Summary
Renal cell carcinoma metastasis to the parotid gland after tumour nephrectomy is extremely rare. Herewith a review of the literature on this topic is discussed and a case report is presented of a 69-year-old man affected by parotid localization of renal clear cell carcinoma with neck lymph node metastases and involvement of the masseter muscle 2 years after nephrectomy. When an otolaryngologist encounters a parotid mass, diverse differential diagnoses have to be considered. A high level of suspicion of metastatic disease from the specific primary site will help in achieving correct diagnosis and evaluation of the extension of the disease. Surgical resection, even enlarged parotidectomy with neck dissection, should be considered as a therapeutic option for exclusive location of the disease in the head and neck.
Keywords: Parotid, Malignant tumours, Metastasis, Renal cell carcinoma, Therapy
Riassunto
Dopo una nefrectomia, la metastasi parotidea da carcinoma a cellule renali è un evento estremamente raro. Abbiamo effettuato una revisione della letteratura riguardante questo argomento e presentiamo il caso di un paziente di 69 anni che 2 anni dopo una nefrectomia ha sviluppato una metastasi parotidea da carcinoma a cellule renali con metastasi linfonodali laterocervicali ed estensione al muscolo massetere. Quando l’otorinolaringoiatra valuta una massa della parotide deve avere presente varie diagnosi differenziali. Sospettare la presenza di una metastasi parotidea servirà nel formulare una diagnosi corretta e nel definire l’estensione della malattia. L’intervento chirurgico, anche qualora si trattasse di una parotidectomia allargata associata allo svuotamento laterocervicale, va considerato fra le opzioni terapeutiche nei casi che si presentino esclusivamente localizzati a livello cervico-facciale.
Case-report
In May 2005, a 67-year-old man underwent right nephrectomy for renal clear cell carcinoma (pT2N0, G2). During his adolescence, the patient had been affected by tubercular pleuritis. In 1998, moderate chronic renal failure was diagnosed.
After right nephrectomy, renal failure rapidly worsened requiring dialysis with subsequent clinical improvement.
For the remainder of 2005, the patient was free of disease until November 2006 when physicians discovered a deeply adherent, painless mass in the right parotid region. On clinical examination, there was no facial weakness.
Fine needle aspiration biopsy (FNAB) was immediately performed and the pathologist’s report showed metastasis from renal cell carcinoma. On a computed tomography (CT) scan with contrast of the head and neck, a large bulge of the right parotid gland involving the masseter muscle and two suspicious ipsilateral neck lymphoadenopathies were visible (Figs. 1, 2).
Fig. 1.
Computed tomography scan revealing enhancing mass in parotid gland with extension to masseter muscle.
Fig. 2.
Computed tomography scan showing highly suspicious neck lymph nodes.
Metastatic work-up, by total-body 6FDG-PET, was completely negative, except for the parotid gland and neck.
Total right parotidectomy and selective neck dissection (levels I-V) were performed (Figs. 3, 4).
Fig. 3.
Pre-operative image of mass in right parotid gland.
Fig. 4.
Image of an intra-operative view.
A large part of the masseter muscle and the inferior branch of the facial nerve were involved in the tumour mass requiring resection.
Inferior right facial weakness remained but no other post-operative complication occurred.
The pathological specimen showed a 6 x 4 cm parotid tumour and 3 x 3 cm neck lymph nodes.
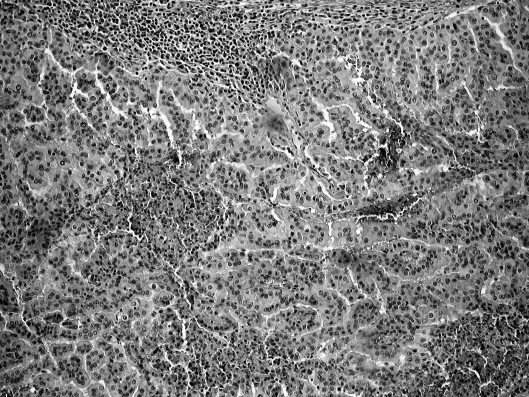
On histological and immunohistochemical examination, patterns of renal clear cell carcinoma, diffusely infiltrating, and the presence of two massive neck lymph node metastases were confirmed (Fig. 5). Negative surgical margins were obtained. The treatment was completed by radiotherapy.
Fig. 5.
Microphotograph demonstrating metastatic renal clear cell carcinoma.
Discussion
Metastasis to the parotid gland rarely occurs and usually proceeds from skin cancers of the head and neck, such as melanoma in 45% of cases and squamous cell carcinoma in 37%. Melanoma is more frequently observed in paraparotid lymph nodes (70%) while squamous cell carcinoma of the skin involves the intraglandular lymph nodes (47%) 1.
When the primary cancer originates in sites below the clavicle, metastases to the head and neck are uncommon 2–6. Parotid localization from renal cell carcinoma is an extremely rare finding 7 8. In a large series of patients with renal cell carcinoma, with metastases to the head and neck, parotid metastases never occurred 9.
The mechanism by which a renal cell carcinoma reaches the parotid gland is probably the haematogeneous spread. In fact, renal cell carcinomas are hypervascular tumours associated with multiple arteriovenous shunt. Considering the fact that kidneys receive 25% of circulating blood volume, renal cell carcinoma has a high haematogeneous spreading potential 7 10.
In order of frequency, renal cell carcinoma commonly metastatizes to lung, bone, liver, brain and skin, while metastases to the head and neck region are rarer (8-14%), the thyroid accounting for a large percentage of cases 4.
The English language literature identifies 26 cases of renal cell carcinoma, metastatic to the parotid gland, while taking into account that most patients presented multiple metastases and solitary parotid location is extremely rare 7 10.
In 14 of these patients, parotid metastasis was the initial sign of malignancy in the kidney. On the other hand, in 12 patients, parotid metastasis occurred after the primary treatment for renal cell carcinoma, at a time interval ranging from months to years 7 10. To our knowledge, the longest interval from nephrectomy to solitary parotid metastasis is 10 years, with only one case reported in the literature 10.
In patients presenting with parotid bulk, unless one maintains a high index of suspicion, the unsuspected disease may be completely overlooked. Radiological findings are indistinguishable from those of a primary cancer. Parotid ultrasonography reveals a heterogeneous lesion and head and neck CT with contrast findings are not specific 3.
As in our case, some Authors confirm the diagnosis using FNAB although false-positive and false-negative cases have been reported 4 5 7 8 10–12. Even when FNAB cannot differentiate between primary parotid cancer and metastases from other primary lesions, it provides important information for management of the patient.
In recent years, new diagnostic techniques have provided the possibility to evaluate the metabolism of several lesions by the uptake of radioactive glucose 13 14. If carcinoma is identified on parotid FNAB in a patient with a history of renal cell carcinoma, re-staging with 6FDG-PET is mandatory. In our case, data of previous nephrectomy and actual renal cell carcinoma metastasis were strongly suspicious because of neoplastic emboli spreading in multiple sites.
On the basis of the extension of the disease, treatment is consistently different. Treatment of diffuse metastatic disease is a combination of chemotherapy, immunotherapy, hormone therapy and radiation therapy, but the results are dismal 7 15. On the other hand, it is well known that management for clinically solitary metastasis is aggressive surgical resection. In patients with a solitary metastasis amenable to surgical resection the five-year survival rate was 53% 16. Solitary parotid metastasis and a long interval are favourable prognostic factors. If the parotid gland is the only site affected, the patient should undergo superficial parotidectomy with preservation of the facial nerve 3 4 7 8 10.
Taking into account our experience and our review of the literature, when parotid metastasis extends to the surrounding anatomical structures, their surgical resection is, in our opinion, a correct approach to cure the patient. In the patient described herewith, parotidectomy was enlarged to the deep lobe, the masseter muscle, the inferior branch of the facial nerve and selective (level I-V) neck dissection was performed.
The involvement of structures, like muscle and nerve, that give the cancer cells a theoretical way of spreading and two massive metastases present in the lymph nodes in the neck, argued in favour of performing radiotherapy.
In conclusion, we want to emphasize the following items:
when parotid bulk appears, the history of the patient should be checked carefully;
FNAB is of major importance in orientating the diagnosis;
6FDG-PET contributes greatly to cancer re-staging;
surgery, even with resection wider than superficial parotidectomy, possibly associated with post-operative radiotherapy, should be considered as a therapeutic option when metastatic disease affects the parotid gland, its surrounding structures and the lymph nodes, on that side of the neck, but is not present in other parts of the body.
References
- 1.Coppa GF, Oszczakiewicz M. Parotid gland metastasis from renal cell carcinoma. Int Surg 1990;75:198-202. [PubMed] [Google Scholar]
- 2.Batsakis J. Parotid gland and its lymph nodes as metastatic sites. Ann Otol Rhinol Laryngol 1983;92:209-10. [DOI] [PubMed] [Google Scholar]
- 3.Vara A, Madrigal B, Perez del Rio MJ, Diaz A, Mateos A, Sales C. Parotid metastasis from renal clear cell adenocarcinoma. An unusual site for metastasis. Urol Int 1998;61:196-8. [DOI] [PubMed] [Google Scholar]
- 4.Sykes TCF, Patel A, Archer D, Fisher C, Hendry WF. Parotid metastasis from renal cell carcinoma. Br J Urol 1995;76:398-9. [DOI] [PubMed] [Google Scholar]
- 5.Borghi L, Bianchini E, Ballotta MR, Reale D. Metastatic renal cell carcinoma presenting as a parotid tumour. A case report. Pathologica 1995;87:168-70. [PubMed] [Google Scholar]
- 6.Som PM, Norton KJ, Shugar JM, Reede DL, Norton L, Biller HF, et al. Metastatic hypernephroma to the head and neck. Am J Neuroradiol 1987;8:1103-6. [PMC free article] [PubMed] [Google Scholar]
- 7.Park YW, Hlivo TJ. Parotid gland metastasis from renal cell carcinoma. Laryngoscope 2002;112:453-6. [DOI] [PubMed] [Google Scholar]
- 8.Kundu S, Eynon-Lewis NJ, Radcliffe GJ. Extensive metastatic renal cell carcinoma presenting as facial nerve palsy. J Laryngol Otol 2001;115:488-90. [DOI] [PubMed] [Google Scholar]
- 9.Saitoh H. Distant metastasis of renal adenocarcinoma. Cancer 1981;48:1487-91. [DOI] [PubMed] [Google Scholar]
- 10.Gögüs Ç, Kiliç Ö, Tulunay Ö, Tulunay Ö, Bedük Y. Solitary metastasis of renal cell carcinoma to the parotid gland 10 years after radical nephrectomy. Int J Urol 2004;11:894-6. [DOI] [PubMed] [Google Scholar]
- 11.Melnick SF, Amazon K, Dembrow V. Metastatic renal cell carcinoma presenting as a parotid tumour; a case report with immunohistochemical findings and a review of the literature. Hum Pahol 1989;20:195-7. [DOI] [PubMed] [Google Scholar]
- 12.Frable MA, Frable WJ. Fine needle aspiration biopsy of salivary glands. Laryngoscope 1991;101:245-9. [DOI] [PubMed] [Google Scholar]
- 13.Stokkel MP, ten Broek FW, van Rijk PP. The role of FDG PET in the clinical management of head and neck cancer. Oral Oncol 1998;34:466-71. [DOI] [PubMed] [Google Scholar]
- 14.Manolidis S, Donald PJ, Volk P, Pounds TR. The use of Positron Emission Tomography scanning in occult and recurrent head and neck cancer. Acta Otolaryngol 1992;S534:5-11. [DOI] [PubMed] [Google Scholar]
- 15.Amato RJ. Renal cell carcinoma: review of novel single-agent therapeutics and combination regimens. Ann Oncol 2005;16:7-15. [DOI] [PubMed] [Google Scholar]
- 16.Marulli G, Sartori F, Bassi PF, Dal Moro F, Gino Favretto A, Rea F. Long-term results of surgical management of pulmonary metastases from renal cell carcinoma. Thorac Cardiovasc Surg 2006;54:544-7. [DOI] [PubMed] [Google Scholar]