Abstract
Objective
To examine the differential gene expression in telomerase transduced osteoarthritis fibroblast-like synoviocytes (hTERT-OA 13A FLS) and telomerase transduced rheumatoid arthritis FLS (hTERT-RA 516 FLS) and test the hypothesis that longterm culture of hTERT-OA 13A FLS display a disease-specific gene expression profile.
Methods
Gene expression in passage 8 hTERT-OA 13A FLS and passage 8 hTERT-RA 516 FLS were compared using microarray assays. Differential expression of selected genes was further examined by reverse transcription-polymerase chain reaction (RT-PCR). After continuous expansion in culture for an additional 4 months, gene expression in the longterm cultures of hTERT-OA 13A FLS and hTERT-RA 516 FLS was again examined with microarray and real-time RT-PCR.
Results
hTERT-OA 13A FLS displayed a distinct gene expression profile. While hTERT-RA 516 FLS expressed ADAMTS1, ADAMTS3, ADAMTS5, and several carboxypeptidases, hTERT-OA 13A FLS expressed matrix metalloproteinase (MMP)1, MMP3, and several cathepsins at higher levels. Numerous genes classified in the immune response, lipid transport/catabolism, and phosphate transport biological processes were also expressed at higher levels in hTERT-OA 13A FLS. In contrast, numerous genes classified in the positive regulation of cell proliferation, anti-apoptosis, and angio-genesis biological processes were expressed at higher levels in hTERT-RA 516 FLS. Further, of the recently proposed 21 candidate synovial biomarkers of OA, 12 (57%) were detected in our study.
Conclusion
The findings indicate that OA FLS may not be a passive bystander in OA and that telomerase transduced OA FLS offer an alternative tool for the study of synovial disease markers and for the identification of new therapeutic targets for OA therapy.
Keywords: OSTEOARTHRITIS, SYNOVIOCYTES, DISEASE MARKERS, ADAMTS, MATRIX METALLOPROTEINASE, RHEUMATOID ARTHRITIS, TELOMERASE
Osteoarthritis (OA) is a progressive disorder characterized by the degeneration of articular cartilage, formation of osteophytes, and mild synovial inflammation. Because the most striking pathological changes are found in articular cartilage, OA is mainly considered a degenerative disease of articular cartilage. OA synovium has traditionally been considered to be “normal” and was used as controls in many studies to investigate the pathological changes in the synovium of patients with rheumatoid arthritis (RA)1-4. OA fibroblast-like synoviocytes (FLS) were used as controls in studies investigating the cellular alterations in RA FLS5-8. However, there is increasing evidence that the OA synovium may not be a passive bystander in the initiation or progression of OA9,10. A low degree of synovium inflammation exists in OA11-15. OA synovium and OA FLS display differential gene expressions compared to RA synovium and RA FLS or compared to normal synovium and normal FLS16,17. These observations support the hypothesis that OA FLS, similar to RA FLS, is abnormal.
Analyses of differential gene expressions between OA synovium and RA synovium, or between OA synovium and normal synovium are important for understanding the in vivo state of OA synovium; however, such work provides no information regarding cell type specific differential gene expressions. Analyses of primary FLS provide information that is more cell type specific, but they also have drawbacks. Differential gene expressions detected using primary OA FLS and RA FLS may vary due to the variations in the methods of cell preparation or the different passage numbers. Non-FLS types of cells coexist in primary FLS preparations that secrete inflammatory cytokines and express cell type specific proteins18, which, in turn, may affect the gene expressions in FLS. Primary FLS of early passages (passages 2−3) used in many reported studies may contain up to 5% non-FLS cell types calculated according to the doubling time of synovial cells and initial cell populations18. It has been reported that the expressions of numerous genes in arthritis-derived FLS change considerably with passages17. The passage-dependent gene expressions in primary FLS not only make it difficult to get consistent and repeatable results using primary FLS derived from a specific patient, but also make it difficult to compare the results from different laboratories. Moreover, the differential gene expression detected using primary FLS (passages 2−3) may not reflect the “true” disease characteristics of the FLS examined but reflect the characteristics of the FLS mixed with other types of cells. These drawbacks can be partially overcome by the examination of telomerase-transduced FLS, since the coexistence of other cell types in telomerase-transduced FLS is highly unlikely and the differential expression of a majority of genes is largely maintained with time.
Currently, diagnosis of OA depends on clinical and radiographic findings such as joint pain and radiographic changes in articular cartilage. These approaches are only effective in detecting intermediate or late-stage OA. New diagnostic methods, especially for early diagnosis of OA, are needed. A recent study reported that OA synovial tissues displayed distinct differential expression patterns compared to RA synovial tissues, and suggested that the differential expression of selected genes might be useful as disease markers16. Another study reported that OA FLS displayed distinct differential expression patterns compared to RA FLS and also suggested that the differential expression of selected genes might be useful as disease markers17. In our laboratory, we recently successfully established human telomerase-transduced OA FLS and telomerase-transduced RA FLS19,20. In the work reported here we examine the differential gene expression between hTERT-OA 13A FLS and hTERT-RA 156 FLS to investigate whether hTERT-OA 13A FLS display a stable and distinctive gene expression profile compared to hTERT-RA 516 FLS, and whether certain distinct gene expression patterns are disease-specific.
MATERIALS AND METHODS
Materials and cells
Dulbecco's modified eagle medium, fetal bovine serum, stock antibiotic and antimycotic mixture were products of Invitrogen (Carlsbad, CA, USA). hTERT-OA 13A FLS and hTERT-RA 516 FLS have been described. They were established from passage 5 primary OA FLS and passage 5 primary RA FLS, respectively, with the approval of the authors’ Institutional Review Board19,20.
Cell culture and RNA extraction
hTERT-OA 13A FLS (passage 8) and hTERT-RA 516 FLS (passage 8) were plated in 100 mm plates at 60% confluence. On the second day, medium containing 10% serum was added and cells were cultured for 24 h. Total RNA was extracted using Trizol reagent (Invitrogen), and purified using Oligotex kit (Qiagen, Valencia, CA). Agilent microarray and semi-quantitative reverse transcription-polymerase chain reaction (RT-PCR) were performed using these RNA samples. The passage 8 hTERT-OA 13A FLS and passage 8 hTERT-RA 516 FLS were continuously expanded for 4 months. The longterm cultured hTERT-OA 13A FLS (passage 25) and hTERT-RA 516 FLS (passage 25) were plated in 100 mm plates at 60% confluence and cultured for 24 h. RNA was extracted using Trizol reagent and purified using Oligotex kit (Qiagen, Valencia, CA). Affymetrix microarray and quantitative real time RT-PCR were performed using these RNA samples.
Agilent microarrays
Microarray experiments were carried out to examine the differential gene expression between passage 8 hTERT-OA 13A FLS and passage 8 hTERT-RA 516 FLS using Agilent human cDNA array B chips (Agilent, Palo Alto, CA) as described20. Microarray was scanned at 10 μm resolution using a GenePix 4000A scanner (Axon Instruments, Union City, CA) and image was analyzed using the GenePix Pro 5.1 software (Axon Instruments, Union City, CA) for normalization and statistical analysis. Data was filtered for unreliable data points using Acuity software (Axon Instruments, Union City, CA). Filtered data was imported into GeneSpring software for further statistical analysis (Silicon Genetics, Redwood City, CA). Differentially expressed genes were classified according to gene ontology category biological process using Onto-Express software (http://vortex.cs.wayne.edu/Projects.html).
Affymetrix microarray
Double-stranded DNA was synthesized using SuperScript double-stranded cDNA synthesis kit (Invitrogen, San Diego, CA). The DNA product was purified using GeneChip sample cleanup module (Affymetrix, Santa Clara, CA). cRNA was synthesized and biotin labeled using BioArray high yield RNA transcript labeling kit (Enzo Life Sciences, Farmingdale, NY). The cRNA product was purified using GeneChip sample cleanup module and subsequently chemically fragmented. The fragmented, biotinylated cRNA was hybridized to HGU133_Plus_2 gene chip using Affymetrix Fluidics Station 400. Fluorescent signal was quantified during 2 scans by Agilent Gene Array Scanner G2500A (Agilent Technologies), and GeneChip operating Software (Affymetrix). For further analysis of fold changes, false discovery rate, and gene ontology, Genesifter software (VizX Labs, Seattle, WA) was used.
Semiquantitative RT-PCR
Briefly, 1 μg of RNA sample was reverse transcribed at 60°C for 60 min, followed by enzyme inactivation at 85°C for 5 min. PCR experiments were carried out using ThermoScript RT-PCR machine (Invitrogen, Carlsbad, CA). Amplifications were carried out for 30−40 cycles by denaturing at 95°C for 30 s, annealing at 55°C for 30 s, and extending at 72°C for 45 s, with a final extension at 72°C for 10 min. The products were electrophoresed on 2% agarose gels, stained with ethidium bromide, and photographed using a low light image system (ChemiImager 4000, Alpha Innotech Corporation, San Leandro, CA). Each RT-PCR experiment was repeated at least 3 times using 2 or 3 different RNA batches.
Real-time RT-PCR
cDNA was synthesized using TaqMan® Reverse Transcription Reagents (Applied Biosystems, Inc., University Park, IL). Quantitative real time RT-PCR was then performed. Briefly, quantification of relative transcript levels for selected genes and the housekeeping gene glyceraldehyde-3-phosphate dehydrogenase (GAPDH) was performed using the ABI7000 Real Time PCR system (Applied Biosystems). TaqMan® Gene Expression assays (Applied Biosystems) were used, which contains a FAM-MGB probe for fluorescent detection. The probe information can be obtained on request from the manufacturer. cDNA samples were amplified with an initial Taq DNA polymerase activation step at 95°C for 10 min, followed by 40 cycles of denaturation at 95°C for 15 s and annealing at 60°C for 1 min. For each gene, Ct values were obtained in triplicate. Fold change was calculated21 and the expression level of the genes of interest was normalized to the expression level of GAPDH. Each real time RT-PCR experiment was repeated twice in triplicate using 2 different RNA batches.
RESULTS
Differential gene expression in passage 8 FLS
Agilent microarray analyses of the differential gene expression in passage 8 hTERT-OA 13A FLS and passage 8 hTERT-RA 516 FLS were carried out as described in Materials and Methods. We found that the dye bias was substantial, and caused many false positive results. Therefore, 2 microarrays were performed by reverse labeling with Cy3 and Cy5. Only the genes that showed similar differential gene expression in both microarrays were selected for further study and/or discussion. Among the more than 22,605 transcripts examined, a total of 178 differentially-expressed genes (more than 2.5-fold) were detected; 62 genes were expressed at higher levels and 116 genes were expressed at lower levels in hTERT-OA 13A FLS compared to hTERT-RA 516 FLS (data not shown). These differentially expressed genes were classified according to gene ontology category biological process. Selected genes, which are involved in a specific biological process that has been implicated in OA or is suspected to play a role in OA pathological calcification such as ectonucleotide pyrophosphatase-phosphodiesterase 2 (ENPP2) and adenylate cyclase 3 (ADCY3), are listed in Table 1.
Table 1.
Selected differentially expressed genes detected by Agilent microarray.
| Funtional Family | Gene Name | Differ Expre (fold)* | Description |
|---|---|---|---|
| Immune response | |||
| HLA-DR beta 4 | 6.1 (35.6) | Beta 4 chain of HLA-DR, a subunit of MHC class II molecules that bind peptides and present them to CD4+ T lymphocytes | |
| DPP4 | 3.7 (5.4) | Dipeptidylpeptidase IV, a serine type peptidase, removes N-terminal X-Pro and X-Ala dipeptides from regulatory peptides | |
| HLA-DR beta 3 | 2.6 (0) | Major histocompatibility complex class II DR beta 3, a class II major histocompatibility complex antigen | |
| INDO | 2.6 (0) | Indoleamine-pyrrole 2−3 dioxygenase, catabolizes tryptophan, reduces tryptophan abundance and thereby suppresses T cell | |
| HLA-DR beta 5 | 2.5 (11.7) | Major histocompatibility complex class II DR beta 5, subunit of an MHC class II molecule | |
| HLA-DPA1 | 2.5 (12.7) | MHC class II DP alpha 1, subunit of the HLA-DP dimmer that functions as a major histocompatibility complex class II protein | |
| IL-7 | 6.8 (8.9) | Interleukin 7, a hematopoietic growth factor required for nomral growth and development of B cells and T cells | |
| SEMA3C | 2.5 (1.9) | Semaphorin 3C (semaphorin E), a member of the semaphorin family involved in neuronal growth cone guidance | |
| IGJ | −2.8 (−14.9) | Immunoglobulin J polypeptide, regulates polymer formation of immunoglobulins IgA and IgM, and helps promote their secretion | |
| CCL26 | −2.7 (0) | Eotaxin-3, a CC class chemokine and chemoattractant for basophils, eosinophils, T cells, and monocytes | |
| F3 | −2.7 (−65) | Coagulation factor III (tissue factor), integral membrane protein and receptor for factor VIIa (F7) | |
| CCL2 | −4.4 (−4.8) | Cytokine A2, CC chemokine that attracts monocytes, memory T-cells, natural killer cells and endothelial cells, plays a role in the inflammatory | |
| Lipid transport, catabolism and metabolism | |||
| MSR1 | 7.3 (48.4) | Macrophage scavenger receptor type I, binds and internalizes low-density lipoprotein and activates protein kinase C | |
| SCARA5 | 3.3 (75.3) | Scavenger receptor class A, member 5 | |
| CD36 | 4.3 (22.8) | An integral membrane receptor, binds thrombospondin, collagen, oxidized low density lipoprotein, long chain fatty acids | |
| HSD11B1 | 11.1 (12.7) | 11-beta-hydroxysteroid dehydrogenase type 1, catalyzes the interconversion of inactive cortisone and active cortisol | |
| PLA2G2A | 4.6 (4.7) | Phospholipase A2, group IIA (platelets, synovial fluid), nuclear gene encoding mitochondrial protein | |
| AKR1C2 | 3.3 (1.8) | Aldo keto reductase family 1 member C2, functions in bile transport, steroid metabolism, and xenobiotic metabolism | |
| AKR1C3 | 3.3 (2.2) | Aldo keto reductase family 1 member C3, a type 2 3 alpha (17 beta)-hydroxysteroid dehydrogenase | |
| NR2F2 | 3.0 (25.9 | Nuclear receptor subfamily 2 group F member 2, binds to hormone-responsive elements in APOB, APOA2, apoCIII | |
| ALDH1A3 | −4.7 (−3.6) | Aldehyde dehydrogenase 1 family member A3, catalyzes the oxidation of all-trans-retinaldehyde to retinoic | |
| PTGIS | −2.2 (−1.8) | Prostaglandin 12 synthase, a member of the cytochrome P450 family of proteins, converts prostaglandin H2 to the vasodilator | |
| Phosphate transport | |||
| MSR1 | 7.3 (48.4) | Macrophage scavenger receptor type I, binds and internalizes low-density lipoprotein and activates protein kinase C | |
| SCARA5 | 3.3 (75.3) | Scavenger receptor class A, member 5 | |
| COL8A1 | −2.5 (−2.5) | Alpha 1 subunit of type VIII collagen, contains a non-triple helical (NC1) domain which | |
| Miscellaneous | |||
| ENPP2 | 4.4 (5.2) | Ectonucleotide pyrophosphatase-phosphodiesterase 2, hydrolyzes nucleotides, lipids, generating pyrophosphate/phosphate. | |
| ENTPD1 | 2.8 (18.3) | Ectonucleoside triphosphate diphosphohydrolase 1, hydrolyzes extracellular ATP and ADP to AMP, generating pyrophosphate/phosphate | |
| ADCY3 | 2.8 (2.6) | Adenylyl cyclase 3, a membrane-associated ATP to cAMP-converting enzyme, generating pyrophosphate | |
| RAB27B | 4.3 (5.9) | Ras-related GTP-binding protein 27b, GTP-binding protein and GTPase, may be involved in exocytosis | |
| CES1 | 3.9 (6.2) | Carboxylesterase 1 (monocyte-macrophage serine esterase 1), hydrolyzes aromatic and aliphatic esters, expressed only in the monocyte-macrophage | |
| ADA | 3.2 (3.8) | Adenosine deaminase, plays a role in immune response, binds to CD26 (DPP4); deficiency causes a form of severe combined immunodeficiency |
Positive number indicates elevated expression (fold) in hTERT-OA 13A FLS (passage 8) compared to hTERT-RA 516 FLS (passage 8). Negative number indicates decreased expression (fold) in hTERT-OA 13A FLS (passage 8) compared to hTERT-RA 516 FLS (passage 8) or indicates elevated expression (fold) in hTERT-RA 516 FLS (passage 8) compared to hTERT-OA 13A FLS (passage 8). The number inside the parenthesis indicates the differential gene expressions detected using Affymetrix microarray between 25 passage hTERT-OA13A FLS and 25 passage hTERT-RA 516 FLS.
A distinct and notable differential gene expression pattern was the elevated expression of many genes classified into the biological process immune response in the hTERT-OA 13A FLS (passage 8) compared to hTERT-RA 516 FLS (passage 8). Of the 12 genes classified into the biological process immune response, 8 genes displayed elevated expressions and only 4 genes displayed decreased expression in hTERT-OA 13A FLS compared to hTERT-RA 516 FLS. Another notable differential gene expression pattern was the elevated expression of several genes associated with lipid transport, catabolism, and metabolism biological processes in the hTERT-OA 13A FLS compared to hTERT-RA 516 FLS.
Many genes implicated in calcification process in OA have been recently identified, including ectonucleotide pyrophosphatase-phosphodiesterase 1 (ENPP1/PC-1), ADCY3, progressive ankylosis homolog (ANKH), and tissue nonspecific alkaline phosphatase (TNSAP)22-25. These proteins share a common feature in that they are all in some way related to pyrophosphate. Interestingly, ADCY3, ENPP2, and ectonucleoside triphosphate diphosphohydrolase 1 (ENTPD1), which are related to pyrophosphate, were found to be expressed at elevated levels in the passage 8 hTERT-OA 13A FLS compared to passage 8 hTERT-RA 516 FLS (Table 1). The elevated expression of these 3 genes was also detected in passage 25 hTERT-OA 13A FLS (Table 1, column 3; the numbers inside the parentheses indicate the differential expression of these genes between passage 25 hTERT-OA 13A FLS and 25 passage hTERT-RA 516 FLS).
Validation of differential expression of selected genes
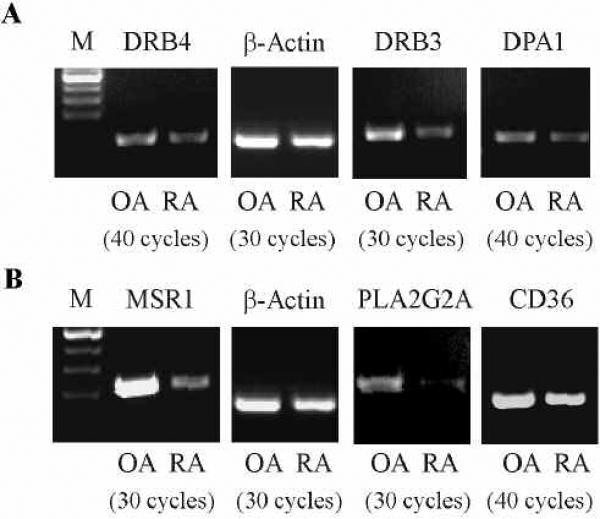
We carried out semiquantitative 6RT-PCR to validate the differential expression of 3 genes classified into the biological process immune response: major histocompatibility complex, class II, DR beta 4 (HLA-DRB4); MHC, class II, DR beta 3 (HLA-DRB3); and MHC, class II, DP alpha 1 (HLA-DPA). As shown in Figure 1, elevated expression of these 3 genes in passage 8 hTERT-OA 13A FLS compared to passage 8 hTERT-RA 516 FLS was confirmed. We also carried out semiquantitative RT-PCR to validate the differential expression of 3 genes involved in lipid transport and catabolism: macrophage scavenger receptor type 1 (MSR1), phospholipase A2 group IIA (PLA2G2A), and CD36 antigen (CD36). The differential expression of these 3 genes between hTERT-OA 13A FLS and hTERT-RA 516 FLS was also confirmed by semiquantitative RT-PCR (Figure 1).
Figure 1.
Validation of the differential expression of selected genes. hTERT-OA 13A FLS (passage 8) and hTERT-RA 516 FLS (passage 8) were plated in 100 mm plates at 60% confluence. On the second day, medium containing 10% serum was added and the cells cultured for another 24 h. RNA samples were extracted and examined by semiquantitative RT-PCR. A. The mRNA levels of HLA-DRB4, HLA-DRB3, HLA-DPA1, and ß-Actin. B. The mRNA levels of MSR1, PLA2G2A, CD36, and ß-Actin. Experiments were repeated at least 3 times and used 2 different RNA batches. Similar results were obtained.
Differential gene expression in longterm cultures of FLS
To determine the genotypic and phenotypic stability of hTERT-OA 13A FLS, and further investigate the differential gene expressions, a microarray experiment using Affymetrix HGU133_Plus_2 gene chips and RNA samples extracted from the longterm culture of hTERT-OA 13A FLS (passage 25) and hTERT-RA 516 FLS (passage 25) were performed. We decided to use Affymetrix microarray this time instead of Agilent microarray because we found that Agilent microarray was less sensitive than Affymetrix microarray in detecting differential gene expressions and Affymetrix HGU133_Plus_2 gene chip covers more transcripts (more than 50,000 transcripts) than Agilent human cDNA array B chip (22,605 transcripts). Of more than 50,000 transcripts examined, 2,033 genes that displayed differential gene expression (more than 2-fold) were identified; 895 genes were expressed at higher levels and 1,138 genes at lower levels in passage 25 hTERT-OA 13A FLS compared to passage 25 hTERT-RA 516 FLS (data not shown).
Differentially-expressed genes were classified according to gene ontology category biological process and selected results are listed in Table 2. We were particularly interested in identifying distinct differential gene expression patterns. As shown in Table 2, distinct differential gene expression patterns were apparent. For example, of the 62 differentially-expressed genes classified into the immune response biological process, 39 genes had elevated expressions and 23 genes had decreased expression in hTERT-OA 13A FLS compared to hTERT-RA 516 FLS. In other words, 39 genes had elevated expressions in hTERT-OA 13A FLS compared to hTERT-RA 516 FLS, and 23 genes had elevated expressions in hTERT-RA 516 FLS compared to hTERT-OA 13A FLS. Of the 15 differentially expressed genes classified into the phosphate transport biological process, 10 genes had an elevated expression and only 5 genes had decreased expression in hTERT-OA 13A FLS compared to hTERT-RA 516 FLS. Of the 14 genes classified into the lipid catabolic process/lipid transport biological processes, 11 genes had an elevated expression and only 4 genes had decreased expression in hTERT-OA 13A FLS compared to hTERT-RA 516 FLS. Of the 6 differentially expressed genes classified into the fatty acid metabolic process, 4 genes had an elevated expression and 2 genes had decreased expressions in hTERT-OA 13A FLS.
Table 2.
Selected differentially expressed genes detected by Affymetrix microarray.
| Funtional Family | Gene Name | Differ Expre (fold)* | Description |
|---|---|---|---|
| Proteolysis | |||
| MMP3 | 4.0 | Matrix metalloproteinase 3 | |
| MMP1 | 1.7 | Matrix metalloproteinase 1 | |
| CTSC | 4.9 | Cathepsin C | |
| CTSF | 2.1 | Cathepsin F | |
| CTSH | 3.7 | Cathepsin H | |
| CTSL | 2.5 | Cathepsin L | |
| CTSL | 1.8 | Cathepsin-L-like | |
| ADAM10 | 1.9 | Disintegrin and metalloproteinase domain 10 | |
| ADAM23 | 1.8 | Disintegrin and metalloproteinase domain 23 | |
| ADAM32 | 1.9 | Disintegrin and metalloprotease domain 32 | |
| PAPPA2 | 6.6 | Pappalysin 2 | |
| CFB | 2.2 | Complement factor B | |
| CFD | 2.7 | Complement factor D (adipsin) | |
| C1R | 1.8 | Cmplement component 1, r subcomponent | |
| C1S | 1.9 | Human complement subcomponent C1s, alpha- and beta-chains | |
| C5 | 3.8 | Complement component 5 | |
| PSMB9 | 2.7 | Proteasome (prosome, macropain) subunit, beta type, 9 | |
| PSMB10 | 2.7 | Proteasome (prosome, macropain) subunit, beta type, 10 | |
| FBXO6 | 3.6 | F-box protein 6 | |
| DPP4 | 5.4 | Dipeptidyl-peptidase 4 (CD26, adenosine deaminase complexing protein 2) | |
| MME | 4.2 | Membrane metallo-endopeptidase (neutral endopeptidase, enkephalinase) | |
| XPNPEP3 | 9.5 | X-prolyl aminopeptidase (aminopeptidase P) 3 | |
| CD55 | 3.3 | CD55 molecule, decay accelerating factor for complement | |
| FBXL2 | 4.8 | Lucine-rich repeat-containing F-box protein FBL2 mRNA | |
| UCHL1 | 4.5 | Ubiquitin carboxyl-terminal esterase L1 (ubiquitin thiolesterase) | |
| SERPING1 | 2.9 | Serpin peptidase inhibitor, clade G (C1 inhibitor), member 1 | |
| NAALADL1 | 2.6 | N-acetylated alpha-linked acidic dipeptidase-like 1 | |
| HTRA3 | 2.5 | HtrA serine peptidase 3 | |
| TMPRSS6 | 2.4 | Transmembrane protease, serine 6 | |
| LRP8 | 2.4 | Low density lipoprotein receptor-related protein 8, apolipoprotein e receptor | |
| AI671186 | 2.4 | Regeneration associated muscle protease | |
| CAPN7 | 2.2 | Calpain 7 | |
| SIAH1 | 2.2 | Seven in absentia homolog 1 (Drosophila) | |
| OMA1 | 2.1 | OMA1 homolog, zinc metallopeptidase (S. cerevisiae) | |
| AI671186 | 2.4 | DKFZP586H2123 protein | |
| UBE2E1 | 2.3 | Homo sapiens cDNA FLJ12000 fis, clone HEMBB1001531 | |
| AK000110 | 2.3 | Homo sapiens cDNA FLJ20103 fis, clone COL04793. | |
| SIAH1 | 2.1 | Seven in absentia (Drosophila) homolog 1 | |
| ESPL1 | 1.7 | Cluster Incl. D79987:Human mRNA for KIAA0165 gene | |
| MASP1 | 1.7 | ESTs, Highly similar to JN0883 Ra-reactive factor | |
| AI828007 | 1.8 | ESTs, Weakly similar to serin protease with IGF-binding motif | |
| CASP8 | 1.7 | Cspase 8, apoptosis-related cysteine protease (CASP8) | |
| CTRB1 | 1.7 | Cymotrypsinogen B1 | |
| USP32 | 1.8 | Homo sapiens mRNA for TL132 | |
| CLN8 | 1.8 | Putative transmembrane protein mRNA | |
| SENP1 | 1.8 | SntrinSUMO-specific protease 1 | |
| SENP7 | 1.7 | SntrinSUMO-specific protease 7 | |
| PYCARD | 1.8 | Homo sapiens, clone MGC:10332 | |
| UBE2C | 1.8 | Uiquitin carrier protein E2-C | |
| ADAMTS1 | −4.7 | ADAM metallopeptidase with thrombospondin type 1 motif 1 | |
| ADAMTS3 | −23.6 | ADAM metallopeptidase with thrombospondin type 1 motif 3 | |
| ADAMTS5 | −4.1 | ADAM metallopeptidase with thrombospondin type 1 motif 5 | |
| ADAM12 | −2.4 | ADAM metallopeptidase domain 12 (meltrin alpha) Adam 12 | |
| CPA4 | −2.5 | Carboxypeptidase A4 | |
| CPXM2 | −11.4 | Carboxypeptidase X (M14 family), member 2 | |
| CPZ | −3.0 | Carboxypeptidase Z | |
| CTSD | −3.6 | Cathepsin D | |
| CFH | −3.9 | Complement factor H | |
| CFI | −2.6 | Complement factor I | |
| C3 | −2.4 | Complement component 3 | |
| CASP2 | −2.1 | Caspase 2, apoptosis-related cysteine peptidase | |
| CASP8 | −5.0 | Caspase 8, apoptosis-related cysteine peptidase | |
| AGC1 | −8.6 | Aggrecan 1 | |
| AK023795 | −4.5 | Homo sapiens cDNA FLJ13733 fis, clone PLACE3000147 | |
| IBRDC2 | −7.4 | ESTs, Moderately similar to ALU1_HUMAN ALU SUBFAMILY J | |
| PPP4R2 | −3.7 | ESTs, Moderately similar to ALU7_HUMAN ALU SUBFAMILY SQ | |
| ABHD5 | −3.2 | Abhydrolase domain containing 5 | |
| QPCT | −3.5 | Glutaminyl-peptide cyclotransferase (glutaminyl cyclase) | |
| ENC1 | −2.7 | Ectodermal-neural cortex (with BTB-like domain) | |
| AEBP1 | −8.2 | AE binding protein 1 | |
| PCSK1 | −2.9 | Proprotein convertase subtilisin/kexin type 1 | |
| PLAU | −2.5 | Plasminogen activator, urokinase | |
| LRAP | −2.6 | Leukocyte-derived arginine aminopeptidase | |
| C9orf3 | −2.6 | Chromosome 9 open reading frame 3 | |
| SERPINE1 | −2.4 | Serpin peptidase inhibitor, clade E | |
| SERPINE2 | −2.0 | trinucleotide repeat containing 3 | |
| PCSK5 | −4.6 | Proprotein convertase subtilisin/kexin type 5 | |
| PRSS12 | −2.1 | Protease, serine, 12 (neurotrypsin, motopsin) | |
| DPP7 | −2.2 | Dipeptidyl-peptidase 7 | |
| KLKB1 | −2.1 | Homo sapiens cDNA FLJ12052 fis, clone HEMBB1002042 | |
| USP3 | −1.7 | Homo sapiens cDNA FLJ14136 fis, clone MAMMA1002744 | |
| USP12 | −1.8 | Ubiquitin specific protease 12 | |
| USP25 | −1.8 | Homo sapiens ubiquitin-specific processing protease | |
| USP53 | −2.6 | KIAA1350 protein | |
| U13022 | −1.8 | Cluster Incl. U13022:Human negative regulator of programmed cell death | |
| MASP1 | −1.8 | Mannan-binding lectin serine protease 1 | |
| UCHL3 | −1.8 | Ubiquitin carboxyl-terminal esterase L3 (ubiquitin thiolesterase) | |
| NLN | −1.7 | KIAA1226 protein | |
| RNF11 | −1.7 | Homo sapiens mRNA for Sid1669p, complete cds | |
| FBXO11 | −1.7 | Homo sapiens hypothetical protein FLJ12673 | |
| MALT1 | −1.7 | Homo sapiens clone 24631 mRNA | |
| FBXL7 | −1.7 | F-box and leucine-rich repeat protein 7 | |
| Immune response | |||
| HLA-DRA | 65.0 | Major histocompatibility complex, class II, DR alpha | |
| HLA-DRB1 | 50.2 | Major histocompatibility complex, class II, DR beta 1 | |
| HLA-DRB4 | 35.6 | Major histocompatibility complex, class II, DR beta 4 | |
| HLA-DRB5 | 11.7 | Major histocompatibility complex, class II, DR beta 5 | |
| HLA-DRB6 | 2.9 | Major histocompatibility complex, class II, DR beta 6 | |
| HLA-DPA1 | 12.7 | Major histocompatibility complex, class II, DP alpha 1 | |
| HLA-DPB1 | 4.7 | Major histocompatibility complex, class II, DP beta 1 | |
| HLA-DMA | 9.2 | Major histocompatibility complex, class II, DM alpha | |
| HLA-DQA1 | 7.1 | Major histocompatibility complex, class II, DQ alpha 1 | |
| CD77 | 4.7 | CD74 molecule, major histocompatibility complex, class II invariant chain | |
| IL1R1 | 2.1 | Interleukin 1 receptor, type I | |
| IL-7 | 8.9 | Interleukin 7 | |
| IL-7R | 2.4 | Interleukin 7 receptor | |
| NFIL3 | 2.3 | Nuclear factor, interleukin 3 regulated | |
| CXCL6 | 3.9 | Chemokine (C-X-C motif) ligand 6 (granulocyte chemotactic protein 2) | |
| CLCL2 | 2.8 | Chemokine (C-X-C motif) ligand 2 | |
| CCR1 | 2.3 | Chemokine (C-C motif) receptor 1 | |
| LST1 | 3.1 | Leukocyte specific transcript 1 | |
| IFIH1 | 2.2 | Interferon induced with helicase C domain 1 | |
| IFIT3 | 2.1 | Interferon-induced protein with tetratricopeptide repeats 3 | |
| C5 | 3.8 | Complement component 5 | |
| CFB | 2.2 | Complement factor B | |
| CFD | 2.7 | Complement factor D (adipsin) | |
| CD55 | 3.3 | CD55 molecule, decay accelerating factor for complement | |
| CD55 | 3.3 | CD55 molecule, decay accelerating factor for complement | |
| PSMB10 | 2.7 | Proteasome (prosome, macropain) subunit, beta type, 10 | |
| PSMB9 | 2.7 | Proteasome (prosome, macropain) subunit, beta type, 9 | |
| BST1 | 3.7 | Bone marrow stromal cell antigen 1 | |
| BST2 | 3.7 | Bone marrow stromal cell antigen 2 | |
| COLEC12 | 2.5 | Collectin sub-family member 12 | |
| KIR3DL1 | 3.9 | Killer cell immunoglobulin-like receptor, three domains | |
| KIR2DL1 | 4.5 | Killer cell immunoglobulin-like receptor, two domains | |
| OAS1 | 2.3 | 2,5-oligoadenylate synthetase 1, 40/46kDa | |
| TRIM22 | 2.1 | Tripartite motif-containing 22 | |
| DPP4 | 5.4 | Dipeptidyl-peptidase 4 (CD26, adenosine deaminase complexing protein 2) | |
| SECTM1 | 5.7 | Secreted and transmembrane 1 | |
| CTSC | 5.0 | Cathepsin C | |
| ADA | 3.8 | Adenosine deaminase | |
| ETS1 | 3.0 | V-ets erythroblastosis virus E26 oncogene homolog 1 (avian) | |
| IGHG1 | 2.1 | Immunoglobulin heavy constant gamma 1 (G1m marker) | |
| IL-11 | −2.7 | Interleukin 11 | |
| IL-26 | −9.9 | Interleukin 26 | |
| TIRAP | −2.0 | Toll-interleukin 1 receptor (TIR) domain containing adaptor protein | |
| IL1RL1 | −3.3 | Interleukin 1 receptor-like 1 | |
| TGFB1 | −2.5 | Transforming growth factor, beta 1 | |
| TGFB2 | −2.7 | Transforming growth factor, beta 2 | |
| CFH | −3.9 | Complement factor H | |
| CFI | −2.6 | Complement factor I | |
| C3 | −2.4 | Complement component 3 | |
| TNFRSF9 | −2.6 | Tumor necrosis factor receptor superfamily, member 9 | |
| TNFRSF11A | −3.3 | Tumor necrosis factor receptor superfamily, member 11a, NFKB activator | |
| CD24 | −16.5 | CD24 molecule | |
| IFI27 | −12.5 | Interferon, alpha-inducible protein 27 | |
| F3 | −6.5 | Coagulation factor III (thromboplastin, tissue factor) | |
| PTGER4 | −5.8 | Prostaglandin E receptor 4 (subtype EP4) | |
| CCL2 | −4.8 | Chemokine (C-C motif) ligand 2 | |
| PDCD1LG2 | −3.6 | Programmed cell death 1 ligand 2 | |
| PAWR | −3.4 | PRKC, apoptosis, WT1, regulator | |
| IGSF4 | −2.9 | Immunoglobulin superfamily, member 4 | |
| TRPM4 | −2.3 | Transient receptor potential cation channel, subfamily M, member 4 | |
| SMAD3 | −2.1 | SMAD family member 3 | |
| ARL6IP2 | −2.0 | ADP-ribosylation factor-like 6 interacting protein 2 | |
| OAS2 | −2.3 | 2−5-oligoadenylate synthetase 2, 69/71kDa | |
| Phosphate transport | |||
| MSR1 | 48.4 | Macrophage scavenger receptor 1 | |
| SCARA5 | 75.3 | Scavenger receptor class A, member 5 (putative) | |
| COL1A2 | 2.2 | Collagen, type I, alpha 2 | |
| COL3A1 | 2.6 | Collagen, type III, alpha 1 | |
| COL5A3 | 11.3 | Collagen, type V, alpha 3 | |
| COL8A1 | −2.5 | Collagen, type VIII, alpha 1 | |
| COL8A2 | 6.2 | Collagen, type VIII, alpha 2 | |
| COL11A1 | −4.0 | Collagen, type XI, alpha 1 | |
| COL12A1 | 2.4 | Collagen, type XII, alpha 1 | |
| COL13A1 | −2.1 | Collagen, type XIII, alpha 1 | |
| COL15A1 | 5.9 | Collagen, type XV, alpha 1 | |
| CCBE1 | 2.4 | Collagen and calcium binding EGF domains 1 | |
| COLEC12 | 2.5 | Collectin sub-family member 12 | |
| GLDN | −6.2 | Gliomedin | |
| ANKH | −3.2 | Ankylosis, progressive homolog (mouse) | |
| Lipid catabolic process | |||
| PLA2G2A | 4.7 | Phosphatase A2, group IIA (platelets, synovial fluid) | |
| PLA2G4C | 3.5 | Phospholipase A2, group IVC (cytosolic, calcium-independent) | |
| PPT1 | 3.0 | Palmitoyl-protein thioesterase 1 | |
| WNT1 | 3.0 | WNT1 inducible signaling pathway protein 2 | |
| LIPC | 2.6 | Lipase, hepatic | |
| FLRT2 | 2.5 | Fibronectin leucine rich transmembrane protein 2 | |
| PLCB4 | −3.8 | Phospholipase C, beta 4 | |
| Lipid transport | |||
| APOL6 | 2.8 | Apolipoprotein L, 6 | |
| SLC27A3 | 3.3 | Solute carrier family 27 (fatty acid transporter), member 3 | |
| OSBPL1A | 2.2 | Oxysterol binding protein-like 1A | |
| STARD3 | 2.5 | START domain containing 3 | |
| APOL3 | 2.3 | Apolipoprotein L, 3 | |
| STARD5 | −2.3 | START domain containing 5 | |
| ATP8A1 | −2.2 | ATPase, aminophospholipid transporter, Class I, type 8A, member 1 | |
| Fatty acid metabolic process | |||
| CD36 | 22.8 | CD36 molecule (thrombospondin receptor) | |
| PNPLA8 | 3.7 | Patatin-like phospholipase domain containing 8 | |
| CYB5A | 2.4 | Cytochrome b5 type A (microsomal) | |
| HADHA | 2.1 | Hydroxyacyl-Coenzyme A dehydrogenase, alpha | |
| ACSL5 | −3.1 | Acyl-CoA synthetase long-chain family member 5 | |
| ACSL1 | −2.1 | Acyl-CoA synthetase long-chain family member 1 | |
| Cytoskeleton-dependent intracellular transport | |||
| KIF14 | 2.2 | Kinesin family member 14 | |
| KIF15 | 2.3 | Kinesin family member 15 | |
| KIF18A | 2.4 | Kinesin family member 18A | |
| KIF23 | 2.5 | Kinesin family member 23 | |
| MYO1E | 2.5 | Myosin IE | |
| MYO9B | 2.4 | Myosin IXB | |
| RHOT1 | 2.3 | Ras homolog gene family, member T1 | |
| UCHL1 | 4.5 | Ubiquitin carboxyl-terminal esterase L1 (ubiquitin thiolesterase) | |
| MYRIP | −15.8 | Myosin VIIA and Rab interacting protein | |
| TUBA1 | −3.5 | Tubulin, alpha 1 | |
| KIFI13 | −2.1 | Kinesin family member 1B | |
| Positive regulation of cell proleferation | |||
| IL-7 | 8.9 | Interleukin 7 | |
| LAMA1 | 2.9 | Laminin, alpha 1 | |
| LAMC1 | 2.8 | Laminin, gamma 1 (formerly LAMB2) | |
| ADRA2A | 10.5 | Adrenergic, alpha-2A-, receptor | |
| 1RS2 | 4.0 | Insulin receptor substrate 2 | |
| SSR1 | 2.5 | Signal sequence receptor, alpha (translocon-associated protein alpha) | |
| CDC25B | 2.9 | Cell division cycle 25 homolog B (S. cerevisiae) | |
| LRP5 | 2.6 | Low density lipoprotein receptor-related protein 5 | |
| PBEF1 | 2.3 | Pre-B-cell colony enhancing factor 1 | |
| P21 | 2.0 | Cyclin-dependent kinase inhibitor 1A (p21, Cip1) | |
| FGF2 | −3.3 | Fibroblast growth factor 2 (basic) | |
| FGF9 | −19.1 | Fibroblast growth factor 9 (glia-activating factor) | |
| FGF10 | −2.0 | Fibroblast growth factor 10 | |
| TGFB1 | −2.5 | Transforming growth factor, beta 1 | |
| TGFB2 | −2.6 | Transforming growth factor, beta 2 | |
| TGFBR1 | −2.6 | Transforming growth factor, beta receptor I | |
| ID4 | −4.1 | Inhibitor of DNA binding 4, dominant negative helix-loop-helix protein | |
| LYN | −5.1 | V-yes-1 Yamaguchi sarcoma viral related oncogene homolog | |
| J05008 | −4.8 | Endothelin 1 | |
| CSF1 | −3.3 | Colony stimulating factor 1 (macrophage) | |
| PDCD1LG2 | −3.6 | Programmed cell death 1 ligand 2 | |
| CLEC11A | −3.8 | C-type lectin domain family 11, member A | |
| PTHLH | −4.3 | Parathyroid hormone-like hormone | |
| BNC1 | −3.2 | Basonuclin 1 | |
| PTN | −3.3 | Pleiotrophin (heparin binding growth factor 8) | |
| ERPB2 | −3.7 | V-erb-b2 erythroblastic leukemia viral oncogene homolog 2 | |
| VEGFC | −3.6 | Vascular endothelial growth factor C | |
| TNFRSF11A | −3.3 | Tumor necrosis factor receptor superfamily, member 11a, NFKB activator | |
| HBEGF | −3.0 | Heparin-binding EGF-like growth factor | |
| IL-11 | −2.7 | Interleukin 11 | |
| EDG3 | −2.7 | Endothelial differentiation, sphingolipid G-protein-coupled receptor, 3 | |
| IGF1R | −2.4 | Insulin-like growth factor 1 receptor | |
| STAMBP | −2.1 | STAM binding protein | |
| LAMB1 | −2.1 | Laminin, beta 1 | |
| Anti-apoptosis | |||
| ATF5 | 4.9 | Activating transcription factor 5 | |
| SERPINB9 | 4.7 | Serpin peptidase inhibitor, clade B (ovalbumin), member 9 | |
| HRK | 3.1 | Harakiri, BCL2 interacting protein (contains only BH3 domain) | |
| BRE | 2.1 | Brain and reproductive organ-expressed (TNFRSF1A modulator) | |
| BIRC6 | 2.0 | Baculoviral IAP repeat-containing 6 (apollon) | |
| SERPINB2 | −17.3 | Serpin peptidase inhibitor, clade B (ovalbumin), member 2 | |
| CCL2 | −4.8 | Chemokine (C-C motif) ligand 2 | |
| TNFRSF10D | −3.1 | TNF receptor superfamily, member 10d, decoy with truncated death domain | |
| SFRP1 | −3.1 | Secreted frizzled-related protein 1 | |
| ERC1 | −3.1 | ELKS/RAB6-interacting/CAST family member 1 | |
| U37546 | −3.4 | Baculoviral IAP repeat-containing 3 | |
| IGF1R | −2.3 | Insulin-like growth factor 1 receptor | |
| BCL2A1 | −2.4 | BCL2-related protein A1 | |
| DHCR24 | −2.3 | 24-dehydrocholesterol reductase | |
| POGK | −2.3 | Pogo transposable element with KRAB domain | |
| BNIP3 | −2.2 | BCL2/adenovirus E1B 19kDa interacting protein 3 | |
| CASP2 | −2.1 | Caspase 2, apoptosis-related cysteine peptidase | |
| TNFAIP3 | −2.1 | Tumor necrosis factor, alpha-induced protein 3 | |
| STAM | −2.1 | STAM binding protein | |
| HDAC1 | −2.1 | Histone deacetylase 1 | |
| HTATIP2 | −2.1 | HIV-1 Tat interactive protein 2, 30kDa | |
| HSPB1 | −2.0 | Heat shock 27kDa protein 1 | |
| Angiogenesis | |||
| SERPINF1 | 6.3 | Serpin peptidase inhibitor, clade F, member 1 | |
| COL15A1 | 5.9 | Collagen, type XV, alpha 1 | |
| ARTS-1 | 5.8 | Type 1 tumor necrosis factor receptor shedding aminopeptidase regulator | |
| PLXND1 | 2.5 | Plexin D1 | |
| TMPRSS6 | 2.4 | Transmembrane protease, serine 6 | |
| ANGPT1 | −3.5 | Angiopoietin 1 | |
| VEGFC | −3.6 | Vascular endothelial growth factor C | |
| EDNRA | −3.0 | Endothelin receptor type A | |
| FGF1 | −2.1 | Fibroblast growth factor 1 (acidic) | |
| FGF2 | −3.3 | Fibroblast growth factor 2 (basic) | |
| CTGF | −4.7 | Connective tissue growth factor | |
| RUNX1 | −2.1 | Runt-related transcription factor 1 | |
| THBS1 | −3.3 | Thrombospondin 1 | |
| TGFB2 | −2.6 | Transforming growth factor, beta 2 | |
| ERBB2 | −3.7 | V-erb-b2 erythroblastic leukemia viral oncogene homolog 2 (avian) | |
| HBEGF | −3.0 | Heparin-binding EGF-like growth factor | |
| SEPPINB8 | −2.1 | Serpin peptidase inhibitor, clade E, member 1 | |
| HTATIP2 | −2.1 | HIV-1 Tat interactive protein 2, 30kDa | |
| JAG1 | −2.0 | Jagged 1 (Alagille syndrome) | |
| BMP4 | −2.0 | Bone morphogenetic protein 4 |
Positive number indicates elevated expression (fold) in hTERT-OA 13A FLS (passage 25) compared to hTERT-RA 516 FLS (passage 25). Negative number indicates decreased expression (fold) in hTERT-OA 13A FLS (passage 25) compared to hTERT-RA 516 FLS (passage 25) or indicates elevated expression (fold) in hTERT-RA 516 FLS (passage 25) compared to hTERT-OA 13A FLS (passage 25).
In contrast, the genes that had elevated expressions in hTERT-RA 516 FLS fell into a different category of biological processes. For example, of the 34 differentially expressed genes classified into the positive regulation of cell proliferation biological process, 24 genes had an elevated expression and only 10 genes had decreased expression in hTERT-RA 516 FLS compared to hTERT-OA 13A FLS. Of the 22 differentially expressed genes classified into the anti-apoptosis biological process, 17 genes had an elevated expression and only 5 genes had a decreased expression in hTERT-RA 516 FLS compared to hTERT-OA 13A FLS. Of the 20 differentially expressed genes classified into the angiogenesis biological process, 15 genes had an elevated expression in hTERT-RA 516 FLS and only 5 genes had decreased expression. These distinct distributions of the differentially-expressed genes in different sets of biological processes suggest that OA 13A FLS and hTERT-RA 516 FLS have definitely different cellular properties and activities.
Validation of differential expression of selected genes by real-time RT-PCR
The genes selected for validation included MHC, class II, DR alpha (HLA-DRA), microsomal glutathione S-transferase 1 (MGST1), matrix metalloproteinase (MMP)1, 3 rab genes and 2 collagen genes. A disintegrin and metalloproteinase with thrombospondin type 1 motif (ADAMTS1), which was expressed at a lower level in both the passage 8 and passage 25 hTERT-OA 13A FLS compared to hTERT-RA 516 FLS, was also selected for validation. The results of quantitative real-time RT-PCR are listed in Table 3. As shown, the differential expression of these genes in the longterm culture of hTERT-OA 13A FLS and hTERT-RA 516 FLS were confirmed by quantitative real-time RT-PCR.
Table 3.
Differential expression detected by microarray versus that detected by real-time RT-PCR between hTERT-OA 13AFLS and hTERT-RA 516 FLS. Numbers are the ratio of the relative expression level of a gene in hTERT-OA 13A FLS to the relative expression level of a gene in hTERT-RA 516 FLS.
| Gene | Microarray (passage 8) | Microarray (passage 25) | RT-PCR (passage 25) | Description |
|---|---|---|---|---|
| HLA-DRA | 2.5 | 82 | 89.6 | Major histocompatibility complex, class II, DR alpha |
| MGST1 | 4.5 | 164 | 230.1 | Microsomal glutathione S-transferase 1 |
| RAB27B | 4.3 | 6.8 | 16.6 | Ras-related GTP-binding protein 27b, GTP-binding protein and GTPase |
| MMP1 | – | 1.74 | 5.2 | Matrix metalloproteinase 1 |
| COL5A3 | – | 11.38 | 12.41 | Collagen, type III, Alpha 1 |
| COL8A2 | – | 8.04 | 12.28 | Collagen, type V, alpha 3 |
| ADAMTS1 | 0.16 | 0.20 | 0.36 | ADAM metallopeptidase with thrombospondin type 1 motif 1 |
DISCUSSION
In our study, we demonstrate that hTERT-OA 13A FLS display a stable differential gene expression profile compared to hTERT-RA 516 FLS. Of the 62 genes that were detected with elevated expressions in passage 8 hTERT-OA 13A FLS compared to passage 8 hTERT-RA 516 FLS, 43 genes (69%) showed elevated expression in passage 25 hTERT-OA 13A FLS compared to passage 25 hTERT-RA 516 FLS. All the genes listed in Table 1 which displayed elevated expression in passage 8 hTERT-OA 13A FLS were found to display elevated expression in passage 25 hTERT-OA 13A FLS with the exception of HLA-DRB3, indoleamine-pyrrole 2−3 dioxygenase (INDO) and CCL26/eotaxin-3 (Table 1). There was no elevated expression of HLA-DRB3, INDO, and CCL26/eotaxin-3 detected in passage 25 hTERT-OA 13A FLS (Table 1).
As hTERT-OA 13A FLS and hTERT-RA 516 FLS contain no other types of cells, the differential expressions between hTERT-OA 13A FLS and hTERT-RA 516 FLS may reflect the FLS-specific “true” disease characteristics of OA 13A FLS and RA 516 FLS. In addition, because the differential expression of a majority of genes remains largely unchanged with time, telomerase transduced FLS offer a valuable tool for the study of arthritis-derived FLS and for the identification of disease candidate genes.
MMP, cathepsins, and ADAMS are all implicated in arthritis3,8,26-30. MMP-1 and MMP13 degrade type II collagen. MMP2, MMP3, MMP9, and ADAMTS degrade proteoglycans. Our microarray data revealed that a similar number of genes encoding proteolytic proteins was expressed at higher levels in hTERT-OA 13A FLS (49 genes) (Table 2, column 3, the positive numbers) and in hTERT-RA 516 FLS (44 genes) (Table 2, column 3, the negative numbers), indicating that proteolytic proteins play an important role in both OA and RA. However, the functional family classifications of the upregulated genes in hTERT-OA 13A FLS were different from the functional family classifications of the upregulated genes in hTERT-RA 516 FLS. MMP3, MMP1, and several cathepsins were expressed at higher levels in hTERT-OA 13A FLS compared to hTERT-RA 516 FLS (Table 2, column 3, the positive numbers). In contrast, ADAMTS5, ADAMTS3, ADAMTS1, and several carboxypeptidases were expressed at higher levels in hTERT-RA 516 FLS compared to hTERT-OA 13A FLS (Table 2, column 3, the negative numbers). The findings that ADAMTS5 and ADAMTS1 are expressed at decreased levels in hTERT-OA 13A FLS compared to hTERT-RA 516 FLS are consistent with a previous finding that ADAMTS5 and ADAMTS1 are expressed at decreased levels in OA synovium and OA articular cartilage31. These findings together suggest that OA FLS may be involved in the degradation of both proteoglycans and type II collagen, and that RA FLS may be mainly involved in the degradation of proteoglycans, consistent with the clinical observations that degradation of type II collagen in articular cartilage is much more prominent in OA than in RA except at the pannus-cartilage junction. At the pannus-cartilage junction, RA FLS may be involved in the degradation of collagen by secreting inflammatory cytokines and stimulating the expression of collagen II degrading enzymes by articular chondrocytes.
In addition to MMP and ADAMS, many other genes previously found to be aberrantly expressed in OA were detected in our study. They include PLA232, collagen, type XI, alpha 1 (COL11A1)33,34, ANKH35,36, interleukin (IL)-737, IL1 receptor alpha 1 (IL1R1)16, fibronectin 1 (FN1)16, human complement subcomponent C1s (C1S)38, and v-ets erythroblastosis virus E26 oncogene homolog 1 (ETS1)39. PLA2 is expressed at higher or similar levels in OA joint tissues compared with RA joint tissues, and may play a role in inflammation32. Decreased expression of COL11A1 due to a mutation has been shown to cause OA-like changes including reduced mechanical function of articular cartilage and increased degradation of type II collagen33,34. IL-7 is expressed in OA chondrocytes and the expression of collagen-degrading enzymes such as MMP13 is induced by IL-737. Lost-function mutations of ANKH cause calcification and degeneration of articular cartilage35,36. Aberrant expression of IL1R1 and FN1 are potential disease markers of OA16. C1S and ETS1 have been implicated in RA40,41. The consistency between our findings and previous findings provides further support for the hypothesis that OA FLS is not a bystander in OA. In addition, it suggests the validity of our approach to the study of OA FLS, and our approach to the identification of potential disease candidate genes using telomerase transduced OA FLS.
OA is recognized as having a genetic component. Many genes harboring susceptibility for primary OA have been recently identified through genome-wide linkage scan of genetic polymorphisms and association analysis. We recently did a literature search for these genes. The genes we found from published articles are listed in Table 6. Incredibly, of the 28 genes harboring susceptibility for primary OA, 11 genes (39%) are detected in our study and are differentially expressed between hTERT-OA 13A FLS and hTERT-RA 516 FLS (Table 4). This match not only demonstrates that telomerase transduced FLS is a valuable tool for the study of arthritis derived FLS but also provides further support for the previous findings that ADAM metallopeptidase domain 12 (ADAM12), ADAMTS-5, asporin (ASPN), cartilage oligomeric matrix protein (COMP), deiodinase type II (DIO2), ENPP1, estrogen receptor 1 (ESR1), growth differentiation factor 5 (GDF5), isocitrate dehydrogenase (IDH1), neuropilin 2 (NRP2), and matrilin 3 (MATN3) harbor susceptibility for primary OA.
Table 6.
Comparison of the differential expressions of genes detected in our study with those previously reported17.
| Gene | Differential Expression* | Differential Expression** | Description |
|---|---|---|---|
| LILRB1 | ↓ | ↓ | Leukocyte immunoglobulin-like receptor, subfamily A |
| C9orf47 | ↓ | ↓ | Endo differentiation, sphingolipid G-protein-coupled receptor, 3 |
| NRN1 | ↓ | ↓ | Homo sapiens neuritin |
| PLCB4 | ↓ | ↓ | Phospholipase C, beta 4 |
| GATA6 | ↓ | ↓ | Homo sapiens mRNA for GATA-6 |
| THY1 | ↓ | ↓ | Thy-1 cell surface antigen |
| LRRC15 | ↓ | ↓ | Leucine-rich repeat containing 5 |
| MAB21L2 | ↑ | ↑ | Homo sapiens MAB21L2 protein |
| CES1 | ↑ | ↑ | Carboxylesterase |
| SFRP2 | ↑ | ↑ | Secreted frizzled-related protein 2 |
| SEMA3A | ↓ | ↑ | Sema domain, immunoglobulin domain (Ig), (semaphorin) 3A |
| SFRP1 | ↓ | ↑ | Secreted frizzled-related protein 1 |
| LMO2 | ↓ | ↑ | LIM domain only 2 |
| CRLF1 | ↓ | ↑ | Cytokine receptor-like factor 1 |
| TMOD1 | ↓ | ↑ | Homo sapiens, tropomodulin |
| PRG4 | ↓ | ↑ | Proteoglycan 4 |
| HLA-DQA1 | ↑ | ↓ | MHC class II, DQ alpha 1 |
| HLA-DRA | ↑ | ↓ | MHC class 22 HLA-DR-alpha |
| HLA-DRB4 | ↑ | ↓ | MHC class II DR beta 4 |
| CTSC | ↑ | ↓ | Cathepsin C |
| TBX5 | ↑ | ↓ | ESTs, AW269421 |
| HOXD13 | ↑ | ↓ | Homeo box D13 |
| BST1 | ↑ | ↓ | Bone marrow stromal cell antigen 1 |
This study.
Previously reported17.
↑ indicates elevated expression in hTERT-OA 13A FLS (passage 25) compared to hTERT-RA 516 FLS (passage 25) or in primary OA FLS (passage 2−3) compared to primary RA FLS (passages 2−3). ↓ indicates decreased expression in hTERT-OA 13A FLS (passage 25) compared to hTERT-RA 516 FLS (passage 25) or in primary OA FLS (passages 2−3) compared to primary RA FLS (passages 2−3).
Table 4.
Genes harboring susceptibility for OA, and their differential expressions between hTERT-OA 13A FLS (25 passages) and hTERT-RA 516 FLS (25 passages).
| Gene | Differential Expression |
|---|---|
| AACT (1) | |
| ADAM12 (1) | −2.4 |
| ADAMTS-5 (2) | −4.1 |
| ASPN (3) | 2.1 |
| BMP2 (1) | |
| CALM1 (3) | |
| CLIP (1) | |
| COL2A1 (3) | |
| COMP (3) | −3.3 |
| COX2 (1) | |
| DIO2 (4) | −3.6 |
| ENPP1 (5) | 1.5 |
| ESR1 (1) | 1.6 |
| FRZB (3) | |
| GDF5 (6) | −1.5 |
| IDH1 (7) | 1.6 |
| IL-1 (8) | |
| ILR4 (9) | |
| NRP2 (7) | −1.6 |
| MATN3 (2) | −2.1 |
| OPG (1) | |
| PLA2G4A (10) | |
| PTGS2 (10) | |
| RHOB (11) | |
| TNA (1) | |
| TXNDC3 (11) | |
| VDR (1) |
Genes harboring susceptibility for OA from the literature: (1) Arthritis Rheum 2006; 54:533−9. (2) Arthritis Rheum 2008; 58:435−41. (3) Arthritis Rheum 2007; 56:137−46. (4) Hum Mol Genet 2008; 17:1867−75. (5) Arthritis Res Ther 2005; 7:R1082−90. (6) Hum Mol Genet 2008; 17:1497−504. (7) Eur J Hum Genet 2007; 15:791−9. (8) Arthritis Rheum 2004; 50:1179−86. (9) Expert Rev Mol Med 2005; 7:1−12. (10) AM J Hum Genet 2008; 82:1231−40. (11) Am J Hum Genet 2006; 78:793−803.
Phosphate-containing crystals are detected in synovial fluid of up to 70% of patients with OA. These crystals may accelerate the progression of OA42-45. It has been reported that phosphate plays a role in IL-8 induced hypertrophy of articular chondrocytes46, and that phosphate affects growth plate chondrocyte maturation, apoptosis, and mineralization47,48. In our study, we found that many genes involved in phosphate transport were highly expressed in hTERT-OA 13A FLS (Tables 1 and 2). This distinct differential gene expression pattern suggests that the regulation of phosphate in OA FLS is different from that in RA FLS. Interestingly, several genes implicated in promoting or inhibiting pathological calcification are also expressed at higher levels in passage 25 hTERT-OA 13A FLS compared to passage 25 hTERT-RA 516 FLS including ENPP1 (1.5-fold), ENPP2 (5.2-fold), ENTPD1 (18.3-fold), and ADCY3 (2.6-fold). Although the implication of these differential gene expression patterns is unclear at present, it warrants further study because the deposition of phosphate-containing crystals in the knee joints of patients with OA is a prominent clinical phenomenon.
Increasing evidence suggests that oxidized low density lipoproteins (ox-LDL) may play a role in the pathogenesis of OA49,50. The percentage of ox-LDL-positive chondrocytes is much higher in OA chondrocytes and correlates with OA grade51,52. Because phospholipid is one of the components of ox-LDL, and has been implicated in calcification53,54, elevated transport and catabolism of ox-LDL may disturb local homeostasis of phosphate and play a role in pathological calcification. Interestingly, our microarray data revealed that many genes involved in the transport and catabolic process of lipids and ox-LDL were expressed at higher levels in hTERT-OA 13A FLS (Table 2), suggesting a possible involvement of synovial lipids and ox-LDL in the disease process of OA.
Our microarray data also revealed distinct distributions of the genes classified into the positive regulation of cell proliferation biological process including fibroblast growth factor (FGF)2, FGF9, and FGF10, the anti-apoptosis biological process including secreted frizzled-related protein 1 (SFRP1), bcl-2-related protein A1 (BCL2A1), and tumor necrosis factor receptor-related receptor for TRAIL (TNFRSF10D/TRAIL receptor 4) and the angiogenesis biological process including angiopoietin 1 (ANGPT1), vascular endothelial growth factor C (VEGFC), FGF1, and connective tissue growth factor (CTGF) (Table 2). These distinct distributions appear consistent with the clinical observations that severe synovial hyperplasia occurs in RA but not in OA, suggesting an abnormal regulation of proliferation, apoptosis, and angiogenesis in RA FLS. On the other hand, apoptosis of articular chondrocytes has been implicated in OA. The decreased release by OA FLS of certain soluble factors involved in above 3 biological processes may have certain effects on the survival of articular chondrocytes in OA. This subject may warrant further study.
Kato, et al16 reported that the differential expression of selected genes between OA synovium and RA synovium might be used as a synovial disease marker of OA. Significantly, of the proposed 12 group I candidate biomarkers, 7 (58%) were detected in this study, and 5 displayed similar differential gene expressions (Table 5). Of the proposed 9 group II candidate biomarkers, 5 (56%) were detected in our study (Table 5). The consistency between our findings and the previous report16 suggests that human telomerase-transduced OA FLS display a disease-specific gene expression profile. In addition, this supports the application of selected differential gene expressions as disease markers of OA.
Table 5.
Comparison of the differential expressions of putative disease markers.
| Gene | Differential Expression* (hTERT-OA 13A FLS/hTERT-RA 516 FLS) (passage 25) | Gene Name | Differential Expression** (OA synovium/RA synovium) | Mean Absolute Deviation**† | Description |
|---|---|---|---|---|---|
| Group I | |||||
| IL1R1 | 2.05 | ILIR1 | 2.15 | Interleukin 1 receptor, type I | |
| P4HA2 | 2.37 | P4HA2 | 1.93 | Procollagen-proline, 2-oxoglutarate 4-dioxygenase | |
| COL3A1 | 2.35 | COL3A1 | 1.96 | Collagen, type III, alpha 1 | |
| SORD | 0.49 | SORD | 0.59 | Hyman L-iditol-2 dehydrogenase | |
| PGK1 | 0.58 | PGK1 | 0.24 | Phosphoglycerate kinase (alternatively spliced) | |
| EXT1 | 2.47 | EXT1 | 0.61 | Homo sapiens insert cDNA clone YP87D03. | |
| LIMK2 | 0.36 | LIMK2 | 1.38 | LIM domain kinase 2, transcript variant 2a | |
| Group II | |||||
| RPL15 | 2.23 | NA | NA | 1.4 | ESTs, AI939308 |
| CXCL2 | 2.82 | NA | 1.32 | Human gro-beta mRNA, complete cds | |
| GSTT1 | 1.78 | NA | 1.30 | Glutathione S-transferase theta 1 | |
| PPP2R5C | 1.65 | NA | 1.42 | Homo sapiens mRNA; cDNA DKFZp761H0317 | |
| FN1 | 0.40 | NA | 1.40 | Homo sapiens mRNA for MSF-FN70 (FN gene) |
This study. Numbers are the ratio of the relative expression level of a gene in hTERT-OA 13A FLS to relative expression level of a gene in hTERT-RA 516 FLS.
Previously reported16. Numbers are the ratio of the relative expression level of a gene in OA synovium to relative expression level of a gene in RA synovium.
Mean absolute deviation of the expression levels of a gene in OA synovium from the mean of the expression levels of a gene in normal synovium. Group I: The genes that displayed either elevated expression or decreased expression in all OA synovium samples compared to all RA synovium samples. Group II: The genes that displayed greater differential gene expression (judged by mean absolute deviation) between OA synovium and RA synovium, although in some OA synovium samples expression of the gene of interest was up and in other OA synovium samples expression was down compared to RA synovium samples16.
Our findings are consistent with many clinical observations and previous experimental data; however, unexpected findings were also uncovered. OA is a degenerative disease, whereas RA is an abnormal immune response disease. Naturally, one would expect that the number of immune response genes displaying elevated expressions in RA FLS would outnumber the number of immune response genes displaying elevated expressions in OA FLS. However, we observed the opposite. A possible explanation for this unexpected finding is that OA 13A FLS possess certain traits of macrophage-like synoviocytes (MLS). The elevated expression of HLA-DPA1, HLA-DRB4, HLA-DQA1, and carboxylesterase 1/monocyte-macrophage serine esterase 1 (CES1) in hTERT-OA 13A FLS provides support for this explanation55. Recently it has been shown that synovial macrophages mediate the formation of osteophyte in OA56. It is worth noting that the association of osteophytes with OA may be partially explained by our finding that OA FLS possess certain traits of MLS. OA-FLS, together with OA-MLS, may promote the formation of osteophyte. However, further study is needed to examine the role of OA FLS in the formation of osteophytes.
Galligan, et al17 recently reported that 287 differentially expressed genes were detected between OA FLS and RA FLS. Among these genes, 67 genes displayed significant differential gene expressions from control base line. Of the 67 genes, 23 (34%) are detected in our study. However, only 10 genes (44%) among the 23 displayed similar differential gene expressions; 7 had decreased expression and 3 had elevated expression in OA FLS compared to RA FLS (Table 6, the 3 columns from the left). The other 13 genes display opposite differential gene expressions (Table 6, the 3 columns from the right). One possible explanation for this “inconsistency” is that primary FLS of passages 2−3 may contain up to 5% of other types of cells, but telomerase-transduced FLS contain no other types of cells. The elevated expression of HLA-DRA and HLA-DRB4 in primary passage RA FLS compared to primary early passage OA FLS, especially in passage 2 FLS, might result from the elevated expressions of these genes in RA MLS rather than in RA FLS56. In contrast, the elevated expression of HLA-DRA and HLA-DRB4 in hTERT-OA 13A FLS compared to hTERT-RA 516 FLS might actually reflect the intrinsic characteristics of the OA 13A FLS.
Our study has limitations. All gene expressions were examined at transcription levels. In order to draw a more definite conclusion, confirmation at the protein level is needed. Another limitation is that the gene expressions were compared between one telomerase-transduced OA FLS and one telomerase-transduced RA FLS. Although many of our findings are consistent with findings reported from other laboratories where a large number of primary OA synovium/FLS and RA synovium/FLS was used, it is still uncertain how many of the differentially expressed genes (Table 2) are disease-specific rather than individual-specific. It is also unclear whether longterm cultures of telomerase-transduced OA FLS can be classified into different subgroups according to their gene expression profiles. A larger number of telomerase-transduced OA and RA FLS are needed to address these issues. We plan to establish a larger number of telomerase-transduced OA and RA FLS, and will carry out further studies to address these limitations.
Acknowledgments
Supported in part by a Charlotte-Mecklenburg Science Services Foundation grant to Y.S., and NIH Grant R01 AR45347 to G.S.F.
REFERENCES
- 1.Muller-Ladner U, Kriegsmann J, Tschopp J, Gay RE, Gay S. Demonstration of granzyme A and perforin messenger RNA in the synovium of patients with rheumatoid arthritis. Arthritis Rheum. 1995;38:477–84. doi: 10.1002/art.1780380404. [DOI] [PubMed] [Google Scholar]
- 2.Jorgensen C, Sun R, Rossi JF, et al. Expression of a multidrug resistance gene in human rheumatoid synovium. Rheumatol Int. 1995;15:83–6. doi: 10.1007/BF00262714. [DOI] [PubMed] [Google Scholar]
- 3.Konttinen YT, Li TF, Mandelin J, et al. Increased expression of extracellular matrix metalloproteinase inducer in rheumatoid synovium. Arthritis Rheum. 2000;43:275–80. doi: 10.1002/1529-0131(200002)43:2<275::AID-ANR6>3.0.CO;2-#. [DOI] [PubMed] [Google Scholar]
- 4.Busteed S, Bennett MW, Molloy C, et al. Bcl-x(L) expression in vivo in rheumatoid synovium. Clin Rheumatol. 2006;25:789–93. doi: 10.1007/s10067-005-0191-0. [DOI] [PubMed] [Google Scholar]
- 5.Aicher WK, Heer AH, Trabandt A, et al. Overexpression of zinc-finger transcription factor Z-225/Egr-1 in synoviocytes from rheumatoid arthritis patients. J Immunol. 1994;152:5940–8. [PubMed] [Google Scholar]
- 6.Cagnard N, Letourneur F, Essabbani A, et al. Interleukin-32, CCL2, PF4F1 and GFD10 are the only cytokine/chemokine genes differentially expressed by in vitro cultured rheumatoid and osteoarthritis fibroblast-like synoviocytes. Eur Cytokine Netw. 2005;16:289–92. [PubMed] [Google Scholar]
- 7.Wang N, Lu HS, Guan ZP, et al. Involvement of PDCD5 in the regulation of apoptosis in fibroblast-like synoviocytes of rheumatoid arthritis. Apoptosis. 2007;12:1433–41. doi: 10.1007/s10495-007-0070-z. [DOI] [PubMed] [Google Scholar]
- 8.Devauchelle V, Marion S, Cagnard N, et al. DNA microarray allows molecular profiling of rheumatoid arthritis and identification of pathophysiological targets. Genes Immun. 2004;5:597–608. doi: 10.1038/sj.gene.6364132. [DOI] [PubMed] [Google Scholar]
- 9.Pavlovich RI, Lubowitz J. Current concept in synovial tissue of the knee joint. Orthopedics. 2008;31:160–3. doi: 10.3928/01477447-20080201-24. [DOI] [PubMed] [Google Scholar]
- 10.Goldring MB, Goldring SR. Osteoarthritis. J Cell Physiol. 2007;213:626–34. doi: 10.1002/jcp.21258. [DOI] [PubMed] [Google Scholar]
- 11.Pearle AD, Scanzello CR, George S, et al. Elevated high-sensitivity C-reactive protein levels are associated with local inflammatory findings in patients with osteoarthritis. Osteoarthritis Cartilage. 2007;15:516–23. doi: 10.1016/j.joca.2006.10.010. [DOI] [PubMed] [Google Scholar]
- 12.Benito MJ, Veale DJ, FitzGerald O, van den Berg WB, Bresnihan B. Synovial tissue inflammation in early and late osteoarthritis. Ann Rheum Dis. 2005;64:1263–7. doi: 10.1136/ard.2004.025270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Smith MD, Triantafillou S, Parker A, Youssef PP, Coleman M. Synovial membrane inflammation and cytokine production in patients with early osteoarthritis. J Rheumatol. 1997;24:365–71. [PubMed] [Google Scholar]
- 14.Saito I, Koshino T, Nakashima K, Uesugi M, Saito T. Increased cellular infiltrate in inflammatory synovia of osteoarthritic knees. Osteoarthritis Cartilage. 2002;10:156–62. doi: 10.1053/joca.2001.0494. [DOI] [PubMed] [Google Scholar]
- 15.Haynes MK, Hume EL, Smith JB. Phenotypic characterization of inflammatory cells from osteoarthritic synovium and synovial fluids. Clin Immunol. 2002;105:315–25. doi: 10.1006/clim.2002.5283. [DOI] [PubMed] [Google Scholar]
- 16.Kato H, Matsumine A, Wakabayashi T, et al. Large-scale gene expression profiles, differentially represented in osteoarthritic synovium of the knee joint using cDNA microarray technology. Biomarkers. 2007;12:384–402. doi: 10.1080/13547500601162482. [DOI] [PubMed] [Google Scholar]
- 17.Galligan CL, Baig E, Bykerk V, Keystone EC, Fish EN. Distinctive gene expression signatures in rheumatoid arthritis synovial tissue fibroblast cells: correlates with disease activity. Genes Immun. 2007;8:480–91. doi: 10.1038/sj.gene.6364400. [DOI] [PubMed] [Google Scholar]
- 18.Goto M, Sasano M, Yamanaka H, et al. Spontaneous production of an interleukin 1-like factor by cloned rheumatoid synovial cells in long-term culture. J Clin Invest. 1987;80:786–96. doi: 10.1172/JCI113135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sun Y, Firestein G, Wenger L, Wang CY, Cheung H. Telomerase transduced osteoarthritic fibroblast-like synoviocyte cell line. Biochem Biophys Res Commun. 2004;323:1287–92. doi: 10.1016/j.bbrc.2004.09.005. [DOI] [PubMed] [Google Scholar]
- 20.Sun Y, Firestein G, Boyle D, Gruber H, Cheung H. Longterm culture of telomerase-transduced rheumatoid arthritis fibroblast-like synoviocytes display a distinct gene expression pattern. J Rheumatol. 2007;34:1959–70. [PubMed] [Google Scholar]
- 21.Pfaffl M, Meyer HH, Sauerwein H. Quantification of insulin-like growth factor-1 (IGF-1) mRNA: development and validation of an internally standardised competitive reverse transcription-polymerase chain reaction. Exp Clin Endocrinol Diabetes. 1998;106:506–13. doi: 10.1055/s-0029-1212025. [DOI] [PubMed] [Google Scholar]
- 22.Johnson K, Pritzker K, Goding J, Terkeltaub R. The nucleoside triphosphate pyrophosphohydrolase isozyme PC-1 directly promotes cartilage calcification through chondrocyte apoptosis and increased calcium precipitation by mineralizing vesicles. J Rheumatol. 2001;28:2681–91. [PubMed] [Google Scholar]
- 23.Ryan LM, Kurup IV, Cheung HS. Transduction mechanisms of porcine chondrocyte inorganic pyrophosphate elaboration. Arthritis Rheum. 1999;42:555–60. doi: 10.1002/1529-0131(199904)42:3<555::AID-ANR21>3.0.CO;2-Z. [DOI] [PubMed] [Google Scholar]
- 24.Williams CJ, Zhang Y, Timms A, et al. Autosomal dominant familial calcium pyrophosphate dihydrate deposition disease is caused by mutation in the transmembrane protein ANKH. Am J Hum Genet. 2002;71:985–91. doi: 10.1086/343053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hessle L, Johnson KA, Anderson HC, et al. Tissue-nonspecific alkaline phosphatase and plasma cell membrane glycoprotein-1 are central antagonistic regulators of bone mineralization. Proc Natl Acad Sci USA. 2002;99:9445–9. doi: 10.1073/pnas.142063399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Tchetverikov I, Lohmander LS, Verzijl N, et al. MMP protein and activity levels in synovial fluid from patients with joint injury, inflammatory arthritis, and osteoarthritis. Ann Rheum Dis. 2005;64:694–8. doi: 10.1136/ard.2004.022434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Freemont AJ, Hampson V, Tilman R, Goupille P, Taiwo Y, Hoyland JA. Gene expression of matrix metalloproteinases 1, 3, and 9 by chondrocytes in osteoarthritic human knee articular cartilage is zone and grade specific. Ann Rheum Dis. 1997;56:542–9. doi: 10.1136/ard.56.9.542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Shlopov BV, Lie WR, Mainardi CL, Cole AA, Chubinskaya S, Hasty KA. Osteoarthritic lesions: involvement of three different collagenases. Arthritis Rheum. 1997;40:2065–74. doi: 10.1002/art.1780401120. [DOI] [PubMed] [Google Scholar]
- 29.Naito K, Takahashi M, Kushida K, et al. Measurement of matrix metalloproteinases (MMPs) and tissue inhibitor of metalloproteinases-1 (TIMP-1) in patients with knee osteoarthritis: comparison with generalized osteoarthritis. Rheumatology Oxford. 1999;38:510–5. doi: 10.1093/rheumatology/38.6.510. [DOI] [PubMed] [Google Scholar]
- 30.Martel-Pelletier J, Welsch DJ, Pelletier JP. Metalloproteases and inhibitors in arthritic diseases. Best Pract Res Clin Rheumatol. 2001;15:805–29. doi: 10.1053/berh.2001.0195. [DOI] [PubMed] [Google Scholar]
- 31.Davidson RK, Waters JG, Kevorkian L, et al. Expression profiling of metalloproteinases and their inhibitors in synovium and cartilage. Arthritis Res Ther. 2006;8:R124. doi: 10.1186/ar2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Pruzanski W, Bogoch E, Stefanski E, Wloch M, Vadas P. Enzymatic activity and distribution of phospholipase A2 in human cartilage. Life Sci. 1991;48:2457–62. doi: 10.1016/0024-3205(91)90381-k. [DOI] [PubMed] [Google Scholar]
- 33.Xu L, Flahiff CM, Waldman BA, et al. Osteoarthritis-like changes and decreased mechanical function of articular cartilage in the joints of mice with the chondrodysplasia gene (cho). Arthritis Rheum. 2003;48:2509–18. doi: 10.1002/art.11233. [DOI] [PubMed] [Google Scholar]
- 34.Jakkula E, Melkoniemi M, Kiviranta I, et al. The role of sequence variations within the genes encoding collagen II, IX and XI in non-syndromic, early-onset osteoarthritis. Osteoarthritis Cartilage. 2005;13:497–507. doi: 10.1016/j.joca.2005.02.005. [DOI] [PubMed] [Google Scholar]
- 35.Ho AM, Johnson MD, Kingsley DM. Role of the mouse ank gene in control of tissue calcification and arthritis. Science. 2000;289:265–70. doi: 10.1126/science.289.5477.265. [DOI] [PubMed] [Google Scholar]
- 36.Pendleton A, Johnson MD, Hughes A, et al. Mutations in ANKH cause chondrocalcinosis. Am J Hum Genet. 2002;71:933–40. doi: 10.1086/343054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Long DL, Blake S, Song XY, Lark M, Loeser RF. Human articular chondrocytes produce IL-7 and respond to IL-7 with increased production of MMP-13. Arthritis Res Ther. 2008;10:R23. doi: 10.1186/ar2376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Appleton CT, Pitelka V, Henry J, Beier F. Global analyses of gene expression in early experimental osteoarthritis. Arthritis Rheum. 2007;56:1854–68. doi: 10.1002/art.22711. [DOI] [PubMed] [Google Scholar]
- 39.Sato T, Konomi K, Yamasaki S, et al. Comparative analysis of gene expression profiles in intact and damaged regions of human osteoarthritic cartilage. Arthritis Rheum. 2006;54:808–17. doi: 10.1002/art.21638. [DOI] [PubMed] [Google Scholar]
- 40.Nakagawa K, Sakiyama H, Tsuchida T, et al. Complement C1s activation in degenerating articular cartilage of rheumatoid arthritis patients: immunohistochemical studies with an active form specific antibody. Ann Rheum Dis. 1999;58:175–81. doi: 10.1136/ard.58.3.175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Wernert N, Justen HP, Rothe M, et al. The Ets 1 transcription factor is upregulated during inflammatory angiogenesis in rheumatoid arthritis. J Mol Med. 2002;80:258–66. doi: 10.1007/s00109-001-0316-0. [DOI] [PubMed] [Google Scholar]
- 42.Cheung HS, McCarty DJ. Mechanisms of connective tissue damage by crystals containing calcium. Rheum Dis Clin North Am. 1988;14:365–76. [PubMed] [Google Scholar]
- 43.Schumacher HR. Osteoarthritis: the role of articular crystals. Ariz Med. 1978;35:23–5. [PubMed] [Google Scholar]
- 44.Carroll GJ, Stuart RA, Armstrong JA, Breidahl PD, Laing BA. Hydroxyapatite crystals are a frequent finding in osteoarthritic synovial fluid, but are not related to increased concentrations of keratan sulfate or interleukin 1 beta. J Rheumatol. 1991;18:861–6. [PubMed] [Google Scholar]
- 45.Derfus BA, Kurian JB, Butler JJ, et al. The high prevalence of pathologic calcium crystals in pre-operative knees. J Rheumatol. 2002;29:570–4. [PubMed] [Google Scholar]
- 46.Cecil DL, Rose DM, Terkeltaub R, Liu-Bryan R. Role of interleukin-8 in PiT-1 expression and CXCR1-mediated inorganic phosphate uptake in chondrocytes. Arthritis Rheum. 2005;52:144–54. doi: 10.1002/art.20748. [DOI] [PubMed] [Google Scholar]
- 47.Mansfield K, Rajpurohit R, Shapiro IM. Extracellular phosphate ions cause apoptosis of terminally differentiated epiphyseal chondrocytes. J Cell Physiol. 1999;179:276–86. doi: 10.1002/(SICI)1097-4652(199906)179:3<276::AID-JCP5>3.0.CO;2-#. [DOI] [PubMed] [Google Scholar]
- 48.Magne D, Bluteau G, Faucheux C, et al. Phosphate is a specific signal for ATDC5 chondrocyte maturation and apoptosis-associated mineralization: possible implication of apoptosis in the regulation of endochondral ossification. J Bone Miner Res. 2003;18:1430–42. doi: 10.1359/jbmr.2003.18.8.1430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Henrotin YE, Bruckner P, Pujol JP. The role of reactive oxygen species in homeostasis and degradation of cartilage. Osteoarthritis Cartilage. 2003;11:747–55. doi: 10.1016/s1063-4584(03)00150-x. [DOI] [PubMed] [Google Scholar]
- 50.Mehta JL, Chen J, Hermonat PL, Romeo F, Novelli G. Lectin-like, oxidized low-density lipoprotein receptor-1 (LOX-1): a critical player in the development of atherosclerosis and related disorders. Cardiovasc Res. 2006;69:36–45. doi: 10.1016/j.cardiores.2005.09.006. [DOI] [PubMed] [Google Scholar]
- 51.Akagi M, Kanata S, Mori S, Itabe H, Sawamura T, Hamanishi C. Possible involvement of the oxidized low-density lipoprotein/lectin-like oxidized low-density lipoprotein receptor-1 system in pathogenesis and progression of human osteoarthritis. Osteoarthritis Cartilage. 2007;15:281–90. doi: 10.1016/j.joca.2006.07.010. [DOI] [PubMed] [Google Scholar]
- 52.Kanata S, Akagi M, Nishimura S, et al. Oxidized LDL binding to LOX-1 upregulates VEGF expression in cultured bovine chondrocytes through activation of PPAR-gamma. Biochem Biophys Res Commun. 2006;348:1003–10. doi: 10.1016/j.bbrc.2006.07.133. [DOI] [PubMed] [Google Scholar]
- 53.Wu LN, Genge BR, Kang MW, Arsenault AL, Wuthier RE. Changes in phospholipid extractability and composition accompany mineralization of chicken growth plate cartilage matrix vesicles. J Biol Chem. 2002;277:5126–33. doi: 10.1074/jbc.M107899200. [DOI] [PubMed] [Google Scholar]
- 54.Kirsch T, Ishikawa Y, Mwale F, Wuthier RE. Roles of the nucleational core complex and collagens (types II and X) in calcification of growth plate cartilage matrix vesicles. J Biol Chem. 1994;269:20103–9. [PubMed] [Google Scholar]
- 55.Seidel MF, Koch FW, Vetter H. Macrophage-like synoviocytes display phenotypic polymorphisms in a serum-free tissue-culture medium. Rheumatol Int. 2006;26:244–51. doi: 10.1007/s00296-004-0545-y. [DOI] [PubMed] [Google Scholar]
- 56.Blom AB, van Lent PL, Holthuysen AE, et al. Synovial lining macrophages mediate osteophyte formation during experimental osteoarthritis. Osteoarthritis Cartilage. 2004;12:627–35. doi: 10.1016/j.joca.2004.03.003. [DOI] [PubMed] [Google Scholar]