Abstract
Prevalence rates reported for malaria in pregnancy in Nigeria vary considerably. The accuracy of results of malaria diagnosis is dependent on training, experience, and motivation of the microscopist as well as the laboratory facility available. Results of training programmes on malaria microscopy have shown low levels of sensitivity and specificity of those involved in malaria diagnosis routinely and for research. This study was done to ascertain the true prevalence of malaria in pregnancy in Lagos, South-West Nigeria. A total of 1,084 pregnant women were recruited into this study. Blood smears stained with Giemsa were used for malaria diagnosis by light microscopy. Malaria infection during pregnancy presents mostly as asymptomatic infection. The prevalence of malaria in this population was 7.7% (95% confidence interval; 6.2-9.4%). Factors identified to increase the risk of malaria infection include young maternal age (< 20 years), and gravidity (primigravida). In conclusion, this study exposes the over-diagnosis of malaria in pregnancy and the need for training and retraining of laboratory staffs as well as establishing the malaria diagnosis quality assurance programme to ensure the accuracy of malaria microscopy results at all levels.
Keywords: malaria, diagnosis, prevalence rate, pregnancy, Nigeria
Malaria control still remains a challenge in Africa where 45 countries, including Nigeria, are endemic for malaria, and about 588 million people are at risk [1]. The protection of pregnant women living in malaria-endemic countries has been of particular interest to many National Malaria Control Programmes because of their reduced immunity. Most cases of malaria in pregnancy in areas of stable malaria transmission are asymptomatic [2,3]. This is attributed to anti-disease immunity acquired during previous exposures which protects against clinical malaria [4]. Unfortunately, this subclinical infection still poses great danger to both the mother and the fetus. The principal impact of malaria infection is due to the presence of parasites in the placenta causing maternal anemia (potentially responsible for maternal death when severe) and low birth weight (LBW) [5,6].
The recent World Malaria Report, which indicated that Nigeria accounts for a quarter of all malaria cases in the 45 malaria-endemic countries in Africa, clearly showed the challenge of malaria in Nigeria [1]. This may be due to the large population, approximately 140 million people [7] living in areas of high malaria transmission. In Nigeria, 11% of maternal deaths are attributed to malaria [8]. To further buttress the worrisome malaria picture, many researchers have reported high prevalence rates of malaria in pregnancy in different parts of Nigeria, ranging from 19.7% to 72.0% [9-12]. Thus, pregnant women, who are known to be one of the groups at high risk of the effects of malaria infection, need special protective measures to ensure their survival and improve birth outcome. However, these reports create the impression that the efforts to control malaria by the Government and other agencies like the Roll Back Malaria programme, WHO, UNICEF, and many other non-governmental agencies might not be effective. While there are reports of up to 50% reduction in malaria episodes and deaths in some African countries between 2000 and 2006 [1], reports from Nigeria has not shown significant reduction, especially with regards to malaria in pregnancy. The reasons adduced for the change in malaria prevalence in other countries are good surveillance and high intervention coverage [1].
Generally, the method employed in any diagnosis is an important criterion in reporting valid results. In this case, the accuracy of malaria microscopy is determined by factors such as training and re-training, experience, motivation, and laboratory facilities [13-15]. These factors work synergistically to ensure that the sensitivity and specificity of the microscopist is sufficiently high to guarantee accurate malaria microscopy results. Interestingly, these factors are more imperative in settings where there are no existing malaria microscopy quality assurance programmes.
Considering the wide variation in reports of the prevalence of malaria in pregnancy in Nigeria, it became imperative for a closer assessment of the malaria prevalence among pregnant women in Lagos, South-West Nigeria. Standard malaria microscopy procedures were employed following pre-qualification of our microscopists before the study to ensure accuracy of results.
A total of 1,084 pregnant women who attended the antenatal clinics of Ajeromi General Hospital and St. Kizito Primary Health Center in Lagos, Nigeria, who gave informed consent to participate in the study were recruited at booking between March 2007 and February 2008. Ethical approval for this study was obtained from the Ethics Committee of the College of Medicine of the University of Lagos and Lagos University Teaching Hospital, Lagos, Nigeria. Lagos is an area of stable malaria transmission. Brief demographic information of the pregnant women was collected using a structured questionnaire. Venipuncture was done to collect blood samples for malaria diagnosis by microscopy and for a total leucocyte count.
Thin and thick blood films were prepared immediately upon blood collection on the same slide. For thick films, 12 µl of blood was spread over a diameter of 15 mm, while 2 µl of blood was used for thin films. The slides were made in duplicates (one to be read, and the other archived as part of our quality assurance process) and labeled appropriately. The thin film was fixed in absolute methanol for 1-2 sec and air dried. The blood films were stained after 24-48 hr with 3% Giemsa stain solution at pH 7.2. The stained slides were read by 2 competent independent microscopists, Reader 1 and Reader 2. In determining the parasite density, the number of malaria parasites (parasite count) and leukocytes were counted per high power field. The absolute parasite density was calculated using the formula below:
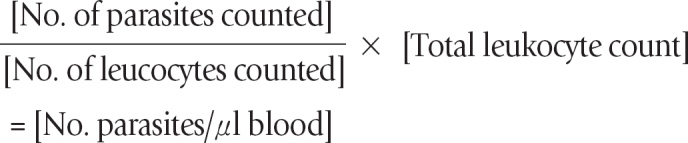
A definitive diagnosis of malaria was made when a reddish chromatin dot with a purple or blue cytoplasm of the malaria parasites are seen together. A slide was pronounced negative when 100 high power fields have been examined using ×100 oil immersion objective lens.
Any discrepant (discordance) result in terms of the presence of parasites is re-read by a more experienced microscopist (Reader 3). The discrepant microscopy result is resolved by calculating the percentage discrepancy. The percentage discrepancy was determined using the formula:
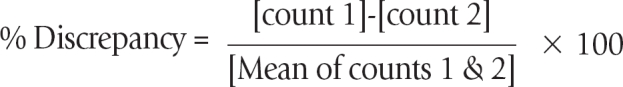
For parasite counts with % discrepancy less than 20%, the count is accepted and the mean parasite count was taken as the parasite density. For parasite counts with % discrepancy ≥ 20%, the films were examined by Reader 3. The count by Reader 3 and the closest from either Reader 1 or Reader 2 were used to calculate the % discrepancy, and their mean count was taken as parasite density provided the % discrepancy is < 20%. Alternatively, the slides were re-read by Reader 1 and Reader 2. The total leukocyte count determination for each participant was done using the improved Neubauer chamber as described by Baker and Silverton [16].
The data were analyzed using EPI INFO 2002 statistical software (CDC, Atlanta, Georgia, USA). Tests for associations and differences were done by chi-square analysis. Statistical significance was set at P value < 0.05.
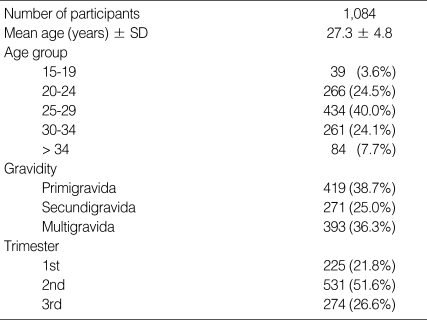
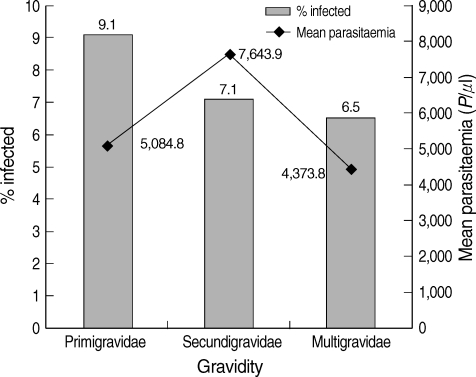
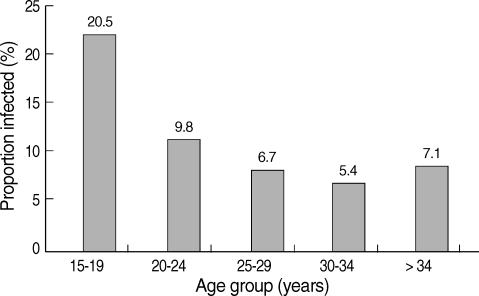
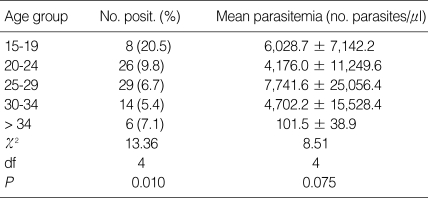
A total of 1,084 pregnant women participated in the study. Their mean age ± SD was 27.4 ± 4.8 year. Of these, 572 (49.8%) were in the second trimester of pregnancy. The pregnant women with secondary education were 42.0%. The characteristics of the participants are shown in Table 1. Positive malaria slides were recorded in 83 pregnant women thus giving a malaria prevalence rate of 7.7% (95% confidence interval; 6.2-9.4%). The parasite density (mean and SD) among the infected pregnant women was 5,420 ± 17,522 parasites/µl. There was a reduction (though not significant, χ2 = 2.06; degree of freedom [df] = 2; P = 0.357) in the proportion of those with malaria infection as gravidity increased, with the primigravidae having the highest, 9.1% (Fig. 1). This association between the age of the pregnant women and proportion of those infected was significant (χ2 = 13.36; df = 4; P = 0.010). The 15-19 year age group had the highest rate of infection (20.5%) (Fig. 2). There was, however, no significant difference (χ2 = 8.51; df = 4; P = 0.075) in the mean parasitemia of the various age groups (Table 2).
Table 1.
Characteristics of the pregnant women who participated in the study
Fig. 1.
Comparison of mean parasitaemia and proportion of infected pregnant women by gravidity.
Fig. 2.
Relationship between malaria infection and age of pregnant women.
Table 2.
Comparison of mean parasitemia
Until now, the reports of the prevalence of malaria in pregnancy were variable and high, especially in the South-West Nigeria where prevalence rates of between 36.5% and 72% [2,9,11] have been reported. These reports contrast sharply with our findings in this same region with a prevalence rate of 7.7% among pregnant women attending antenatal clinics for the first time during current pregnancy.
The differences in the reported prevalence rates of malaria may be attributed to the skill and experience of the laboratory personnel involved in blood film preparation, staining, and reading of the slides. In our study, we ensured that the sensitivity and specificity of our microscopists were above 90% through frequent training and the institution of a malaria microscopy quality assurance programme. Strict adherence to procedures for slide preparation and staining [17] ensured the production of clear, well stained slides, thereby reducing errors due to artefacts. The inaccurate diagnosis of malaria is not peculiar to Nigeria. In Tanzania, Mwanziva et al. [18] reported a very appalling case, where < 1% of the slides read by clinic microscopists as malaria positive were confirmed as positive by trained research scientists.
The consequences of over-reporting of malaria cases are: 1) Inability to properly assess the impact of malaria control programmes, as the baseline information before implementation may not be correct; 2) In clinical settings, there will be unnecessary treatments with antimalarial drugs for febrile cases that may not be due to malaria, thereby, increasing the chances of the emergence of antimalarial drug resistance and wastage; 3) National and world malaria statistics based on inaccurate data could misrepresent the actual reality on ground.
Our current results call for a total re-assessment of existing malaria prevalence data. This can only be achieved prospectively after pre-qualifying the microscopists. Our results showed that primigravidas (8.5%) were more often infected than women of other gravidities (Fig. 1). Primigravidas have been reported to be at a greatest risk of malaria in pregnancy because they lack the specific immunity to placental malaria which is acquired from exposure to malaria parasites during pregnancy [4,19]. This immunity accumulates with successive pregnancies, provided there is exposure to malaria infection [20]. The similar malaria prevalence rates in secundigravidas and multigravidas seen in this study suggest that there is no difference in the level of specific immunity to placental malaria and in line with existing data [20]. When this is considered, the reported high prevalence rates of malaria in pregnant women [9-12] seem to nullify the usefulness of this acquired immunity which has been shown to be able to prevent placental malaria by blocking parasite adhesion to placental circumsporozoite antigen (CSA) and opsonize malaria-infected erythrocytes for interaction with Fc receptors on phagocytic cells [19].
In this study, the highest malaria prevalence was seen in pregnant women < 20 year (20.5%) (Fig. 2). This finding is consistent with earlier reports [21,22] where age group of < 24 year was reported to be at a high risk. To stem this trend, awareness on malaria prevention measures during pregnancy should target young women even before they get married preferably at schools, and religious and social gatherings. Our results showed that malaria prevalence decreased with increasing age but increased in age group > 34 year. Marielle et al. [23] reported a high prevalence of malaria in pregnant women within a similar age group (36-39 year) in Gabon.
As our study has shown the over-reporting in the prevalence of malaria in pregnancy, there is need to ensure that competent microscopists whose levels of sensitivity and specificity are critical in settings where laboratory-based confirmation of clinically suspected malarial fever is done. There is, therefore, a need for the institution of a malaria quality assurance programme in laboratories involved in malaria diagnosis.
References
- 1.World Health Organization. World Malaria Report 2008. Switzerland: World Health Organization; 2008. pp. 99–101. [Google Scholar]
- 2.Anorlu RI, Odum CU, Essien EE. Asymptomatic malaria parasitaemia in pregnant women at booking in a primary health care facility in a periurban community in Lagos, Nigeria. Afr J Med Med Sci. 2001;30:39–41. [PubMed] [Google Scholar]
- 3.Mockenhaupt FP, Ulmen U, von Gaertner C, Bedu-Addo G, Bienzle U. Diagnosis of placental malaria. J Clin Microbiol. 2002;40:306–308. doi: 10.1128/JCM.40.1.306-308.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Staalsoe T, Shulman CE, Buhner JN, Kawuondo K, Marsh K, Hviid L. Variant surface antigen-specific IgG and protection against clinical consequences of pregnancy-associated Plasmodium falciparum malaria. Lancet. 2004;363:283–289. doi: 10.1016/S0140-6736(03)15386-X. [DOI] [PubMed] [Google Scholar]
- 5.Newman RD, Hailemariam A, Jimma D, Degifie A, Kebede D, Rietveld AE, Nahlen BL, Barnwell JW, Steketee RW, Parise ME. Burden of malaria during pregnancy in areas of stable and unstable transmission in Ethiopia during a nonepidemic year. J Infect Dis. 2003;187:1765–1772. doi: 10.1086/374878. [DOI] [PubMed] [Google Scholar]
- 6.Rogerson SJ, Boeuf P. New approaches to malaria in pregnancy. Parasitology. 2007;134:1883–1893. doi: 10.1017/S003118200700011X. [DOI] [PubMed] [Google Scholar]
- 7.2006 National Census. National Beaureau of Statistics. http://www.nigerianstat.gov.ng/Connections/Pop2006.pdf.
- 8.Federal Ministry of Health. Malaria situation analysis document. Nigeria: Federal Ministry of Health; 2000. p. 14. [Google Scholar]
- 9.Okwa OO. The status of malaria among pregnant women: a study in Lagos, Nigeria. Afr J Reprod Health. 2003;7:77–83. [PubMed] [Google Scholar]
- 10.Kagu MB, Kawuwa MB, Gadzama GB. Anaemia in pregnancy: a cross-sectional study of pregnant women in a Sahelian tertiary hospital in Northeastern Nigeria. J Obstet Gynecol. 2007;27:676–679. doi: 10.1080/01443610701612144. [DOI] [PubMed] [Google Scholar]
- 11.Adefioye OA, Adeyeba OA, Hassan WO, Oyeniran OA. Prevalence of malaria parasite infection among pregnant women in Osogbo, southwest, Nigeria. American-Eurasian J Sci Res. 2007;2:43–45. [Google Scholar]
- 12.Uneke CJ. Assessment of malaria in pregnancy using rapid diagnostic tests and its association with HIV infection and haematologic parameters in south-eastern Nigeria. Haematologica. 2008;93:143–144. doi: 10.3324/haematol.11695. [DOI] [PubMed] [Google Scholar]
- 13.Bates I, Bekoe V, Asamoa-Adu A. Improving the accuracy of malaria-related laboratory tests in Ghana. Malar J. 2004;3:38. doi: 10.1186/1475-2875-3-38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Prudhomme O'Meara W, Barcus M, Wongsrichanalai C, Muth S, Maguire J, Jordan R, Prescott WR, McKenzie FE. Reader technique as a source of variability in determining malaria parasite density by microscopy. Malar J. 2006;5:118. doi: 10.1186/1475-2875-5-118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ohrt C, Obare P, Nanakorn A, Adhiambo C, Awuondo K, Prudhomme O'Meara W, Remich S, Martin K, Cook E, Chretien JP, Lucas C, Osoga J, McEvoy P, Owaga ML, Odera JS, Ogutu B. Establishing a malaria diagnostic center of excellence in Kisumu, Kenya. Malar J. 2007;6:79. doi: 10.1186/1475-2875-6-79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Baker FJ, Silverton RE. Introduction to Medical Laboratory Technology. 6th ed. London, UK: Butterworths; 1985. The full blood count; pp. 320–323. [Google Scholar]
- 17.World Health Organization. Basic laboratory methods in medical parasitology. Geneva, Switzerland: World Health Organization; 1991. p. 114. [Google Scholar]
- 18.Mwanziva C, Shekalaghe S, Ndaro A, Mengerink B, Megiroo S, Mosha F, Sauerwein R, Drakeley C, Gosling R, Bousema T. Overuse of artemisinin-combination therapy in Mto wa Mbu (river of mosquitoes), an area misinterpreted as high endemic for malaria. Malar J. 2008;7:232. doi: 10.1186/1475-2875-7-232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Elliott SR, Brennan AK, Beeson JG, Tadesse E, Molyneux ME, Brown GV, Rogerson SJ. Placental malaria induces variant-specific antibodies of the cytophilic subtypes immunoglobulin G1 (IgG1) and IgG3 that correlate with adhesion inhibitory activity. Infect Immun. 2005;73:5903–5907. doi: 10.1128/IAI.73.9.5903-5907.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Beeson JG, Duffy PE. The immunology and pathogenesis of malaria during pregnancy. Curr Top Microbiol Immunol. 2005;297:187–227. doi: 10.1007/3-540-29967-x_6. [DOI] [PubMed] [Google Scholar]
- 21.Bouyou-Akotet MK, Ionete-Collard DE, Mabika-Manfoumbi M, Kendjo E, Matsiegui PB, Mavoungou E, Kombila M. Prevalence of Plasmodium falciparum in pregnant women in Gabon. Malar J. 2003;2:18. doi: 10.1186/1475-2875-2-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Tako EA, Zhou A, Lohoue J, Leke R, Taylor DW, Leke RFG. Risk factor for placental malaria and its effect on pregnancy outcome in Yaounde, Cameroon. Am J Trop Med Hyg. 2005;72:236–242. [PubMed] [Google Scholar]
- 23.Marielle KBA, Denisa EIC, Modeste MM, Eric K, Pierre BM, Elie M, Maryvome K. Prevalence of Plasmodium falciparum Infection in pregnant women in Gabon. Malar J. 2003;2:1–17. doi: 10.1186/1475-2875-2-18. [DOI] [PMC free article] [PubMed] [Google Scholar]