Abstract
Rationale
A single 90-mg dose of the cannabinoid CB1 receptor antagonist rimonabant attenuates effects of smoked cannabis in humans.
Objectives
The objective of this study is to evaluate whether repeated daily 40-mg doses of rimonabant can attenuate effects of smoked cannabis to the same extent as a single higher (90 mg) dose.
Materials and methods
Forty-two male volunteers received one of three oral drug regimens in a randomized, double blind, parallel group design: (1) 40 mg rimonabant daily for 15 days, (2) placebo for 14 days, then 90 mg rimonabant on day 15, or (3) placebo for 15 days. All participants smoked an active or placebo cannabis cigarette 2 h after medication on days 8 and 15. Subjective effects were measured with visual analog scales and the marijuana-scale of the Addiction Research Center Inventory.
Results
Cannabis-induced tachycardia was significantly lower for the 40-mg group on day 8 and for the 40 and 90 mg rimonabant groups on day 15 as compared to placebo. The 40-mg dose significantly decreased peak subjective effects on day 8. Neither the 90-mg nor 40-mg doses significantly decreased peak subjective effects on day 15. Rimonabant treatment did not significantly affect Δ9-tetrahydrocannabinnol pharmacokinetics.
Conclusions
Repeated lower daily rimonabant doses (40 mg) attenuated the acute physiological effects of smoked cannabis to a similar degree as a single 90-mg dose; repeated 40-mg doses attenuated subjective effects after 8 but not 15 days.
Keywords: Rimonabant, Cannabinoids, Receptor, Antagonist, Human, Subjective effects, Heart rate
Introduction
Δ9-Tetrahydrocannabinnol (THC) is the major psychoactive component of cannabis and is responsible for producing its characteristic physiological and psychological effects (Huestis et al. 1992b; Mechoulam and Gaoni 1965). THC effects are mediated through the cannabinoid CB1 receptor, a G-protein coupled receptor (Matsuda et al. 1990; Westlake et al. 1994). The functional effects of cannabinoid receptor activation are numerous, including analgesia, decreased locomotor activity, hypothermia, appetite stimulation, and cognitive impairment (Chaperon and Thiebot 1999; Grotenhermen 2004; Howlett 1995; Walker and Huang 2002).
Rimonabant is a selective, potent, and orally active cannabinoid CB1 receptor antagonist that exhibits high affinity for the CB1 receptor (Ki=2 nM), located in various tissues but primarily found in the central nervous system (Matsuda et al. 1990; Westlake et al. 1994), and very low affinity for the CB2 receptor (Ki>1,000 nM; Rinaldi-Carmona et al. 1994), primarily located in the peripheral immune system (Derocq et al. 1995; Galiegue et al. 1995). Rimonabant blocks the effects of THC in vitro (Rao et al. 2004; Tomasini et al. 2002), in animals (Compton et al. 1996; Tseng and Craft 2004), and in humans (Huestis et al. 2001). Furthermore, rimonabant has been shown in animals to modulate cannabinoid signaling in the reward circuitry in the brain (Le Foll and Goldberg 2005), thereby reducing opioid self-administration (Navarro et al. 2004), relapse to methamphetamine seeking (Anggadiredja et al. 2004) or cocaine seeking (De Vries et al. 2001), and alcohol self-administration (Arnone et al. 1997; de Fonseca et al. 2004). Rimonabant also has shown promising clinical results for weight loss and metabolic disorders in obese individuals (Despres et al. 2005; Pi-Sunyer et al. 2006; Van Gaal et al. 2005) and for smoking cessation (Cleland et al. 2004).
We previously demonstrated in adult male cannabis users that a single 90-mg oral dose of rimonabant 2 h before smoking a cannabis cigarette (2.64% THC) produced significant 38−43% reductions in subjective effects visual analog scale (VAS) ratings of “How high do you feel now,” “How stoned on marijuana are you now,” and “How strong is the drug effect you feel now” (Huestis et al. 2001). A trend toward decreased cannabis-induced tachycardia was observed. Orthogonal polynomial trend tests demonstrated significant blockade of the tachycardia and subjective responses produced by smoked cannabis across the dose range of 1 to 90 mg rimonabant. Rimonabant alone produced no significant physiological or psychological effects and did not alter THC pharmacokinetics.
The long half-life of rimonabant, around 6−9 days in healthy young adults (Turpault et al. 2006), suggests that repeated lower doses might produce the same blockade of THC effects as a single higher dose. In addition, potential clinical uses for rimonabant (e.g., smoking cessation and alcohol or other drug dependence) are expected to require repeated drug dosing. For these reasons, we investigated the effects of multiple oral 40-mg doses of rimonabant on THC pharmacodynamics and pharmacokinetics in humans and compared these effects with those of a single oral 90-mg rimonabant dose.
Materials and methods
Subjects
Forty-two adult male subjects with a history of smoked cannabis use and no substance use disorder (except cannabis, caffeine, or nicotine) were randomized to receive study medication. Women were excluded because of the absence of adequate safety data regarding rimonabant and pregnancy. This created an unfavorable risk/benefit ratio for female subjects in this phase I study which conferred no direct benefit to subjects. Six subjects did not complete dosing: two withdrew consent, one was discharged for administrative reasons, and three had nonserious adverse events (see “Pharmacodynamics”). The remaining 36 subjects were included in analyses.
Participants were in good physical and psychological health, as demonstrated by medical history, physical examination, clinical laboratory tests, electrocardiogram (ECG), electroencephalogram, and standard psychological tests. Subjects resided on the closed clinical research unit of the National Institute on Drug Abuse (NIDA) Intramural Research Program for the duration of the study and returned for follow-up safety evaluations 1 and 3 weeks after receiving their last rimonabant dose. All subjects provided written informed consent before their inclusion in the study and were paid for their participation. The study was approved by the NIDA Institutional Review Board and conducted in accordance with the ethical standards of the Declaration of Helsinki.
Study design and procedures
A single site, randomized, double-blind, placebo-controlled, double-dummy, parallel group design was used. Participants were randomly assigned to one of three treatment groups: (1) 40-mg oral doses of rimonabant once daily for 15 days (n=12), (2) oral doses of placebo rimonabant once daily for 14 days, followed by a single 90-mg oral dose of rimonabant on day 15 (n=12), or (3) oral doses of placebo rimonabant once daily for 15 days (n=12). The 40-mg daily dose is twice the highest daily dose (20 mg) used in phase III clinical trials for obesity and cigarette smoking (Cleland et al. 2004; Despres et al. 2005; Pi-Sunyer et al. 2006; Van Gaal et al. 2005) and was chosen to maximize the chance of observing significant blockade. The 90-mg single dose was chosen to replicate the highest single dose used in our prior study (Huestis et al. 2001). The dosing intervals of 8 and 15 days were chosen as a compromise between achieving steady-state concentrations of rimonabant (median time to achieve steady-state plasma trough concentrations in healthy, non-obese young adults is around 13 days [Turpault et al. 2006]) and the practicality of housing subjects in a closed residential setting. To avoid possible elicitation of cannabis withdrawal by rimonabant, medication dosing did not begin until urine cannabinoid concentration was less than 20 ng/ml.
During experimental sessions on days 8 and 15, each subject smoked one placebo or active cannabis cigarette from 10:50−11:00 am while seated in a small study room, accompanied only by a study nurse. Smoking occurred 2 h after oral dosing (9 am), the expected time of peak rimonabant plasma concentrations. Ten subjects within each treatment group received active cannabis on both days. To maintain double-blind conditions and decrease subject and investigator expectation bias, one subject in each group received placebo cannabis on day 8 and active cannabis on day 15; another subject in each group received active cannabis on day 8 and placebo on day 15. Cannabis administration consisted of eight puffs from the cigarette at 60-s intervals with ad libitum puff duration and retention. Subjects were not required to smoke the entire cigarette so as not to force them to inhale more cannabis smoke than they were used to (a requirement of the Institutional Review Board). Measurement of THC plasma concentrations confirmed the degree of THC exposure. Physiological and subjective measures were assessed repeatedly for 90 min after cannabis smoking.
Medications
Machine-rolled cannabis and placebo cigarettes were provided by the NIDA Chemistry and Physiological Systems Research Branch. Active cannabis cigarettes weighed an average of 764 mg, contained 2.78% THC by weight, as determined by gas chromatography/mass spectrometry, and were estimated to contain approximately 20 mg of THC. Placebo cigarettes were prepared by solvent extraction of cannabinoids from active cigarettes, yielding cigarettes identical in appearance and smell. Rimonabant and matching placebo capsules were supplied by Sanofi-Aventis, Malvern, PA.
Assessments
Primary measures of THC pharmacodynamic effects were heart rate and subjective measures of cannabis intoxication. Heart rate was recorded continuously from an ECG chest lead and analyzed as 5-min averages at baseline, 5, 10, 15, 20, 25, 30, 35, 45, 55, 65, 75, and 85 min after cigarette smoking. Subjective measures of intoxication included three 100-mm VAS questions (Folstein and Luria 1973) and the marijuana subscale (M-scale) of the Addiction Research Center Inventory (Chait et al. 1985). Subjects viewed each VAS question separately on a video monitor: “How high do you feel right now?”, “How strong is the drug effect you feel now?”, and “How stoned on marijuana are you now?” Subjects responded by moving a cursor along a 100-mm line anchored on the left end by “not at all” and on the right end by “extremely.” A composite VAS score was calculated as the mean VAS score of the three individual questions; thus, the maximum possible score was 100. The M-scale consists of 12 true or false questions corresponding to symptoms of cannabis intoxication; the maximum possible score was 12. VAS and M-scale responses were collected 1 h before oral dosing and 1 h before and 5, 10, 15, 20, 25, 55, and 85 min after cigarette smoking.
The pharmacokinetics of THC and rimonabant were assessed to document the degree of THC exposure, evaluate possible pharmacokinetic interactions between the two drugs, and pharmacodynamic–pharmacokinetic relationships (data to be presented elsewhere). Venous blood samples were collected 10 min before and 60, 90, 120, 122, 125, 130, 135, 140, 155, 175, 195, 240, 480, 720, and 1,440 min after rimonabant dosing (−130, −60, −30, 0, 2, 5, 10, 15, 20, 35, 55, 75, 120, 360, 600, and 1,320 min relative to cannabis administration) on days 8 and 15. Heparinized plasma was collected and stored at −20°C before analysis. THC concentrations were quantified in plasma samples using negative chemical ionization gas chromatography/mass spectrometry with a 0.5 μg/l limit of quantification (Huang et al. 2001). Rimonabant plasma concentrations were measured using a liquid chromatography-tandem mass spectrometry method with a 1.0 μg/l limit of quantification (Sanofi-Aventis).
Data analysis
Pharmacodynamics
Pharmacodynamic data were expressed as: (1) peak change from baseline and (2) area under the curve (AUC) for heart rate and (3) peak effect and (4) AUC for subjective measures. Peak physiological and subjective effects have been shown to occur within the first hour after cannabis smoking; therefore, peak and AUC were determined for this 1-h period. Actual times were used to calculate the AUC for each subject and time point, yielding weighted average values (AUC0−60) for each subject. The times of peak heart rate change and peak effect also were determined. For purposes of analysis on day 8, the placebo and 90-mg groups were combined (subjects in both groups received placebo through day 14). t-Tests (for day 8 data) and one-way (treatment group) analyses of variance (ANOVAs; for day 15 data) were used to evaluate the effects of rimonabant treatment group (placebo, 40 mg, 90 mg) on each pharmacodynamic measure. Tukey “honest significant difference” post hoc tests were used for pair-wise comparisons of the three treatment groups on day 15. A two-tailed p value of ≤0.05 was considered significant. Data from individuals who smoked placebo THC cigarettes were not included in the analysis.
Percent blockade of the peak cannabis effect at each rimonabant dose was calculated as:
where PΔ9 and SRΔ9 are group means estimated for the placebo rimonabant/active cannabis group and the active rimonabant/active cannabis group, respectively. Feiller's theorem was used to calculate 95% confidence intervals.
Pharmacokinetics
THC, 11-nor-9-carboxy-Δ9-tetrahydrocannabinol (THCCOOH, the primary inactive metabolite of THC), and rimonabant maximum concentrations (Cmax) were obtained from concentration time profiles. To compare the pharmacokinetics of THC and THCCOOH across rimonabant treatment groups, the area under the concentration-time curve (AUC) for THC and THCCOOH was calculated from the time of cannabis dosing until 1.25 h after dosing (AUC0−1.25). To compare the pharmacokinetics of rimonabant across treatment groups, the AUC for rimonabant was calculated as the area from the time of rimonabant dosing until 24 h after the dose (AUC0−24) and for the 1.25-h period after cannabis smoking (AUC2−3.25).
For comparison to pharmacodynamic outcomes, AUCs for the 75-min time period after cannabis smoking (AUC0−1.25 for cannabis, AUC2−3.25 for rimonabant) were utilized. The linear trapezoid method was used in the calculation of all AUC's. Pharmacokinetic variables were analyzed similarly to pharmacodynamic variables, i.e., by t-test and ANOVA. Elimination rate constants and terminal elimination half-lives were not estimated for either drug, due to the short sampling time relative to the drugs’ long terminal elimination phases.
Results
Subject characteristics
Thirty-six of the 42 enrolled subjects completed the study (12 whites, 24 African-American). All subjects tested positive for urine cannabinoids at study entry. Their mean (SD) age was 28.9 (6.3) years, height 174.5 (13.5) cm, weight 76.4 (13.5) kg, and body mass index (BMI) 25.5 (6.6) kg/m2. They had used cannabis an average of 20.3 (9.6) days in the 30 days before screening for the study. There were no significant group differences in age, weight, height, BMI, cannabis use in the 30 days before screening or race among the three treatment groups (Table 1).
Table 1.
Demographic characteristics of 36 adult male cannabis smokers according to treatment group
| Rimonabant dose group |
||||
|---|---|---|---|---|
| 40 mg |
90 mg |
Placebo |
||
| N | 12 | 12 | 12 | |
| Age (years) | Mean | 28.6 | 30.6 | 27.6 |
| SD | 6.7 | 6.9 | 5.4 | |
| Weight (kg) | Mean | 80.2 | 73.7 | 75.3 |
| SD | 17.0 | 12.7 | 10.3 | |
| Height (cm) | Mean | 175.4 | 169.5 | 178.8 |
| SD | 8.7 | 20.6 | 5.8 | |
| BMI (kg/m2) | Mean | 25.8 | 27.0 | 23.5 |
| SD | 3.2 | 10.7 | 2.4 | |
| Cannabis use in 30 days before screening (days) | Mean | 20.9 | 23.5 | 16.5 |
| SD | 11.1 | 9.4 | 7.6 | |
| Lifetime cannabis use (years) | Mean | 10.8 | 12.3 | 8.5 |
| SD | 9.0 | 7.4 | 5.4 | |
| Race | White | 3 | 3 | 6 |
| African-American | 9 | 9 | 6 | |
There were no significant group differences in age, weight, height, BMI, cannabis use in the 30 days before screening, lifetime cannabis use, or race.
Pharmacodynamics
Heart rate
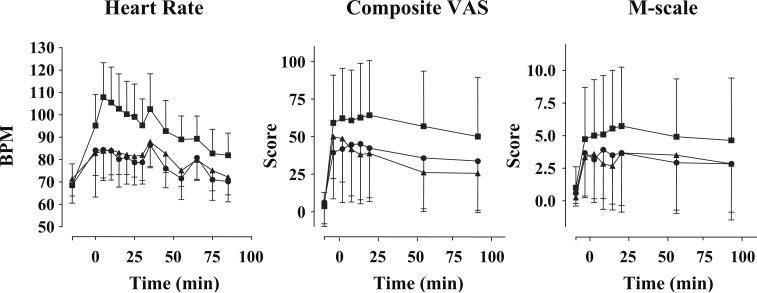
The 2.78% THC cigarette produced the expected effect of increased heart rate (placebo rimonabant group; Table 2, Fig. 1). Rimonabant significantly reduced the cannabis-induced increase in heart rate on day 8 at 40 mg (Table 2; t=4.7, p=0.0001), producing 75.7% blockade. Both the 40- and 90-mg (F=14.6, p=0.0001) rimonabant groups differed significantly from the placebo rimonabant group on day 15 (p=0.0001 for both comparisons by Tukey test), producing 65.6 and 64.3% blockade, respectively (Table 3). Maximum changes from baseline heart rate were comparable between the 40-mg group on days 8 and 15 and the 90-mg group on day 15. There were no significant differences in mean heart rate increases, time of maximum heart rate changes, or AUC0−55 min between active rimonabant groups.
Table 2.
Effect of rimonabant or placebo on heart rate and subjective responses to a smoked cannabis cigarette (2.78% THC) in 34 adult male cannabis users
| Day 8 |
Day 15 |
|||||
|---|---|---|---|---|---|---|
| Placeboa (daily) | 40 mgb (daily) | Placebob (daily) | 90 mgb (day 15 only) | 40 mgb (daily) | ||
| Heart rate increase (bpm) | Mean | 47.8c | 12.2 | 38.4 | 13.7 | 13.2 |
| Median | 49.4 | 10.6 | 37.4 | 11.8 | 14.4 | |
| Range | 15.4−95.2 | 2−19.8 | 18−74.2 | −1.6−33.2 | 0.4−31.2 | |
| 95% CI | 37.7−57.9 | 9.1−15.3 | 29.1−47.8 | 6.8−20.6 | 7.9−18.6 | |
| Tmax (min) | Mean change | 16.3c | 22.5 | 16.2 | 26.4 | 22.4 |
| Median | 9.0 | 14.0 | 7.3 | 34.0 | 34.0 | |
| Range | 2−54 | 3−65 | 4−35 | 1−67 | 1−35 | |
| 95% CI | 10.6−21.7 | 11.2−33.7 | 7.6−24.8 | 14.5−38.2 | 13.2−31.6 | |
| AUC0−55 min | Mean Change | 31.6c | 2.8 | 25.3 | 4.4 | 4.1 |
| Median | 29.4 | 2.5 | 22.5 | 3.4 | 2.5 | |
| Range | 6.3−74.2 | −2.6−10.9 | 7.5−52.3 | −7.5−16.7 | −4.1−13.5 | |
| 95% CI | 23.6−39.7 | 0.6−5.1 | 17.7−32.9 | −.0.4−9.3 | 0.5−7.7 | |
| VAS (mm) composite | Mean Peak | 80.0 | 64.6 | 69.8 | 49.3 | 59.8 |
| Median | 79.0 | 64.7 | 76.7 | 76.7 | 65.3 | |
| Range | 48−100 | 31.3−98 | 4.7−100 | 3.3−84.7 | 4.7−96.7 | |
| 95% CI | 72.9−87.0 | 54.1−75.1 | 51.1−88.4 | 27.7−70.9 | 43.9−75.8 | |
| Tmax (min) | Mean | 18.1 | 25.3 | 19.7 | 17.5 | 14.0 |
| Median | 13.5 | 23.7 | 24 | 17 | 12 | |
| Range | 7−60 | 7−59 | 6−30.2 | 6−28 | 7−23 | |
| 95% CI | 12.9−23.2 | 17.4−33.1 | 13.5−25.9 | 13.4−21.7 | 10.2−17.9 | |
| AUC0−55 min | Mean | 66.3 | 53.2 | 60.3 | 40.7 | 38.1 |
| Median | 66.5 | 48.2 | 53.2 | 61.4 | 41.8 | |
| Range | 28−99.9 | 13.7−96.5 | 2.9−97.8 | 0.6−79.2 | 0.6−88.4 | |
| 95% CI | 56.2−76.3 | 40.5−66.0 | 41.0−79.6 | 20.1−61.3 | 22.6−53.5 | |
| M-scale | Mean Peak | 8.1 | 5.5 | 6.5 | 5.0 | 5.0 |
| Median | 8.5 | 6 | 6 | 5 | 4 | |
| Range | 2−12 | 2−11 | 1−12 | 0−12 | 0−11 | |
| 95% CI | 6.8−9.4 | 4.0−7.1 | 4.2−8.9 | 2.7−7.3 | 2.6−7.4 | |
| Tmax (min) | Mean | 23.8 | 19.9 | 19.3 | 13.9 | 14.5 |
| Median | 22.0 | 10 | 22 | 8 | 12 | |
| Range | 8−65 | 8−62 | 7−31 | 7−28 | 7−28 | |
| 95% CI | 16.5−31.2 | 7.6−32.3 | 14.1−24.5 | 9.4−18.4 | 9.8−19.2 | |
| AUC0−55 min | Mean | 6.1 | 3.6 | 5.5 | 3.7 | 3.7 |
| Median | 6.5 | 4.3 | 3.9 | 3.0 | 1.7 | |
| Range | 1.1−10.7 | 0.3−7.6 | 0.2−11.9 | 0−11.8 | 0−10.2 | |
| 95% CI | 4.8−7.5 | 2.3−5.0 | 3.1−7.9 | 1.5−5.9 | 1.3−6.1 | |
Heart rate Change from baseline (before oral rimonabant dosing); VAS composite mean of scores on three 100-mm visual analog scales for “How high do you feel now?”, “How strong is the drug effect you feel now?” and “How stoned on marijuana are you now?” Maximum possible score=100; M-scale marijuana subscale of Addiction Research Center Inventory. Maximum possible score=12; Tmax time during session that maximum value of variable was reached
n=22
n=11
n=23
Fig. 1.
Time course of rimonabant blockade on day 15 of smoked cannabis effects. Composite VAS mean score of three 100-mm VAS: “High,” “Stoned,” and strength of drug effect (maximum possible score=100). M-scale marijuana subscale of the Addiction Research Center Inventory (maximum possible score=12). N=11 for each dose group. Cannabis cigarette (2.78% THC) was smoked at time 0, 2 h after oral rimonabant dosing. Vertical bars indicate standard deviations. Square placebo rimonabant daily, triangle 40 mg rimonabant daily, circle 90 mg rimonabant on day 15 only (placebo on days 1−14)
Table 3.
Percent blockade (95% confidence interval) of peak cannabis effect by oral rimonabant in 22 adult male subjects who smoked an active cannabis (2.78% THC) cigarette on day 8 or 15 (n = 11 for each dose group)
| Pharmacodynamic measure | Day 15 |
Day 8 |
|
|---|---|---|---|
| 40 mg daily for 15 days | 90 mg (day 15 only) | 40 mg daily for 8 days | |
| ΔHeart rate | 65.6 (36.3, 100) |
64.3 (35.1, 98.9) |
75.7 (35.7, 124) |
| VAS composite | 14.3 (−26.3, 57.3) |
29.4 (−10.6, 74.4) |
19.2 (3.1, 35.7) |
| M-scale | 23.6 (−30.8, 85.8) |
23.6 (−30.8, 85.8) |
30.3 (2.2, 60.0) |
ΔHeart Rate Change from baseline (before rimonabant dosing); VAS composite mean of scores on three 100-mm visual analog scales for "How high do you feel now?", "How strong is the drug effect you feel now?" and "How stoned on marijuana are you now?"; M-scale marijuana subscale of Addiction Research Center Inventory
Subjective effects
The 2.78% THC cigarette produced the expected subjective experience of cannabis intoxication (placebo rimonabant group; Table 2, Fig. 1). Mean peak VAS composite scores and M-scale scores occurred from 14 to 25 min after the end of smoking, but exhibited large variability within each treatment group (Table 2). Rimonabant significantly reduced composite VAS ratings on day 8 (t=2.4, p=0.02, Table 2), producing 19.2% blockade (Table 3). Rimonabant also significantly reduced peak M-scale scores (t=2.4, p=0.02) on day 8 (Table 2), producing 30.3% blockade (Table 3). On day 15, there was no significant blockade of cannabis’ subjective effects (F=1.13, p=0.34 for VAS composite scores; F=0.55, p=0.58 for M-scale scores), although mean peak scores and AUC tended to be lower for the rimonabant groups than the placebo group. A contributing factor to the differences between findings on days 8 and 15 could be the smaller sample size on day 15 for the placebo group (n=11 rather than 22). There were no significant differences between peak subjective scores, time of peak scores, or AUC0−55 between the 40-mg group on days 8 and 15 and the 40 and 90-mg groups on day 15. All primary subjective pharmacodynamic variables showed comparable reductions in cannabis’ effects on day 15. No subject receiving rimonabant reported qualitatively different subjective effects from those experienced in the community or reported by subjects receiving placebo.
Rimonabant was well tolerated by subjects. There were no serious adverse events and no differences in type or frequency of adverse events among the three study groups. Three subjects were discontinued from the study because of adverse events: one because of transient elevation in serum liver transaminase concentrations (placebo rimonabant/active cannabis group); one because of nonspecific ECG changes (with no evidence of underlying heart disease; placebo rimonabant/active cannabis group); and one because of minor trauma unrelated to the study (90-mg rimonabant/active cannabis group, before receiving rimonabant).
Pharmacokinetics
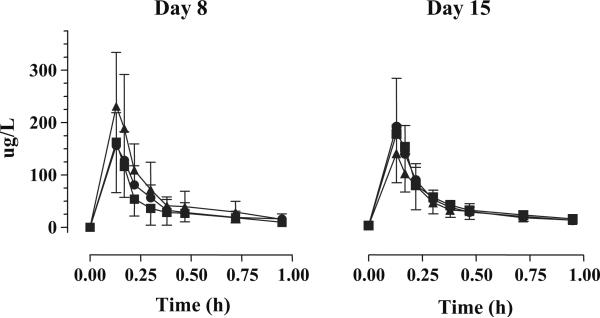
Mean THC Cmax ranged from 129.4 to 204.8 μg/l and occurred in the first blood specimen collected (Table 4, Fig. 2) in all groups on both days. THC mean Cmax were not significantly different across treatment groups for those individuals who smoked cannabis on day 8 (t=1.2, p=0.23) and on day 15 (F=1.17, p=0.32). There also were no differences between the time of peak THC concentrations on day 8 (t=1.1, p=0.29) or day 15 (F=0.52, p=0.60), and the AUC0−1.25 (day 8, t=1.8, p=0.09; day 15, F=0.67, p=0.52). THCCOOH Cmax occurred later (19 to 24 min), were lower than parent compound concentrations, as expected, and ranged from 23.2 to 37.1 μg/l. There were no significant differences in THCCOOH Cmax (t=0.58, p=0.57 on day 8; F=2.23, p=0.13 on day 15), time of peak (t=0.57, p=0.58 on day 8; F=0.83, p=0.45 on day 15), or AUC0−1.25 (t=0.73, p=0.47 on day 8; F=1.75, p=0.19 on day 15) across treatment groups (Table 5). Group mean THC plasma profiles are shown in Fig. 2.
Table 4.
Pharmacokinetic parameters for Δ9-tetrahydrocarmabinol (THC) in 36 adult males after smoking one cannabis cigarette (2.78% THC) on day 8 and on day 15
| Parameter | Day 8 |
Day 15 |
|||
|---|---|---|---|---|---|
| 40 mga | Placebob | 40 mga | 90 mga | Placeboc | |
| Cmax (μg/l) | |||||
| Mean | 162.5 | 204.8 | 166.0 | 179.8 | 129.4 |
| Median | 183.9 | 191.2 | 160.9 | 155.3 | 119.7 |
| Range | 11.3−372.9 | 58.6−414.1 | 23.8−306.5 | 89.0−360.0 | 56.9−222.2 |
| 95% CI | 105.7−219.3 | 166.7−242.8 | 113.9−218.2 | 129.4−230.3 | 97.6−161.1 |
| Tmax (min) | |||||
| Mean | 8.0 | 7.6 | 8.0 | 7.5 | 7.8 |
| Median | 7.8 | 7.8 | 7.8 | 7.8 | 7.8 |
| Range | 7.8−10.2 | 3.0−10.2 | 7.8−10.2 | 1.8−10.2 | 7.8 |
| 95% Cl | 7.6−8.5 | 7.1−8.1 | 7.6−8.5 | 6.3−8.6 | NA |
| AUC0−1.25 (μg·h/l) | |||||
| Mean | 44.5 | 62.6d | 48.3 | 44.5 | 37.7e |
| Median | 44.5 | 55.3 | 46.8 | 47.6 | 32.3 |
| Range | 4.7−99.4 | 19.0−108.4 | 8.4−94.9 | 21.9−77.9 | 14.5−64.5 |
| 95% CI | 30.4−58.7 | 50.1 −75.2 | 32.5−64.2 | 35.6−54.1 | 26.7−48.7 |
n=11
n=22
n=10
n=21
n=9
Fig. 2.
Δ9-Tetrahydrocannabinol (THC) plasma pharmacokinetic profiles for 75 min after smoking of a 2.78% THC cannabis cigarette by 33 adult men. Each symbol is the group mean of plasma THC concentrations (n=11 for each dose group). Triangle placebo rimonabant daily, square 40 mg rimonabant daily for 15 days, circle 90 mg rimonabant day 15 only (placebo on days 1−14). Vertical bars indicate standard deviation
Table 5.
Pharmacokinetic parameters for 11-nor-9-carboxy-Δ9-tetrahydrocannabinol in 36 adult males after smoking one cannabis cigarette (2.78% THC) on day 8 and on day 15
| Parameter | Day 8 |
Day 15 |
|||
|---|---|---|---|---|---|
| 40 mga | Placebob | 40 mga | 90 mga | Placeboc | |
| Cmax (μg/l) | |||||
| Mean | 28.2 | 30.9 | 33.4 | 37.1 | 23.2 |
| Median | 25.2 | 30.4 | 30.0 | 32.7 | 22.2 |
| Range | 4.7−50.4 | 12.4−51.8 | 6.1−71.0 | 20.9−66.1 | 10.6−44.9 |
| 95% CI | 20.7−35.8 | 25.5−36.3 | 21.8−45.1 | 27.3−46.9 | 16.8−29.5 |
| Tmax (min) | |||||
| Mean | 22.0 | 21.2 | 24.3 | 19.7 | 20.3 |
| Median | 22.8 | 19.0 | 22.8 | 18.0 | 18.0 |
| Range | 18.0−24.0 | 13.2−28.2 | 18.0−58.2 | 12.0−28.2 | 18.0−22.8 |
| 95% CI | 20.8−23.2 | 19.1−23.3 | 17.4−31.3 | 17.2 −22.2 | 18.5−21.7 |
| AUC0−1.25 (μg·h/l) | |||||
| Mean | 27.2 | 31.0 | 31.6 | 34.1 | 22.0d |
| Median | 24.4 | 27.6 | 27.3 | 29.9 | 19.5 |
| Range | 5.1−48.9 | 12.5−55.5 | 5.6−71.0 | 21.1−60.0 | 10.9−42.1 |
| 95% CI | 20.2−34.1 | 25.3−36.7 | 20.6−42.6 | 25.5−42.7 | 15.6−28.4 |
n=11
n=17
n=10
n=9
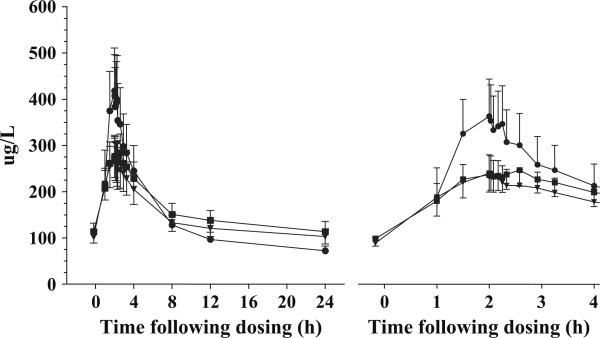
Mean rimonabant Cmax were 307.8, 334.6, and 478.6 μg/l for the 40-mg group on days 8 and 15 and the 90 mg group on day 15, respectively. Mean peak concentrations occurred 1.77, 2.35, and 3.05 h after oral dosing, respectively. Although there was more variability in rimonabant Cmax concentrations after the single oral 90-mg dose (up to 10-fold) than after 15 daily 40-mg doses (up to 3.8-fold), there were no significant differences between the two active rimonabant groups (F=1.86, p=0.19; Table 6, Fig. 3) or between the 40-mg group on days 8 and 15 (F=0.18, p=0.67). Neither were there significant differences in the AUC2−3.25 or AUC0−24 between the 40 and 90-mg rimonabant groups on day 15 (F=0.60, p=0.45; F=0.25, p=0.62, respectively).
Table 6.
Pharmacokinetic parameters for rimonabant in adult men receiving 40 mg daily for 15 days (n=12) or 90 mg once (n=12)
| Parameter | Day 8 |
Day 15 |
|
|---|---|---|---|
| 40 mg | 40 mg | 90 mg | |
| Cmax (μg/l) | |||
| Mean | 307.8 | 334.6 | 478.6 |
| Median | 240.0 | 294.5 | 431.5 |
| Range | 157.0−576.0 | 185.0−705.0 | 90.2−958.0 |
| 95% CI | 221.6−393.9 | 246.3−422.9 | 291.4−665.8 |
| Tmax (h) | |||
| Mean | 1.77 | 2.35 | 3.05 |
| Median | 1.75 | 2.39 | 2.13 |
| Range | 0.82−3.25 | 1.00−4.00 | 1.00−8.00 |
| 95% Cl | 1.38−2.17 | 1.78−2.92 | 1.67−4.43 |
| AUC0−24 (μg·h/l) | |||
| Mean | 3341.4 | 3681.7a | 3260.1a |
| Median | 2860.6 | 3201.4 | 2722.8 |
| Range | 1145.3−6536.6 | 1394.4−8362.8 | 1151.1−7582.6 |
| 95% CI | 2387.1−4295.6 | 2488.7−4874.6 | 2123.0−4397.3 |
| AUC2−3.25 (μg·h/l) | |||
| Mean | 307.2 | 335.6 | 416.3 |
| Median | 236.9 | 285.3 | 403.8 |
| Range | 104.7−598.9 | 190.2−692.0 | 72.4−1113.4 |
| 95% CI | 210.7−403.7 | 246.6−425.0 | 233.3−599.4 |
n=11
Fig. 3.
Rimonabant plasma pharmacokinetic profiles for 24 h (left panel) and 3 h (right panel) after oral rimonabant dosing. Each symbol is the group mean of plasma rimonabant concentrations (n=11 for each dose group). A cannabis (2.78% THC) cigarette was smoked 2 h after rimonabant dosing. Inverted triangle 40 mg daily rimonabant, day 8, square 40 mg daily rimonabant, day 15, circle 90 mg rimonabant day 15 only (placebo on days 1−14). Vertical bars indicate standard deviations
Discussion
Rimonabant attenuated the physiological and psychological effects of smoked cannabis in humans, without altering THC and THCCOOH pharmacokinetics. Consistent with our hypothesis, a rimonabant regimen of 40 mg daily for 8 days reduced physiological and psychological responses to cannabis to a similar degree as a single higher dose of 90 mg in our previous human study (Huestis et al. 2001). The similar degree of blockade produced by the two dosing regimens (Table 3) may reflect the production of similar rimonabant Cmax, AUC2−3.25 and AUC0−24 as found in the present study (Table 6). The single 90-mg dose in the present study significantly reduced cannabis-induced tachycardia by about two-thirds, consistent with the 59% blockade produced by this single dose in our previous human study (Huestis et al. 2001).
A rimonabant regimen of 40 mg daily for 15 days or a single 90-mg dose did not significantly block subjective measures, although the percentage decreases (14 and 29%, respectively) were comparable to those seen after 40 mg daily for 8 days (19%). The inconsistency vs. the 40-mg 8-day dosing regimen may be due to the between-subject study design and large intersubject variability of these subjective measures, which reduced the power to detect between-group differences in subjective measures. The number of placebo subjects available on day 8 for comparison with the rimonabant group (40 mg daily) was twice as large as the number available on day 15 because it combined two identically treated groups, placebo rimonabant and 90-mg rimonabant (which received placebo on days 1−14). Were the placebo group on day 15 as large as the one on day 8, our power to detect group differences would have been about 25% greater (even assuming no decrease in group variability).
Conversely, the significant effects observed on day 8 were not an artifact of the larger placebo sample size. Separate day 8 analyses using only the 11 subjects who received placebo on days 1−15 (i.e., omitting the 11 subjects who received placebo on days 1−14 and rimonabant 90 mg on day 15) gave similar results to the analyses using the combined day 8 placebo groups (22 subjects). The rimonabant 40 mg daily group, compared to this smaller placebo group, still had significantly reduced cannabis-induced increased heart rate (F=23.95, p<0.0001), composite VAS score (F= 9.19, p=0.005), and M-scale score (F=5.55, p=0.025).
It is also theoretically possible that the lesser degree of blockade by the 40-mg dose after 15 daily doses as compared to after 8 daily doses was due to adaptation to rimonabant action (i.e., some form of tolerance). In rodent studies, tolerance to some appetite-suppressing and intestinal motility effects of rimonabant occurs within several days of daily dosing (Carai et al. 2004; Gessa et al. 2006), possibly reflecting diminished blockade of the effects of endogenous CB1 receptor agonists. In human studies, daily dosing of 20 mg rimonabant for up to 2 years does not generate tolerance to its weight loss effects (Despres et al. 2005; Pi-Sunyer et al. 2006; Van Gaal et al. 2005).
In our previous study, a single 90-mg oral rimonabant dose produced a significant 38−43% blockade of the same subjective measures (Huestis et al. 2001). Several factors may account for the different effects of a single 90-mg rimonabant dose between the two studies. First, the large intra- and intersubject variability in subjective measures, especially as compared with heart rate (e.g., see Fig. 1), reduced the power to demonstrate statistically significant effects. Second, there may have been differences in the strength of cannabis effects available for blockade due to individual differences in smoking dynamics (Huestis et al. 1992a) and THC bioavailability (Ohlsson et al. 1981, 1982). Third, differences in study design and subject experience, such as length of stay on the research unit before testing or number of prior cannabis cigarettes smoked in the study (none vs. one) may have altered subjects’ responsiveness to cannabis. These factors may also contribute to the differences in day 8 vs. day 15 findings in the present study. Finally, in analyses conducted in the previous trial (Huestis et al. 2001), the effect of placebo cannabis was subtracted from the effect of active cannabis when calculating blockade by rimonabant. This is not expected to be a major contributing factor because subjective responses to placebo cannabis were found to be minimal and short-lived in the previous study, as well as in the current study (data not shown).
The blockade of smoked cannabis’ physiological and psychological effects by rimonabant was not due to altered THC or THCCOOH pharmacokinetics. The absence of change in pharmacokinetics of THCCOOH, the primary inactive metabolite of THC, makes it unlikely that rimonabant shifted THC metabolism to an alternative pathway that might have included active metabolites, e.g., 11-hydroxy-THC. The THC and THCCOOH Cmax Tmax, and AUC0−1.25 were not significantly different in the placebo rimonabant and two active rimonabant groups. These findings are consistent with results from the previous single-dose study in which no pharmacokinetic interaction was observed (Huestis et al. 2001).
The ability of rimonabant, at well-tolerated doses, to attenuate effects of cannabinoids in vivo in humans suggests potential therapeutic applications. Animal studies have implicated endocannabinoids and exogenous THC in several clinically relevant behaviors, including stimulation of food intake (DiMarzo et al. 2001; Fride et al. 2001; Gomez et al. 2002; Hilairet et al. 2003; Jamshidi and Taylor 2001; Kirkham 2003; Ravinet Trillou et al. 2004; Williams and Kirkham 1999) and brain mechanisms related to drug reward and self-administration (Le Foll and Goldberg 2004, 2005). Rimonabant reduces spontaneous food intake and promotes weight loss in animals (Arnone et al. 1997; Ravinet Trillou et al. 2003; Simiand et al. 1998), presumably by blocking the binding of endogenous cannabinoids to the CB1 receptor. Moreover, rimonabant increases expression of adiponectin, a key adipocyte cytokine (Bensaid et al. 2003). Rimonabant blocks nicotine-induced dopamine release in the shell of the nucleus accumbens and decreases nicotine self-administration in rats, without itself substituting for nicotine (Cohen et al. 2002). These studies suggest the potential of rimonabant as a treatment for obesity and tobacco dependence. In recently completed phase III clinical trials, rimonabant was a promising treatment for obesity and related metabolic disorders (Despres et al. 2005; Pi-Sunyer et al. 2006; Van Gaal et al. 2005) and for tobacco smoking cessation (Cleland et al. 2004).
Rimonabant reduces self-administration or relapse to self-administration of alcohol (Arnone et al. 1997; Cippitelliet al. 2005; de Fonseca et al. 2004; Wanget al. 2003), heroin (Navarro et al. 2004), methamphetamine (Anggadiredja et al. 2004), and cocaine (De Vries et al. 2001) in animals, suggesting that it also may have therapeutic potential for a wide range of drug addictions, including cannabis dependence. However, the incomplete blockade of positive subjective cannabis effects achieved after 15 days of 40 mg/day dosing suggests that rimonabant at these doses may not be an effective cannabis-dependence treatment through a direct mechanism of blockade of exogenous cannabis effects, analogous to naltrexone treatment of heroin dependence. It remains possible that rimonabant could be effective treatment acting indirectly via modulation of the endocannabinoid system, its presumed mechanism in reducing self-administration of non-cannabinoid drugs. This would be analogous to the indirect mechanism of naltrexone treatment for alcohol dependence (i.e., modulation of the endogenous opioid system).
One potential limitation to the external validity (generalizability) of this study is the absence of female participants (excluded for safety reasons [see “Subjects,” above]). Rodent and monkey studies suggest that rimonabant produces similar attenuation of CB1 receptor agonist-induced behavioral, analgesic, and hormonal effects in male and female animals (McMahon 2006; Tseng and Craft 2004). The published phase III clinical trials of rimonabant for the treatment of obesity and related metabolic disorders have included at least half women participants and have reported significant rimonabant effects (Despres et al. 2005; Pi-Sunyer et al. 2006; Van Gaal et al. 2005). Therefore, we believe that our findings are likely to apply equally to men and women.
In conclusion, the results of this study indicate that oral rimonabant treatment, with a single 90-mg dose or with a 40-mg daily dose for 8 or 15 days, significantly blocks acute cardiovascular effects and significantly attenuates (after 8 days of dosing) subjective effects of smoked cannabis. Subjective effects were not blocked after 15 days of rimonabant. The antagonism of THC effects is not due to a change in THC or THCCOOH pharmacokinetics, but rather to the antagonist properties of rimonabant at the CB1 receptor. This study suggests that chronic daily dosing with rimonabant can produce a similar degree of CB1 receptor blockade as a single higher dose, at least with regard to cardiovascular effects, and also confirms the ability of rimonabant to act as an in vivo tool for selectively investigating pharmacological actions associated with the cannabinoid CB1 receptor.
Acknowledgements
We thank Dr. Jennifer Schroeder for help with the statistical analysis. This work was supported by the Intramural Research Program of the National Institutes of Health, National Institute on Drug Abuse, and Sanofi-Aventis and conducted under a Cooperative Research and Development Agreement (CRADA) between the National Institutes of Health and Sanofi-Aventis. Drs. Bonnet and Le Fur work for the study sponsor, Sanofi-Aventis. The other authors are National Institute on Drug Abuse (NIDA) scientists and have no conflicts to declare. The investigators and sponsor contributed to study design and data management and analysis. The NIDA investigators collected all data and prepared the manuscript. The sponsor controlled the allocation schedule and reviewed the manuscript.
References
- Anggadiredja K, Nakamichi M, Hiranita T, Tanaka H, Shoyama Y, Watanabe S, Yamamoto T. Endocannabinoid system modulates relapse to methamphetamine seeking: possible mediation by the arachidonic acid cascade. Neuropsychopharmacology. 2004;29:1470–1478. doi: 10.1038/sj.npp.1300454. [DOI] [PubMed] [Google Scholar]
- Arnone M, Maruani J, Chaperon F, Thiebot MH, Poncelet M, Soubrie P, LeFur G. Selective inhibition of sucrose and ethanol intake by SR 141716, an antagonist of central cannabinoid (CB1) receptors. Psychopharmacology. 1997;132:104–106. doi: 10.1007/s002130050326. [DOI] [PubMed] [Google Scholar]
- Bensaid M, Gary-Bobo M, Esclangon A, Maffrand JP, Le Fur G, Oury-Donat F, Soubrie P. The cannabinoid CB1 receptor antagonist SR141716 increases Acrp30 mRNA expression in adipose tissue of obese fa/fa rats and in cultured adipocyte cells. Mol Pharmacol. 2003;63:908–914. doi: 10.1124/mol.63.4.908. [DOI] [PubMed] [Google Scholar]
- Carai MA, Colombo G, Gessa GL. Rapid tolerance to the intestinal prokinetic effect of cannabinoid CB1 receptor antagonist, SR 141716 (rimonabant). Eur J Pharmacol. 2004;494:221–224. doi: 10.1016/j.ejphar.2004.05.005. [DOI] [PubMed] [Google Scholar]
- Chait LD, Fischman MW, Schuster CR. Hangover effects the morning after marijuana smoking. Drug Alcohol Depend. 1985;15:229–238. doi: 10.1016/0376-8716(85)90002-x. [DOI] [PubMed] [Google Scholar]
- Chaperon F, Thiebot MH. Behavioral effects of cannabinoid agents in animals. Crit Rev Neurobiol. 1999;13:243–281. doi: 10.1615/critrevneurobiol.v13.i3.20. [DOI] [PubMed] [Google Scholar]
- Cippitelli A, Bilbao A, Hansson AC, del Arco I, Sommer W, Heilig M, Massi M, Bermudez-Silva FJ, Navarro M, Ciccocioppo R, de Fonseca FR. Cannabinoid CB1 receptor antagonism reduces conditioned reinstatement of ethanol-seeking behavior in rats. Eur J Neurosci. 2005;21:2243–2251. doi: 10.1111/j.1460-9568.2005.04056.x. [DOI] [PubMed] [Google Scholar]
- Cleland JG, Ghosh J, Freemantle N, Kaye GC, Nasir M, Clark AL, Coletta AP. Clinical trials update and cumulative meta-analyses from the American College of Cardiology: WATCH, SCD-HeFT, DINAMIT, CASINO, INSPIRE, STRATUS-US, RIO-Lipids and cardiac resynchronisation therapy in heart failure. Eur J Heart Fail. 2004;6:501–508. doi: 10.1016/j.ejheart.2004.04.014. [DOI] [PubMed] [Google Scholar]
- Cohen C, Perrault G, Voltz C, Steinberg R, Soubrie P. SR141716, a central cannabinoid (CB1) receptor antagonist, blocks the motivational and dopamine-releasing effects of nicotine in rats. Behav Pharmacol. 2002;13:451–463. doi: 10.1097/00008877-200209000-00018. [DOI] [PubMed] [Google Scholar]
- Compton DR, Aceto MD, Lowe J, Martin BR. In vivo characterization of a specific cannabinoid receptor antagonist (SR141716A): inhibition of delta-9-tetrahydrocannabinol-induced responses and apparent agonist activity. J Pharmacol Exp Ther. 1996;277:586–594. [PubMed] [Google Scholar]
- de Fonseca FR, Del Arco I, Bermudez-Silva FJ, Bilbao A, Cippitelli A, Navarro M. The endocannabinoid system: physiology and pharmacology. Alcohol Alcohol. 2004;40:2–14. doi: 10.1093/alcalc/agh110. [DOI] [PubMed] [Google Scholar]
- De Vries TJ, Shaham Y, Homberg JR, Crombag H, Schuurman K, Dieben J, Vanderschuren LJMJ, Schoffelmeer ANM. A cannabinoid mechanism in relapse to cocaine seeking. Nat Med. 2001;7:1151–1154. doi: 10.1038/nm1001-1151. [DOI] [PubMed] [Google Scholar]
- Derocq JM, Segui M, Marchand J, Le Fur G, Casellas P. Cannabinoids enhance human B-cell growth at low nanomolar concentrations. FEBS Lett. 1995;369:177–182. doi: 10.1016/0014-5793(95)00746-v. [DOI] [PubMed] [Google Scholar]
- Despres JP, Golay A, Sjostrom L. Effects of rimonabant on metabolic risk factors in overweight patients with dyslipidemia. N Engl J Med. 2005;353:2121–2134. doi: 10.1056/NEJMoa044537. [DOI] [PubMed] [Google Scholar]
- DiMarzo V, Goparaju SK, Wang L, Liu J, Batkai S, Jaral Z, Fezza F, Miura GI, Palmiter RD, Sugiura T, Kunos G. Leptin-regulated endocannabinoids are involved in maintaining food intake. Nature. 2001;410:822–825. doi: 10.1038/35071088. [DOI] [PubMed] [Google Scholar]
- Folstein MF, Luria R. Reliability, validity, and clinical application of the Visual Analogue Mood Scale. Psychol Med. 1973;3:479–486. doi: 10.1017/s0033291700054283. [DOI] [PubMed] [Google Scholar]
- Fride E, Ginzburg Y, Breuer A, Bisogno T, Di Marzo V, Mechoulam R. Critical role of the endogenous cannabinoid system in mouse pup suckling and growth. Eur J Pharmacol. 2001;419:207–214. doi: 10.1016/s0014-2999(01)00953-0. [DOI] [PubMed] [Google Scholar]
- Galiegue S, Mary S, Marchand J, Dussossoy D, Carriere D, Carayon P, Bouaboula M, Shire D, Le Fur G, Casellas P. Expression of central and peripheral cannabinoid receptors in human immune tissues and leukocyte subpopulations. Eur J Biochem. 1995;252:54–61. doi: 10.1111/j.1432-1033.1995.tb20780.x. [DOI] [PubMed] [Google Scholar]
- Gessa GL, Orru A, Lai P, Maccioni P, Lecca R, Lobina C, Carai MA, Colombo G. Lack of tolerance to the suppressing effect of rimonabant on chocolate intake in rats. Psychopharmacology (Berl) 2006;185:248–254. doi: 10.1007/s00213-006-0327-1. [DOI] [PubMed] [Google Scholar]
- Gomez R, Navarro M, Ferrer B, Trigo JM, Bilbao A, Del Arco I, Cippitelli A, Nava F, Piomelli D, Rodriguez de Fonseca F. A peripheral mechanism for CB1 cannabinoid receptor-dependent modulation of feeding. J Neurosci. 2002;22:9612–9617. doi: 10.1523/JNEUROSCI.22-21-09612.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grotenhermen F. Pharmacology of cannabinoids. Neuro Endocrinol Lett. 2004;25:14–23. [PubMed] [Google Scholar]
- Hilairet S, Bouaboula M, Carriere D, Le Fur G, Casellas P. Hypersensitization of the Orexin 1 receptor by the CB1 receptor: evidence for cross-talk blocked by the specific CB1 antagonist, SR141716. J Biol Chem. 2003;278:23731–23737. doi: 10.1074/jbc.M212369200. [DOI] [PubMed] [Google Scholar]
- Howlett AC. Pharmacology of cannabinoid receptors. Annu Rev Pharmacol Toxicol. 1995;35:607–634. doi: 10.1146/annurev.pa.35.040195.003135. [DOI] [PubMed] [Google Scholar]
- Huang W, Moody DE, Andrenyak DM, Smith EK, Foltz RL, Huestis MA, Newton JF. Simultaneous determination of delta-9-tetrahydrocannabinol and 11-nor-9-carboxy-delta-9-tetrahydrocannabinol in human plasma by solid phase extraction and gas chromatography-negative ion chemical ionization-mass spectrometry. J Anal Toxicol. 2001;25:531–537. doi: 10.1093/jat/25.7.531. [DOI] [PubMed] [Google Scholar]
- Huestis MA, Henningfield JE, Cone EJ. Blood cannabinoids. I. Absorption of THC and formation of 11-OH-THC and THCCOOH during and after smoking marijuana. J Anal Toxicol. 1992a;16:276–282. doi: 10.1093/jat/16.5.276. [DOI] [PubMed] [Google Scholar]
- Huestis MA, Sampson AH, Holicky BJ, Henningfield JE, Cone EJ. Characterization of the absorption phase of marijuana smoking. Clin Pharmacol Ther. 1992b;52:31–41. doi: 10.1038/clpt.1992.100. [DOI] [PubMed] [Google Scholar]
- Huestis MA, Gorelick DA, Heishman SJ, Preston KL, Nelson RA, Moolchan ET, Frank RA. Blockade of effects of smoked marijuana by the CB1-selective cannabinoid receptor antagonist SR141716. Arch Gen Psychiatry. 2001;58:322–330. doi: 10.1001/archpsyc.58.4.322. [DOI] [PubMed] [Google Scholar]
- Jamshidi N, Taylor DA. Anandamide administration into the ventromedial hypothalamus stimulates appetite in rats. Br J Pharmacol. 2001;134:1151–1154. doi: 10.1038/sj.bjp.0704379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kirkham TC. Endogenous cannabinoids: a new target in the treatment of obesity. Am J Physiol Regul Integr Comp Physiol. 2003;284:R343–R344. doi: 10.1152/ajpregu.00706.2002. [DOI] [PubMed] [Google Scholar]
- Le Foll B, Goldberg SR. Rimonabant, a CB1 antagonist, blocks nicotine-conditioned place preferences. Neuroreport. 2004;15:2139–2143. doi: 10.1097/00001756-200409150-00028. [DOI] [PubMed] [Google Scholar]
- Le Foll B, Goldberg SR. Cannabinoid CB1 antagonists as promising new medications for drug dependence. J Pharmacol Exp Ther. 2005;312:875–883. doi: 10.1124/jpet.104.077974. [DOI] [PubMed] [Google Scholar]
- Matsuda LA, Lolait SJ, Brownstein MJ, Young AC, Bonner TI. Structure of a cannabinoid receptor and functional expression of the cloned cDNA. Nature. 1990;346:561–564. doi: 10.1038/346561a0. [DOI] [PubMed] [Google Scholar]
- McMahon LR. Discriminative stimulus effects of the cannabinoid CB(1) antagonist SR 141716A in rhesus monkeys pretreated with Delta(9)-tetrahydrocannabinol. Psychopharmacology (Berl) 2006;188:306–314. doi: 10.1007/s00213-006-0500-6. [DOI] [PubMed] [Google Scholar]
- Mechoulam R, Gaoni Y. A total synthesis of dl-delta-1-tetrahydrocannabinol, the active constituent of hashish. J Am Chem Soc. 1965;87:3273–3274. doi: 10.1021/ja01092a065. [DOI] [PubMed] [Google Scholar]
- Navarro M, Carrera MR, Del Arco I, Trigo JM, Koob GF, Rodriguez de Fonseca F. Cannabinoid receptor antagonist reduces heroin self-administration only in dependent rats. Eur J Pharmacol. 2004;501:235–237. doi: 10.1016/j.ejphar.2004.08.022. [DOI] [PubMed] [Google Scholar]
- Ohlsson A, Lindgren JE, Wahlen A, Agurell S, Hollister LE, Gillespie HK. Plasma levels of delta-9-tetrahydrocannabinol after intravenous, oral and smoke administration. NIDA Res Monogr. 1981;34:250–256. [PubMed] [Google Scholar]
- Ohlsson A, Lindgren JE, Wahlen A, Agurell S, Hollister LE, Gillespie HK. Single dose kinetics of deuterium labelled delta-1-tetrahydrocannabinol in heavy and light cannabis users. Biomed Environ Mass Spectrom. 1982;9:6–10. doi: 10.1002/bms.1200090103. [DOI] [PubMed] [Google Scholar]
- Pi-Sunyer FX, Aronne LJ, Heshmati HM, Devin J, Rosenstock J. Effect of rimonabant, a cannabinoid-1 receptor blocker, on weight and cardiometabolic risk factors in overweight or obese patients: RIO-North America: a randomized controlled trial. JAMA. 2006;295:761–775. doi: 10.1001/jama.295.7.761. [DOI] [PubMed] [Google Scholar]
- Rao GK, Zhang W, Kaminski NE. Cannabinoid receptor-mediated regulation of intracellular calcium by delta(9)-tetrahydrocannabinol in resting T cells. J Leukoc Biol. 2004;75:884–892. doi: 10.1189/jlb.1203638. [DOI] [PubMed] [Google Scholar]
- Ravinet Trillou C, Arnone M, Delgorge C, Gonalons N, Keane P, Maffrand JP, Soubrie P. Anti-obesity effect of SR141716, a CB1 receptor antagonist, in diet-induced obese mice. Am J Physiol Regul Integr Comp Physiol. 2003;284:R345–R353. doi: 10.1152/ajpregu.00545.2002. [DOI] [PubMed] [Google Scholar]
- Ravinet Trillou C, Delgorge C, Menet C, Arnone M, Soubrie P. CB1 cannabinoid receptor knockout in mice leads to leanness, resistance to diet-induced obesity and enhanced leptin sensitivity. Int J Obes. 2004;28:640–648. doi: 10.1038/sj.ijo.0802583. [DOI] [PubMed] [Google Scholar]
- Rinaldi-Carmona MR, Barth F, Heaulme M, Shire D, Calandra B, Congy C, Martinez S, Maruani J, Neliat G, Caput D, Ferrara P, Soubrie P, Breliere JC, Le Fur GL. SR141716, a potent and selective antagonist of the brain cannabinoid receptor. FEBS Lett. 1994;350:240–244. doi: 10.1016/0014-5793(94)00773-x. [DOI] [PubMed] [Google Scholar]
- Simiand J, Keane M, Keane PE, Soubrie P. SR 141716, a CB1 cannabinoid receptor antagonist, selectively reduces sweet food intake in marmoset. Behav Pharmacol. 1998;9:179–181. [PubMed] [Google Scholar]
- Tomasini MC, Ferraro L, Bebe BW, Tanganelli S, Cassano T, Cuomo V, Antonelli T. Delta(9)-tetrahydrocannabinol increases endogenous extracellular glutamate levels in primary cultures of rat cerebral cortex neurons: involvement of CB(1) receptors. J Neurosci Res. 2002;68:449–453. doi: 10.1002/jnr.10242. [DOI] [PubMed] [Google Scholar]
- Tseng AH, Craft RM. CB(1) receptor mediation of cannabinoid behavioral effects in male and female rats. Psychopharmacology (Berlin) 2004;172:25–30. doi: 10.1007/s00213-003-1620-x. [DOI] [PubMed] [Google Scholar]
- Turpault S, Kanamaluru V, Lockwood GF, Bonnet D, Newton J. Rimonabant pharmacokinetics in healthy and obese subjects. Clin Pharmacol Ther. 2006;79:P50. [Google Scholar]
- Van Gaal LF, Rissanen AM, Scheen AJ, Ziegler O, Rossner S. Effects of the cannabinoid-1 receptor blocker rimonabant on weight reduction and cardiovascular risk factors in overweight patients: 1-year experience from the RIO-Europe study. Lancet. 2005;365:1389–1397. doi: 10.1016/S0140-6736(05)66374-X. [DOI] [PubMed] [Google Scholar]
- Walker JM, Huang SM. Cannabinoid analgesia. Pharmacol Ther. 2002;95:127–135. doi: 10.1016/s0163-7258(02)00252-8. [DOI] [PubMed] [Google Scholar]
- Wang L, Liu J, Harvey-White J, Zimmer A, Kunos G. Endocannabinoid signaling via cannabinoid receptor 1 is involved in ethanol preference and its age-dependent decline in mice. Proc Natl Acad Sci U S A. 2003;100:1393–1398. doi: 10.1073/pnas.0336351100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Westlake TM, Howlett AC, Bonner TI, Matsuda LA, Herkenham M. Cannabinoid receptor binding and messenger RNA expression in human brain: an in vitro receptor autoradiography and in situ hybridization histochemistry study of normal aged and Alzheimer's brains. Neuroscience. 1994;63:637–652. doi: 10.1016/0306-4522(94)90511-8. [DOI] [PubMed] [Google Scholar]
- Williams CM, Kirkham TC. Anandamide induces overeating: mediation by central cannabinoid (BC1) receptors. Psychopharmacology. 1999;143:315–317. doi: 10.1007/s002130050953. [DOI] [PubMed] [Google Scholar]