Abstract
BACKGROUND:
Stress-induced cardiomyopathy is usually associated with an increased level of cardiac enzymes, leading to difficulties in differentiating this condition from acute coronary syndrome. The final diagnosis is usually made based on angiographic findings revealing normal coronary arteries. It was hypothesized that maximal cardiac enzyme elevation in these patients should have an upper limit. In the present study, reported cases of stress cardiomyopathy were compared with documented cardiac enzyme levels to evaluate the upper cut-off point of troponin in this population.
METHOD:
All of the articles published in PubMed and MEDLINE from November 2007 to July 2008, on takotsubo or stress-induced cardiomyopathy, were identified. Only the cases that reported the absolute or mean level of cardiac enzymes were included. The level of various enzymes were correlated with cardiac function, and the upper limit of enzyme elevation was calculated in these patients.
RESULTS:
A total of 114 patients (mean [± SD] age 63.5±14.5 years) were included in the study. Seventy-one per cent of the patients were older than 50 years of age and 86% were female. Mean values for troponin I, troponin T, creatine kinase (CK) and CK-MB were 6.5 ng/mL, 3.6 ng/mL, 556 U/L and 32.9 U/L, respectively. All of the patients with takotsubo cardiomyopathy had a troponin T level of 6 ng/mL or less and troponin I level of 15 ng/mL or less. Troponin T showed a significant inverse correlation with initial ejection fraction (R2=0.6), which was not seen with the levels of troponin I, CK and CK-MB. Takotsubo cardiomyopathy was classified as classic (66.7%), mid-cavitary (10%), reverse (23.3%) or local (0%).
CONCLUSION:
Among patients with takotsubo cardiomyopathy, troponin T level correlated with initial ejection fraction. Furthermore, the diagnosis of takotsubo cardiomyopathy appears to be unlikely in patients with troponin T greater than 6 ng/mL or troponin I greater than 15 ng/mL.
Keywords: Acute coronary syndrome, Cardiomyopathy, Correlation, Ejection fraction, Left ventricular ejection fraction, Myocardial infarction, Stress cardiomyopathy, Troponin I, Troponin T
Stress-induced (takotsubo) cardiomyopathy is a reversible cardiac syndrome characterized by acute onset of chest pain and classic wall motion abnormalities involving the apical region of the myocardium while sparing the base of the heart in the majority of cases. As the name suggests, it is usually triggered by physical or emotional stress, commonly among postmenopausal women. Stress-induced cardiomyopathy mimics symptoms of acute myocardial infarction with acute chest pain, electrocardiographic changes and a transient increase in the level of cardiac biomarkers including troponins. In 1991, Dote et al (1) first described this transient contractile dysfunction, naming it takotsubo cardiomyopathy because of its similarity with the Japanese octopus fishing pot. On left ventriculography, typical wall motion abnormalities – such as apical and mid-ventricular akinesia – and a hypercontractile base can be identified. Because stress-induced cardiomyopathy mimics acute coronary syndrome in its presentation with cardiac enzyme elevations and electrocardiogram changes, the diagnosis of this syndrome is based on exclusion of coronary disease. Due to the reversible nature of stress-induced cardiomyopathy and the normal appearance of the coronary arteries, we hypothesized that the level of cardiac enzymes should be lower in this syndrome than in patients with myocardial infarction and it should be possible to identify an upper cut-off point of cardiac enzyme elevation in these patients. To this purpose, we reviewed reported cardiac enzyme elevation in a large cohort of patients with stress-induced cardiomyopathy.
METHODS
A literature search of PubMed and MEDLINE for articles published from November 2007 to July 2008 was conducted using the terms “stress-induced cardiomyopathy” and “Tako-Tsubo cardiomyopathy”. All languages were searched, and studies that reported absolute or mean levels of cardiac enzymes were identified. Most of the patients were women, ranging in age from 20 to 90 years (mean [± SD] age 63.5±14.5 years). Most of these patients demonstrated the following features:
triggering event – either physical or emotional stress, in the majority it was emotional stress;
presentation – substernal chest discomfort, panic attack or breathlessness;
electrocardiogram changes – T wave inversion, ST elevation, ST depression and arrthymias;
echocardiography or ventriculography changes – differentiating into classic type, mid-cavitary type, reverse type or local type;
coronary angiogram – no significant atherosclerotic coronary artery stenosis; and
course of disease – normalization of systolic function with time.
The study initially had 220 patients, of which 106 were excluded because they did not report any absolute or mean cardiac enzyme levels. Thus, 114 patients were included in the final analysis. Based on echocardiographic and ventriculographic findings describing the anatomical location of the abnormality, stress cardiomyopathy was classified into four different types, previously described in the literature (2) as follows:
classic type: apical ballooning or takotsubo type and is the most commonly reported variety;
reverse type: hyperdynamic apex and akinesia of the base of the left ventricular wall (reverse takotsubo or reverse apical ballooning type). This type is rarely described in the literature (3–7);
mid-ventricular type: involves the mid left ventricular wall, sparing the base and the apex (8–10); and
local type: localized wall motion abnormality affecting a segment of the left ventricular wall, usually the anterior wall (5,11–14).
The absolute values of troponin T, troponin I, creatine kinase (CK) and CK-MB were collected, along with initial ejection fraction (EF) measured by echocardiogram, for 114 patients. Blood samples for troponin level were obtained within 24 h of admission.
Statistical analysis
The statstical program SPSS version 15 (SPSS Inc, USA) was used. The mean, maximum and minimum of reported cardiac enzyme elevations were calculated for the study patients. Furthermore, any correlation between various cardiac enzyme levels and reported EF at admission was evaluated using Pearson’s correlation. When appropriate, values were reported as mean ± SD.
RESULTS
A total of 114 patients were included in the final analysis. The mean age of the study population was 63.5±14.5 years (minimum age 18 years, maximum age 88 years), with a median age of 65 years. There were 98 women (87.5%) and 14 men (12.5%). Ninety-two patients (84.4%) were older than 50 years of age, 15 (13.3%) were between 40 and 50 years, and six (5.4%) were between 20 and 40 years. Measurements of cardiac enzymes were as follows:
troponin I: lowest level was 3 ng/mL, highest level was 13 ng/mL, mean level was 6.5 ng/mL;
troponin T: lowest level was 3 ng/mL, highest level was 7 ng/mL, mean level was 3.6 ng/mL;
CK: lowest level was 20 U/L, highest level was 3395 U/L, mean level was 556.1 U/L; and
CK-MB: lowest level was 2 U/L, highest level was 111 U/L, mean level was 32.9 U/L.
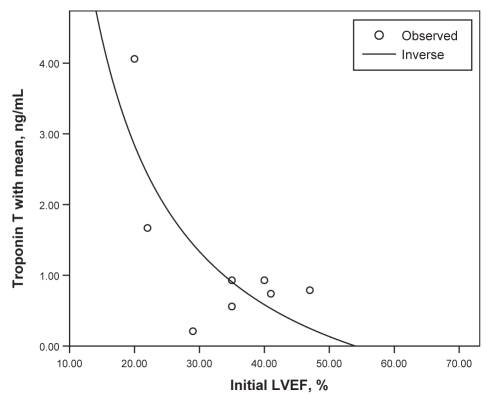
When the association between initial EF and cardiac enzymes was studied, there was no significant correlation for CK, CK-MB and troponin I. However, troponin T showed a significant inverse correlation with initial EF (R2=0.6; P=0.02) (Figure 1). The rates of presentation of the documented types of stress-induced cardiomyopathies are as follows: classic 66.7%, mid-cavitary 10%, reverse 23.3% and local 0%.
Figure 1).
Inverse relation between troponin T and intial left ventricular ejection fraction (LVEF)
DISCUSSION
Previous reports have shown that patients with stress-induced cardiomyopathy are mostly women in the postmenopausal period. Our study confirmed this by showing that 87.5% were female and 84.4% were over the age of 50 years in our sample. The pathogenesis of this disease is not known. Sex-related differences in the response of the adrenal medulla to sudden high-intensity sympathetic discharge, and differing pharmacokinetics of adrenaline release, could explain the increased rate in women (15).
Almost all patients with stress-induced cardiomyopathy and left ventricular impairment will recover within a few weeks. There are no data on frequency of patients with residual long-term left ventricular impairment (16). In our study, the most common presentation among the patients with stress-induced cardiomyopathy was chest pain, and all patients recovered from this event.
The patients with stress-induced cardiomyopathy have been shown to have increased levels of plasma catecholamines and stress-related neuropeptides. Unlike polymorphonuclear inflammation seen with infarction, in stress cardiomyopathy there is contraction band necrosis, a unique form of myocyte injury characterized by hypercontracted sarcomeres, dense eosinophilic transverse bands and an interstitial mononuclear inflammatory response (17). Cardiac biomarkers, namely troponins, CK and CK-MB, have been used for the diagnosis of myocardial infarction. It is usually difficult to distinguish between myocardial infarction secondary to coronary obstruction and stress-induced cardiomyopathy by the use of cardiac enzymes alone. However, based on our study, all patients with takotsubo cardiomyopathy had a troponin T level of 6 ng/mL or less and a troponin I level of 15 ng/mL or less. Therefore, the diagnosis of takotsubo cardiomyopathy appears to be unlikely in patients with troponin T level greater than 6 ng/mL or troponin I level greater than 15 ng/mL.
We found a direct correlation between EF and cardiac troponin T levels, but not with troponin I or CK. The cause of this association is not known. However, a similar correlation between troponin T and decreased EF has been found to be more pronounced in nonischemic cardiomyopathy than in ischemic cardiomyopathy (18). This suggests that a different mechanism is involved in the cause of troponin subgroup elevation. It is important to mention that mild elevation of troponin level in patients presenting with acute coronary syndrome should not be taken lightly. Mild elevation of troponin has been found to be associated with a high cardiovascular event rate, and should trigger appropriate workup and treatment of these patients.
Limitations
Our study was a retrospective study of reported cases, limiting our results. The number of patients with reported troponin T level was small, limiting the value of troponin T correlation with EF. Troponin level in different institutions could have been measured using a different technique with different cutoff values as upper normal, limiting the mathematical calculation of the mean troponin value. However, we used absolute values of troponin level and not just positive or negative reports, making the calculated upper limit of troponin measured in this population valid.
CONCLUSION
Our study suggests that if the levels of troponin T are greater than 6 ng/mL and troponin I are greater than 15 ng/mL, the diagnosis of takotsubo cardiomyopathy is unlikely and, therefore, obstructive coronary disease should be considered in these patients regardless of other findings. Furthermore, the patients with stress-induced cardiomyopathy have a direct correlation only with troponin T elevation but not with other cardiac markers.
REFERENCES
- 1.Dote K, Sato H, Tateishi H, Uchida T, Ishihara M. [Myocardial stunning due to simultaneous multivessel coronary spasms: A review of 5 cases.] J Cardiol. 1991;21:203–14. [PubMed] [Google Scholar]
- 2.Movahed MR, Mostafizi K. Reverse or inverted left ventricular apical ballooning syndrome (reverse takotsubo cardiomyopathy) in a young woman in the setting of amphetamine use. Echocardiography. 2008;25:429–32. doi: 10.1111/j.1540-8175.2007.00604.x. [DOI] [PubMed] [Google Scholar]
- 3.Bonnemeier H, Schafer U, Schunkert H. Apical ballooning without apical ballooning. Eur Heart J. 2006;27:2246. doi: 10.1093/eurheartj/ehi820. [DOI] [PubMed] [Google Scholar]
- 4.Bonnemeier H, Ortak J, Burgdorf C, et al. “The artichoke heart”: The inverse counterpart of left ventricular apical ballooning. Resuscitation. 2007;72:342–3. doi: 10.1016/j.resuscitation.2006.07.008. [DOI] [PubMed] [Google Scholar]
- 5.Haghi D, Papavassiliu T, Fluchter S, et al. Variant form of the acute apical ballooning syndrome (takotsubo cardiomyopathy): Observations on a novel entity. Heart. 2006;92:392–4. doi: 10.1136/hrt.2005.061044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ennezat PV, Pesenti-Rossi D, Aubert JM, et al. Transient left ventricular basal dysfunction without coronary stenosis in acute cerebral disorders: A novel heart syndrome (inverted Takotsubo) Echocardiography. 2005;22:599–602. doi: 10.1111/j.1540-8175.2005.40046.x. [DOI] [PubMed] [Google Scholar]
- 7.Simoes MV, Marin-Neto JA, Maciel BC. Variable regional left ventricular dysfunction in takotsubo cardiomyopathy syndrome. Echocardiography. 2007;24:893. doi: 10.1111/j.1540-8175.2007.00548.x. [DOI] [PubMed] [Google Scholar]
- 8.Hurst RT, Askew JW, Reuss CS, et al. Transient midventricular ballooning syndrome: A new variant. J Am Coll Cardiol. 2006;48:579–83. doi: 10.1016/j.jacc.2006.06.015. [DOI] [PubMed] [Google Scholar]
- 9.Ohtsubo M, Sakai H, Takano H, et al. [Atypical takotsubo cardiomyopathy with preservation of apical contraction: A case report including pathological findings.] J Cardiol. 2005;46:237–42. [PubMed] [Google Scholar]
- 10.Tamura A, Kawano Y, Watanabe T, et al. A report of 2 cases of transient mid-ventricular ballooning. Int J Cardiol. 2007;122:e10–2. doi: 10.1016/j.ijcard.2006.11.060. [DOI] [PubMed] [Google Scholar]
- 11.Mazzarotto P, Stecconi P, Gemelli F, Azzarito M, Farnetti F. [A case of ballooning syndrome with atypical anterior localization.] Ital Heart J Suppl. 2005;6:730–4. [PubMed] [Google Scholar]
- 12.Suzuki K, Osada N, Akasi YJ, et al. An atypical case of “Takotsubo cardiomyopathy” during alcohol withdrawal: Abnormality in the transient left ventricular wall motion and a remarkable elevation in the ST segment. Intern Med. 2004;43:300–5. doi: 10.2169/internalmedicine.43.300. [DOI] [PubMed] [Google Scholar]
- 13.Strunk B, Shaw RE, Bull S, et al. High incidence of focal left ventricular wall motion abnormalities and normal coronary arteries in patients with myocardial infarctions presenting to a community hospital. J Invasive Cardiol. 2006;18:376–81. [PubMed] [Google Scholar]
- 14.Lamm G, Auer J, Eber B. Atypical form of left ventricular ballooning after a violent attack. Int J Cardiol. 2007;119:395–7. doi: 10.1016/j.ijcard.2006.07.168. [DOI] [PubMed] [Google Scholar]
- 15.Lyon AR, Rees PS, Prasad S, Poole-Wilson PA, Harding SE. Stress (Takotsubo) cardiomyopathy – a novel pathophysiological hypothesis to explain catecholamine-induced acute myocardial stunning. Nat Clin Pract Cardiovasc Med. 2008;5:22–9. doi: 10.1038/ncpcardio1066. [DOI] [PubMed] [Google Scholar]
- 16.Ramaraj R. Stress cardiomyopathy: Aetiology and management. Postgrad Med J. 2007;83:543–6. doi: 10.1136/pgmj.2007.058776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wittstein IS, Thiemann DR, Lima JA, et al. Neurohumoral features of myocardial stunning due to sudden emotional stress. N Engl J Med. 2005;352:539–48. doi: 10.1056/NEJMoa043046. [DOI] [PubMed] [Google Scholar]
- 18.Gorenek B, Kudaiberdieva G, Taraktas M, et al. Correlation between left ventricular ejection fraction and cardiac troponin T concentration is more pronounced in patients with nonischemic cardiomyopathy. J Electrocardiology. 2007;40:S75. [Google Scholar]