Abstract
CYP27B1, encoding 25-hydroxyvitamin D-1α-hydroxylase, converts 25-hydroxyvitamin D to its active form, 1,25-dihydroxyvitamin D, and is expressed primarily in the kidney but also in nontraditional sites including the parathyroid glands. Whereas the role of locally produced 1,25-dihydroxyvitamin D is not yet clear, it is possible that it contributes importantly to vitamin D–mediated inhibition of parathyroid cell growth, so CYP27B1 can be considered a candidate parathyroid tumor suppressor gene in that its acquired inactivation in a parathyroid cell could confer a tumorigenic growth advantage. Expression of CYP27B1 has also been reported to be altered in parathyroid neoplasms. Because detection of inactivating mutations is the central criterion for validating a candidate tumor suppressor, we directly sequenced the coding region and all splice sites of CYP27B1 in 31 sporadic parathyroid adenomas and 31 parathyroid tumors from patients with refractory secondary/tertiary hyperparathyroidism. No nonsense, frameshift, or other inactivating mutations were found, and there was no sign of homozygous deletion. Our findings indicate that CYP27B1 does not commonly serve as a classical tumor suppressor gene in the development of sporadic parathyroid adenomas or of refractory secondary/tertiary hyperparathyroidism.
Key words: parathyroid, vitamin D, PTH
INTRODUCTION
25-hydroxyvitamin D-1α-hydroxylase [1α-(OH)ase], a mitochondrial cytochrome P450 enzyme encoded by CYP27B1, is responsible for the conversion of 25-hydroxyvitamin D to 1,25-dihydroxyvitamin D [1,25(OH)2D3], which is the active form of the vitamin. 1,25(OH)2D3 has a multitude of actions, among them increasing calcium absorption in the intestine and, in the parathyroid glands, inhibiting PTH gene transcription, PTH secretion, and parathyroid cell growth.(1,2)
Mutations in CYP27B1 are responsible for the autosomal recessive disease in humans termed vitamin D–dependent rickets type I (VDDR I) or pseudovitamin D deficiency rickets (PDDR). Affected individuals develop rickets and osteomalacia, as well as secondary hyperparathyroidism, growth retardation, hypotonia, and abnormal mineral homeostasis.(3,4) The phenotype is reflected by a mouse knockout model of CYP27B1.(5,6)
The primary site of CYP27B1 expression is the proximal tubule of the kidney(7); however, the enzyme is also expressed in various extrarenal sites, including the parathyroid glands,(8) colon, and pancreas.(9) Because 1α-(OH)ase is expressed in the parathyroids, it is possible that local 1α-hydroxylation is responsible for a significant proportion of the total effect of 1,25(OH)2D3 on the parathyroid gland. This local production may be especially important in patients with chronic renal failure, because of their diminished ability to produce 1,25(OH)2D3 in the kidneys and their low circulating 1,25(OH)2D3 levels. That said, the role of locally active 1α-hydroxylation in the parathyroids remains uncertain, and the important possibility that its acquired loss could cause a clonal selective advantage is not directly spoken to by the hyperparathyroid phenotype in humans and mice with germline inactivation of the 1α-(OH)ase gene.
Monoclonality is a central feature of sporadic primary adenomas,(10) as well as the majority of parathyroid glands removed because of severe refractory secondary/tertiary hyperparathyroidism,(11) indicating that these tumors developed from a single cell with a selective growth advantage. Tumor suppressor genes are defined as those in which inactivating mutations contribute to tumorigenesis,(12) with MEN1 and HRPT2 being two such genes already implicated in parathyroid neoplasia.(13,14) Whereas many tumor suppressors have normal functions in processes like cell cycle control or signaling, a wide variety of tumor suppressor functions exists.(15) Given the antiproliferative properties of 1,25(OH)2D3 in the parathyroid and reported abnormalities in its expression, a crucial question is whether acquired inactivation of CYP27B1 is a primary driving contributor to clonal parathyroid growth, serving as a classic tumor suppressor gene. Segersten et al.(8) found the majority of parathyroid adenomas to have strong but somewhat variable and irregular immunohistochemical staining for the 1α-(OH)ase enzyme, whereas a subset of parathyroid adenomas had weak staining. These patterns are consistent with the possibility that CYP27B1 acts as a tumor suppressor gene in adenomas, because one would generally expect that a subset of tumors would result from inactivation of a specific tumor suppressor, with some of these showing decreased protein levels. Glands from patients with renal failure had irregular strong staining, but the intensity was notably less in areas of nodular (often monoclonal) growth, potentially consistent with an even higher prevalence of CYP27B1 inactivation. However, despite the intriguing nature of these expression patterns, they could reflect secondary changes or epiphenomena, and mutational analyses are therefore crucial in definitively addressing CYP27B1’s candidacy.(12) We analyzed CYP27B1 for inactivating mutations by direct sequencing in sporadic parathyroid adenomas and also in parathyroid tumors from patients with severe refractory secondary/tertiary hyperparathyroidism.
MATERIALS AND METHODS
Patients and samples
We studied 31 sporadic parathyroid adenomas and 31 parathyroid tumors from patients with chronic kidney disease (CKD) and refractory secondary or tertiary hyperparathyroidism. All parathyroid adenomas were typical examples of single gland disease, both clinically and histologically. Criteria for parathyroidectomy in CKD patients were as previously described,(11,16) based on development of hypercalcemia and/or symptoms resistant to standard medical therapy, and are known to yield a high prevalence of monoclonal parathyroid neoplasia. All tissue specimens were obtained in accordance with institutional review board–approved protocols for human studies.
Parathyroid specimens were frozen in liquid nitrogen after surgical removal and stored at −80°C. High molecular weight genomic DNA was extracted from frozen tissue using standard procedures including proteinase K digestion, phenol-chloroform extraction, and ethanol precipitation.
CYP27B1 sequencing
The entire nine exon coding region and splice sites of CYP27B1 were amplified by PCR (Fig. 1), using published primer sequences.(3) Primers were optimized at an annealing temperature of 55°C, with the exception of primers for exon 6, which had an annealing temperature of 59°C. PCR reactions were performed in 20-μl reaction volumes containing 25 ng genomic DNA, 20 pmol of each primer, 200 μM of each dNTP, 2 mM magnesium chloride, and 1.25 U of Amplitaq Gold DNA Polymerase (Applied Biosystems, Foster City, CA, USA). Each PCR reaction was performed in conjunction with a negative control that did not contain any template DNA; such control reactions were uniformly and appropriately negative. The thermocycling conditions included an initial denaturation step of 95°C for 10 min; 35 cycles of 95°C for 30 s, the optimized Ta for 30 s, and 72°C for 30 s; and a final extension step at 72°C for 10 min. PCR products were purified and sequenced using standard methods on ABI3730xl instruments (Agencourt Bioscience). Sequence data were analyzed with Sequencher software (GeneCodes, Ann Arbor, MI, USA) and compared with the reference sequence (RefSeq ID: NM_000785).
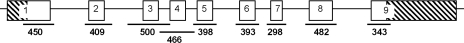
FIG. 1.
Schematic diagram of CYP27B1 with PCR amplification and sequencing strategy. All nine exons are shown as boxes: protein coding, open; 5` and 3` UTRs, hatched. PCR products are shown below, with their corresponding size in base pairs.
RESULTS
We analyzed 31 sporadic parathyroid adenomas and 31 parathyroid tumors from patients with severe secondary or tertiary hyperparathyroidism by direct sequencing for intragenic mutations of the CYP27B1 gene. We sequenced all coding regions and splice sites in a search for clonal inactivating mutations. No point mutations, deletions, or insertions were uncovered in any of the 62 samples studied. All exons of each sample were able to be amplified by PCR, providing evidence against homozygous deletion. Furthermore, in a prior report from our group, loss of heterozygosity, a common mechanism for tumor suppressor activation, was present at chromosome 12q, the location of CYP27B1, in only 1 of the 29 examined adenomas and in none of the secondary hyperparathyroid tumors,(16,17) thus reinforcing our current observations.
DISCUSSION
The active form of vitamin D, 1,25(OH)2D3, has a crucial function in the parathyroid glands, where it decreases PTH gene expression and secretion and parathyroid cell growth. Local expression of 1α-(OH)ase in the parathyroid glands may be required to achieve adequate levels of the hormone to suppress cell growth. Thus, CYP27B1 is an important candidate tumor suppressor gene that could acquire loss of function mutations specifically in the parathyroid cell genome, leading to a selective advantage and tumor development. Our approach was designed to rigorously test the possibility that CYP27B1 serves as a classic tumor suppressor in the parathyroids. Only recurrent inactivating mutations can provide this critical evidence for a primary driving role,(15) because gene expression changes can reflect secondary phenomena not necessarily involved in tumorigenesis. Therefore, we explored the mutational status of this gene and found no mutations in any of the 62 tumors studied. Whereas our approach does not exclude the possibility of epigenetic changes or mutations in the unsequenced regions like introns, the promoter region, or the untranslated regions (UTRs), it would be unprecedented if inactivating alterations in an authentic tumor suppressor gene were to be found exclusively in these regions without ever appearing in the coding region.
These observations complement previous study of the vitamin D system in this context. The vitamin D receptor gene (VDR) was sequenced in sporadic parathyroid adenomas and in parathyroids from patients with severe hyperparathyroidism of uremia, and it was found that clonal mutations in VDR occur rarely, if at all, in these tumors.(18,19) However, it remains possible that influences on local production of 1,25(OH)2D3 could still contribute to parathyroid tumorigenesis in a less direct fashion,(20,21) but our observations make a direct driving role very unlikely.
In summary, our observations strongly suggest that CYP27B1 acts infrequently, if at all, as a classical tumor suppressor gene in the molecular pathogenesis of parathyroid adenomas or refractory secondary/tertiary hyperparathyroidism.
ACKNOWLEDGMENTS
The authors thank Kristin Corrado for expert technical assistance. This work was supported in part by the Medical Scientist Training Program T32-GM008607 from the National Institutes of Health, National Research Service Award F30 DK081270-01 from the National Institutes of Health, the Student Scholar Grant from the American Society of Nephrology, and by the Murray-Heilig Fund in Molecular Medicine.
Footnotes
The authors state that they have no conflicts of interest.
REFERENCES
- 1.Silver J, Levi R. Regulation of PTH synthesis and secretion relevant to the management of secondary hyperparathyroidism in chronic kidney disease. Kidney Int. 2005;67(Suppl 95):S8–S12. doi: 10.1111/j.1523-1755.2005.09501.x. [DOI] [PubMed] [Google Scholar]
- 2.Silver J, Naveh-Many T, Mayer H, Schmelzer HJ, Popovtzer MM. Regulation by vitamin D metabolites of parathyroid hormone gene transcription in vivo in the rat. J Clin Invest. 1986;78:1296–1301. doi: 10.1172/JCI112714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kim CJ, Kaplan LE, Perwad F, Huang N, Sharma A, Choi Y, Miller WL, Portale AA. Vitamin D 1alpha-hydroxylase gene mutations in patients with 1alpha-hydroxylase deficiency. J Clin Endocrinol Metab. 2007;92:3177–3182. doi: 10.1210/jc.2006-2664. [DOI] [PubMed] [Google Scholar]
- 4.St-Arnaud R, Messerlian S, Moir JM, Omdahl JL, Glorieux FH. The 25-hydroxyvitamin D 1-alpha-hydroxylase gene maps to the pseudovitamin D-deficiency rickets (PDDR) disease locus. J Bone Miner Res. 1997;12:1552–1559. doi: 10.1359/jbmr.1997.12.10.1552. [DOI] [PubMed] [Google Scholar]
- 5.Panda DK, Miao D, Tremblay ML, Sirois J, Farookhi R, Hendy GN, Goltzman D. Targeted ablation of the 25-hydroxyvitamin D 1alpha-hydroxylase enzyme: Evidence for skeletal, reproductive, and immune dysfunction. Proc Natl Acad Sci USA. 2001;98:7498–7503. doi: 10.1073/pnas.131029498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dardenne O, Prud'homme J, Glorieux FH, St-Arnaud R. Rescue of the phenotype of CYP27B1 (1alpha-hydroxylase)-deficient mice. J Steroid Biochem Mol Biol. 2004;89–90:327–330. doi: 10.1016/j.jsbmb.2004.03.026. [DOI] [PubMed] [Google Scholar]
- 7.Zehnder D, Bland R, Walker EA, Bradwell AR, Howie AJ, Hewison M, Stewart PM. Expression of 25-hydroxyvitamin D3-1alpha-hydroxylase in the human kidney. J Am Soc Nephrol. 1999;10:2465–2473. doi: 10.1681/ASN.V10122465. [DOI] [PubMed] [Google Scholar]
- 8.Segersten U, Correa P, Hewison M, Hellman P, Dralle H, Carling T, Akerstrom G, Westin G. 25-hydroxyvitamin D(3)-1alpha-hydroxylase expression in normal and pathological parathyroid glands. J Clin Endocrinol Metab. 2002;87:2967–2972. doi: 10.1210/jcem.87.6.8604. [DOI] [PubMed] [Google Scholar]
- 9.Zehnder D, Bland R, Williams MC, McNinch RW, Howie AJ, Stewart PM, Hewison M. Extrarenal expression of 25-hydroxyvitamin d(3)-1 alpha-hydroxylase. J Clin Endocrinol Metab. 2001;86:888–894. doi: 10.1210/jcem.86.2.7220. [DOI] [PubMed] [Google Scholar]
- 10.Arnold A, Staunton CE, Kim HG, Gaz RD, Kronenberg HM. Monoclonality and abnormal parathyroid hormone genes in parathyroid adenomas. N Engl J Med. 1988;318:658–662. doi: 10.1056/NEJM198803173181102. [DOI] [PubMed] [Google Scholar]
- 11.Arnold A, Brown MF, Urena P, Gaz RD, Sarfati E, Drueke TB. Monoclonality of parathyroid tumors in chronic renal failure and in primary parathyroid hyperplasia. J Clin Invest. 1995;95:2047–2053. doi: 10.1172/JCI117890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Haber D, Harlow E. Tumour-suppressor genes: Evolving definitions in the genomic age. Nat Genet. 1997;16:320–322. doi: 10.1038/ng0897-320. [DOI] [PubMed] [Google Scholar]
- 13.Heppner C, Kester MB, Agarwal SK, Debelenko LV, Emmert-Buck MR, Guru SC, Manickam P, Olufemi SE, Skarulis MC, Doppman JL, Alexander RH, Kim YS, Saggar SK, Lubensky IA, Zhuang Z, Liotta LA, Chandrasekharappa SC, Collins FS, Spiegel AM, Burns AL, Marx SJ. Somatic mutation of the MEN1 gene in parathyroid tumours. Nat Genet. 1997;16:375–378. doi: 10.1038/ng0897-375. [DOI] [PubMed] [Google Scholar]
- 14.Carpten JD, Robbins CM, Villablanca A, Forsberg L, Presciuttini S, Bailey-Wilson J, Simonds WF, Gillanders EM, Kennedy AM, Chen JD, Agarwal SK, Sood R, Jones MP, Moses TY, Haven C, Petillo D, Leotlela PD, Harding B, Cameron D, Pannett AA, Hoog A, Heath H, III, James-Newton LA, Robinson B, Zarbo RJ, Cavaco BM, Wassif W, Perrier ND, Rosen IB, Kristoffersson U, Turnpenny PD, Farnebo LO, Besser GM, Jackson CE, Morreau H, Trent JM, Thakker RV, Marx SJ, Teh BT, Larsson C, Hobbs MR. HRPT2, encoding parafibromin, is mutated in hyperparathyroidism-jaw tumor syndrome. Nat Genet. 2002;32:676–680. doi: 10.1038/ng1048. [DOI] [PubMed] [Google Scholar]
- 15.Fearon E. Tumor suppressor genes. In: Vogelstein B, Kinzler KW, editors. The Genetic Basis of Human Cancer. 2nd ed. vol. 6. New York, NY, USA: McGraw Hill; 1999. pp. 233–234. [Google Scholar]
- 16.Imanishi Y, Tahara H, Palanisamy N, Spitalny S, Salusky IB, Goodman W, Brandi ML, Drueke TB, Sarfati E, Urena P, Chaganti RS, Arnold A. Clonal chromosomal defects in the molecular pathogenesis of refractory hyperparathyroidism of uremia. J Am Soc Nephrol. 2002;13:1490–1498. doi: 10.1097/01.asn.0000018148.50109.c0. [DOI] [PubMed] [Google Scholar]
- 17.Palanisamy N, Imanishi Y, Rao PH, Tahara H, Chaganti RS, Arnold A. Novel chromosomal abnormalities identified by comparative genomic hybridization in parathyroid adenomas. J Clin Endocrinol Metab. 1998;83:1766–1770. doi: 10.1210/jcem.83.5.4806. [DOI] [PubMed] [Google Scholar]
- 18.Brown SB, Brierley TT, Palanisamy N, Salusky IB, Goodman W, Brandi ML, Drueke TB, Sarfati E, Urena P, Chaganti RS, Pike JW, Arnold A. Vitamin D receptor as a candidate tumor-suppressor gene in severe hyperparathyroidism of uremia. J Clin Endocrinol Metab. 2000;85:868–872. doi: 10.1210/jcem.85.2.6426. [DOI] [PubMed] [Google Scholar]
- 19.Samander EH, Arnold A. Mutational analysis of the vitamin D receptor does not support its candidacy as a tumor suppressor gene in parathyroid adenomas. J Clin Endocrinol Metab. 2006;91:5019–5021. doi: 10.1210/jc.2006-1543. [DOI] [PubMed] [Google Scholar]
- 20.Perwad F, Zhang MY, Tenenhouse HS, Portale AA. Fibroblast growth factor 23 impairs phosphorus and vitamin D metabolism in vivo and suppresses 25-hydroxyvitamin D-1alpha-hydroxylase expression in vitro. Am J Physiol Renal Physiol. 2007;293:F1577–F1583. doi: 10.1152/ajprenal.00463.2006. [DOI] [PubMed] [Google Scholar]
- 21.Usatii M, Rousseau L, Demers C, Petit JL, Brossard JH, Gascon-Barre M, Lavigne JR, Zahradnik RJ, Nemeth EF, D'Amour P. Parathyroid hormone fragments inhibit active hormone and hypocalcemia-induced 1,25(OH)2D synthesis. Kidney Int. 2007;72:1330–1335. doi: 10.1038/sj.ki.5002532. [DOI] [PubMed] [Google Scholar]