1. Introduction
A multitude of roles for the endogenous cannabinoid system has been proposed by recent research efforts. A large number of endogenous cannabinoid neurotransmitters or endocannabinoids have been identified, and the CB-1 and CB-2 cannabinoid receptors have been characterized. The presence of other receptors, transporters, and enzymes responsible for the synthesis or metabolism of endocannabinoids are becoming known at an extraordinary pace. The complex functions of this novel system have created multiple new targets for pharmacotherapies. Research has focused on separating the behavioral psychoactive effects of cannabinoid agonists from therapeutic effects. These efforts have been largely unsuccessful. Another strategy centers on changing the pharmacokinetics of drug delivery to maximize therapeutic effect and minimize cognitive and subjective drug effects. Development of oral, rectal, and transdermal medications of synthetic Δ9-tetrahydrocannabinol (THC)1) are examples of this type of approach. Additionally, the potential therapeutic benefits of administering unique combinations of cannabinoids and other chemicals present in the plant Cannabis sativa is being investigated by the oromucosal route. There also is strong interest in medications based on antagonizing endocannabinoid action. 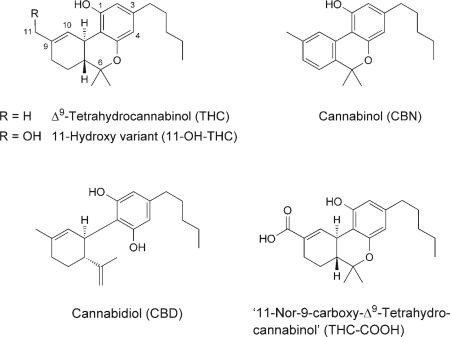
We have shown that the cardiovascular and subjective effects of cannabis are blocked by rimonabant, the first CB-1 cannabinoid-receptor antagonist, documenting that CB-1 receptors mediate these effects of smoked cannabis in humans. It is clear that the endogenous cannabinoid system plays a critical role in physiological and behavioral processes, and extensive research effort is being devoted to the biology, chemistry, pharmacology, and toxicology of cannabinoids.
Cannabis is one of the oldest and most commonly abused drugs in the world, and its use is associated with pathological and behavioral toxicity. Thus, it is important to understand cannabinoid pharmacokinetics and the disposition of cannabinoids into biological fluids and tissues. Understanding the pharmacokinetics of a drug is essential to understanding the onset, magnitude, and duration of its pharmacodynamic effects, maximizing therapeutic and minimizing negative side effects.
Cannabinoid pharmacokinetics encompasses absorption after diverse routes of administration and from different drug formulations, analyte distribution throughout the body, metabolism by the liver and extra-hepatic tissues, and elimination in the feces, urine, sweat, oral fluid, and hair. Pharmacokinetic processes are dynamic, may change over time, and may be affected by the frequency and magnitude of drug exposure. The many contributions to our understanding of cannabinoid pharmacokinetics from the 1970s and 1980s are reviewed, and the findings of recent research expanding upon this knowledge are detailed. Cannabinoid pharmacokinetics research is challenging due to low analyte concentrations, rapid and extensive metabolism, and physico-chemical characteristics hindering the separation of drugs of interest from biological matrices and from each other. Drug recovery is reduced due to adsorption of compounds of interest to multiple surfaces. Much of the early cannabinoid data are based on radiolabeled cannabinoids yielding highly sensitive, but less specific, measurement of individual cannabinoid analytes. New extraction techniques and mass-spectrometric (MS) developments now permit highly sensitive and specific measurement of cannabinoids in a wide variety of biological matrices, improving our ability to characterize cannabinoid pharmacokinetics.
Cannabis sativa contains over 421 different chemical compounds, including over 60 cannabinoids [1-3]. Cannabinoid plant chemistry is far more complex than that of pure THC, and different effects may be expected due to the presence of additional cannabinoids and other chemicals. Eighteen different classes of chemicals, including nitrogenous compounds, amino acids, hydrocarbons, carbohydrates, terpenes, and simple and fatty acids, contribute to the known pharmacological and toxicological properties of cannabis. THC is usually present in Cannabis plant material as a mixture of monocarboxylic acids, which readily and efficiently decarboxylate upon heating. THC decomposes when exposed to air, heat, or light; exposure to acid can oxidize the compound to cannabinol (CBN), a much less-potent cannabinoid. In addition, cannabis plants dried in the sun release variable amounts of THC through decarboxylation. During smoking, more than 2,000 compounds may be produced by pyrolysis. The pharmacokinetics of THC, the primary psychoactive component of cannabis, its metabolites ‘11-hydroxytetrahydrocannabinol’ (11-OH-THC) and ‘11-nor-9-carboxy-tetrahydrocannabinol’ (THC-COOH)]2), and another cannabinoid present in high concentration, cannabidiol (CBD), a non-psychoactive agent with an interesting array of potential therapeutic indications, are included. Mechoulam et al. elucidated the structure of THC in 1964, enabling studies of the drug's pharmacokinetics [4]. THC, containing no N-atom, but with two stereogenic centers in a trans configuration, has been described by two different atom-numbering systems, either the dibenzopyran (or Δ9) or the monoterpene (or Δ1) system. In this review, the dibenzopyran (Δ9) system is employed.
2. Pharmacokinetics of Cannabinoids
2.1. Absorption
2.1.1. Smoking
Route of drug administration and drug formulation determine the rate of drug absorption. Smoking, the principal route of cannabis administration, provides a rapid and efficient method of drug delivery from the lungs to the brain, contributing to its abuse potential. Intense pleasurable and strongly reinforcing effects may be produced due to almost immediate drug exposure to the central nervous system (CNS). Slightly lower peak THC concentrations are achieved after smoking as compared to intravenous administration [5]. Bioavailability following the smoking route was reported as 2−56%, due in part to intra- and inter-subject variability in smoking dynamics, which contributes to uncertainty in dose delivery [6-9]. The number, duration, and spacing of puffs, hold time, and inhalation volume, or smoking topography, greatly influences the degree of drug exposure [10-12]. Expectation of drug reward also may affect smoking dynamics. Cami et al. noted that subjects were able to change their method of smoking hashish cigarettes to obtain higher plasma concentrations of THC, when they expected to receive active drug in comparison to placebo cigarettes [13].
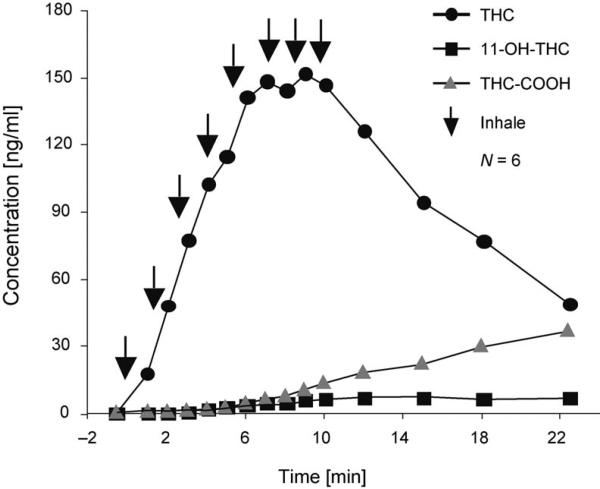
A continuous blood-withdrawal pump, collecting blood at a rate of 5 ml/min, enabled capture of the rapid THC absorption phase during smoking for the first time. Formation of 11-OH-THC and THC-COOH was slower, and peak concentrations were much lower [14]. The disposition of THC and its metabolites were followed for a period of 7 d after smoking a single placebo, and cigarettes containing 1.75% or 3.55% of THC. The mean (±S.D.) THC concentrations were 7.0±8.1 ng/ml and 18.1±12.0 ng/ml upon single inhalation of the low-dose (1.75% THC, ca. 16 mg) or the high-dose (3.55% THC, ca. 34 mg) cigarette, respectively, as determined by gas-chromatography/mass spectrometry (GC/MS) [14]. THC, detected in plasma immediately after the first cigarette puff (Fig. 1), was accompanied by the onset of cannabinoid effects [15]. Concentrations increased rapidly, reaching mean peaks of 84.3 ng/ml (range 50−129) and 162.2 ng/ml (range 76−267) for the above two cigarettes, respectively. Peak concentrations occurred at 9.0 min, prior to initiation of the last puff sequence at 9.8 min.
Fig. 1.
Mean (N=6) plasma concentrations of THC, 11-OH-THC, and THC-COOH during smoking of a single cannabis cigarette containing 3.55% of THC. Arrows (↓) indicate one inhalation or puff on the cannabis cigarette. Reprinted and adapted with permission by Springer-Verlag, ‘Handbook of Experimental Pharmacology’, 2005, p. 660, Fig. 1.
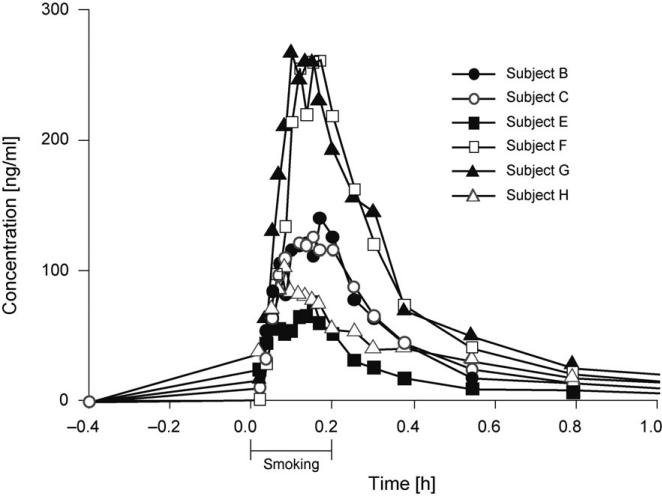
Despite a computer-paced smoking procedure that controlled the number of puffs, length of inhalation, hold time, and time between puffs, there were large inter-subject differences in plasma THC concentrations due to differences in the depth of inhalation, as participants titrated their THC dose (Fig. 2). The mean THC concentrations were ca. 60 and 20% of the peak concentrations 15 and 30 min post smoking, respectively. Within 2 h, plasma THC concentrations were ≤ 5 ng/ml. THC Detection windows (GC/MS detection limit 0.5 ng/ml) varied from 3 to 12 h after smoking the low-dose (1.75% THC) cannabis cigarette, and from 6 to 27 h in the case of the high-dose (3.55% THC) cigarette.
Fig. 2.
Time-dependent THC concentrations for six individuals (subjects B, C, and E–H) following smoking of a single cannabis cigarette containing 3.55% of THC. Reprinted and adapted with permission by Journal of Analytical Toxicology, p. 280 in [14], Fig. 1.
Similar mean maximum THC concentrations were reported in specimens collected immediately after cannabis smoking was completed. The mean peak THC concentrations were 94.3, 107.4, and 155.1 ng/ml after smoking single cigarettes of 1.32, 1.97, or 2.54% THC, respectively [16]. Other reported peak THC concentrations ranged between 45.6 and 187.8 ng/ml following smoking of a cigarette containing 1% of THC [17], and 33−118 ng/ml 3 min after ad libitum smoking of a cigarette containing ca. 2% of THC [5]. The smoking route is preferred by many cannabis users because of its rapid drug delivery and resultant fast onset of effects, but also for the ability to titrate dose to the desired degree of effect. In our controlled smoked-cannabis experiments described above, the individual with the lowest peak plasma concentration had the greatest cardiovascular response [15].
The average concentrations in more than 30,000 cannabis preparations confiscated in the U.S. between 1980 and 1997 were 3.1% THC and only 0.3% CBD [18]. However, cannabis-based medicine extracts and clinical-grade cannabis contain high quantities of CBD, which frequently equal the percentage of THC [19]. CBD may modify the effects of THC and reportedly may inhibit cytochrome P450 (CYP 450)-mediated conversion of THC to 11-OH-THC [20][21], although results are not always consistent across studies. The formation of THC from CBD neither occurs by heat during smoking [22] nor by human metabolism.
2.1.2. Oral
There are fewer studies on the disposition of THC and its metabolites after oral administration of cannabis as compared to the smoked route. THC is readily absorbed due to its high octanol/water partition coefficient (P), estimated to be between 6,000 and over 9 × 106, depending on the method of determination [23]. The advantages of cannabinoid smoking are offset by the harmful effects of cannabinoid smoke; hence smoking is generally not recommended for therapeutic applications. Synthetic THC, i.e., dronabinol (Marinol®) preparations, are usually taken orally, but may also be administered rectally. In addition, abuse of cannabis by the oral route also is common. Absorption is slower when cannabinoids are ingested, with lower, more-delayed peak THC concentrations [24][25]. Dose, route of administration, vehicle, and physiological factors such as absorption and rates of metabolism and excretion can influence drug concentrations in circulation. Perez-Reyes et al. described the efficacy of five different vehicles for oral administration of THC in gelatin capsules [26]. Glycocholate and sesame oil improved the bioavailability of oral THC; however, there was considerable variability in peak concentrations and rates of absorption, even when the drug was administered in the same vehicle. Oral THC bioavailability was reported to be 10−20% by Wall et al. [27]. Participants were dosed with either 15 mg (women) or 20 mg (men) of THC dissolved in sesame oil and contained in gelatin capsules. THC Plasma concentrations peaked ca. 4−6 h after ingestion of 15−20 mg of THC in sesame oil. A percentage of the THC was radiolabeled; however, investigators were unable to differentiate labeled THC from its labeled metabolites. Thus, THC concentrations were overestimated.
Possibly a more accurate assessment of oral bioavailability of THC in plasma samples was reported by Ohlsson et al., based on GC/MS experiments [5]. The peak THC concentrations ranged from 4.4 to 11 ng/ml, occurring 1−5 h following ingestion of 20 mg of THC in a chocolate cookie; the oral bioavailability was estimated to be 6%. Slow rates of absorption and low THC concentrations occur after oral administration of THC or cannabis. Several factors may account for the low oral bioavailability of 4−20% (as compared to intravenous drug administration), including variable absorption, degradation of drug in the stomach, and significant first-pass metabolism to active 11-OH-THC and inactive metabolites in the liver.
Currently, synthetic THC (Marinol®) is approved in the U.S.A. for reduction of nausea and vomiting in cancer chemotherapy, and to increase appetite in HIV-wasting disease. Potential new indications include the reduction of spasticity, analgesia, and as an agonist-replacement pharmacotherapy for cannabis dependence. Thus, the pharmacokinetics of oral THC is of great importance to the successful application of new therapeutic approaches. In a study of the plasma concentrations of THC, 11-OH-THC, and THC-COOH in 17 volunteers upon intake of a single Marinol® capsule (10 mg of THC), mean peak concentrations of 3.8 ng/ml of THC (range 1.1−12.7 ng/ml), 3.4 ng/ml of 11-OH-THC (range 1.2−5.6 ng/ml), and 26 ng/ml of THC-COOH (range 14−46 ng/ml) were found 1−2 h after ingestion [28]. Similar THC and 11-OH-THC concentrations were observed with consistently higher THC-COOH concentrations. Interestingly, two THC peaks frequently were observed due to enterohepatic circulation. Onset is delayed, peak concentrations are lower, and duration of pharmacodynamic effects generally are extended with a delayed return to baseline, when THC is administered by the oral as compared to the smoked route [29][30].
In addition, THC-containing foods, i.e., hemp oil, beer, and other products, are commercially available for oral consumption. Hemp oil is produced from cannabis seed, and is an excellent source of essential amino acids and ω-linoleic and linolenic fatty acids. The THC content depends upon the effectiveness of cannabis-seed-cleaning and oil-filtration processes. Hemp oil with THC contents ≥ 300 and 1,500 mg/g were available in the U.S.A. and in Europe, respectively. Currently, the THC concentrations of hemp oil in the U.S.A. are low, reflecting the efforts of manufacturers to reduce the amount of THC in hemp-oil products.
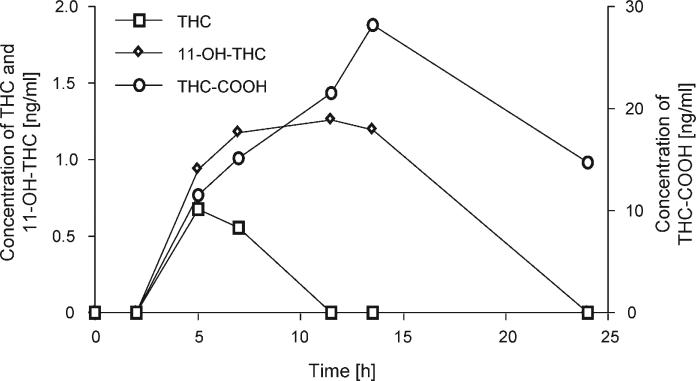
In a recent, controlled cannabinoid-administration study of THC-containing hemp oils and dronabinol, the pharmacokinetics and pharmacodynamics of oral THC were evaluated. Up to 14.8 mg of THC was ingested by six volunteers each day in three divided doses with meals for five consecutive days [31][32]. There was a 10-d washout phase between each of the five dosing sessions. THC was quantified in plasma by solid-phase extraction, followed by GC/MS (positive-mode, chemical-ionization) analysis. THC and 11-OH-THC were rarely detected in plasma following the two lowest doses (0.39 and 0.47 mg/d of THC), while, as shown in Fig. 3, peak plasma concentrations of less than 6.5 ng/ml of THC, <5.6 ng/ml of 11-OH-THC, and <43.0 ng/ml of THC-COOH were found after the two highest THC doses (7.5 and 14.8 mg/d). Interestingly, THC-COOH concentrations after THC administration at a dose of 7.5 mg/d were greater than or equal to those after intake of the high-potency hemp-oil dose (14.8 mg/d). This could be due to the formulation of dronabinol, which afforded greater protection from degradation in the stomach due to encapsulation and perhaps, improved bioavailability of THC in sesame oil, the formulation of synthetic THC or dronabinol. Plasma THC and 11-OH-THC concentrations fell below the method's limits of quantification of 0.5 ng/ml by 25 h, while THC-COOH was still measurable for more than 50 h after the last dose of the higher-concentration hemp oils.
Fig. 3.
Plasma concentrations (N=1) over 24 h for THC, 11-OH-THC, and THC-COOH following administration of two doses (2.5 mg each) of synthetic THC (dronabinol) at 4.5 and 10.5 h. Reprinted and adapted with permission by Elsevier, p. 152 in [32], Fig. 2.
After oral THC dosing, Nadulski et al. reported generally higher THC-COOH concentrations than those of THC almost immediately after dosing, in contrast to what is found after smoking [33]. Concentrations of 11-OH-THC also were higher than those of THC, with an extended detection window. These investigators suggest that ratios of [11-OH-THC]/[THC] >1 and >1.5 within and after 2 h after consumption, respectively, are strong indications for oral intake of THC.
Due to low bioavailability of oral THC formulations, alternative routes of drug administration, including oromucosal or sublingual dosing, vaporization of product and inhalation, and rectal administration, have been developed to improve the amount of delivered cannabinoids.
2.1.3. Oromucosal
Due to the chemical complexity of cannabis plant material compared to synthetic THC, extracts of cannabis that capture the full range of cannabinoids are being explored as therapeutic medications. Cannabis has been used as medicine for thousands of years [34][35]. Cultivation methods have been developed to reproducibly produce plants with defined THC or CBD concentrations. GW Pharmaceuticals has produced two standardized extract preparations, Tetranabinex®, which is high in THC, and Nabidiolex®, which is high in CBD. Sativex® contains equal proportions of Tetranabinex® and Nabidiolex®, and, hence, almost equal amounts of THC and CBD. THC and CBD represent approximately 70% of the product, with 5% of other cannabinoids, the remainder being terpenoids, flavonoids, sterols, alkanes, and other chemicals [36]. Clinical trials of the efficacy of these extracts are ongoing for analgesia [37][38] and spasticity, and other indications in affected patients [39]. Sativex® is administered sublingually to avoid first-pass metabolism by the liver. Sativex® is approved in Canada for the treatment of neuropathic pain associated with multiple sclerosis, and in three European countries for a number of indications.
2.1.4. Rectal
Several different suppository formulations were evaluated in monkeys to determine the matrix that maximizes bioavailability and reduces first-pass metabolism [40][41]; THC-hemisuccinate provided the highest bioavailability of 13.5%. Brenneisen et al. evaluated plasma THC concentrations in two patients who were prescribed THC-hemisuccinate suppositories or Marinol® for spasticity [42]. THC did not accumulate in the blood following 10−15 mg daily doses. THC concentrations peaked within 1−8 h after oral administration, and ranged between 2.1 to 16.9 ng/ml. Rectal administration of 2.5−5 mg of THC produced maximum plasma concentrations of 1.1−4.1 ng/ml within 2−8 h. The bioavailability of the rectal route was approximately twice that of the oral route due to higher absorption and lower first-pass metabolism.
2.1.5. Transcutaneous
Another route of cannabinoid exposure that avoids first-pass metabolism and improves THC bioavailability is topical administration [43]. Cannabinoids are highly hydrophobic, making transport across the aqueous layer of the skin the rate-limiting step in the diffusion process [44][45]. In vitro diffusion studies may underestimate in vivo transdermal flux [43]. After application of a dermal patch, mean steady-state plasma concentration of Δ8-THC was 4.4 ng/ml within 1.4 h, and was maintained for at least 48 h. Permeabilities of CBD and CBN were found to be 10-fold higher than for Δ8-THC. In vivo studies of transdermal drug delivery in guinea pigs noted the presence of significant amounts of plasma metabolites after topical application of THC [46]. Additional research is planned with combinations of cannabinoids in EtOH to increase drug absorption.
Transdermal delivery of cannabinoids is hoped to reduce negative side effects seen with inhalation dosing [47]. Transdermal delivery also bypasses first-pass metabolism of cannabinoids. These properties could improve the utility of transdermal cannabinoid medications. Applying a transdermal patch several hours before chemotherapy, and wearing it for several days, would be a convenient means for treating associated nausea and vomiting. Also, wearing a patch for a week to stimulate appetite could be a good alternative to twice a day oral dosing of dronabinol.
The drug-abuse potential of cannabinoid transdermal patches is expected to be low because of slow delivery of THC to the brain. However, extraction of cannabinoids from the patch for administration by a more-rapid method has not been evaluated. Diversion of fentanyl patches by drug abusers for use in such a manner has been a significant problem.
2.1.6. Intravenous
Although THC is not abused by the intravenous route, pharmacodynamic and pharmacokinetic cannabinoid research has employed this technique. Recently, D'Souza et al. administered THC intravenously to evaluate the association between cannabinoids and psychosis [48]. The double-blind, randomized, and placebo-controlled study investigated the behavioral, cognitive, and endocrine effects of 0, 2.5, and 5 mg of THC in healthy individuals with a history of cannabis exposure, but never diagnosed with a cannabis-abuse disorder. After 10 min, the plasma THC concentrations were 82±87.4 and 119.2±166.5 for intravenous doses of 2.5 and 5.0 mg, ng/ml respectively; the respective THC-COOH concentrations were 43.8±26.1 and 81.9±47 ng/ml. Some subjects withdrew from the study due to acute paranoia (1), panic (1), hypotension (2), withdrawal of consent due to dislike of THC effects (3), and other issues (2). One subject experienced a significant, acute paranoid reaction and was treated with 2 mg lorazepam. THC produced schizophrenia-like positive and negative symptoms and euphoria, and altered aspects of cognitive function. Plasma cortisol concentrations were not affected. THC produced a broad range of transient symptoms, behaviors, and cognitive deficits in healthy individuals that resembled endogenous psychoses. The investigators suggested that brain-cannabinoid-receptor function could be an important factor in the pathophysiology of psychotic disorders.
2.1.7. Cannabidiol Absorption
Cannabidiol (CBD) is a natural, non-psychoactive [49][50] constituent of Cannabis sativa, but possesses pharmacological activity, which is explored for therapeutic applications. CBD has been reported to be neuroprotective [51], analgesic [37][38][52], sedating [37][38][53][54], anti-emetic [54], anti-spasmodic [55], and anti-inflammatory [56]. In addition, it has been reported that CBD blocks anxiety produced by THC [57], and may be useful in the treatment of autoimmune diseases [53]. CBD also has been reported to decrease some of the side effects of THC [36]. These potential therapeutic applications alone warrant investigation of CBD pharmacokinetics. Further, the controversy over whether CBD alters the pharmacokinetics of THC in a clinically significant manner needs to be resolved [58][59].
Ohlsson et al. reported CBD levels of 37−61 ng/ml (n=3, mean 48.4 ng/ml) 1 h after intravenous injection of 20 mg of deuterium-labeled CBD, and of 3.0−17.8 ng/ml (n=3, mean 10.2 ng/ml) 1 h after smoking a cigarette containing 19.2 mg of deuterium-labeled CBD [60]. Average bioavailability by the smoked route was 31 13% in five subjects, with a fourfold difference in availability noted. Based on the area under the curve (AUC) for 72 h and the dose after intravenous administration, a plasma clearance of 960−1560 ml/min was calculated. Agurell et al. found 1.1−11 ng/ml of CBD 1 h after oral application of 40 mg of CBD (n=12, mean 5.5 ng/ml) in chocolate cookies [61]. Recently, Nadulski et al. reported CBD concentrations of 0.30−2.57 ng/ml (mean: 0.95 ng/ml) 1 h after oral intake of 5.4 mg of CBD [33]. CBD remained detectable for 3−4 h after administration. The authors suggest that identification and quantification of CBD could be an additional proof of cannabis exposure and could improve interpretation of THC effects considering the potential ability of CBD to modify THC effects.
When comparing sublingual administration of THC (25 mg) alone vs. THC/CBD (25 mg each) in cannabis-based medicinal extracts, no statistically significant differences in mean THC maximum concentration, half-life, or AUC for THC and 11-OHTHC were observed [62]. The only statistically significant difference was in the time of maximum THC concentration. Despite administration of equivalent amounts of THC and CBD, lower plasma concentrations of CBD were always observed. The pharmacokinetics of THC, 11-OH-THC, and CBD also were evaluated after administration of 10 mg each of THC and CBD, either via the sublingual, buccal, oromucosal, or oral routes [63]. All three analytes were detectable ca. 30 min after dosing, with higher THC than CBD concentrations. 11-OH-THC generally exceeded THC concentrations within 45 min of dosing. Mean maximum concentrations for THC, CBD, and 11-OH-THC were <5, <2, and <7 ng/ml, respectively, across all administration routes. High intra- and inter-subject variability was noted.
2.2. Distribution
THC Plasma concentrations decrease rapidly after the end of smoking due to rapid distribution into tissues and metabolism in the liver. THC is highly lipophilic and initially taken up by tissues that are highly perfused, such as the lung, heart, brain, and liver. Tracer doses of radioactive THC documented the large volume of distribution of THC and its slow elimination from body stores. In animals, after intravenous administration of labeled THC, higher levels of radioactivity were present in lung than in other tissues [64]. Studies of the distribution of THC into brain are especially important for understanding the relationships between THC dose and behavioral effects. After single intra-muscular administration of 14C-labeled Δ8-THC to rats, maximal radioactivity was reached in brain after 2−4 h, representing 0.06% of the administered dose [65]. Plasma concentrations were of similar magnitude to those measured in men exposed to marihuana smoke. Kreuz and Axelrod were the first to describe the persistent and preferential retention of radiolabeled THC in neutral fat after multiple doses, in contrast to limited retention in brain [66]. The ratio of fat to brain THC concentration was approximately 21 : 1 after 7 d of consecutive exposure, and 64 : 1 after 27 d. Other investigators also found that the amount of THC retained in the brain after administration of radiolabeled THC was less than 1% of the administered dose [67][68]. With prolonged drug exposure, THC concentrates in human fat, being retained for extended periods of time [69]. It is suggested that fatty acid conjugates of THC and 11-OH-THC may be formed, increasing the stability of these compounds in fat [70].
Distribution of THC into peripheral organs and the brain was found to be similar in THC-tolerant vs. non-tolerant dogs [71]. In addition, these investigators found that tolerance to the behavioral effects of THC in pigeons was not due to decreased uptake of cannabinoids into the brain. Tolerance also was evaluated in humans. Hunt and Jones found that tolerance in humans developed during oral administration of 30 mg of THC every 4 h, for 10−12 d [72]. Few pharmacokinetic changes were noted during chronic administration, although average total metabolic clearance and initial apparent volume of distribution increased from 605 to 977 ml/min, and from 2.6 to 6.4 l/kg, respectively. Pharmacokinetic changes after chronic oral THC administration could not account for observed behavioral and physiologic tolerance, suggesting rather that tolerance was due to pharmacodynamic adaptation.
Adams and Martin studied the THC dose required to induce pharmacological effects in humans [73]. They determined that 2−22 mg of THC must be present in a cannabis cigarette to deliver 0.2−4.4 mg of THC, based on 10−25% bioavailability for smoked THC. Only 1% of this dose at peak concentration was found in the brain, indicating that only 2−44 μg of THC penetrates to the brain.
In a recent, highly interesting study, Mura et al. analyzed paired blood and brain specimens in 12 postmortem cases for THC and THC-COOH, and also for 11-OH-THC, in two regular cannabis smokers by GC/MS [74]. The THC concentrations in blood and brain ranged from <0.2 to 11.5 ng/ml, and from 0.9 to 29.9 ng/g, respectively. There was no correlation between blood and brain concentrations; brain levels were always higher than blood levels, and in three cases measurable drug concentrations remained in the brain, when no longer detectable in the blood. In two additional cases, sufficient brain tissue was available to monitor THC, 11-OH-THC, and THC-COOH concentrations in both blood and seven brain areas known to have high concentrations of cannabinoid CB-1 receptors. THC, 11-OH-THC, and THC-COOH were found in substantial concentrations in all brain areas, including locus niger, hippocampus, occipital lobe, striatum-putamen-palladium, frontal lobe, spinal cord, and corpus callosum, the order generally being THC≥THC-COOH>11-OH-THC. Blood concentrations were lower than in the two-paired brains. The authors postulate that long-lasting effects of cannabis during abstinence in heavy users may be due to residual THC and 11-OH-THC concentrations in the brain. The consequences of THC-COOH in the brain remain unknown.
Storage of THC after chronic exposure could also contribute to observed toxicities in other tissues. After single intramuscular administration of radioactive THC in rats, only 0.023% of the original THC dose was found in testis, although total radioactivity in epididymal fat was five- and eight times higher than that in the brain after 4 and 24 h, respectively [65]. After multiple injections, concentrations of THC remained low in plasma, brain, and testis, not exceeding 2−7 ng/g, but the epididymal-fat tracer concentration was 40 to 80 times higher. The authors suggest that the blood–brain and blood–testicular barriers limit storage of THC in brain and testis during acute exposure; however, during THC chronic exposure, pharmacokinetic mechanisms are insufficient to prevent accumulation of THC in tissues, with subsequent deregulation of cellular processes, including apoptosis of spermatogenic cells.
In one of the latest investigations on THC distribution in tissues, the large-white-pig model was selected due to similarities with humans in drug biotransformation, including enzymes and isoenzymes of drug biotransformation, size, feeding patterns, digestive physiology, dietary habits, kidney structure and function, pulmonary vascular bed structure, coronary-artery distribution, propensity to obesity, respiratory rates, and tidal volume [75]. THC Plasma pharmacokinetics was found to be similar to those in humans. Eight pigs received 200 mg/kg intra-jugular THC injections, and two pigs were sacrificed 30 min, 2, 6, and 24 h later. At 30 min, high THC concentrations were noted in lung, kidney, liver, and heart, with comparable elimination kinetics in kidney, heart, spleen, muscle, and lung as observed in blood. The fastest THC elimination was noted in liver, where concentrations fell below measurable levels by 6 h. Mean brain concentration was approximately twice the blood concentration at 30 min, with highest levels in the cerebellum, and occipital and frontal cortex, and lowest concentrations in the medulla oblongata. THC Concentrations decreased in brain tissue slower than in blood. The slowest THC elimination was observed for fat tissue, where THC was still present at substantial concentrations 24 h later. 11-OH-THC was only found at high concentrations in the liver. The THC-COOH level was <5 ng/g in most tissues, except in bile, where it increased for 24 h following THC injection. The authors suggest that the prolonged retention of THC in brain and fat in heavy cannabis users is responsible for the prolonged detection of THC-COOH in urine and cannabis-related flashbacks. The author of this review hypothesizes that this residual THC may also contribute to cognitive deficits noted early during abstinence in chronic cannabis users.
THC accumulation in the lung occurs because of high exposure from cannabis smoke, extensive perfusion of the lung, and high uptake of basic compounds in lung tissue. Lung tissue is readily available during postmortem analysis, and would be a good matrix for investigation of cannabis exposure.
Metabolism of THC to 11-OH-THC, THC-COOH, and other analytes also contributes to the reduction of THC in blood. Perez-Reyes et al. compared the pharmacokinetics and pharmacodynamics of tritiated THC and 11-OH-THC in 20 male volunteers [76]. Although equal doses produced equal psychoactive effects, drug effects were perceived more rapidly after exposure to 11-OH-THC than to THC. In addition, 11-OH-THC left the intravascular compartment faster than THC. These data suggest that 11-OH-THC diffuses into the brain more readily than THC does. Other possible explanations include lower plasma-protein binding of 11-OH-THC or enhanced crossing of the blood–brain barrier by the hydroxylated metabolite.
The distribution volume (Vd) of THC is large, ca. 10 l/kg, despite the fact that it is 95−99% protein-bound in plasma, primarily to lipoproteins [72][77]. Protein-binding values for THC-COOH and THC-COOH glucuronide were similar to those of THC proper (ca. 97%) [78]. More recently, with the benefit of advanced analytical techniques, the steady state Vd value of THC was estimated to be 3.4 l/kg [70]. THC-COOH was found to be far less lipophilic than the parent drug, whose partition coefficient P value at neutral pH has been measured at 6,000 (or higher), and more lipophilic than the glucuronide [78]. The fraction of THC glucuronide present in blood after different routes of administration has not been adequately resolved, but, recently, the partition coefficient of this compound indicated an unexpectedly high lipophilicity, ca. 18 at pH 7.4.
THC rapidly crosses the placenta, although concentrations were lower in canine and ovine fetal blood and tissues than in maternal plasma and tissues [79]. The metabolites 11-OH-THC and THC-COOH crossed the placenta much less efficiently [80][81]. No THC-COOH was detected in fetal plasma and tissues, indicating a lack of transfer across the placenta, and a lack of metabolism of THC in fetal monkey [80]. Blackard and Tennes reported that THC in cord blood was three to six times less than in maternal blood [82]. Transfer of THC to the fetus was greater in early pregnancy. THC also concentrates into breast milk from maternal plasma due to its high lipophilicity [83][84]. THC Concentration in breast milk was 8.4 times higher than in plasma in one woman, yielding a daily THC exposure to the infant of 0.01 to 0.1 mg/d, assuming that the mother smokes one to two cannabis cigarettes each day [84].
2.3. Metabolism
2.3.1. Hepatic Metabolism
Burstein and co-workers were the first to show that 11-OH-THC and THC-COOH are primary metabolites of THC in rabbits and rhesus monkeys [85-87]. They also documented that THC can be metabolized in the brain. Harvey et al. monitored the metabolism of THC, CBD, and CBN in mice, rats, and guinea pigs, and found extensive metabolism, but with inter-species variation [88]. Phase-I oxidation reactions of THC include allylic and aliphatic hydroxylations, oxidation of alcohols to ketones and acids, β-oxidation, and degradation of the pentyl side chain. Conjugation with glucuronic acid is a common Phase-II reaction. 11-OH-THC was the primary metabolite in all three species, followed by 8α-OH-THC in the mouse and rat, and 8β-OH-THC in guinea pig. Side-chain hydroxylation was common in all three species. THC-COOH concentrations were higher in the mouse and rat, while THC-COOH glucuronide concentrations predominated in the guinea pig. THC Concentrations accumulated in the liver, lung, heart, and spleen.
Hydroxylation of THC at C(9) by the hepatic CYP 450 enzyme system leads to production of the equipotent metabolite 11-OH-THC [89][90], originally thought by early investigators to be the true psychoactive analyte [64]. CYP 450 2C9, 2C19, and 3A4 are involved in the oxidation of THC [90]. More than 100 THC metabolites, including di- and trihydroxy compounds, ketones, aldehydes, and carboxylic acids, have been identified [21][70][91]. Although 11-OH-THC predominates as the first oxidation product, significant amounts of 8β-OH-THC and lower amounts of the 8α-OH-THC are formed. Much lower plasma 11-OH-THC concentrations (ca. 10% of THC concentrations) are found after cannabis smoking than after oral administration [27]. Peak 11-OH-THC concentrations occurred ca. 13 min after the start of smoking [14]. Bornheim et al. reported that 11-OH-THC and 8β-OH-THC were formed at the same rate in human-liver microsomes, with smaller amounts of ‘epoxyhexahydrocannabinol’, 8α-OH-THC, and 8-keto-THC [92]. CYP 450 2C9 is thought to be primarily responsible for the formation of 11-OH-THC, whereas CYP 450 3A catalyzes the formation of 8β-OH-THC, ‘epoxyhexahydrocannabinol’, and other minor metabolites. Less than fivefold variability in 2C9 rates of activity was observed, while much higher variability was noted for the 3A enzyme. Dihydroxylation of THC yields 8β,11-di-OH-THC. Excretion of 8β,11-di-OH-THC in urine was reported to be a good biomarker for recent cannabis use [93].
Oxidation of the psychoactive 11-OH-THC produces the inactive metabolite THC-COOH [64][94]. THC-COOH and its glucuronide conjugate are the major end products of biotransformation in most species, including man [91][95]. THC-COOH concentrations gradually increase, and are greater than THC concentrations 30−45 min after the end of smoking [96]. After ingestion of a single oral dose of Marinol® (10 mg THC), plasma THC-COOH concentrations were higher than those of THC and 11-OH-THC as early as 1 h after dosing [97]. Unlike after smoking, THC and 11-OH-THC concentrations are similar after oral THC administration.
Phase-II metabolism of THC-COOH involves addition of glucuronic acid, and, less commonly, of sulfate, glutathione, amino acids, and fatty acids via the 11-COOH group. The phenolic OH group may be a target as well. It is also possible to have two glucuronic acid moieties attached to THC-COOH, although steric hindrance at the phenolic OH group could be a factor. Addition of the glucuronide group improves water solubility, facilitating excretion, but renal clearance of these polar metabolites is low due to extensive protein binding [72]. No significant differences in metabolism between men and women have been reported [27].
After the initial distribution phase, the rate-limiting step in the metabolism of THC is its redistribution from lipid depots into blood [98]. Lemberger et al. suggested that frequent cannabis smoking could induce THC metabolism [99]. However, later studies did not corroborate this finding [8][91].
More than 30 metabolites of CBD were identified in urine, with hydroxylation of the 7-Me group and subsequent oxidation to the corresponding carboxylic acid as the main metabolic route, in analogy to THC [100].
2.3.2. Extrahepatic Metabolism
Other tissues, including brain, intestine, and lung, may contribute to the metabolism of THC, although alternate hydroxylation pathways may be more prominent [86][101-104]. An extrahepatic metabolic site should be suspected whenever total body clearance exceeds blood flow to the liver, or when severe liver dysfunction does not affect metabolic clearance [102]. Of the ten mammalian classes of CYP 450 systems, the cytochrome families 1−4 primarily metabolize xenobiotics, which are found in the liver, small intestine, peripheral blood, bone marrow, and mast cells in decreasing concentrations, with the lowest concentrations in the brain, pancreas, gall bladder, kidney, skin, salivary glands, and testes. Within the brain, higher concentrations of CYP 450 enzymes are found in the brain stem and cerebellum [102]. The hydrolyzing enzymes – non-specific esterases, β-glucuronidases, and sulphatases–are primarily found in the gastrointestinal tract. Side-chain hydroxylation of THC is prominent in THC metabolism by the lung. Metabolism of THC by fresh biopsies of human intestinal mucosa yielded polar hydroxylated metabolites that directly correlated with time and amount of intestinal tissue [101].
In a study of the metabolism of THC in the brains of mice, rats, guinea pigs, and rabbits, Watanabe et al. found that brain microsomes oxidized THC to monohydroxylated metabolites [103]. Hydroxylation of C(4) of the pentyl side chain produced the most common THC metabolite in the brains of these animals, similar to THC metabolites produced in the lung. These metabolites are pharmacologically active, but their relative activity is unknown.
2.3.3. Metabolism of Cannabidiol
CBD Metabolism is similar to that of THC, with primary oxidation of C(9) to the alcohol and carboxylic acid [8][100], as well as side-chain oxidation [88][100]. Like THC, CBD is subjected to a significant first-pass effect; however, unlike THC, a large proportion of the dose is excreted unchanged in the feces [105]. Benowitz et al. reported that CBD is an in vitro inhibitor of liver microsomal drug-metabolizing enzymes, inhibiting hexobarbital metabolism in humans [50]. Others have reported that CBD selectively inhibits THC-metabolite formation in vitro [58]. Hunt et al. reported that the pharmacokinetics of THC were not affected by CBD, except for a slight slowing of the metabolism of 11-OH-THC to THC-COOH [106]. Co-administration of CBD did not significantly affect the total clearance, volume of distribution, and terminal elimination half-lives of THC metabolites. Concentration vs. time curves, and ratios of the maximum average concentration and AUC values for 11-OH-THC/THC, THC-COOH/THC, and THC-COOH/11-OH-THC showed that CBD only partially inhibited the hydroxylation of THC to 11-OH-THC catalyzed by CYP 2C, when data were compared after oral administration of THC alone, as compared to a THC and CBD preparation [107]. THC and CBD concentrations are high in the liver after oral administration, and there is high first-pass metabolism of THC. However, the effect of CBD on hydroxylation of THC was small in comparison to overall variability.
2.4. Elimination
Within 5 d, a total of 80−90% of THC is excreted, mostly as hydroxylated and carboxylated metabolites [21][95]. More than 65% is excreted in the feces, ca. 20% being eliminated in the urine [27]. Numerous acidic metabolites are found in the urine, many of which are conjugated with glucuronic acid to increase their water solubility. The primary urinary metabolite is the acid-linked THC-COOH glucuronide conjugate [108], while 11-OH-THC predominates in the feces [21]. The concentration of free THC-COOH, and the cross-reactivity of glucuronide-bound THC-COOH enable cannabinoid immunoassays to be performed directly on non-hydrolyzed urine, but confirmation and quantification of THC-COOH is usually performed after alkaline hydrolysis or β-glucuronidase hydrolysis to free THC-COOH for measurement by GC/MS. It was initially thought that little or no THC and 11-OH-THC were excreted in the urine.
2.4.1. Terminal Elimination Half-Lives of THC-COOH
Another common problem with studying the pharmacokinetics of cannabinoids in humans is the need for highly sensitive procedures to measure low cannabinoid concentrations in the terminal phase of excretion, and the requirement for monitoring plasma concentrations over an extended period to adequately determine cannabinoid half-lives. Many studies utilized short sampling intervals of 24−72 h that underestimate terminal THC and THC-COOH half-lives. The slow release of THC from lipid-storage compartments and significant enterohepatic circulation contribute to a long terminal half-life of THC in plasma, reported to be greater than 4.1 d in chronic cannabis users [109]. Isotopically labeled THC and sensitive analytical procedures were used to obtain this drug half-life. Garrett and Hunt reported that 10−15% of the THC dose is enterohepatically circulated in dogs [98]. Johansson et al. reported a THC-COOH plasma-elimination half-life of up to 12.6 d in a chronic cannabis user, when monitoring THC-COOH concentrations over four weeks [110]. Mean plasma THC-COOH elimination half-lives were 5.2±0.8 and 6.2±6.7 d for frequent and infrequent cannabis users, respectively. Similarly, when sensitive analytical procedures and sufficient sampling periods were employed for determining the terminal urinary excretion half-life of THC-COOH, it was estimated to 3−4 d [111]. Urinary THC-COOH concentrations drop rapidly until reaching a value of ca. 20−50 ng/ml, and then decrease at a much slower rate. No significant pharmacokinetic differences between chronic and occasional users have been substantiated [112].
2.4.2. Percentage of THC Excreted as Urinary THC-COOH
An average of 93.9±24.5 mg of THC-COOH (range 34.6−171.6 μg) was measured in urine over a period of 7 d, following smoking of a single cannabis cigarette containing ca. 18 mg (1.75%) of THC [113]. The average amount of THC-COOH excreted in the same time period following the high dose (3.55% THC cigarette, ca. 34 mg THC) was 197.4±33.6 μg (range 107.5−305.0 μg). This represents an average of only 0.54±0.14 and 0.53±0.09% of the original amount of THC in the low- and high-dose cigarettes, respectively. These small percentages of the total THC dose found in the urine as THC-COOH are not surprising, considering the many factors that influence THC-COOH excretion after smoking. Prior to harvesting, cannabis plant material contains little active THC. When smoked, THC carboxylic acids spontaneously decarboxylate to produce THC, with nearly complete conversion upon heating. Pyrolysis of THC during smoking destroys additional drug. Drug availability is further reduced by loss of drug in the side-stream smoke and drug remaining in the unsmoked cigarette butt. These factors contribute to high variability in drug delivery by the smoked route. It is estimated that the systemic availability of smoked THC is ca. 8−24%, and that bioavailability depends strongly upon the experience of the cannabis users [5][17][114]. THC Bioavailability is reduced due to the combined effect of these factors; the actual available dose is much lower than the amount of THC and THC precursor present in the cigarette. Most of the THC dose is excreted in the feces (30−65%), rather than in the urine (20%) [27][115]. Another factor affecting the low amount of recovered dose is measurement of a single metabolite. However, numerous cannabinoid metabolites are produced in humans as a result of THC metabolism, most of which are not detected or included in the calculations based on GC/MS analysis.
Following controlled oral administration of THC in dronabinol or hemp oil, urinary cannabinoid excretion was characterized in 4,381 urine specimens [116][117]. THC Doses of 0.39−14.8 mg/d (from hemp oils or Marinol®) were administered for 5 d. All urine voids, collected over ten weeks, were tested by immunoassay and GC/MS analysis. With the U.S. federally mandated 50 μg/l immunoassay cutoff, and during ingestion of the two low doses typical of current hemp-oil THC concentrations (<0.5 mg/d), mean detection rates were below 0.2% [116]. The two high doses (7.5 and 14.8 mg/d) produced mean detection rates of 23−46%, with intermittent positive tests up to 118 h. Maximum THC-COOH concentrations were 5.4−38.2 ng/ml for the low, and 19.0−436 μg/l for the high doses. The availability of cannabinoid-containing foodstuffs, cannabinoid-based therapeutics, and continued abuse of oral cannabis require scientific data for the accurate interpretation of cannabinoid tests. These data demonstrate that it is possible, but unlikely, for a urine specimen to test positive at the federally mandated cannabinoid cutoffs, following manufacturer's dosing recommendations for the ingestion of hemp oils of low THC concentration. Urine tests have a high likelihood of being positive following Marinol® therapy.
These investigators also reported no significant differences (P≤0.05) in mean time of maximum excretion rate, mean maximum excretion rate, and mean terminal elimination half-life between the four THC doses (0.39−14.8 mg/d), with ranges of 67.4−94.9 h, 0.9−16.3 μg/h, and 44.2−64.0 h, respectively [117]. Mean apparent elimination half-lives (t1/2) of 24.1±7.8 and 21.1±4.3 h for the low (7.5 mg/d) and high (14.8 mg/d) doses, respectively, were calculated from the excretion-rate curve prior to the last urine sample, with a THC-COOH concentration ≥15 ng/ml. An average of only 2.9±1.6%, 2.5±2.7%, 1.5±1.4%, and 0.6±0.5% of the THC in the dose of 0.39, 0.47, 7.5, and 14.8 mg/d, respectively, was excreted in the form of THC-COOH in the urine over each dosing session (14 d). This study demonstrated that the terminal urinary elimination half-life of THC-COOH following oral administration is ca. 2−3 d for doses ranging from 0.39−14.8 mg/d. These data also demonstrate that the apparent THC-COOH urinary elimination half-life, prior to reaching a concentration of 15 ng/ml, is significantly shorter than the terminal urinary elimination half-life.
2.4.3. Cannabinoid–Glucuronide Conjugates
Specimen preparation for cannabinoid testing frequently includes a hydrolysis step to free cannabinoids from their glucuronide conjugates. Most GC/MS procedures of urine samples measure total THC-COOH, following either an enzymatic hydrolysis with β-glucuronidase or, more commonly, an alkaline hydrolysis with NaOH. Alkaline hydrolysis appears to efficiently hydrolyze the ester glucuronide linkage.
2.4.4. Urinary Biomarkers of Recent Cannabis Use
Significantly higher concentrations of THC and 11-OH-THC in urine are observed, when Escherichia coli β-glucuronidase is used in the hydrolysis method, compared to either β-glucuronidase from Helix pomatia or base treatment [118][119]. THC and 11-OH-THC primarily are excreted in urine as glucuronide conjugates that are resistant to cleavage by alkaline hydrolysis or by enzymatic hydrolysis employing some types of β-glucuronidase. Kemp et al. demonstrated that β-glucuronidase from E. coli was needed to hydrolyze the ether glucuronide linkages of the active cannabinoid analytes. Mean THC concentrations in urine specimens from seven subjects, collected after each had smoked a single marijuana cigarette (3.58% of THC), was 22 ng/ml, when the E. coli β-glucuronidase hydrolysis method was used; in contrast, the observed THC concentrations were nearly zero when using either H. pomatia β-glucuronidase or base hydrolysis [118][119]. Similar differences were found for 11-OH-THC, with a mean concentration of 72 ng/ml for the E. coli method, but concentrations <10 ng/ml for the other methods. The authors suggested that finding THC and/or 11-OH-THC in the urine might provide a reliable marker of recent cannabis use, but adequate data from controlled drug-administration studies were not yet available to support or refute this observation. Using a modified analytical method with E. coli β-glucuronidase, we have analyzed hundreds of urine specimens collected after controlled THC administration. We found that 11-OH-THC may be excreted in the urine of chronic cannabis users for a much longer period of time, beyond the period of pharmacodynamic effects and performance impairment. Additional research is necessary to determine the validity of estimating time of cannabis use from THC and 11-OH-THC concentrations in urine.
3. Interpretation of Cannabinoid Concentrations in Biological Fluids
3.1. Plasma Concentrations
Compared to other drugs of abuse, analysis of cannabinoids presents some difficult challenges. THC and 11-OH-THC are highly lipophilic, and present in low concentrations in body fluids. Complex specimen matrices, i.e., blood, sweat, or hair, may require multi-step extractions to separate cannabinoids from endogenous lipids and proteins. Care must be taken to avoid low recoveries of cannabinoids due to their high affinity to glass and plastic containers, and to alternate matrix-collection devices [120-123]. THC and THC-COOH are predominantly found in the plasma fraction of blood, where 95−99% are bound to lipoproteins. Only ca. 10% of either compound is found in the erythrocytes [124]. Whole-blood cannabinoid concentrations are approximately one-half the concentrations found in plasma specimens, due to the low partition coefficient of drug into erythrocytes [96][125][126].
3.1.1. Intravenous THC Administration
Kelly et al. intravenously administered 5 mg of THC to eight males, and then periodically monitored THC, THC-COOH, and THC-COOH–glucuronide conjugates by GC/MS (1 ng/ml detection limit for THC and THC-COOH) in plasma with and without alkaline hydrolysis for up to 10 h, and then once daily for up to 12 d [77]. The elimination half-lives of THC, THC-COOH, and THC-COOH–glucuronide conjugate in the plasma of frequent cannabis users were 116.8 min, 5.2 d, and 6.8 d, respectively, and 93.3 min, 6.2 d, and 3.7 d in infrequent users. Conjugated THC-COOH was detected in the plasma of 75% of the frequent and 25% of the infrequent users after 12 d.
3.1.2. Smoked Cannabis
THC Detection times in plasma of 3.5−5.5 h were reported in individuals who smoked two cannabis cigarettes containing a total of ca. 10 mg of THC (GC/MS detection limit 0.8 ng/ml) [93], and up to 13 d for deuterated THC in the blood of chronic cannabis users, who smoked four cigarettes containing deuterium-labeled THC (GC/MS detection limit 0.02 ng/ml) [109]. In the latter study, the terminal half-life of THC in plasma was determined to be ca. 4.1 d, as compared to frequent estimates of 24−36 h in several other studies [27][59][127] that lacked the sensitivity and the lengthy monitoring window of the radiolabeled protocol.
Few controlled drug-administration studies have monitored active 11-OH-THC plasma concentrations. Huestis et al. found plasma 11-OH-THC concentrations to be ca. 6−10% of the concurrent THC concentrations for up to 45 min after the start of smoking [14]. Mean peak 11-OH-THC concentrations occurred 13.5 min (range 9.0−22.8 min) after the start of smoking, and were 6.7 ng/ml (range 3.3−10.4 ng/ml) and 7.5 ng/ml (range 3.8−16 ng/ml) after smoking one cannabis cigarette containing 1.75 or 3.55% of THC, respectively. The concentrations of 11-OH-THC decreased gradually, with mean detection times of 4.5 and 11.2 h after the two doses.
The concentrations of THC-COOH were monitored in human plasma for 7 d after controlled cannabis smoking [14]. This inactive metabolite was detected in the plasma of all subjects by 8 min after the start of smoking. THC-COOH concentrations in plasma increased slowly, and reached a plateau for up to 4 h. Peak concentrations were consistently lower than peak THC concentrations, but were higher than 11-OH-THC peak concentrations. Mean peak THC-COOH concentrations were 24.5 ng/ml (range 15−54 ng/ml) and 54.0 ng/ml (range 22−101 ng/ml) after smoking the low- (1.75% of THC) or high-dose (3.55% of THC) cigarette, respectively. Following smoking of the lower dose, THC-COOH was detected from 48−168 h, with a mean of 84 h. Detection times ranged from 72−168 h, with a mean of 152 h, following smoking of the higher dose. The time course of detection of THC-COOH is much longer than either that of THC or 11-OH-THC. The AUC for the mean data from 0−168 h was 36.5 and 72.2 ng × h/ml, respectively, for the low- and high-dose conditions, demonstrating a dose-response relationship for the mean data [14]. Fig. 2 (see above) shows individual THC-concentration time profiles for six subjects, demonstrating the large inter-subject variability of the smoked route of drug administration. Moeller et al. measured serum THC and THC-COOH concentrations in 24 experienced users from 40−220 min after smoking cannabis cigarettes with a THC content of 300 μg/kg [128]. Mean serum THC and THC-COOH concentrations were ca. 13 and 22 ng/ml at 40 min, and 1 and 13 ng/ml at 220 min after smoking, respectively. The half-life of the rapid-distribution phase of THC was estimated to be 55 min over this short sampling interval.
Most plasma or whole-blood analytical methods for the determination of cannabinoids have not included measurement of the glucuronide conjugates of THC, 11-OH-THC, or THC-COOH. The relative percentages of free and conjugated cannabinoids in plasma after different routes of drug administration are unclear. Even the efficacy of alkaline- and enzymatic-hydrolysis procedures to release analytes from their conjugates is not fully understood [24][77][93][115][118][119][129-133]. In general, the concentrations of conjugate are believed to be lower in plasma, following intravenous or smoked administration, but may be of much greater magnitude after oral intake. There is no indication that the glucuronide conjugates are active, although supporting data are lacking.
3.1.3. Oral Administration
After oral and sublingual administration of THC, THC-containing food products, or cannabis-based extracts, the concentrations of THC and 11-OH-THC are much lower than those found upon smoked administration. Plasma concentrations of THC in patients receiving 10−15 mg of Marinol® as an anti-emetic were low or even non-measurable in 57 patients [134]. After daily administration of 10−15 mg of Marinol®, Brenneisen et al. found peak plasma concentrations of THC and THC-COOH of 2.1−16.9 ng/ml within 1−8 h, and of 74.5−244 ng/ml within 2−8 h, respectively [42]. In our oral, controlled THC-administration studies, peak plasma THC, 11-OH-THC, and THC-COOH concentrations were less than 6.5, 5.6, and 24.4 ng/ml, respectively, following up to 14.8 mg/d of THC in the form of THC-containing food products or Marinol® [135]. Peak concentrations and time-to-peak concentrations varied sometimes considerably between subjects. Plasma THC and 11-OH-THC were negative for all participants and for all doses by 16 h after administration of the last THC dose. Plasma THC-COOH persisted for a longer period of time, following the two highest doses of 7.5 mg/d of dronabinol, and 14.8 mg/d of THC in hemp oil. Ohlsson et al. reported that orally administered THC (20 mg) in a cookie yielded low and irregular plasma concentrations, compared to intravenous and inhaled THC [5].
3.1.4. Cannabinoid Concentrations after Frequent Use
Most THC plasma data have been collected following acute exposure; less is known of plasma THC concentrations in frequent users. Peat reported THC, 11-OH-THC, and THC-COOH plasma concentrations in frequent cannabis users of 0.86±0.22, 0.46±0.17, and 45.8±13.1 ng/ml, respectively, a minimum of 12 h after the last smoked dose [136]. No difference in terminal half-life in frequent or infrequent users was observed. Johansson et al. administered radiolabeled THC to frequent cannabis users, and found a terminal elimination half-life of 4.1 d for THC in plasma, due to extensive storage and release from body fat [109].
3.1.5. Prediction Models for Estimation of Cannabis Exposure
There continues to be controversy in the interpretation of cannabinoid results from blood analysis, some general concepts having wide support. A dose-response relationship has been demonstrated for smoked THC and THC plasma concentrations [16][17]. It is well-established that plasma THC concentrations begin to decline prior to the time of peak effects, although it has been shown that THC effects appear rapidly after initiation of smoking [15]. Individual drug concentrations and ratios of cannabinoid metabolite to parent drug concentration have been suggested as potentially useful indicators of recent drug use [24][137]. Some 45 min after cannabis smoking, the ratio [THC-COOH]/[THC] in the plasma was reported to be >1 [77]. This is in agreement with results reported by Mason and McBay [96], and those by Huestis et al. [15], who found that peak effects occurred when THC and THC-COOH concentrations reached equivalency, within 30−45 min after initiation of smoking. Measurement of cannabinoid analytes with short time courses of detection (e.g., 8β,11-dihydroxytetrahydrocannabinol) as markers of recent THC exposure has not found widespread use [96]. Recent exposure (6−8 h) and possible impairment have been linked to plasma THC concentrations in excess of 2−3 ng/ml [14][96]. Gjerde et al. [138] suggested that 1.6 ng/ml of THC in whole blood may indicate possible impairment. This correlates well with the suggested concentration of plasma THC, due to the fact that THC in hemolyzed blood is approximately one-half the concentration of plasma THC [139]. Interpretation is further complicated by residual THC and THC-COOH concentrations found in blood of frequent cannabis users. In general, it is suggested that chronic cannabis smokers may have residual plasma THC concentrations of <2 ng/ml some 12 h after smoking cannabis [136]. Significantly higher residual concentrations of THC-COOH may be found.
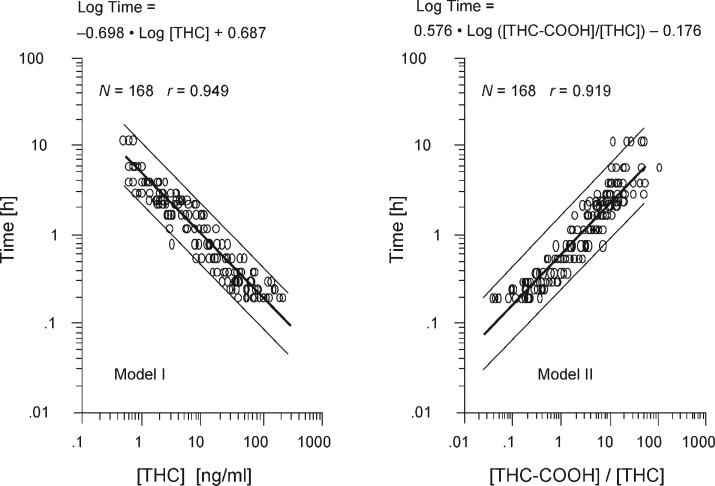
Accurate prediction of the time of cannabis exposure would provide valuable information in establishing the role of cannabis as a contributing factor to events under investigation. Two mathematical models for the prediction of time of cannabis use from the analysis of a single plasma specimen for cannabinoids were developed [140]. Model I is based on THC concentrations, and model II is based on the ratio [THC-COOH]/[THC] in the plasma (Fig. 4). Both models correctly predicted the times of exposure within the 95%-confidence interval for more than 90% of the specimens evaluated. Furthermore, plasma THC and THC-COOH concentrations reported in the literature, following oral and smoked cannabis exposure, in frequent and infrequent cannabis smokers, and with measurements obtained by a wide variety of methods (including radioimmunoassay and GC/MS analysis), were evaluated with these models. Plasma THC concentrations <2.0 ng/ml were excluded from use in both models, due to the possibility of residual THC concentrations in frequent smokers. Manno et al. evaluated the usefulness of these models in predicting the time of cannabis use in a controlled cannabis-smoking study [132]. The models were found to accurately predict the time of last use within the 95%-confidence intervals. Due to the limited distribution of THC and THC-COOH into red blood cells, it is important to remember, when comparing whole-blood THC and/or THC-COOH concentrations to plasma concentrations, to double the whole-blood concentration prior to comparison.
Fig. 4.
Predictive mathematical models for estimating the elapsed time of last cannabis use based on plasma THC and THC-COOH concentrations. Reprinted and adapted with permission by Journal of Analytical Toxicology, p. 285 in [140], Fig. 1.
More recently, the validation of these predictive models was extended to include estimation of time of use after multiple doses of THC and at low THC concentrations (0.5−2 ng/ml), situations that were not included in the original models [141]. Some 38 cannabis users each smoked a cigarette containing 2.64% of THC in the morning, and 30 also smoked a second cigarette in the afternoon. Blood specimens (n=717) were collected at intervals after smoking, and plasma THC and THC-COOH concentrations were measured by GC/MS analysis. The predicted times of cannabis smoking, based on each model, were then compared to the actual smoking times. The most accurate approach applied a combination of models I and II. For all 717 plasma specimens, 99% of the predicted times of last use were within the 95%-confidence interval, 0.9% were overestimated, and none was underestimated. For 289 plasma specimens collected after multiple doses, 97% were correct, with no underestimates. All time estimates were correct for 77 plasma specimens, with THC concentrations of 0.5−2.0 ng/ml, a concentration range not previously examined. The models provide an objective, validated method for assessing the contribution of cannabis to accidents or clinical symptoms.
These models also appeared to be valuable when applied to the small amount of data from published studies of oral ingestion available at the time. Additional studies were performed to determine if the predictive models could estimate last usage after multiple oral doses, a route of administration more popular with the advent of cannabis therapies. A total of 18 subjects received oral THC, as Marinol® or hemp oil [142]. Each of twelve subjects in one group received a single oral dose of dronabinol (10 mg of synthetic THC). In another protocol, six subjects received four different oral daily doses, divided into thirds, and administered with meals for five consecutive days. There was a 10-d washout period between each dosing regimen. The daily doses were 0.39, 0.47, and 14.8 mg of THC in hemp oil, and 7.5 mg in the form of dronabinol. Blood specimens were collected throughout the study, and analyzed for plasma THC and THC-COOH levels by GC/MS analysis, with quantification limits of 0.5 and 1.0 ng/ml, respectively. The actual times between ingestion of THC and blood collection spanned 0.5−16 h. All plasma specimens with analyte concentrations that were equal to or larger than the quantification limit (n=90) were evaluated. Models I and II correctly predicted the time of last THC ingestion in the case of 74.4 and 90.0% of the plasma specimens, respectively. Some 96.7% of the predicted times were correct, with one overestimate and two underestimates, using the time interval defined by the lowest and highest 95%-confidence limit of both models. These results provide further evidence of the usefulness of the predictive models in estimating the time of last oral THC ingestion following single or multiple doses.
3.2. Urine Concentrations
Detection of cannabinoids in urine is indicative of prior cannabis exposure, but the long excretion half-life of THC-COOH in the body, especially in chronic cannabis users, makes it difficult to predict the timing of past drug use. In a single extreme case, one individual's urine was positive at a concentration >20 ng/ml (by immunoassay) up to 67 d after last drug exposure [143]. This individual had used cannabis heavily for more than ten years. However, a naive user's urine may be found negative by immunoassay after only a few hours following smoking of a single cannabis cigarette [144]. Assay cutoff concentrations and the sensitivity and specificity of the immunoassay affect drug-detection times. A positive urine test for cannabinoids indicates only that drug exposure has occurred. The result does not provide information on the route of administration, the amount of drug exposure, when drug exposure occurred, or the degree of impairment.
To date, there are too few urinary data on THC and 11-OH-THC levels to guide interpretation of positive urine cannabinoid tests; however, data are available for guiding interpretation of total urinary THC-COOH concentrations. Total THC-COOH concentrations include both the free THC-COOH and THC-COOH–glucuronide conjugate concentrations determined after alkaline or enzymatic hydrolysis. Substantial intra- and inter-subject variability occurs in patterns of THC-COOH excretion. THC-COOH concentration in the first specimen after smoking is indicative of how rapidly the metabolite can appear in urine. Mean first urine THC-COOH concentrations were 47±22.3 and 75.3±48.9 ng/ml after smoking one cigarette containing 1.75 or 3.55% of THC, respectively [113]. Some 50% of the subjects’ first urine specimen after the low dose, and some 83% of the first urine specimens after the high dose were positive by GC/MS at a THC-COOH cutoff concentration of 15 ng/ml. Thus, THC-COOH concentrations in the first urine specimen are dependent upon the relative potency of the cigarette, the elapsed time following drug administration, smoking efficiency, and individual differences in drug metabolism and excretion. Mean peak urine THC-COOH concentrations averaged at 89.8±31.9 ng/ml (range 20.6−234.2 ng/ml) and 153.4±49.2 ng/ml (range 29.9−355.2 ng/ml) following smoking of ca. 15.8 and 33.8 mg of THC, respectively. The mean times of peak urine concentration were 7.7±0.8 h and 13.9±3.5 h for the low and high dose, respectively. Although peak concentrations appeared to be dose-related, there was a twelvefold variation between individuals.
3.2.1. THC-COOH Detection Windows in Urine
Drug detection time, or the duration of time after drug administration in which the urine of an individual tests positive for cannabinoids, is an important factor in the interpretation of urine drug results. Detection time is dependent on pharmacological factors (e.g., drug dose, type of administration, rates of metabolism and excretion) and analytical factors (e.g., assay sensitivity, specificity, accuracy). Mean detection times in urine following smoking vary considerably between subjects, even in controlled smoking studies, where cannabis dosing is standardized and smoking is computer-paced. During the terminal elimination phase, consecutive urine specimens may fluctuate between positive and negative, as THC-COOH concentrations approach the cutoff concentration. It may be important in drug-treatment settings or in clinical trials to differentiate between new drug use and residual excretion of previously used cannabinoids. After smoking a cigarette containing 1.75% of THC, three out of six subjects had additional positive urine samples interspersed between negative urine samples [144]. This had the effect of producing much longer detection times for the last positive specimen. With a currently accepted confirmation cutoff of 15 ng/ml for THC-COOH, which is most often used in urine-drug testing, the mean GC/MS THC-COOH detection times for the last positive urine sample, following the smoking of a single cigarette with 1.75 or 3.55% of THC, were 33.7±9.2 h (range 8−68.5 h) and 88.6±23.2 h (range 57−122.3 h), respectively. Wingert et al. reported that lowering the urine immunoassay cutoff from 50 to 20 ng/ml, and employing a confirmation cutoff of 10 ng/ml, increased the THC positive rate from 2.8 to 4.1% [145].
3.2.2. Normalization of Cannabinoid Urine Concentrations to Urine Creatinine Concentrations
Normalization of cannabinoid concentration to urine creatinine concentration aids in the differentiation of new from prior cannabis use, and reduces the variability of drug measurement due to urine dilution. Due to the long half-life of drug in the body, especially in chronic cannabis users, toxicologists and practitioners are frequently asked to determine if a positive urine test represents a new episode of drug use or represents continued excretion of residual drug. Random urine specimens contain varying amounts of creatinine, depending on the degree of concentration of the urine. Hawks first suggested creatinine normalization of urine test results to account for variations in urine volume in the bladder [146]. Whereas urine volume is highly variable due to changes in liquid, salt, and protein intake, exercise, and age, creatinine excretion is much more stable.
Manno et al. recommended that an increase of 150% in the creatinine-normalized cannabinoid concentration above the previous specimen can be considered indicative of a new episode of drug exposure [147]. If the increase is greater than or equal to the threshold selected, then new use is predicted. This approach has received wide attention for potential use in treatment and employee-assistance programs, but there was limited evaluation of the usefulness of this ratio under controlled dosing conditions.
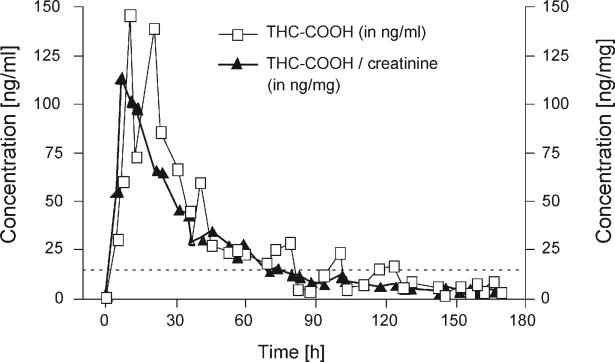
Huestis and Cone conducted a controlled clinical study of the excretion profile of creatinine and cannabinoid metabolites in a group of six cannabis users, who smoked two different doses of cannabis, separated by weekly intervals [148]. As seen in Fig. 5, normalization of urinary THC-COOH concentration to the urinary creatinine concentration produces a smoother excretion pattern and facilitates interpretation of consecutive urine drug-test results.
Fig. 5.
Urine concentrations of THC-COOH and THC-COOH/creatinine for one subject following smoking of a single cannabis cigarette containing 3.55% of THC. Reprinted and adapted with permission by Journal of Analytical Toxicology, p. 450 in [148], Fig. 3.
Being able to differentiate new cannabis use from residual THC-COOH excretion in urine would be highly useful for drug treatment, criminal justice, and employee assistance drug testing programs. We evaluated the ratios of creatinine normalized THC-COOH concentrations from more than 1800 pairs of urine specimens collected during a controlled smoked THC administration study. The ratio times 100 of the creatinine normalized later specimen divided by the creatinine normalized earlier specimen were evaluated for determining the best ratio to predict new cannabis use. A relative operating characteristic (ROC) curve was constructed from sensitivity and specificity data for 26 different cutoffs, ranging from 10 to 200%. The most accurate ratio (85.4%) was 50%, with a sensitivity of 80.1%, a specificity of 90.2%, and false positive and false negative predictions of 5.6 and 7.4%, respectively. When the previously recommended increase of 150% was used as a threshold for new use, sensitivity of detecting new use was only 33.4%, and specificity was high (99.8%), for an overall accuracy prediction of 74.2%. To further substantiate the validity of the derived ROC curve, urine-cannabinoid-metabolite and creatinine data from another controlled clinical trial that specifically addressed water dilution as a means of specimen adulteration were evaluated [149]. Sensitivity, specificity, accuracy, and false positives and negatives were 71.9, 91.6, 83.9, 5.4, and 10.7%, respectively, when the 50% criteria was applied. These data indicate that selection of a threshold to evaluate sequential creatinine-normalized urine drug concentrations can improve the ability to distinguish residual excretion from new drug usage.
Lafolie et al. reported the results of urinary excretion of cannabinoids by a heavy cannabis smoker [150]. Cannabinoids were detectable for 93 d after cessation of smoking, with a decreasing ratio of cannabinoids to creatinine over time. An excretion half-life of 32 d was determined. When cannabinoid concentrations had not been normalized to creatinine concentrations, a number of false positive indications of new drug use would have occurred.
Fraser et al. conducted a series of studies evaluating the application of [THC-COOH]/[creatinine] ratios for urine specimens collected at least 96 h apart from heavy, chronic cannabis users in an outpatient setting [151-153]. Mean urinary THC-COOH concentrations, mean [THC-COOH]/[creatinine] ratios, and mean [THC-COOH]/[creatinine] ratios from consecutively collected specimens were considerably above the proposed 50% ratio to differentiate new use. The proposed 50% ratio was developed from more than 1,800 urine specimens collected after occasional cannabis use on a secure research unit [148]. As suggested, the 50% ratio may not be appropriate for differentiating new drug use from residual drug excretion in heavy users. [THC-COOH]/[Creatinine] ratios decrease reliably until THC-COOH concentrations are between 20−50 ng/ml. Within this range, cannabinoid excretion is more variable, most likely based on the slow and variable release of stored THC from fat tissue. The factors governing release of THC stores are not known. Additional research is being performed to attempt to determine appropriate ratio cutoffs for reliably predicting new drug use in heavy, chronic users.
3.3. Oral-Fluid Testing
Oral fluid also is a suitable specimen for monitoring cannabinoid exposure, and is being evaluated for driving under the influence of drugs, drug treatment, workplace drug testing, and for clinical trials [154-159]. Adequate sensitivity is best achieved with an assay directed toward detection of THC, rather than of 11-OH-THC or THC-COOH. The oral mucosa is exposed to high concentrations of THC during smoking, and serves as the source of THC found in oral fluid. Only minor amounts of drug and metabolites diffuse from the plasma into oral fluid [146]. Following intravenous administration of radiolabeled THC, no radioactivity could be demonstrated in oral fluid [160]. No measurable 11-OH-THC or THC-COOH were found by GC/MS (detection limit 0.5 ng/ml) in oral fluid for 7 d, following cannabis smoking [161], or in oral fluid from 22 subjects positive for THC-COOH in the urine [162]. Oral fluid collected with the Salivette collection device was positive for THC in 14 of these 22 participants. Although no 11-OH-THC or THC-COOH was identified by GC/MS, CBN and CBD were found in addition to THC. Several hours after smoking, the oral mucosa serves as a depot for release of THC into the oral fluid. In addition, as detection limits continue to decrease with the development of new analytical instrumentation, it may be possible to measure low concentrations of THC-COOH in oral fluid.
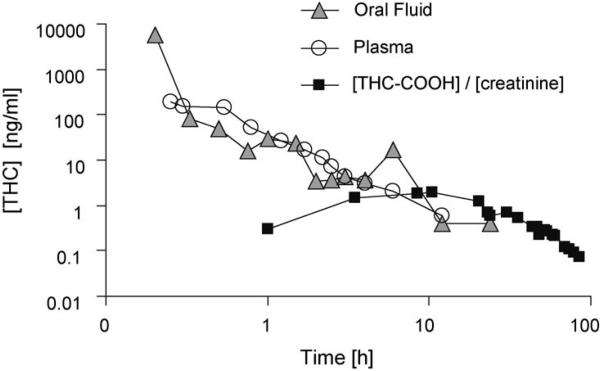
Detection times of cannabinoids in oral fluid are shorter than in urine, and more indicative of recent cannabis use [154][156]. Oral-fluid THC concentrations temporally correlate with plasma cannabinoid concentrations and behavioral and physiological effects, but wide intra- and inter-individual variation precludes the use of oral-fluid concentrations as indicators of drug impairment [161][163]. THC may be detected at low concentrations by radioimmunoassay for up to 24 h after use.
Fig. 6 depicts excretion of THC in oral fluid and plasma, as well as creatinine-normalized THC-COOH excretion in urine in one subject after smoking a single cannabis cigarette containing 3.55% of THC [164]. After smoking cannabis, oral-fluid cannabinoid tests were positive for THC by GC/MS/MS, with a cutoff of 0.5 ng/ml for 13±3 h (range 1−24 h) [165]. After these times, occasional positive oral-fluid results were interspersed with negative tests for up to 34 h.
Peel et al. tested oral-fluid samples from 56 drivers, suspected of being under the influence of cannabis, with the EMIT® screening test and by GC/MS analysis [166]. They suggested that the ease and non-invasiveness of sample collection made oral fluid a useful alternative matrix for detection of recent cannabis use. Oral-fluid samples also are being evaluated in the European Union's Roadside Testing Assessment (ROSITA) project to reduce the number of individuals driving under the influence of drugs and to improve road safety. The ease and non-invasiveness of oral-fluid collection, reduced hazards in specimen handling and testing, and shorter detection window are attractive attributes to the use of this specimen for identifying the presence of potentially performance-impairing drugs.
Laloup et al. compared THC levels in oral fluid (collected with the Intercept® device) and plasma from 139 individuals suspected of driving under the influence of drugs, using LC/MS/MS [167]. They determined that, with a limit of quantification of 0.5 ng/ml in the plasma, the optimal cut-off in oral fluid was 1.2 ng/ml, yielding a sensitivity of 94.7% and a specificity of 92.0%. When a higher plasma cutoff was the target (2 ng/ml), oral fluid THC concentrations of 5.2 ng/ml reliably predicted a positive blood THC result, with a sensitivity of 91.6% and a specificity of 88.6%.
In a recent study of smoked and oral cannabis, the Intercept DOA Oral-Specimen-Collection Device and GC/MS/MS (cutoff 0.5 ng/ml) were paired to monitor oral-fluid cannabinoids in ten participants [165]. As mentioned above, oral-fluid specimens tested positive for up to 34 h. A different oral-fluid collection device, the Cozart RapiScan device, was used with a cannabinoid cutoff of 10 ng/ml to screen for cannabis use [168]. Positive oral-fluid cannabinoid tests were not obtained more than 2 h after last use, suggesting that much lower cutoff concentrations were needed to improve sensitivity. A procedure for direct analysis of cannabinoids in oral fluid with solid-phase micro-extraction and ion-trap GC/MS has been developed, with a limit of detection of 1.0 ng/ml [169]. Detection of cannabinoids in oral fluid is a rapidly developing field; however, there are many scientific issues to resolve. One of the most important is the degree of absorption of the drug to oral-fluid collection devices.
Recently, there has been renewed interest in oral-fluid drug testing for programs associated with drug treatment, workplace, and driving under the influence of drugs. Small and inconsistent specimen volume collection, poor extraction of cannabinoids from the collection device, low analyte concentrations for cannabinoids, and the potential for external contamination from environmental smoke are limitations to this monitoring method. Recently, independent evaluations of the extraction of cannabinoids from the collection device [170-173] and measurement of oral-fluid THC-COOH in concentrations as low as picograms per milliliter appear to adequately address these potential problems. Day et al. reached a detection limit of 10 pg/ml for THC-COOH in oral fluid by GC/MS/MS [174]. Moore et al. developed a GC/MS method using a micro-fluidic Dean's switch for two-dimensional (2D) chromatography to sufficiently improve signal to noise, allowing the monitoring of THC-COOH concentrations of ≥ 2 pg/ml in oral fluid [175]. Extraction efficiency for THC-COOH from the Quantisal™ (Immunalysis, Pomona, CA) oral-fluid collection device was 80% at a concentration of 10 pg/ml, with a coefficient of variation of 8.23%. The extraction efficiency of the buffer was reported to be between 79.6 and 91.4% for various concentrations of THC [173]. Specimens collected almost immediately after smoking cannabis, i.e., after 15 and 45 min, and later, after 1, 2, and 8 h, all contained THC-COOH. This new method was used for the analysis of 143 oral-fluid specimens, screening positive for cannabinoids by Enzyme-Linked Immunosorbent Assay (ELISA). Some 95 specimens (66.4%) tested positive for THC and THC-COOH; 14 (9.7%) were positive for THC-COOH only, and 27 (18.8%) were positive for THC only [176]. The observation that THC-COOH was found in 76.2% of the tested oral-fluid specimens, screening positive for cannabinoids, suggests that there is a definitive means of differentiating passive cannabis exposure from actual cannabis usage. This limitation has curtailed the use of oral-fluid testing to monitor cannabis use.
Niedbala et al. evaluated passive contamination of oral fluid in individuals exposed to cannabis smoke in an enclosed car [177]. First, oral-fluid collection devices were contaminated when opened within the smoke-filled car. When the specimens were collected outside of the car, immediately following smoking, specimens from passive smokers were negative. Environmental cannabis smoke can contaminate collection devices, unless specimens are collected outside the area of smoke contamination.
3.4. Cannabinoids in Sweat
To date, there are no published data on the excretion of cannabinoids in sweat following controlled THC administration, although our laboratory at NIH is conducting such research. Sweat testing is being applied to monitor cannabis use in drug treatment, criminal justice, workplace drug testing, and clinical studies [161][178]. In 1989, Balabanova and Schneider used radioimmunoassay to detect cannabinoids in apocrine sweat [179]. Currently, there is a single commercially available sweat-collection device, the PharmChek patch (PharmChem Laboratories, Texas, USA). Generally, the patch is worn for 7 d, and then exchanged for a new patch once each week during visits to the treatment clinic or parole officer. Theoretically, this permits constant monitoring of drug use throughout the week, extending the window of drug detection and improving test sensitivity. As with oral-fluid testing, this is a developing analytical technique, with much to be learned about the pharmacokinetics of cannabinoid excretion in sweat, potential re-absorption of THC by the skin, possible degradation of THC on the patch, and adsorption of THC onto the patch-collection device. It is known that THC is the primary analyte detected in sweat, with little 11-OH-THC and THC-COOH. Understanding the pharmacokinetics of THC excretion also is important for the interpretation of hair cannabinoid tests, as sweat has been shown to contribute to the amount of drug found in hair (see below).
Several investigators have evaluated the sensitivity and specificity of different screening assays for detecting cannabinoids in sweat [157][180]. Kintz et al. identified THC (4−38 ng/patch) in 20 known heroin abusers who wore the PharmChek patch for 5 d, while attending a detoxification center [181]. Sweat was extracted with MeOH, and analyzed by GC/MS. The same investigators also evaluated forehead swipes with cosmetic pads for monitoring cannabinoids in sweat from individuals suspected of driving under the influence of drugs [162]. THC, but not 11-OH-THC or THC-COOH, was detected (4−152 ng/pad) by GC/EI-MS in the sweat of 16 out of 22 individuals who tested positive for cannabinoids in urine. Ion-trap tandem mass spectrometry also has been used to measure cannabinoids in sweat collected with the PharmChek sweat patch, with a detection limit of 1 ng/patch [182].
3.5. Cannabinoids in Hair
There are multiple mechanisms for the incorporation of cannabinoids in hair. THC and its metabolites may be incorporated into the hair bulb that is surrounded by capillaries. Drug may also diffuse into hair from sebum secreted onto the hair shaft, and from sweat excreted onto the skin surface. Drug may also be incorporated into hair from the environment. Cannabis is primarily smoked, providing an opportunity for environmental contamination of hair with THC in cannabis smoke. Basic drugs such as cocaine and methamphetamine concentrate in hair due to ionic bonding to melanin, the pigment in hair that determines hair color. The more neutral and lipophilic THC is not strongly bound to melanin, resulting in much lower concentrations of THC in hair as compared to other drugs of abuse. Usually, THC is present in hair at a higher concentration than its THC-COOH metabolite [183-186].
An advantage of measuring THC-COOH in hair is that this compound is not present in cannabis smoke, avoiding the issue of passive exposure from the environment. Analysis of cannabinoids in hair is challenging due to the high analytical sensitivity required. THC-COOH is present in the femto- to picogram range per milligram of hair. GC/MS/MS Analysis has been required in most analytical investigations, but a new procedure based on GC/MS equipped with a Dean's switch and cryofocusing was recently published [187]. Cirimele et al. [188] proposed a novel approach to the screening of hair specimens for the presence of cannabinoids in hair. They developed a rapid, simple GC/MS screening method for THC, CBN, and CBD in hair, which did not require derivatization prior to analysis. The method was found to be a sensitive screen for cannabis detection by GC/MS analysis; identification of THC-COOH was recommended as a confirmatory procedure.
It is difficult to conduct controlled cannabinoid-administration studies on the disposition of cannabinoids in hair because of the inability to differentiate administered drug from previously self-administered cannabis. If isotopically labeled drug were administered, it would be possible to identify newly administered drug in hair. There are advantages to monitoring drug use with hair testing, including a wide window of drug detection, a less invasive specimen-collection procedure, and the ability to collect a second specimen at a later time. However, one of the weakest aspects of testing for cannabinoids in hair is the low sensitivity of drug detection in this alternate matrix.
In the only controlled cannabinoid dosing study published to date, Huestis et al. collected 53 head-hair specimens from 38 males with a history of cannabis use documented by questionnaire, urinalysis, and controlled, double-blind administration of THC [189]. Subjects completed a questionnaire indicating daily cannabis use (N=18) or non-daily use, i.e., smoking one to five cannabis cigarettes per week (N=20). Hair specimens were collected from each subject at the time of admittance to a closed research unit, following smoking of two cigarettes containing 2.7% of THC (N=13), or following multiple oral doses with a total of 116 mg THC (N=2). Pre- and post-dose detection rates did not differ statistically. Therefore, all 53 specimens were considered as one group. Some 19 specimens (36%) had no detectable THC or THC-COOH at the GC/MS/MS limits of quantification of 1.0 and 0.1 pg/mg hair, respectively. Two specimens (3.8%) had measurable THC only, 14 (26%) showed THC-COOH only, and 18 (34%) had both cannabinoids. Detection rates were significantly different (p<0.05, Fisher's exact test) between daily cannabis users (85%) and non-daily users (52%). There was no difference in detection rates between African, American, and Caucasian subjects (p>0.3, Fisher's exact test). For specimens with detectable cannabinoids, concentrations ranged from 3.4 to >100 pg THC/mg, and from 0.10 to 7.3 pg THC-COOH/mg hair. THC and THC-COOH concentrations were positively correlated (r=0.38, p<0.01, Pearson's product moment correlation). Only about one-third of non-daily users and two-thirds of daily cannabis users gave rise to positive cannabinoid hair tests by GC/MS/MS, with detection limits of 1 and 0.1 ng/mg for THC and THC-COOH, respectively. All participants showed positive urine cannabinoid tests at the time of hair collection.
4. Conclusions
An understanding of human cannabinoid pharmacokinetics is important for the development and monitoring of new therapeutic medications and to the interpretation of cannabinoid test results in a wide variety of biological matrices, including blood, plasma, urine, oral fluid, sweat, and hair. With the advent of new preparations containing THC, CBD, and other cannabinoids, and new administration routes, additional research is needed. Also, controlled drug-administration studies that provide the scientific database for interpreting cannabinoid concentrations in biological fluids and tissues are increasingly difficult to conduct due to safety and ethical concerns, and because of the high costs of performing human research. However, these data are essential for appropriate application of pharmacotherapies, and for drug testing in treatment, workplace, and forensic cases.
Fig. 6.
Excretion patterns of THC in oral fluid and plasma, and urinary THC-COOH/creatinine levels in a human subject following smoking of a single cannabis cigarette containing 3.55% of THC. The THC-COOH/creatinine ratio is illustrated for all urine specimens collected through the last positive specimen. Analyses were performed by GC/MS at cutoff concentrations of 0.5 ng/ml for oral-fluid and plasma samples, and at 15 ng/ml for urine samples, resp. Reprinted and adapted with permission by Journal of Analytical Toxicology, p. 397 in [164], Fig. 2.
Footnotes
Unless noted otherwise, THC always refers to the Δ9-variant.
Non-systematic compound names cited in the literature are used for the sake of clarity.
REFERENCES
- 1.Turner CE, ElSohly MA, Boeren EG. J. Nat. Prod. 1980;43:169. doi: 10.1021/np50008a001. [DOI] [PubMed] [Google Scholar]
- 2.Claussen U, Korte F. Justus Liebigs Ann. Chem. 1968;713:162. doi: 10.1002/jlac.19687130119. [DOI] [PubMed] [Google Scholar]
- 3.ElSohly HN, Boeren EG, Turner CE, ElSohly MA. In: The Cannabinoids: Chemical, Pharmacologic and Therapeutic Aspects. Agurell S, Dewey WL, Willette RE, editors. Academic Press; Orlando: 1984. p. 89. [Google Scholar]
- 4.Mechoulam R. Science. 1970;168:1159. doi: 10.1126/science.168.3936.1159. [DOI] [PubMed] [Google Scholar]
- 5.Ohlsson A, Lindgren JE, Wahlen A, Agurell S, Hollister LE, Gillespie HK. Clin. Pharmacol. Ther. 1980;28:409. doi: 10.1038/clpt.1980.181. [DOI] [PubMed] [Google Scholar]
- 6.Agurell S, Leander K. Acta Pharm. Suecica. 1971;8:391. [PubMed] [Google Scholar]
- 7.Ohlsson A, Agurell S, Londgren JE, Gillespie HK, Hollister LE. In: Pharmacokinetics and Pharmacodynamics of Psychoactive Drugs. Barnett G, Chiang CN, editors. Mosby Yearbook; St. Louis: 1985. p. 75. [Google Scholar]
- 8.Agurell S, Halldin M, Lindgren JE, Ohlsson A, Widman M, Gillespie H, Hollister L. Pharmacol. Rev. 1986;38:21. [PubMed] [Google Scholar]
- 9.Ohlsson A, Lindgren JE, Wahlen A, Agurell S, Hollister LE, Gillespie HK. Biomed. Environ. Mass Spectrom. 1982;9:6. doi: 10.1002/bms.1200140904. [DOI] [PubMed] [Google Scholar]
- 10.Azorlosa JL, Heishman SJ, Stitzer ML, Mahaffey JM. J. Pharmacol. Exper. Ther. 1992;261:114. [PubMed] [Google Scholar]
- 11.Heishman SJ, Stitzer ML, Yingling JE. Pharmacol. Biochem. Behav. 1989;34:173. doi: 10.1016/0091-3057(89)90369-9. [DOI] [PubMed] [Google Scholar]
- 12.Perez-Reyes M. NIDA Res. Monograph. 1990;99:42. [PubMed] [Google Scholar]
- 13.Cami J, Guerra D, Ugena B, Segura J, de La Torre R. Pharmacol. Biochem. Behav. 1991;40:115. doi: 10.1016/0091-3057(91)90330-5. [DOI] [PubMed] [Google Scholar]
- 14.Huestis MA, Henningfield JE, Cone EJ. J. Anal. Toxicol. 1992;16:276. doi: 10.1093/jat/16.5.276. [DOI] [PubMed] [Google Scholar]
- 15.Huestis MA, Sampson AH, Holicky BJ, Henningfield JE, Cone EJ. Clin. Pharmacol. Ther. 1992;52:31. doi: 10.1038/clpt.1992.100. [DOI] [PubMed] [Google Scholar]
- 16.Perez-Reyes M, Di Guiseppi S, Davis KH, Schindler VH, Cook CE. Clin. Pharmacol. Ther. 1982;31:617. doi: 10.1038/clpt.1982.86. [DOI] [PubMed] [Google Scholar]
- 17.Perez-Reyes M, Owens SM, Di Guiseppi S. J. Clin. Pharmacol. 1981;21:201S. doi: 10.1002/j.1552-4604.1981.tb02596.x. [DOI] [PubMed] [Google Scholar]
- 18.ElSohly MA, Ross SA, Mehmedic Z, Arafat R, Banahan BFI. J. Forensic Sci. 2000;45:24. [PubMed] [Google Scholar]
- 19.Russo EB, McPartland JM. Psychopharmacology. 2003;165:431. doi: 10.1007/s00213-002-1348-z. [DOI] [PubMed] [Google Scholar]
- 20.Bornheim LM, Grillo MP. Chem. Res. Toxicol. 1998;11:1209. doi: 10.1021/tx9800598. [DOI] [PubMed] [Google Scholar]
- 21.Harvey DJ. In: Marijuana and Medicine. Nahas GG, Sutin KM, Harvey DJ, Agurell S, editors. Humana Press; Totowa: 2001. p. 91. [Google Scholar]
- 22.Mechoulam R, Hanus L. Chem. Phys. Lipids. 2002;121:35. doi: 10.1016/s0009-3084(02)00144-5. [DOI] [PubMed] [Google Scholar]
- 23.Harder S, Rietbrock S. Int. J. Clin. Pharmacol. Ther. 1997;35:155. [PubMed] [Google Scholar]
- 24.Law B, Mason PA, Moffat AC, Gleadle RI, King LJ. J. Pharm. Pharmacol. 1984;36:289. doi: 10.1111/j.2042-7158.1984.tb04376.x. [DOI] [PubMed] [Google Scholar]
- 25.Ohlsson A, Lindgren JE, Wahlen A, Agurell S, Hollister LE, Gillespie HK. NIDA Res. Monograph. 1981;34:250. [PubMed] [Google Scholar]
- 26.Perez-Reyes M, Lipton MA, Timmons MC, Wall ME, Brine DR, Davis KH. Clin. Pharmacol. Ther. 1973;14:48. doi: 10.1002/cpt197314148. [DOI] [PubMed] [Google Scholar]
- 27.Wall ME, Sadler BM, Brine D, Taylor H, Perez-Reyes M. Clin. Pharmacol. Ther. 1983;34:352. doi: 10.1038/clpt.1983.179. [DOI] [PubMed] [Google Scholar]
- 28.Kim KR, Yoon HR. J. Chromatogr., Sect. B. 1996;682:55. doi: 10.1016/0378-4347(96)00045-x. [DOI] [PubMed] [Google Scholar]
- 29.Binitie A. Psychopharmacologia. 1975;44:301. doi: 10.1007/BF00428911. [DOI] [PubMed] [Google Scholar]
- 30.Meier HJ, Vonesch HJ. Schweiz. Med. Wochenschr. 1997;127:214. [PubMed] [Google Scholar]
- 31.Goodwin RS, Gustafson RA, Barnes A, Nebro W, Moolchan ET, Huestis MA. Ther. Drug Monit. 2006;28:545. doi: 10.1097/00007691-200608000-00010. [DOI] [PubMed] [Google Scholar]
- 32.Gustafson RA, Moolchan ET, Barnes A, Levine B, Huestis MA. J. Chromatogr., B. 2003;798:145. doi: 10.1016/j.jchromb.2003.09.022. [DOI] [PubMed] [Google Scholar]
- 33.Nadulski T, Sporkert F, Schnelle M, Stadelmann AM, Roser P, Schefter T, Pragst F. J. Anal. Toxicol. 2005;29:782. doi: 10.1093/jat/29.8.782. [DOI] [PubMed] [Google Scholar]
- 34.Mechoulam R. Br. J. Pharmacol. 2005;146:913. doi: 10.1038/sj.bjp.0706415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Zias J, Stark H, Seligman J, Levy R, Werker E, Breuer A, Mechoulam R. Nature. 1993;363:215. doi: 10.1038/363215a0. [DOI] [PubMed] [Google Scholar]
- 36.Russo E, Guy GW. Med. Hypotheses. 2006;66:234. doi: 10.1016/j.mehy.2005.08.026. [DOI] [PubMed] [Google Scholar]
- 37.Vaughan CW, Christie MJ. In: Cannabis and Cannabinoids: Pharmacology, Toxicology, and Therapeutic Potential. Grotenhermen F, Russo E, editors. The Haworth Integrative Healing Press; New York: 1984. p. 89. [Google Scholar]
- 38.Holdcroft A. In: Cannabis and Cannabinoids: Pharmacology, Toxicology, and Therapeutic Potential. Grotenhermen F, Russo E, editors. The Haworth Integrative Healing Press; New York: 1984. p. 181. [Google Scholar]
- 39.Zajicek J, Fox P, Sanders H, Wright D, Vickery J, Nunn A, Thompson A. Lancet. 2003;362:1517. doi: 10.1016/S0140-6736(03)14738-1. [DOI] [PubMed] [Google Scholar]
- 40.Mattes RD, Shaw LM, Edling-Owens J, Engelman K, ElSohly MA. Pharmacol. Biochem. Behav. 1993;44:745. doi: 10.1016/0091-3057(93)90194-x. [DOI] [PubMed] [Google Scholar]
- 41.Mattes RD, Engelman K, Shaw LM, ElSohly MA. Pharmacol. Biochem. Behav. 1994;49:187. doi: 10.1016/0091-3057(94)90475-8. [DOI] [PubMed] [Google Scholar]
- 42.Brenneisen R, Egli A, ElSohly MA, Henn V, Spiess Y. Int. J. Clin. Pharmacol. Ther. 1996;34:446. [PubMed] [Google Scholar]
- 43.Stinchcomb AL, Valiveti S, Hammell DC, Ramsey DR. J. Pharm. Pharmacol. 2004;56:291. doi: 10.1211/0022357022791. [DOI] [PubMed] [Google Scholar]
- 44.Scheuplein RJ. J. Invest. Dermatol. 1967;48:79. [PubMed] [Google Scholar]
- 45.Challapalli PV, Stinchcomb AL. Int J. Pharm. 2002;241:329. doi: 10.1016/s0378-5173(02)00262-4. [DOI] [PubMed] [Google Scholar]
- 46.Valiveti S, Hammell DC, Earles DC, Stinchcomb AL. J. Pharm. Sci. 2004;93:1154. doi: 10.1002/jps.20036. [DOI] [PubMed] [Google Scholar]
- 47.Vinciguerra V, Moore T, Brennan E. N. Y. State J. Med. 1988;88:525. [PubMed] [Google Scholar]
- 48.D'Souza DC, Perry E, MacDougall L, Ammerman Y, Cooper T, Wu YT, Braley G, Gueorguieva R, Krystal JH. Neuropsychopharmacology. 2004;29:1558. doi: 10.1038/sj.npp.1300496. [DOI] [PubMed] [Google Scholar]
- 49.Perez-Reyes M, Timmons MC, Davis KH, Wall EM. Experientia. 1973;29:1368. doi: 10.1007/BF01922823. [DOI] [PubMed] [Google Scholar]
- 50.Benowitz NL, Nguyen TL, Jones RT, Herning RI, Bachman J. Clin. Pharm. Ther. 1980;28:115. doi: 10.1038/clpt.1980.139. [DOI] [PubMed] [Google Scholar]
- 51.Hampson AJ, Grimaldi M, Axelrod J, Wink D. Proc. Natl. Acad. Sci. U.S.A. 1998;95:8268. doi: 10.1073/pnas.95.14.8268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Karst M, Salim K, Burstein S, Conrad I, Hoy L, Schneider U. J. Am. Med. Assoc. 2003;290:1757. doi: 10.1001/jama.290.13.1757. [DOI] [PubMed] [Google Scholar]
- 53.Melamede R. In: Cannabis and Cannabinoids: Pharmacology, Toxicology, and Therapeutic Potential. Grotenhermen F, Russo E, editors. The Haworth Integrative Healing Press; New York: 1984. p. 111. [Google Scholar]
- 54.Plasse T. In: Cannabis and Cannabinoids: Pharmacology, Toxicology, and Therapeutic Potential. Grotenhermen F, Russo E, editors. The Haworth Integrative Healing Press; New York: 1984. p. 165. [Google Scholar]
- 55.Baker D, Pryce G, Croxford JL, Brown P, Pertwee RG, Huffman JW, Layward L. Nature. 2000;404:84. doi: 10.1038/35003583. [DOI] [PubMed] [Google Scholar]
- 56.Malfait AM, Galllily R, Sumariwalla PF, Malik AS, Andreakos E, Mechoulam R, Feldmann M. Proc. Natl. Acad. Sci. U.S.A. 2000;97:9561. doi: 10.1073/pnas.160105897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Zuardi AW, Shirakawa I, Finkelfarb E, Karniol IG. Psychopharmacology. 1982;76:245. doi: 10.1007/BF00432554. [DOI] [PubMed] [Google Scholar]
- 58.McArdle K, Mackie P, Pertwee R, Guy G, Whittle B, Hawksworth G. Toxicology. 2001;168:133. [Google Scholar]
- 59.Agurell S, Gillespie H, Halldin M, Hollister LE, Johansson E, Lindgren JE, Ohlsson A, Szirmai M, Widman M. In: Marihuana '84: Proceedings of the Oxford Symposium on Cannabis. Harvey DJ, Paton WDM, Nahas GG, editors. IRL Press; Oxford: 1984. p. 49. [Google Scholar]
- 60.Ohlsson A, Lindgren JE, Andersson S, Agurell S, Gillespie H, Hollister LE. Biomed. Environ. Mass Spectrom. 1986;13:77. doi: 10.1002/bms.1200130206. [DOI] [PubMed] [Google Scholar]
- 61.Agurell S, Carlsson S, Lindgren JE, Ohlsson A, Gillespie H, Hollister L. Experientia. 1981;37:1090. doi: 10.1007/BF02085029. [DOI] [PubMed] [Google Scholar]
- 62.Guy GW, Robson PJ. J. Cannabis Ther. 2004;3:121. [Google Scholar]
- 63.Guy GW, Robson PJ. J. Cannabis Ther. 2004;3:79. [Google Scholar]
- 64.Lemberger L, Silberstein SD, Axelrod J, Kopin IJ. Science. 1970;170:1320. doi: 10.1126/science.170.3964.1320. [DOI] [PubMed] [Google Scholar]
- 65.Nahas GG, Frick HC, Lattimer JK, Latour C, Harvey D. Human Psychopharmacol. 2002;17:103. doi: 10.1002/hup.369. [DOI] [PubMed] [Google Scholar]
- 66.Kreuz DS, Axelrod J. Science. 1973;179:391. doi: 10.1126/science.179.4071.391. [DOI] [PubMed] [Google Scholar]
- 67.Garrett ER. Adv. Biosci. 1978;22−23:105. doi: 10.1016/b978-0-08-023759-6.50014-7. [DOI] [PubMed] [Google Scholar]
- 68.Harvey DJ, Leuschner JTA, Paton WDM. In: Marihuana '84: Proceedings of the Oxford Symposium on Cannabis. Harvey DJ, Paton WDM, Nahas GG, editors. IRL Press; Oxford: 1984. p. 77. [Google Scholar]
- 69.Johansson E, Norén K, Sjövall J, Halldin MM. Biomed. Chromatogr. 1989;3:35. doi: 10.1002/bmc.1130030109. [DOI] [PubMed] [Google Scholar]
- 70.Grotenhermen F. Clin. Pharmacokinet. 2003;42:327. doi: 10.2165/00003088-200342040-00003. [DOI] [PubMed] [Google Scholar]
- 71.Dewey WL, McMillan DE, Harris LS, Turk RF. Biochem. Pharmacol. 1972;22:399. doi: 10.1016/0006-2952(73)90420-6. [DOI] [PubMed] [Google Scholar]
- 72.Hunt CA, Jones RT. J. Pharmacol. Exper. Ther. 1980;215:35. [PubMed] [Google Scholar]
- 73.Adams IB, Martin BR. Addiction. 1996;91:1585. [PubMed] [Google Scholar]
- 74.Mura P, Kintz P, Dumestre V, Raul S, Hauet T. J. Anal. Toxicol. 2005;29:842. doi: 10.1093/jat/29.8.842. [DOI] [PubMed] [Google Scholar]
- 75.Brunet B, Doucet C, Venisse N, Hauet T, Hebrard W, Papet Y, Mauco G, Mura P. Forensic Sci. Int. 2006;161:169. doi: 10.1016/j.forsciint.2006.04.018. [DOI] [PubMed] [Google Scholar]
- 76.Perez-Reyes M, Timmons MC, Lipton MA, Davis KH, Wall ME. Science. 1972;177:633. doi: 10.1126/science.177.4049.633. [DOI] [PubMed] [Google Scholar]
- 77.Kelly P, Jones RT. J. Anal. Toxicol. 1992;16:228. doi: 10.1093/jat/16.4.228. [DOI] [PubMed] [Google Scholar]
- 78.Skopp G, Potsch L, Mauden M, Richter B. Forensic Sci. Int. 2002;126:17. doi: 10.1016/s0379-0738(02)00023-3. [DOI] [PubMed] [Google Scholar]
- 79.Lee CC, Chiang CN. NIDA Res. Monograph. 1985;60:110. [PubMed] [Google Scholar]
- 80.Bailey JR, Cunny HC, Paule M, Slikker W., Jr. Toxicol. Appl. Pharmacol. 1987;90:315. doi: 10.1016/0041-008x(87)90338-3. [DOI] [PubMed] [Google Scholar]
- 81.Martin BR, Dewey WL, Harris LS, Beckner JS. Res. Commun. Chem. Pathol. Pharmacol. 1977;17:457. [PubMed] [Google Scholar]
- 82.Blackard C, Tennes K. New Engl. J. Med. 1984;311:797. doi: 10.1056/NEJM198409203111213. [DOI] [PubMed] [Google Scholar]
- 83.Atkinson HC, Begg EJ, Darrlow BA. Clin. Pharmacokinet. 1988;14:217. doi: 10.2165/00003088-198814040-00003. [DOI] [PubMed] [Google Scholar]
- 84.Perez-Reyes M, Wall ME. N. Engl. J. Med. 1982;307:819. doi: 10.1056/NEJM198209233071311. [DOI] [PubMed] [Google Scholar]
- 85.Burstein S, Rosenfeld J, Wittstruck T. Science. 1972;176:422. doi: 10.1126/science.176.4033.422. [DOI] [PubMed] [Google Scholar]
- 86.Ben-Zvi Z, Bergen JR, Burstein S, Sehgal PK, Varanelli C. In: The Pharmacology of Marijuana. Braude MC, Szara S, editors. Raven Press; New York: 1976. p. 63. [Google Scholar]
- 87.Ben-Zvi Z, Burstein S. Res. Commun. Chem. Pathol. Pharmacol. 1974;8:223. [PubMed] [Google Scholar]
- 88.Harvey DJ, Martin BR, Paton WDM. In: Marijuana: Biological Effects. Nahas GG, Paton WDM, editors. Pergamon Press; Oxford: 1979. p. 45. [Google Scholar]
- 89.Iribarne C, Berthou F, Baird S, Dreano Y, Picart D, Bail JP, Beaune P, Menez JF. Chem. Res. Toxicol. 1996;9:365. doi: 10.1021/tx950116m. [DOI] [PubMed] [Google Scholar]
- 90.Matsunaga T, Iwawaki Y, Watanabe K, Yamamoto I, Kageyama T, Yoshimura H. Life Sci. 1995;56:2089. doi: 10.1016/0024-3205(95)00193-a. [DOI] [PubMed] [Google Scholar]
- 91.Harvey DJ, Paton WDM. Rev. Biochem. Toxicol. 1986;6:221. [Google Scholar]
- 92.Bornheim LM, Lasker JM, Raucy JL. Drug Metab. Dispos. 1992;20:241. [PubMed] [Google Scholar]
- 93.McBurney LJ, Bobbie BA, Sepp LA. J. Anal. Toxicol. 1986;10:56. doi: 10.1093/jat/10.2.56. [DOI] [PubMed] [Google Scholar]
- 94.Mechoulam R, Zvi ZB, Agurell S, Nilsson IM, Nilsson JLG, Edery H, Grunfeld Y. Experientia. 1973;29:1193. doi: 10.1007/BF01935065. [DOI] [PubMed] [Google Scholar]
- 95.Halldin MM, Widman M, Bahr CV, Lindgren JE, Martin BR. Drug Metab. Dispos. 1982;10:297. [PubMed] [Google Scholar]
- 96.Mason AP, McBay AJ. J. Forensic Sci. 1985;30:615. [PubMed] [Google Scholar]
- 97.Sporkert F, Pragst F, Ploner CJ, Tschirch A, Stadelmann AM. Annual Meeting of the International Association of Forensic Toxicologists (TIAFT); Prague, Czech Republic. August 26−30, 2001.p. 62. [Google Scholar]
- 98.Garrett ER, Hunt CA. J. Pharm. Sci. 1977;66:395. doi: 10.1002/jps.2600660322. [DOI] [PubMed] [Google Scholar]
- 99.Lemberger L, Tamarkin NR, Axelrod J. Science. 1971;173:72. doi: 10.1126/science.173.3991.72. [DOI] [PubMed] [Google Scholar]
- 100.Harvey DJ, Mechoulam R. Xenobiotica. 1990;20:303. doi: 10.3109/00498259009046849. [DOI] [PubMed] [Google Scholar]
- 101.Greene ML, Saunders DR. Gastroenterology. 1974;66:365. [PubMed] [Google Scholar]
- 102.Krishna DR, Klotz U. Clin. Pharmacokinet. 1994;26:144. doi: 10.2165/00003088-199426020-00007. [DOI] [PubMed] [Google Scholar]
- 103.Watanabe K, Tanaka T, Yamamoto I, Yoshimura H. Biochem. Biophys. Res. Commun. 1988;157:75. doi: 10.1016/s0006-291x(88)80013-5. [DOI] [PubMed] [Google Scholar]
- 104.Widman M, Nordqvist M, Dollery CT, Briant RH. J. Pharm. Pharmacol. 1975;27:842. doi: 10.1111/j.2042-7158.1975.tb10227.x. [DOI] [PubMed] [Google Scholar]
- 105.Wall ME, Brine DR, Perez-Reyes M. In: The Pharmacology of Marihuana. Braude MC, Szara S, editors. Raven Press; New York: 1976. p. 93. [Google Scholar]
- 106.Hunt CA, Jones RT, Herning RI, Bachman J. J. Pharmacokinet. Biopharm. 1981;9:245. doi: 10.1007/BF01059266. [DOI] [PubMed] [Google Scholar]
- 107.Nadulski T, Pragst F, Weinberg G, Roser P, Schnelle M, Fronk EM, Stadelmann AM. Ther. Drug Monit. 2005;27:799. doi: 10.1097/01.ftd.0000177223.19294.5c. [DOI] [PubMed] [Google Scholar]
- 108.Williams PL, Moffat AC. J. Pharm. Pharmacol. 1980;32:445. doi: 10.1111/j.2042-7158.1980.tb12966.x. [DOI] [PubMed] [Google Scholar]
- 109.Johansson E, Agurell S, Hollister LE, Halldin MM. J. Pharm. Pharmacol. 1988;40:374. doi: 10.1111/j.2042-7158.1988.tb05272.x. [DOI] [PubMed] [Google Scholar]
- 110.Johansson E, Halldin MM, Agurell S, Hollister LE, Gillespie HK. Eur. J. Clin. Pharmacol. 1989;37:273. doi: 10.1007/BF00679783. [DOI] [PubMed] [Google Scholar]
- 111.Johansson E, Halldin MM. J. Anal. Toxicol. 1989;13:218. doi: 10.1093/jat/13.4.218. [DOI] [PubMed] [Google Scholar]
- 112.Chiang CN, Rapaka RS. NIDA Res. Monograph. 1987;79:173. [PubMed] [Google Scholar]
- 113.Huestis MA, Mitchell JM, Cone EJ. J. Anal. Toxicol. 1996;20:441. doi: 10.1093/jat/20.6.441. [DOI] [PubMed] [Google Scholar]
- 114.Lindgren JE, Ohlsson A, Agurell S, Hollister L, Gillespie H. Psychopharmacology. 1981;74:208. doi: 10.1007/BF00427095. [DOI] [PubMed] [Google Scholar]
- 115.Wall ME, Perez-Reyes M. J. Clin. Pharmacol. 1981;21:178S. doi: 10.1002/j.1552-4604.1981.tb02594.x. [DOI] [PubMed] [Google Scholar]
- 116.Gustafson RA, Levine B, Stout PR, Klette KL, George MP, Moolchan ET, Huestis MA. Clin. Chem. 2003;49:1114. doi: 10.1373/49.7.1114. [DOI] [PubMed] [Google Scholar]
- 117.Gustafson RA, Kim I, Stout PR, Klette KL, George MP, Moolchan ET, Levine B, Huestis MA. J. Anal. Toxicol. 2004;28:160. doi: 10.1093/jat/28.3.160. [DOI] [PubMed] [Google Scholar]
- 118.Kemp PM, Abukhalaf IK, Manno JE, Manno BR, Alford DD, McWilliams ME, Nixon FE, Fitzgerald MJ, Reeves RR, Wood MJ. J. Anal. Toxicol. 1995;19:292. doi: 10.1093/jat/19.5.292. [DOI] [PubMed] [Google Scholar]
- 119.Kemp PM, Abukhalaf IK, Manno JE, Manno BR, Alford DD, Abusada GA. J. Anal. Toxicol. 1995;19:285. doi: 10.1093/jat/19.5.285. [DOI] [PubMed] [Google Scholar]
- 120.Blanc JA, Manneh VA, Ernst R, Berger DE, de Keczer SA, Chase C, Centofanti JM, DeLizza AJ. Clin. Chem. 1993;39:1705. [PubMed] [Google Scholar]
- 121.Bloom AS. J. Pharmacol. Exper. Ther. 1982;221:97. [PubMed] [Google Scholar]
- 122.Christophersen AS. J. Anal. Toxicol. 1986;10:129. doi: 10.1093/jat/10.4.129. [DOI] [PubMed] [Google Scholar]
- 123.Joern WA. J. Anal. Toxicol. 1992;16:401. doi: 10.1093/jat/16.6.401. [DOI] [PubMed] [Google Scholar]
- 124.Garrett ER, Hunt CA. J. Pharm. Sci. 1974;63:1056. doi: 10.1002/jps.2600630705. [DOI] [PubMed] [Google Scholar]
- 125.Huang W, Moody DE, Andrenyak DM, Smith EK, Foltz RL, Huestis MA, Newton JF. J. Anal. Toxicol. 2001;25:531. doi: 10.1093/jat/25.7.531. [DOI] [PubMed] [Google Scholar]
- 126.Owens SM, McBay AJ, Reisner HM, Perez-Reyes M. Clin. Chem. 1981;27:619. [PubMed] [Google Scholar]
- 127.Lemberger L, Crabtree RE, Rowe HM. Science. 1972;177:62. doi: 10.1126/science.177.4043.62. [DOI] [PubMed] [Google Scholar]
- 128.Moeller MR, Doerr G, Warth S. J. Forensic Sci. 1992;37:969. [PubMed] [Google Scholar]
- 129.Feng S, ElSohly MA, Salamone S, Salem MY. J. Anal. Toxicol. 2000;24:395. doi: 10.1093/jat/24.6.395. [DOI] [PubMed] [Google Scholar]
- 130.Foltz RL. In: Advances in Analytical Toxicology. Baselt RC, editor. Biomedical Publications; Foster City: 1984. p. 125. [Google Scholar]
- 131.Green MD, Belanger G, Hum DW, Belanger A, Tephly TR. Drug Metab. Dispos. 1997;25:1389. [PubMed] [Google Scholar]
- 132.Manno JE, Manno BR, Kemp PM, Alford DD, Abukhalaf IK, McWilliams ME, Hagaman FN, Fitzgerald MJ. J. Anal. Toxicol. 2001;25:538. doi: 10.1093/jat/25.7.538. [DOI] [PubMed] [Google Scholar]
- 133.Wall ME, Taylor HL. In: Marihuana '84: Proceedings of the Oxford Symposium on Cannabis. Harvey DJ, Paton SW, Nahas GG, editors. IRL Press; Oxford: 1984. p. 69. [Google Scholar]
- 134.Shaw LM, Edling-Owens J, Mattes R. Clin. Chem. 1991;37:2062. [PubMed] [Google Scholar]
- 135.Nebro W, Barnes A, Gustafson R, Moolchan E, Huestis M. results presented at the FBI/SOFT/TIAFT Meeting; Washington DC. August 2004. [Google Scholar]
- 136.Peat MA. In: Advances in Analytical Toxicology II. Baselt RC, editor. Year Book Medical Publishers; Chicago: 1989. p. 186. [Google Scholar]
- 137.Hanson VW, Buonarati MH, Baselt RC, Wade NA, Yep C, Biasotti AA, Reeve VC, Wong AS, Orbanowsky MW. J. Anal. Toxicol. 1983;7:96. doi: 10.1093/jat/7.2.96. [DOI] [PubMed] [Google Scholar]
- 138.Gjerde H, Beylich KM, Morland J. Accid. Anal. Prev. 1993;25:479. doi: 10.1016/0001-4575(93)90078-b. [DOI] [PubMed] [Google Scholar]
- 139.Mason AP, McBay AJ. J. Forensic Sci. 1984;29:987. [PubMed] [Google Scholar]
- 140.Huestis MA, Henningfield JE, Cone EJ. J. Anal. Toxicol. 1992;16:283. doi: 10.1093/jat/16.5.283. [DOI] [PubMed] [Google Scholar]
- 141.Huestis MA, Barnes A, Smith ML. Clin. Chem. 2005;51:2289. doi: 10.1373/clinchem.2005.056838. [DOI] [PubMed] [Google Scholar]
- 142.Smith M, Nebro W, Gustafson R, Huestis M. Annual Meeting of the International Association of Forensic Toxicologists (TIAFT); Seoul, Korea. August 29 – September 2, 2005.p. 1. [Google Scholar]
- 143.Ellis GM, Mann MA, Judson BA, Schramm NT, Tashchian A. Clin. Pharmacol. Ther. 1985;38:572. doi: 10.1038/clpt.1985.226. [DOI] [PubMed] [Google Scholar]
- 144.Huestis MA, Mitchell JM, Cone EJ. J. Anal. Toxicol. 1995;19:443. doi: 10.1093/jat/19.6.443. [DOI] [PubMed] [Google Scholar]
- 145.Wingert WE. Clin. Chem. 1997;43:100. [PubMed] [Google Scholar]
- 146.Hawks RL. In: The Cannabinoids: Chemical, Pharmacologic, and Therapeutic Aspects. Agurell S, Dewey W, Willette R, editors. Academic Press; Rockville: 1983. p. 1. [Google Scholar]
- 147.Manno JE, Ferslew KE, Manno BR. In: The Cannabinoids: Chemical, Pharmacologic, and Therapeutic Aspects. Agurell S, Dewey WL, Willette RE, editors. Harcourt Brace Jonanovich; Orlando: 1984. p. 281. [Google Scholar]
- 148.Huestis MA, Cone EJ. J. Anal. Toxicol. 1998;22:445. doi: 10.1093/jat/22.6.445. [DOI] [PubMed] [Google Scholar]
- 149.Cone EJ, Lange R, Darwin WD. J. Anal. Toxicol. 1998;22:460. doi: 10.1093/jat/22.6.460. [DOI] [PubMed] [Google Scholar]
- 150.Lafolie P, Beck O, Blennow G, Boreus L, Borg S, Elwin CE, Karlsson L, Odelius G, Hjemdahl P. Clin. Chem. 1991;37:1927. [PubMed] [Google Scholar]
- 151.Fraser AD, Worth D. Forensic Sci. Int. 2003;137:196. doi: 10.1016/j.forsciint.2003.07.011. [DOI] [PubMed] [Google Scholar]
- 152.Fraser AD, Worth D. Ther. Drug Monit. 2002;24:746. doi: 10.1097/00007691-200212000-00011. [DOI] [PubMed] [Google Scholar]
- 153.Fraser AD, Worth D. Forensic Sci. Int. 2004;143:147. doi: 10.1016/j.forsciint.2004.02.034. [DOI] [PubMed] [Google Scholar]
- 154.Menkes DB, Howard RC, Spears GFS, Cairns ER. Psychopharmacology. 1991;103:277. doi: 10.1007/BF02244217. [DOI] [PubMed] [Google Scholar]
- 155.Gross SJ, Soares JR. J. Anal. Toxicol. 1978;2:98. [Google Scholar]
- 156.Gross SJ, Worthy TE, Nerder L, Zimmermann EG, Soares JR, Lomax P. J. Anal. Toxicol. 1985;9:1. doi: 10.1093/jat/9.1.1. [DOI] [PubMed] [Google Scholar]
- 157.Mura P, Kintz P, Papet Y, Ruesch G, Piriou A. Acta Clin. Belg. 1999;1:35. [PubMed] [Google Scholar]
- 158.Soares JR, Gross SJ. Life Sci. 1976;19:1711. doi: 10.1016/0024-3205(76)90078-3. [DOI] [PubMed] [Google Scholar]
- 159.Soares JR, Grant JD, Gross SJ. NIDA Res. Monograph. 1982;42:44. [PubMed] [Google Scholar]
- 160.Hawks RL. NIDA Res. Monograph. 1982;42:125. [PubMed] [Google Scholar]
- 161.Huestis MA, Cone EJ. In: Drug Abuse Handbook. Karch SB, editor. CRC Press; Boca Raton: 1998. p. 799. [Google Scholar]
- 162.Kintz P, Cirimele V, Ludes B. J. Anal. Toxicol. 2000;24:557. doi: 10.1093/jat/24.7.557. [DOI] [PubMed] [Google Scholar]
- 163.Huestis MA, Dickerson S, Cone EJ. Am. Acad. Forensic Sci. Annual Meeting. 1992:190. [Google Scholar]
- 164.Huestis MA, Cone EJ. J. Anal. Toxicol. 2004;28:394. doi: 10.1093/jat/28.6.394. [DOI] [PubMed] [Google Scholar]
- 165.Niedbala RS, Kardos KW, Fritch DF, Kardos S, Fries T, Waga J. J. Anal. Toxicol. 2001;25:289. doi: 10.1093/jat/25.5.289. [DOI] [PubMed] [Google Scholar]
- 166.Peel HW, Perrigo BJ, Mikhael NZ. J. Forensic Sci. 1984;29:185. [PubMed] [Google Scholar]
- 167.Laloup M, Del Mar Ramirez Fernandez M, Wood M, De Boeck G, Maes V, Samyn N. Forensic Sci. Int. 2006;161:175. doi: 10.1016/j.forsciint.2006.03.033. [DOI] [PubMed] [Google Scholar]
- 168.Jehanli A, Brannan S, Moore L, Spiehler VR. J. Forensic Sci. 2001;46:1214. [PubMed] [Google Scholar]
- 169.Hall BJ, Satterfield-Doerr M, Parikh AR, Brodbelt JS. Anal. Chem. 1998;70:1788. doi: 10.1021/ac971228g. [DOI] [PubMed] [Google Scholar]
- 170.Walsh JM, Flegel R, Crouch DJ, Cangianelli L, Baudys J. J. Anal. Toxicol. 2003;27:429. doi: 10.1093/jat/27.7.429. [DOI] [PubMed] [Google Scholar]
- 171.Crouch DJ. Forensic Sci. Int. 2005;150:165. doi: 10.1016/j.forsciint.2005.02.028. [DOI] [PubMed] [Google Scholar]
- 172.Crouch DJ, Walsh JM, Flegel R, Cangianelli L, Baudys J, Atkins R. J. Anal. Toxicol. 2005;29:244. doi: 10.1093/jat/29.4.244. [DOI] [PubMed] [Google Scholar]
- 173.Quintela O, Crouch DJ, Andrenyak DM. J. Anal. Toxicol. 2006;30:614. doi: 10.1093/jat/30.8.614. [DOI] [PubMed] [Google Scholar]
- 174.Day D, Kuntz DJ, Feldman M, Presley L. J. Anal. Toxicol. 2006;30:645. doi: 10.1093/jat/30.9.645. [DOI] [PubMed] [Google Scholar]
- 175.Moore C, Coulter C, Rana S, Vincent M, Soares J. J. Anal. Toxicol. 2006;30:409. doi: 10.1093/jat/30.7.409. [DOI] [PubMed] [Google Scholar]
- 176.Moore C, Ross W, Coulter C, Adams L, Rana S, Vincent M, Soares J. J. Anal. Toxicol. 2006;30:413. doi: 10.1093/jat/30.7.413. [DOI] [PubMed] [Google Scholar]
- 177.Niedbala RS, Kardos KW, Fritch DF, Kunsman KP, Blum KA, Newland GA, Waga J, Kurtz L, Bronsgeest M, Cone EJ. J. Anal. Toxicol. 2005;29:607. doi: 10.1093/jat/29.7.607. [DOI] [PubMed] [Google Scholar]
- 178.Kidwell DA, Holland JC, Athanaselis S. J. Chromatogr. 1998;713:111. doi: 10.1016/s0378-4347(97)00572-0. [DOI] [PubMed] [Google Scholar]
- 179.Balabanova S, Schneider E. Beitr. Gerichtl. Med. 1989;48:45. [PubMed] [Google Scholar]
- 180.Samyn N, van Haeren C. Int. J. Legal Med. 2000;113:150. doi: 10.1007/s004140050287. [DOI] [PubMed] [Google Scholar]
- 181.Kintz P, Brenniesen R, Bundeli P, Mangin P. Clin. Chem. 1997;43:736. [PubMed] [Google Scholar]
- 182.Ehorn C, Fretthold D, Maharaj M. Annual Meeting of the International Association of Forensic Toxicologists (TIAFT); Tampa, U.S.A.. October 31 – November 4, 1994.p. 11. [Google Scholar]
- 183.Cairns T, Kippenberger DJ, Scholtz H, Baumgartner WA. In: de Zeeuw RA, Al Hosani I, Al Munthiri S, Maqbool A, editors. Hair Analysis in Forensic Toxicology: Proceedings of the 1995 International Conference and Workshop; Abu Dhabi. 1995; Organizing Committee; p. 185. [Google Scholar]
- 184.Cirimele V. In: Drug Testing in Hair. Kintz P, editor. CRC Press; Boca Raton: 1996. p. 181. [Google Scholar]
- 185.Kintz P, Cirimele V, Mangin P. J. Forensic Sci. 1995;40:619. [PubMed] [Google Scholar]
- 186.Moore C, Guzaldo F, Donahue T. J. Anal. Toxicol. 2001;25:555. doi: 10.1093/jat/25.7.555. [DOI] [PubMed] [Google Scholar]
- 187.Moore C, Rana S, Coulter C, Feyerherm F, Prest H. J. Anal. Toxicol. 2006;30:171. doi: 10.1093/jat/30.3.171. [DOI] [PubMed] [Google Scholar]
- 188.Cirimele V, Sachs H, Kintz P, Mangin P. J. Anal. Toxicol. 1996;20:13. doi: 10.1093/jat/20.1.13. [DOI] [PubMed] [Google Scholar]
- 189.Huestis MA, Gustafson RA, Moolchan ET, Barnes A, Bourland JA, Sweeney SA, Hayes EF, Carpenter PM, Smith ML. Forensic Sci. Int. 2007;169:129. doi: 10.1016/j.forsciint.2006.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]