpha and p53 expression. Hum Pathol 4:384–391 [DOI] [PubMed]
- 18.Gupta D, Bronstein IB, Holden JA (2000) Expression of DNA topoisomerase I in neoplasms of the kidney: correlation with histological grade, proliferation, and patient survival. Hum Pathol 31:214–219 [DOI] [PubMed]
- 19.Perego P, Capranico G, Supino R, Zunino F (1994) Topoisomerase I gene expression and cell sensitivity to camptothecin in human cell lines of different tumor types. Anticancer Drugs 5:645–649 [DOI] [PubMed]
- 20.Coleman LW, Bronstein IB, Holden JA (2001) Immunohistochemical staining for DNA topoisomerase I, DNA topoisomerase II-alpha and p53 in gastric carcinomas. Anticancer Res 21:1167–1172 [PubMed]
- 21.Coleman LW, Rohr LR, Bronstein IB, Holden JA (2002) Human DNA topoisomerase I: an anticancer drug target present in human sarcomas. Hum Pathol 33:599–607 [DOI] [PubMed]
- 22.Lynch BJ, Bronstein IB, Holden JA (2001) Elevations of DNA topoisomerase I in invasive carcinoma of the breast. Breast J 7:176–180 [DOI] [PubMed]
- 23.Hafian H, Venteo L, Sukhanova A, Nabiev I, Lefevre B, Pluot M (2004) Immunohistochemical study of DNA topoisomerase I, DNA topoisomerase II alpha, p53, and Ki-67 in oral preneoplastic lesions and oral squamous cell carcinomas. Hum Pathol 35:745–751 [DOI] [PubMed]
- 24.Shamaa AA, Zyada MM, Wagner MM, Awad SS, Osman MM, Abdel Azeem AA (2008) The significance of Epstein Barr Virus (EBV) & DNA topoisomerase IIu (DNA–TopoII) immunoreactivity in normal oral mucosa, oral epithelial dysplasia (OED) and oral squamous cell carcinoma (OSCC). Diagn Pathol 3:45 [Epub ahead of print] [DOI] [PMC free article] [PubMed]
- 25.Heidelberger C, Chaudhuri NK, Danneberg P, Mooren D, Griesbach L, Duschinsky R, Schnitzer RJ, Pleven E, Scheiner J (1957) Fluorinated pyrimidines: a new class of tumor inhibitory compounds. Nature 179:663–666 [DOI] [PubMed]
- 26.Libutti SK, Salz LB, Rustgi AK, Tepper JE (2005) Cancer of the colon. In: Devita VT, Hellman S, Rosenberg S (eds) Cancer: principles and practice of oncology, Chap 29, Sect 8. Lippincott Williams and Wilkins, Philadelphia
- 27.Gouveris P, Lazaris AC, Papathomas TG, Nonni A, Kyriakou V, Delladetsima J, Patsouris ES, Tsavaris N (2007) Topoisomerase I protein expression in primary colorectal cancer and recurrences after 5-FU-based adjuvant chemotherapy. J Cancer Res Clin Oncol 133:1011–1015 [DOI] [PMC free article] [PubMed]
- 28.Lazaris AC, Kavantzas NG, Zorzos HS, Tsavaris NV, Davaris PS (2002) Markers of drug resistance in relapsing colon cancer. J Cancer Res Clin Oncol 128:114–118 [DOI] [PMC free article] [PubMed]
- 29.Zorzos HS, Lazaris AC, Korkolopoulou PA, Kavantzas NG, Tseleni-Balafouta S, Patsouris ES, Tsavaris NV, Davaris PS (2003) Multidrug resistance proteins and topoisomerase II alpha expression in colon cancer: association with metastatic potential. Pathology 35:315–318 [DOI] [PubMed]
- 30.Tsavaris N, Kosmas C, Zorzos H, Lazaris A, Vadiaka M, Dimitrakopoulos A, Siakantaris MP, Rokana S, Papalambros E, Pangalis GA, Davaris P (2004) Breast cancer after curative chemotherapy in non-Hodgkin’s lymphoma: examination of the role of drug resistance and retrospective comparison to the outcome of de novo breast cancer. Oncol Rep 11:899–903 [DOI] [PubMed]
- 31.Ichikawa W, Uetake H, Nihei Z, Mastuo K, Fujita H, Yamada Y (1999) Topoisomerase I (Topo-I) expression correlates to thymidylate synthase (TS) expression in colorectal cancer (CRC). Proc Am Soc Clin Oncol 18:946 (abstract)
- 32.Leichman CG, Lenz HJ, Leichman L, Danenberg K, Baranda J, Groshen S, Boswell W, Metzger R, Tan M, Danenberg PV (1997) Quantitation of intratumoral thymidylate synthase expression predicts for disseminated colorectal cancer response and resistance to protracted-infusion fluorouracil and weekly leucovorin. J Clin Oncol 15:3223–3229 [DOI] [PubMed]
- 33.Hande KR (1998) Clinical applications of anticancer drugs targeted to topoisomerase II. Biochim Biophys Acta 1400:173–184 [DOI] [PubMed]
- 34.Luzzio MJ, Besterman JM, Emerson DL, Evans MG, Lackey K, Leitner PL, McIntyre G, Morton B, Myers PL, Peel M, Sisco JM, Sternbach DD et al (1995) Synthesis and antitumor activity of novel water soluble derivatives of camptothecin as specific inhibitors of topoisomerase I. J Med Chem 38:395–401 [DOI] [PubMed]
- 35.Bleiberg H (1998) Continuing the fight against advanced colorectal cancer: new and future treatment options. Anticancer Drugs 9:18–28 [DOI] [PubMed]
- 36.Wilstermann AM, Bender RP, Godfrey M, Choi S, Anklin C, Berkowitz DB, Osheroff N, Graves DE (2007) Topoisomerase II-drug interaction domains: identification of substituents on etoposide that interact with the enzyme. Biochemistry 46:8217–8225 [DOI] [PMC free article] [PubMed]
- 37.Bognel C, Rekacewicz C, Mankarios H, Pignon JP, Elias D, Duvillard P, Prade M, Ducreux M, Kac J, Rougier P, Eschwège F, Lasser P (1995) Prognostic value of neural invasion in rectal carcinoma: a multivariate analysis on 339 patients with curative resection. Eur J Cancer 31A:894–898 [DOI] [PubMed]
- 38.Rothenberg ML, Burris HA III (1994) Irinotecan as second line therapy for patients with 5-FU refractory colorectal cancer. Proc Am Soc Clin Oncol 13:198 (abstr)
- 39.Conti JA, Saltz L (1994) Irinotecan is an active agent in untreated patients with metastatic colorectal cancer. Proc Am Soc Clin Oncol 13:195 (abstr) [DOI] [PubMed]
- 40.Pitot HC, O’Connell MJ (1994) A phase II trial of CPT-11 in patients with metastatic colorectal carcinoma: a North Central Cancer Treatment Group Study. Proc Am Soc Clin Oncol 13:197 (abstr)
- 41.Gupta E, Lestingi TM, Mick R, Ramirez J, Vokes EE, Ratain MJ (1994) Metabolic fate of irinotecan in humans: correlation of glucuronidation with diarrhea. Cancer Res 54:3723–3725 [PubMed]
- 42.Tsavaris N, Kosmas C, Skopelitis H, Papadoniou N, Polyzos A, Zografos G, Adoniou E, Gryniatsos J, Felekouras E, Zacharakis M, Sigala F, Bacoyiannis C et al (2007) Sequential administration of 5-fluorouracil (5FU)/leucovorin (LV) followed by irinotecan (CPT-11) at relapse versus CPT-11 followed by 5-FU/LV in advanced colorectal carcinoma. A phase III randomized study. Chemotherapy 53:282–291 [DOI] [PubMed]
- 43.Gennatas C, Papaxoinis G, Michalaki V, Mouratidou D, Andreadis C, Tsavaris N, Pafiti A (2006) A prospective randomized study of irinotecan (CPT-11), leucovorin (LV) and 5-fluorouracil (5FU) versus leucovorin and 5-fluorouracil in patients with advanced colorectal carcinoma. J Chemother 18:538–544 [DOI] [PubMed]
- 44.Tsavaris N, Ziras N, Kosmas C, Giannakakis T, Gouveris P, Vadiaka M, Dimitrakopoulos A, Karadima D, Rokana S, Papalambros E, Papastratis G, Margaris H et al (2003) Two different schedules of irinotecan (CPT-11) in patients with advanced colorectal carcinoma relapsing after a 5-fluorouracil and leucovorin combination. A randomized study. Cancer Chemother Pharmacol 52:514–519 [DOI] [PubMed]
- 45.Tsavaris NB, Polyzos A, Gennatas K, Kosmas Ch, Vadiaka M, Dimitrakopoulos A, Macheras A, Papastratis G, Tsipras H, Margaris H, Papalambros E, Giannopoulos A et al (2002) Irinotecan (CPT-11) in patients with advanced colon carcinoma relapsing after 5-fluorouracil-leucovorin combination. Chemotherapy 48:94–99 [DOI] [PubMed]
- 46.Mitry E, Ducreux M, Rougier P (1998) Second-line irinotecan chemotherapy in the treatment of metastatic colorectal cancers: phase III trials. Bull Cancer 38-42 [PubMed]
- 47.Van Cutsem E, Peeters M (1998) Irinotecan monotherapy in the treatment of colorectal cancers: results of phase II trials. Bull Cancer 33-7 [PubMed]
- 48.Boige V, Raymond E, Armand JP (1998) Irinotecan: various administration schedules, study of drug combinations, phase I experience. Bull Cancer 26-32 [PubMed]
- 49.Planting AS, van der Burg ME, van den Bent MJ, de Boer-Dennert M, Stoter G, Verweij J (1996) Phase II study of a short course of weekly high-dose cisplatin combined with long-term oral etoposide in metastatic colorectal cancer. Br J Cancer 73:1265–1267 [DOI] [PMC free article] [PubMed]
- 50.Passalacqua R, Bisagni G, Cocconi G, Boni C, Di Blasio B, Ceci G (1991) Cisplatin and etoposide in advanced colorectal carcinoma. Ann Oncol 2:687–688 [DOI] [PubMed]
- 51.Posner M, Slapak CA, Browne MJ, Clark JW, Curt G, Weitberg A, Calabresi P, Cummings FJ, Wiemann M, Urba S (1990) A phase I-II trial of continuous-infusion cisplatin, continuous-infusion 5-fluorouracil, and VP-16 in colorectal cancer. Am J Clin Oncol 13:455–458 [DOI] [PubMed]
- 52.Colucci G, Maiello E, Giuliani F, Cifarelli RA, Giotta F (1995) Carboplatin and etoposide in previously treated colorectal cancer patients. Tumori 81:36–38 [DOI] [PubMed]
- 53.Zelkowitz RS, Posner MR, Cummings F, Beitz J, Weitberg AB (1989) A phase I/II trial of 5-fluorouracil and etoposide in metastatic colorectal carcinoma. Am J Clin Oncol 12:492–493 [DOI] [PubMed]
- 54.Inaba M, Mitsuhashi J, Kawada S, Nakano H (1994) Different modes of cell-killing action between DNA topoisomerase I and II inhibitors revealed by kinetic analysis. Jpn J Cancer Res 85:187–193 [DOI] [PMC free article] [PubMed]
- 55.Stuart K, Posner M, Campbell K, Huberman M (1995) Cisplatin and chronic oral etoposide as salvage therapy for advanced colorectal carcinoma. Am J Clin Oncol 18:300–302 [DOI] [PubMed]
- 56.Tsavaris N, Kosmas C, Gennatas K, Vadiaka M, Skopelitis E, Xila V, Rokana S, Margaris E, Zografos G, Papastratis G, Kouraklis G (2002) Etoposide, leucovorin (LV) and 5-fluorouracil (5-FU) in 5-FU + LV pre-treated patients with advanced colorectal cancer. J Chemother 14:406–411 [DOI] [PubMed]
- 57.Tsavaris N, Kosmas C, Gennatas K, Vadiaka M, Paliaros P, Dimitrakopoulos A, Diamantis T, Tsipras H, Papastratis G (2002) Etoposide added to weekly leucovorin (LV)/5-fluorouracil (5-FU) in LV/5-FU pre-treated patients with advanced colorectal cancer. Med Sci Monit 8:65–69 [PubMed]