Abstract
Background
Intubation of the trachea in the pre-hospital setting may be lifesaving in severely ill and injured patients. However, tracheal intubation is frequently difficult to perform in this challenging environment, is associated with a lower success rate, and failed tracheal intubation constitutes an important cause of morbidity. Novel indirect laryngoscopes, such as the Glidescope® and the AWS® laryngoscopes may reduce this risk.
Methods
We compared the efficacy of these devices to the Macintosh laryngoscope when used by 25 Advanced Paramedics proficient in direct laryngoscopy, in a randomized, controlled, manikin study. Following brief didactic instruction with the Glidescope® and the AWS® laryngoscopes, each participant took turns performing laryngoscopy and intubation with each device, in an easy intubation scenario and following placement of a hard cervical collar, in a SimMan® manikin.
Results
Both the Glidescope® and the AWS® performed better than the Macintosh, and demonstrate considerable promise in this context. The AWS® had the least number of dental compressions in all three scenarios, and in the cervical spine immobilization scenario it required fewer maneuvers to optimize the view of the glottis.
Conclusion
The Glidescope® and AWS® devices possess advantages over the conventional Macintosh laryngoscope when used by Advanced Paramedics in normal and simulated difficult intubation scenarios in this manikin study. Further studies are required to extend these findings to the clinical setting.
Background
Intubation of the trachea by paramedics in the pre-hospital setting may be lifesaving in severely ill and injured patients [1-3]. However, tracheal intubation is often difficult to perform in this setting, is associated with a lower success rate. Failed tracheal intubation in this setting constitutes an important cause of morbidity, arising from direct airway trauma and the systemic complications of hypoxia [4,5]. In Ireland, Advanced Paramedics (AP's) are a subgroup of Emergency Medicine Technicians that are trained and certified as being competent in the skill of direct laryngoscopy and tracheal intubation.
The recent development of a number of indirect laryngoscopes, which do not require alignment of the oral-pharyngeal-tracheal axes, may reduce the difficult of tracheal intubation in the prehospital setting. Two portable indirect laryngoscopes, which could be included in ambulance equipment inventories, are the Glidescope® (Saturn Biomedical System Inc., Burnaby, Canada) (Figure 1) and the AWS® (Hoya Corporation, Tokyo, Japan) (Figure 2) laryngoscopes. Clinical studies have demonstrated advantages over the Macintosh laryngoscope for both the Glidescope® [6-9], and the AWS® [8,10] laryngoscopes. However, the efficacy of the Glidescope® and the AWS® when used by APs is not known, and the relative efficacies of these devices in comparison to the Macintosh laryngoscope have not been compared in a single study.
Figure 1.
Photograph of the Glidescope laryngoscope. The device is held in the left hand and passed into the mouth over the tongue, and the tip placed in the vallecula or under the epiglottis.
Figure 2.
Photograph of the AWS® laryngoscope. The device is held in the left hand and passed into the mouth over the tongue, and the tip is placed under the epiglottis.
We therefore wished to compare these two novel devices to the Macintosh laryngoscope when used by APs with demonstrated competence in the skill of tracheal intubation using the Macintosh laryngoscope.
Methods
Following ethical committee approval, and written informed consent, 25 Advanced Paramedics certified as competent to perform tracheal intubation consented to participate in this study. These participants constituted a convenience sample of AP's that attended a Resuscitation Conference on the 11th June 2008 in Galway, Ireland, and represents more than 20% of all paramedics in Ireland.
Each AP received a standardized training session with the Glidescope®, the AWS® and the Macintosh laryngoscopes. This included a demonstration of the intubation technique with each device, and verbal instructions regarding the correct use of each device. The use of optimization manoeuvres, such as external laryngeal pressure, to facilitate intubation with the Macintosh was also demonstrated. The total training time for each device was ten minutes. Each participant was then allowed to perform practice attempts with each device until each performed one successful tracheal intubation with each device. This training was carried out by a different member of the study team to the investigator that performed the actual study measurements. All intubations were performed with a 7.5 mm internal diameter cuffed endotracheal tube (ETT). The sequence in which each participant used the devices was initially randomized, and thereafter each participant used the devices in the same sequence throughout the protocol.
The design of the study was a randomized crossover trial. Each AP performed tracheal intubation with each device in a SimMan® manikin (Laerdal®, Kent, UK) in the following laryngoscopy scenarios: (1) normal airway in the supine position; (2) cervical immobilization, achieved by mean of placement of a hard neck collar; and (3) normal airway in the supine position. The aim of the latter scenario was to determine whether there was a learning curve with the newer devices. The primary endpoints were the rate of successful placement of the endotracheal tube (ETT) and the duration of tracheal intubation. The duration of each tracheal intubation attempt was defined as the time taken from insertion of the blade between the teeth until the ETT was deemed to be correctly positioned by each participant. Where the participant visualized the ETT passing through the cords, the attempt was considered complete at this point. Where the participant was unsure as to the position of the ETT, the time taken to connect the ETT to an Ambu® bag and inflate the lungs was also included in the duration of the attempt. In any case, after each intubation attempt an investigator verified the position of the ETT tip. A failed intubation attempt was defined as an attempt in which the trachea was not intubated, or where intubation of the trachea required greater than 60 seconds to perform [11-14].
Additional endpoints included the rate of successful placement of the endotracheal tube (ETT) in the trachea, the number of intubation attempts, the number of optimization maneuvers required (readjustment of head position, second assistant) to aid tracheal intubation and the severity of dental trauma. The severity of dental trauma was calculated based on a grading of pressure on the teeth (none = 0, mild = 1, moderate/severe ≥ 2). To improve reliability the same investigator assessed the severity of dental compression every time thus removing the potential for any inter-rater variability. We have demonstrated in multiple previous studies that this method of assessing dental pressure performs well, and appears to yield reasonably consistent results over time [15-20].
At the end of each scenario, each participant scored the ease of use of each device on a visual analogue scale (from 0 = Extremely Easy to 10 = Extremely Difficult). At the end of this protocol, each participant completed a questionnaire to determine self-assessed comfort and skill level for all three devices.
Statistical analysis
We based our sample size estimation on the duration of the successful tracheal intubation attempt. Based on prior studies [15] we projected that the duration of tracheal intubation would be 15 seconds for the Macintosh laryngoscope, with a standard deviation of 5 seconds, in the easy laryngoscopy scenario with the Macintosh laryngoscope. We considered that an important change in the duration of tracheal intubation would be a 33% absolute change, i.e. an increase to 20 seconds or a reduction to 10 seconds. Based on these figures, using an α = 0.05 and β = 0.2, for an experimental design examining three devices, we estimated that 17 paramedics would be required. We therefore aimed to enroll a minimum of 20 paramedics to the study.
The analysis was performed using Sigmastat 3.5 (Systat Software, San Jose, CA, USA. Data for the duration of the first and the successful intubation attempt, the instrument difficulty score, and the overall device assessment were analyzed using one way Analysis of Variance (ANOVA) or the using the Kruskal-Wallis One Way ANOVA on Ranks depending on the data distribution. Data for the number of intubation attempts, number of optimization maneuvers, severity of dental trauma, and the instrument difficulty score were analyzed using the Kruskal-Wallis One Way Analysis of Variance on Ranks. Data for the success of tracheal intubation attempts was analyzed using Chi square test. Continuous data are presented as means ± standard deviation (SD) or median (interquartile range), and ordinal and categorical data are presented as number and as frequencies. The α level for all analyses was set as P < 0.05.
Results
Twenty-five Advanced Paramedics were approached and each consented to participate in the study.
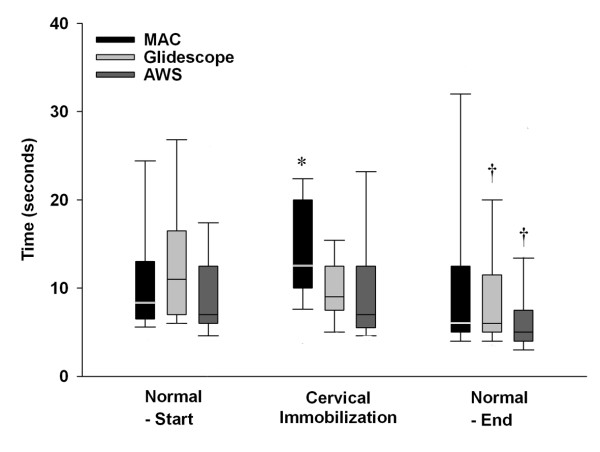
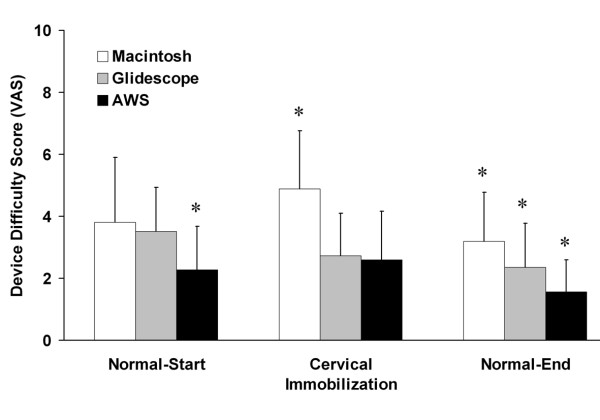
Scenario 1 – Normal Airway Scenario
All 25 APs successfully intubated the trachea with the Macintosh laryngoscope, the Glidescope® and the AWS® (Table 1). All 25 APs successfully intubated the trachea on the first attempt with the AWS®, while one AP needed a second attempt with the Macintosh and one with the Glidescope® (Table 1). The duration of the first and of the successful tracheal intubation attempts, and the number of optimization maneuvers required with each device were not significantly different (Table 1 and Figure 3). The severity of dental compression was significantly greater with the Macintosh compared to both the Glidescope® and AWS® devices and was significantly greater with the Glidescope® compared to the AWS® device (Table 1). The participants found the AWS® devices significantly easier to use than the Macintosh and Glidescope® laryngoscopes in this scenario (Figure 3). There was no significant difference in difficulty of device use between the Macintosh and Glidescope® laryngoscopes.
Table 1.
Data from easy laryngoscopy scenario.
| Parameter Assessed | Macintosh | Glidescope® | AWS® | P value |
| Overall Success Rate (%) | 25 (100) | 25 (100) | 25 (100) | P = 1.0 |
| Duration (sec, 1st attempt) | 8 (7, 13) | 11 (7, 17) | 7 (6, 12) | P = 0.1 |
| No of Intubation Attempts (%) | ||||
| 1 | 24 (96) | 24 (96) | 25 (100) | P = 0.602 |
| 2 | 1 (4) | 1 (4) | 0 | |
| 3 | 0 | 0 | 0 | |
| No of Optimization Maneuvers | ||||
| 0 | 23 (92) | 25 (100) | 25 (100) | P = 0.368 |
| 1 | 2 (8) | 0 | 0 | |
| > 1 | 0 | 0 | 0 | |
| Dental Compression [Severity] | ||||
| 0 | 1 (4)* | 11 (44)* | 18 (72)* | P < 0.001 |
| Mild [+] | 13 (52) | 10 (40) | 5 (20) | |
| Severe [++] | 11 (44) | 4 (16) | 2 (8) |
Notes: Data are reported as mean ± SD, median (interquartile range) or as number (percentage).
* Significantly [P < 0.05] different compared to both other groups
Figure 3.
Box plot representing the duration required to successfully intubate the trachea with each device in each scenario tested. The data are given as median and interquartile range, with the bars representing the 10th and 90th centile. * Indicates significantly different compared to both other Laryngoscopes. †Indicates significantly different from same device at the start of the protocol. Labels: Normal – Start: Intubation of the normal airway at the start of the protocol; Cervical Immobilization – Immobilization of the neck with hard collar; Normal – End: Intubation of the normal airway at the end of the protocol.
Scenario 2 – Cervical Spine Immobilization Scenario
All 25 APs successfully intubated the trachea with the Macintosh laryngoscope, the Glidescope® and the AWS® (Table 2). The duration of both the first and the successful tracheal intubation attempts were significantly longer with the Macintosh compared to the Glidescope® and AWS® devices (Table 2 and Figure 3). There was no significant difference in the duration of tracheal intubation attempts between the Glidescope® and AWS® devices (Table 2). There were no between group differences in the number of intubation attempts required with each device (Table 2). The number of optimization maneuvers required was significantly higher with the Macintosh compared to the Glidescope® or AWS® devices (Table 2). There was no difference in regard to the number of optimization maneuvers required with the Glidescope® and AWS® devices (Table 2). The severity of dental compression was significantly greater with the Macintosh compared to both the Glidescope® and AWS® devices (Table 2). There was no difference in severity of dental compression between the Glidescope® and AWS® devices (Table 2). The participants found the Macintosh laryngoscope significantly more difficult to use than the Glidescope® or AWS® devices in this scenario (Figure 4). There was no significant difference in difficulty of device use between the Glidescope® and AWS® laryngoscopes.
Table 2.
Data from Cervical Immobilization scenario.
| Parameter Assessed | Macintosh | Glidescope® | AWS® | P value |
| Overall Success Rate (%) | 25 (100) | 25 (100) | 25 (100) | P = 1.0 |
| Duration (sec, 1st attempt) | 13 (10, 20)* | 9 (8, 12) | 8 (6, 13) | P = 0.013 |
| No of Intubation Attempts (%) | ||||
| 1 | 23 (92) | 25 (100) | 25 (100) | P = 0.358 |
| 2 | 2 (8) | 0 | 0 | |
| 3 | 0 | 0 | 0 | |
| No of Optimization Maneuvers | ||||
| 0 | 2 (8)* | 24 (96) | 25 (100) | P < 0.001 |
| 1 | 23 (92) | 1 (4) | 0 | |
| > 1 | 0 | 0 | 0 | |
| Dental Compression [Severity] | ||||
| 0 | 0* | 6 (24) | 10 (40) | P = 0.023 |
| Mild [+] | 12 (48) | 10 (40) | 5 (20) | |
| Severe [++] | 13 (52) | 9 (36) | 10 (40) |
Notes: Data are reported as mean ± SD, median (interquartile range) or as number (percentage).
* Significantly [P < 0.05] different compared to both other groups
Figure 4.
Graph representing the user rated degree of difficulty of use of each instrument in each scenario tested. The data are given as mean ± SD. * Indicates significantly different compared to both other Laryngoscopes. Labels: Normal – Start: Intubation of the normal airway at the start of the protocol; Cervical Immobilization – Immobilization of the neck with hard collar; Normal – End: Intubation of the normal airway at the end of the protocol.
Scenario 3 – End protocol Normal Airway Scenario
All 25 APs successfully intubated the trachea on the first attempt with the Macintosh laryngoscope, and the Glidescope®, while one AP needed a second attempt with the AWS® (Table 3). The duration of the first and of the successful tracheal intubation attempts, the number of intubation attempts, and the number of optimization maneuvers required with each device were not significantly different in this scenario (Table 3). The duration of tracheal intubation attempts was significantly shorter with the Glidescope® and the AWS® devices but not with the Macintosh laryngoscopes, in this scenario compared to the first scenario (Tables 1, 3 and Figure 3). The severity of dental compression was significantly greater with the Macintosh compared to both the Glidescope® and AWS® devices (Table 3). There was no difference in severity of dental compression between the Glidescope® and AWS® devices (Table 3). The participants found the Pentax® AWS device significantly easier to use than the Macintosh and Glidescope® laryngoscopes in this scenario. They also found the Glidescope® laryngoscope significantly easier to use than the Macintosh laryngoscope (Figure 4).
Table 3.
Data from repeat easy laryngoscopy scenario.
| Parameter Assessed | Macintosh | Glidescope® | AWS® | P value |
| Overall Success Rate (%) | 25 (100) | 25 (100) | 25 (100) | P = 1.0 |
| Duration (sec, 1st attempt) | 6 (5, 12) | 6 (5, 11) | 5 (4, 8) | P = 0.25 |
| No of Intubation Attempts (%) | ||||
| 1 | 25 (100) | 25 (100) | 24 (96) | P = 0.368 |
| 2 | 0 | 0 | 1 (4) | |
| 3 | 0 | 0 | 0 | |
| No of Optimization Maneuvers | ||||
| 0 | 24 (96) | 25 (100) | 25 (100) | P = 0.368 |
| 1 | 0 | 0 | 0 | |
| > 1 | 1 (4) | 0 | 0 | |
| Dental Compression [Severity] | ||||
| 0 | 4 (16)* | 15 (60) | 20 (80) | P < 0.001 |
| Mild [+] | 11 (44) | 4 (16) | 2 (8) | |
| Severe [++] | 10 (40) | 6 (24) | 3 (12) |
Notes: Data are reported as mean ± SD, median (interquartile range) or as number (percentage).
* Significantly [P < 0.05] different compared to both other groups
End protocol overall device assessment
The APs found the Macintosh significantly more difficult to use than the Glidescope® and AWS® devices (Table 4). There was no significant difference in the ease of use of the Glidescope® and AWS® devices (Table 4). The APs expressed similar levels of confidence in performing tracheal intubation with each of the devices tested (Table 4).
Table 4.
Overall Device assessment by Participants.
| Parameter Assessed | Macintosh | Glidescope® | AWS® | P value |
| Overall Difficulty of Use Score | 4.3 ± 2.0* | 2.9 ± 2.1 | 2.6 ± 2.1 | P = 0.01 |
| Overall Confidence with each device | 7.4 ± 1.5 | 7.1 ± 2.4 | 7.8 ± 2.6 | P = 0.52 |
Notes: Data are reported as mean ± SD or as number (percentage).
* Significantly [P < 0.05] different compared to both other groups
Discussion
In Ireland, Advanced Paramedics are trained and certified as being competent in the skill of direct laryngoscopy and tracheal intubation by the Pre-Hospital Emergency Care Council (PHECC). Following initial training on high fidelity manikins, each AP is then seconded to a hospital for clinical training in the operating suite. Each AP must perform a minimum of 10 successful tracheal intubations under the direct supervision of a senior anaesthetist prior to certification. Once in clinical practice, AP's perform an average of 10–12 tracheal intubations per person per year. Consequently, this cohort possesses a high level of competence in the skill of tracheal intubation, and maintains this skill once in practice.
Outcome in severely ill and injured patients is improved where the airway is successfully secured early by tracheal intubation [1-3]. However, where difficulties or complications arise as a results of difficulties or failure to secure the airway in the pre-hospital patient, significant morbidity and even mortality may ensue [4,5,21]. The pre-hospital environment is a challenging one, and tracheal intubation is frequently difficult to perform and associated with a lower success rate compared to the hospital setting [22]. The need for repeated attempts to secure the airway emergently increases airway-related complications such as hypoxia, pulmonary aspiration and adverse hemodynamic events [5]. Accidental esophageal intubation can result in catastrophic complications, including pulmonary aspiration of gastric contents, cerebral hypoxia, and cardiac arrest [4]. Difficulties in tracheal intubation may also result in severe local complications such as perforation of laryngeal or pharyngeal structures [23].
Given these issues, the practice of pre-hospital tracheal intubation by personnel not fluent in the technique is increasingly questioned [24-26]. A slow learning curve for intubation with the Macintosh blade has been well documented among paramedic personnel [27,28] due to lack of regular exposure to the technique. These difficulties have led to the increasing use of alternative airway devices such as Combitube®, Laryngeal Tube® and Laryngeal Mask Airway® for airway management in the pre-hospital setting contexts [29-31], due to the rapid learning curves associated with these devices [32,33]. However trauma to the airway and aspiration injury remains a significant risk with these devices in these patients.
Conventional direct laryngoscopic laryngoscopes, such as the Macintosh laryngoscope, require the alignment of oral and tracheal axes in order to view the glottic opening. This is a difficult skill to successfully acquire [26,27,34], and to maintain [28], particularly if the opportunities to practice this skill are limited. Both the Glidescope® (Figure 1) and AWS® (Figure 2) devices have an exaggerated blade curvature with enhanced optics that give a view of the glottis without the need to align the oral and tracheal axes. Both devices are portable, and could be easily included in ambulance equipment inventories. We therefore wished to determine whether these devices possessed advantages over the conventional Macintosh laryngoscope when used by paramedics in the setting of normal and simulated difficult intubation.
Our study demonstrated that both the Glidescope® and AWS® devices demonstrated several advantages over the Macintosh laryngoscope, in both the normal and in the difficult intubation scenario. Both devices reduced the duration of tracheal intubation attempts in the cervical immobilization scenario, a situation commonly seen in the emergency pre-hospital setting. While the degree to which these devices reduced the time required to secure the airway appears relatively small, of the order of 5 – 10 seconds, it must be remembered that brain hypoxia may rapidly supervene in the emergency setting. In addition, these devices reduced the number of optimization maneuvers and reduced the potential for dental trauma when compared to the Macintosh laryngoscope. Of the two indirect laryngoscopes studies, despite largely comparable performance in other measures of difficulty, the APs found the AWS® easier to use in each scenario. The AWS® caused the least amount of dental compressions in each scenario. The structure of the blade of the AWS®, particularly the incorporation of a side channel for the ETT, may explain its better performance in these respects compared to the Glidescope.
Both the Glidescope® and AWS® devices exhibited a rapid learning curve, despite a deliberately brief instruction period. In the repeated easy laryngocsopy scenario, the duration of intubation attempts were significantly reduced for both the Glidescope® and AWS® laryngoscopes compared to the first scenario. This finding supports the feasibility of introducing these devices for use by APs in the out-of-hospital setting, and adds to the growing body of literature attesting to the fact that these devices, by reducing the skill required to perform tracheal intubation, may be particularly for advanced life support personnel, that may be called upon to perform this skill relatively infrequently [35-38]. In their overall assessment of the devices studied, the AP's rated the Macintosh most difficult device to use in each scenario. However, when assessing their confidence in the use of each device for tracheal intubation procedures, they rated the three laryngoscopes similarly. This rating probably reflects the familiarity of the AP's with the Macintosh laryngoscope.
A number of important limitations exist regarding this study. Firstly, we acknowledge that the potential for bias exists, as it is impossible to blind the AP's to the device being used. Secondly, this study was carried out in experienced users of the Macintosh laryngoscope. The findings may differ if studies in APs prior to their attaining competence with the Macintosh device. Thirdly, this is a manikin study, and may not adequately mimic clinical conditions, particularly in the emergency setting. A particular issue of particular relevance in the emergency setting is the risk of fogging and contamination of the lens by secretions and/or blood, especially in the traumatized airway. Therefore, these findings need to be confirmed and extended in clinical studies before definitive conclusions can be drawn. Careful consideration would also have to be given to the cost implications of introducing these more expensive laryngoscopes into the pre-hospital emergency care setting. Finally, the relative efficacies of these devices in comparison to other promising devices such as the Airtraq® [39,40], McCoy® [41], McGrath®[19], TruView® [42], LMA CTrach® [14] or Bonfils® [43] have not been determined. We focused on the Glidescope® and AWS® devices in this study due to the fact that these are portable devices that can easily be included in the equipment used by AP's. Nevertheless, further comparative studies are needed with other alternative laryngoscopy devices in order to find the optimal alternatives to the Macintosh laryngoscope.
Conclusion
The Glidescope® and AWS® devices appears to possess advantages over the conventional Macintosh laryngoscope when used by AP's in normal and simulated difficult intubation scenarios. The AWS® performed best overall, and demonstrates considerable promise in this context. Further clinical studies are necessary to confirm these initial positive findings.
Abbreviations
ANOVA: analysis of variance; ETT: endotracheal tube; SD: standard deviation; VAS: Visual analogue scale.
Competing interests
Pentax Ltd provided the AWS® device and the disposable blades free of charge for this study.
Authors' contributions
SN and CM conceived of the study, and participated in its design and execution and helped to draft the manuscript. AM, JO'D, and BDH participated in the study, recruited participants, and helped to draft the manuscript. JL participated in the design and coordination of the study, performed the statistical analysis, and helped to draft the manuscript. All authors read and approved the final manuscript.
Pre-publication history
The pre-publication history for this paper can be accessed here:
Acknowledgments
Acknowledgements
The authors gratefully acknowledge the help of Emmet Forkan, Advanced Paramedic, Galway University Hospitals and Mark Dixon, Project Officer, Centre for Immediate Care Services, University College Dublin, for their help in recruiting Advanced Paramedics for this study. We would like to thank Pentax Ltd, for the provision of the AWS® device. All other support was solely from institutional and/or departmental sources.
Contributor Information
Sajid Nasim, Email: dr_snasim@yahoo.com.
Chrisen H Maharaj, Email: chrisenm@gmail.com.
Muhammad A Malik, Email: manwarmalik@yahoo.com.
John O' Donnell, Email: john.odonnell@hse.ie.
Brendan D Higgins, Email: brendan.higgins@nuigalway.ie.
John G Laffey, Email: john.laffey@nuigalway.ie.
References
- Winchell RJ, Hoyt DB. Endotracheal intubation in the field improves survival in patients with severe head injury. Trauma Research and Education Foundation of San Diego. Arch Surg. 1997;132:592–597. doi: 10.1001/archsurg.1997.01430300034007. [DOI] [PubMed] [Google Scholar]
- Garner A, Rashford S, Lee A, Bartolacci R. Addition of physicians to paramedic helicopter services decreases blunt trauma mortality. Aust N Z J Surg. 1999;69:697–701. doi: 10.1046/j.1440-1622.1999.01688.x. [DOI] [PubMed] [Google Scholar]
- Sanson G, Di Bartolomeo S, Nardi G, Albanese P, Diani A, Raffin L, Filippetto C, Cattarossi A, Scian E, Rizzi L. Road traffic accidents with vehicular entrapment: incidence of major injuries and need for advanced life support. Eur J Emerg Med. 1999;6:285–291. doi: 10.1097/00063110-199912000-00002. [DOI] [PubMed] [Google Scholar]
- Mort TC. Esophageal intubation with indirect clinical tests during emergency tracheal intubation: a report on patient morbidity. J Clin Anesth. 2005;17:255–262. doi: 10.1016/j.jclinane.2005.02.004. [DOI] [PubMed] [Google Scholar]
- Mort TC. Emergency tracheal intubation: complications associated with repeated laryngoscopic attempts. Anesth Analg. 2004;99:607–613. doi: 10.1213/01.ANE.0000122825.04923.15. table of contents. [DOI] [PubMed] [Google Scholar]
- Agro F, Barzoi G, Montecchia F. Tracheal intubation using a Macintosh laryngoscope or a GlideScope in 15 patients with cervical spine immobilization. Br J Anaesth. 2003;90:705–706. doi: 10.1093/bja/aeg560. [DOI] [PubMed] [Google Scholar]
- Sun DA, Warriner CB, Parsons DG, Klein R, Umedaly HS, Moult M. The GlideScope Video Laryngoscope: randomized clinical trial in 200 patients. Br J Anaesth. 2005;94:381–384. doi: 10.1093/bja/aei041. [DOI] [PubMed] [Google Scholar]
- Malik MA, Maharaj CH, Harte BH, Laffey JG. Comparison of Macintosh, Truview EVO2, Glidescope, and Airwayscope laryngoscope use in patients with cervical spine immobilization. Br J Anaesth. 2008;101:723–730. doi: 10.1093/bja/aen231. [DOI] [PubMed] [Google Scholar]
- Cooper RM, Pacey JA, Bishop MJ, McCluskey SA. Early clinical experience with a new videolaryngoscope (GlideScope) in 728 patients. Can J Anaesth. 2005;52:191–198. doi: 10.1007/BF03027728. [DOI] [PubMed] [Google Scholar]
- Enomoto Y, Asai T, Arai T, Kamishima K, Okuda Y. Pentax-AWS, a new videolaryngoscope, is more effective than the Macintosh laryngoscope for tracheal intubation in patients with restricted neck movements: a randomized comparative study. Br J Anaesth. 2008;100:544–548. doi: 10.1093/bja/aen002. [DOI] [PubMed] [Google Scholar]
- Maharaj CH, Buckley E, Harte BH, Laffey JG. Endotracheal Intubation in Patients with Cervical Spine Immobilization: A Comparison of Macintosh and Airtraq™ Laryngoscopes. Anesthesiology. 2007;107:53–59. doi: 10.1097/01.anes.0000267529.71756.f0. [DOI] [PubMed] [Google Scholar]
- Maharaj CH, Costello JF, Harte BH, Laffey JG. Evaluation of the Airtraq and Macintosh laryngoscopes in patients at increased risk for difficult tracheal intubation. Anaesthesia. 2008;63:182–188. doi: 10.1111/j.1365-2044.2007.05316.x. [DOI] [PubMed] [Google Scholar]
- Maharaj CH, O'Croinin D, Curley G, Harte BH, Laffey JG. A comparison of tracheal intubation using the Airtraq or the Macintosh laryngoscope in routine airway management: a randomised, controlled clinical trial. Anaesthesia. 2006;61:1093–1099. doi: 10.1111/j.1365-2044.2006.04819.x. [DOI] [PubMed] [Google Scholar]
- Malik MA, Subramaniam R, Churasia S, Maharaj CH, Harte BH, Laffey JG. Tracheal intubation in patients with cervical spine immobilization: a comparison of the Airwayscope, LMA CTrach, and the Macintosh laryngoscopes. Br J Anaesth. 2009;102:654–661. doi: 10.1093/bja/aep056. [DOI] [PubMed] [Google Scholar]
- Maharaj CH, Higgins B, Harte BH, Laffey JG. Evaluation of ease of intubation with the Airtraq® or Macintosh laryngoscope by anaesthetists in easy and simulated difficult laryngoscopy – A manikin study. Anaesthesia. 2006;61:469–477. doi: 10.1111/j.1365-2044.2006.04547.x. [DOI] [PubMed] [Google Scholar]
- Nasim S, Maharaj CH, Butt I, Malik MA, J OD, Higgins BD, Harte BH, Laffey JG. Comparison of the Airtraq and Truview laryngoscopes to the Macintosh laryngoscope for use by Advanced Paramedics in easy and simulated difficult intubation in manikins. BMC Emerg Med. 2009;9:2. doi: 10.1186/1471-227X-9-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maharaj CH, Costello J, Higgins B, Harte BH, Laffey JG. Learning and performance of Tracheal intubation by novice personnel: A comparison of the Airtraq® and Macintosh laryngoscope. Anaesthesia. 2006;61:671–677. doi: 10.1111/j.1365-2044.2006.04653.x. [DOI] [PubMed] [Google Scholar]
- Maharaj CH, Costello J, Higgins BD, Harte BH, Laffey JG. Retention of tracheal intubation skills by novice personnel: A comparison of the Airtraq® and Macintosh laryngoscopes. Anaesthesia. 2007;62:272–278. doi: 10.1111/j.1365-2044.2007.04938.x. [DOI] [PubMed] [Google Scholar]
- Maharaj CH, McDonnell JG, Harte BH, Laffey JG. A comparison of direct and indirect laryngoscopes and the ILMA in novice users: a manikin study. Anaesthesia. 2007;62:1161–1166. doi: 10.1111/j.1365-2044.2007.05216.x. [DOI] [PubMed] [Google Scholar]
- Maharaj CH, Ni Chonghaile M, Higgins B, Harte BH, Laffey JG. Tracheal intubation by inexperienced medical residents using the Airtraq® and Macintosh laryngoscope – A manikin study. Am J Emerg Med. 2006;24:769–774. doi: 10.1016/j.ajem.2006.03.014. [DOI] [PubMed] [Google Scholar]
- Schlossmacher P, Martinet O, Testud R, Agesilas F, Benhamou L, Gauzere BA. Emergency percutaneous tracheostomy in a severely burned patient with upper airway obstruction and circulatory arrest. Resuscitation. 2006;68:301–305. doi: 10.1016/j.resuscitation.2005.06.021. [DOI] [PubMed] [Google Scholar]
- Adnet F, Jouriles NJ, Le Toumelin P, Hennequin B, Taillandier C, Rayeh F, Couvreur J, Nougiere B, Nadiras P, Ladka A, et al. Survey of out-of-hospital emergency intubations in the French prehospital medical system: a multicenter study. Ann Emerg Med. 1998;32:454–460. doi: 10.1016/S0196-0644(98)70175-1. [DOI] [PubMed] [Google Scholar]
- Koscielny S, Gottschall R. [Perforation of the hypopharynx as a rare life-threatening complication of endotracheal intubation] Anaesthesist. 2005;55:45–52. doi: 10.1007/s00101-005-0873-7. [DOI] [PubMed] [Google Scholar]
- Brambrink AM, Koerner IP. Prehospital advanced trauma life support: how should we manage the airway, and who should do it? Crit Care. 2004;8:3–5. doi: 10.1186/cc2420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nolan JD. Prehospital and resuscitative airway care: should the gold standard be reassessed? Curr Opin Crit Care. 2001;7:413–421. doi: 10.1097/00075198-200112000-00008. [DOI] [PubMed] [Google Scholar]
- Gerbeaux P. Should emergency medical service rescuers be trained to practice endotracheal intubation? Crit Care Med. 2005;33:1864–1865. doi: 10.1097/01.CCM.0000174493.45348.94. [DOI] [PubMed] [Google Scholar]
- Wang HE, Seitz SR, Hostler D, Yealy DM. Defining the learning curve for paramedic student endotracheal intubation. Prehosp Emerg Care. 2005;9:156–162. doi: 10.1080/10903120590924645. [DOI] [PubMed] [Google Scholar]
- Garza AG, Gratton MC, Coontz D, Noble E, Ma OJ. Effect of paramedic experience on orotracheal intubation success rates. J Emerg Med. 2003;25:251–256. doi: 10.1016/S0736-4679(03)00198-7. [DOI] [PubMed] [Google Scholar]
- Deakin CD, Peters R, Tomlinson P, Cassidy M. Securing the prehospital airway: a comparison of laryngeal mask insertion and endotracheal intubation by UK paramedics. Emerg Med J. 2005;22:64–67. doi: 10.1136/emj.2004.017178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kurola J, Harve H, Kettunen T, Laakso JP, Gorski J, Paakkonen H, Silfvast T. Airway management in cardiac arrest – comparison of the laryngeal tube, tracheal intubation and bag-valve mask ventilation in emergency medical training. Resuscitation. 2004;61:149–153. doi: 10.1016/j.resuscitation.2004.01.014. [DOI] [PubMed] [Google Scholar]
- Rumball C, Macdonald D, Barber P, Wong H, Smecher C. Endotracheal intubation and esophageal tracheal Combitube insertion by regular ambulance attendants: a comparative trial. Prehosp Emerg Care. 2004;8:15–22. doi: 10.1080/312703002764. [DOI] [PubMed] [Google Scholar]
- Weksler N, Tarnopolski A, Klein M, Schily M, Rozentsveig V, Shapira AR, Gurman GM. Insertion of the endotracheal tube, laryngeal mask airway and oesophageal-tracheal Combitube. A 6-month comparative prospective study of acquisition and retention skills by medical students. Eur J Anaesthesiol. 2005;22:337–340. doi: 10.1017/S0265021505000578. [DOI] [PubMed] [Google Scholar]
- Vertongen VM, Ramsay MP, Herbison P. Skills retention for insertion of the Combitube and laryngeal mask airway. Emerg Med (Fremantle) 2003;15:459–464. doi: 10.1046/j.1442-2026.2003.00502.x. [DOI] [PubMed] [Google Scholar]
- Mulcaster JT, Mills J, Hung OR, MacQuarrie K, Law JA, Pytka S, Imrie D, Field C. Laryngoscopic intubation: learning and performance. Anesthesiology. 2003;98:23–27. doi: 10.1097/00000542-200301000-00007. [DOI] [PubMed] [Google Scholar]
- Koyama J, Aoyama T, Kusano Y, Seguchi T, Kawagishi K, Iwashita T, Okamoto K, Okudera H, Takasuna H, Hongo K. Description and first clinical application of AirWay Scope for tracheal intubation. J Neurosurg Anesthesiol. 2006;18:247–250. doi: 10.1097/00008506-200610000-00005. [DOI] [PubMed] [Google Scholar]
- Koyama Y, Inagawa G, Miyashita T, Kikuchi T, Miura N, Miki T, Kurihara R, Kamiya Y, Goto T. Comparison of the Airway Scope, gum elastic bougie and fibreoptic bronchoscope in simulated difficult tracheal intubation: a manikin study. Anaesthesia. 2007;62:936–939. doi: 10.1111/j.1365-2044.2007.05152.x. [DOI] [PubMed] [Google Scholar]
- Miki T, Inagawa G, Kikuchi T, Koyama Y, Goto T. Evaluation of the Airway Scope, a new video laryngoscope, in tracheal intubation by naive operators: a manikin study. Acta Anaesthesiol Scand. 2007;51:1378–1381. doi: 10.1111/j.1399-6576.2007.01450.x. [DOI] [PubMed] [Google Scholar]
- Hirabayashi Y. Airway Scope: initial clinical experience with novice personnel. Can J Anaesth. 2007;54:160–161. doi: 10.1007/BF03022021. [DOI] [PubMed] [Google Scholar]
- Maharaj CH, Costello JF, Higgins BD, Harte BH, Laffey JG. Learning and performance of tracheal intubation by novice personnel: a comparison of the Airtraq and Macintosh laryngoscope. Anaesthesia. 2006;61:671–677. doi: 10.1111/j.1365-2044.2006.04653.x. [DOI] [PubMed] [Google Scholar]
- Maharaj CH, Costello JF, McDonnell JG, Harte BH, Laffey JG. The Airtraq as a rescue airway device following failed direct laryngoscopy: A case series. Anaesthesia. 2007;62:598–601. doi: 10.1111/j.1365-2044.2007.05036.x. [DOI] [PubMed] [Google Scholar]
- Uchida T, Hikawa Y, Saito Y, Yasuda K. The McCoy levering laryngoscope in patients with limited neck extension. Can J Anaesth. 1997;44:674–676. doi: 10.1007/BF03015455. [DOI] [PubMed] [Google Scholar]
- Malik MA, O'Donoghue C, Carney J, Maharaj CH, Harte BH, Laffey JG. Comparison of the Glidescope, the Pentax AWS, and the Truview EVO2 with the Macintosh laryngoscope in experienced anaesthetists: a manikin study. Br J Anaesth. 2009;102:128–134. doi: 10.1093/bja/aen342. [DOI] [PubMed] [Google Scholar]
- Rudolph C, Schneider JP, Wallenborn J, Schaffranietz L. Movement of the upper cervical spine during laryngoscopy: a comparison of the Bonfils intubation fibrescope and the Macintosh laryngoscope. Anaesthesia. 2005;60:668–672. doi: 10.1111/j.1365-2044.2005.04224.x. [DOI] [PubMed] [Google Scholar]