Summary
Aim of the present report is to discuss and underline the diagnostic algorithm and the surgical approach to giant parotid pleomorphic adenomas arising in the deep lobe and growing in the parapharyngeal space. Three cases are described and a review is made of the international literature concerning giant deep lobe parotid gland pleomorphic adenoma. Diagnosis was based on imaging, computed tomography scan and magnetic resonance imaging and upon cytology, by means of fine needle aspiration biopsy. The surgical approach varied according to the location of the tumour. All patients were discharged without complications and no cases of permanent facial nerve palsy were observed. An exhaustive pre-operative diagnostic algorithm is required before approaching this lesion. Fine needle aspiration biopsy is, in our opinion, mandatory to avoid histological surprises. The surgical approach should provide excellent visibility with wide surgical exposure to secure local neurovascular structures.
Keywords: Salivary glands, Tumours, Pleomorphic adenoma, Parapharyngeal space, Diagnosis, Surgical treatment
Riassunto
Scopo del lavoro è incentrare l’attenzione sul protocollo diagnostico e sulle tecniche chirurgiche in merito al trattamento degli adenomi pleomorfi giganti del lobo profondo della parotide con crescita nello spazio parafaringeo. Riportiamo la nostra esperienza con tre casi consecutivi recenti di adenoma pleomorfo gigante del lobo profondo della parotide con crescita nello spazio parafaringeo. La diagnosi si fonda sull’impiego di tomografia computerizzata, risonanza magnetica e dell’esame citologico mediante agobiopsia. Le tecniche chirurgiche variano a seconda dell’estensione e della localizzazione della neoplasia. Tutti i pazienti sono stati dimessi dopo una completa asportazione della neoplasia senza presentare complicanze intra- e peri-operatorie e, in particolare, deficit del nervo facciale. In conclusione, un completo e approfondito iter diagnostico è necessario prima di trattare neoplasie localizzate in questa sede. L’agobiopsia, secondo noi, è necessaria per evitare sorprese istologiche spiacevoli. L’approccio chirurgico deve fornire una ampia visione del letto chirurgico in modo da assicurare una completa escissione preservando le strutture neurovascolari.
Introduction
Tumours located in the parapharyngeal space are relatively rare, and experience in diagnosis and treatment is very limited. Management of these tumours is more challenging due to the anatomical location of the parapharyngeal space: this space is situated behind the infra-temporal fossa, laterally to the nasopharynx, and before the cervical column. This space is shaped like an inverted pyramid, the base of which is formed by the base of the cranium (small portion of petrosal bone), and the apex defines the joint between the posterior belly of the digastric muscle and the greater cornu of the hyoid bone. Here, the styloid process and the associated musculature are also found, as well as the internal carotid artery, the sympathetic chain and the IX and XII cranial nerve pairs. Post-styloid masses are usually benign and correspond to neurogenic tumours, paragangliomas, vascular tumours, or aneurysms. Those located in front of the carotid artery are called prestyloid and their origin is much more varied 1.
Pleomorphic adenoma is the most common salivary gland neoplasm, accounting for 63% of all parotid gland tumours 2. Most tumours originate in the superficial lobe but, more rarely, these tumours may involve the deep lobe of the parotid gland 3, growing medially and occupying the parapharyngeal space. It is generally considered to be a benign tumour, even if this lesion presents several histological features due to the different compounds with a mixoid or condroid matrix. The main characteristics are the high recurrence rate and not infrequent malignant conversion. Symptoms are usually rare or not significant; in fact, in most cases, the only sign is asymptomatic swelling, that slowly grows in the parotid region without involving the facial nerve, the function of which remains unchanged. Often, onset of a facial nerve deficit, changes in consistency, more rapid growth as well as pain are signs of malignant transformation. The histological variety of this tumour along with the particular location, increase the difficulty in selecting the best surgical approach to maximize visibility, ensure complete removal of the tumour, and reduce morbidity.
Herewith, three consecutive cases are described of giant deep lobe parotid gland pleomorphic adenoma, treated in our Department. A review has been made of the literature, discussion of which focuses on the diagnosis, the surgical approach and any complementary treatment.
Case reports
Case 1
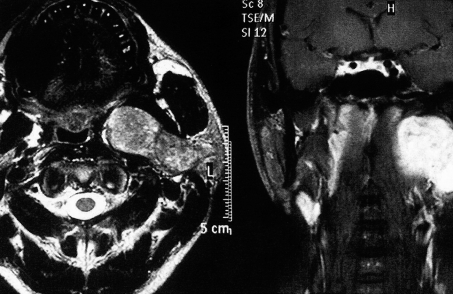
A 36-year-old male with no previous clinical history of importance was referred to our Clinic for a swelling in the left parotid region presenting one year previously. The patient did not complain of any associated symptoms. Physical examination revealed a mass of ~ 5 cm in size, located in the left parotid region, solid in consistency and painless to palpation. Neck ultrasonography (US) revealed a hypo-echogenic polylobulated lesion occupying the deep lobe of the left parotid gland and measuring 25 x 19 x 16 mm, and a second mass located behind the left mandibular angle, measuring 44 x 51 x 46 mm. Magnetic resonance imaging (MRI) showed a large expansive oval mass, measuring about 5 cm in diameter, with apparently regular edges, and located medially to the mandibular angle in the parapharyngeal space. The lesion appeared to be in continuity with the deep lobe of the parotid gland. Moreover, it caused obliteration of the adipose cleavage planes and deformation of the pharyngeal lateral wall with reduction of the air column. The homolateral jugular vein was reduced in calibre and was in a back dislocation (Fig. 1). Fine needle aspiration cytology (FNAC) was not useful in the diagnosis showing reactive lymphadenitis in a lymph node within the parotid.
Fig. 1.
MRI axial and coronal scans reveal a large tumour with high contrast enhancement, located deep in left parapharyngeal space displacing muscles and provoking lateral swelling.
After obtaining the patient’s informed consent to the surgical procedure, complete excision of the lesion was performed using the cervical-transparotid approach preserving the facial nerve. The left parotid superficial lobe was resected. The facial nerve was considerably dislocated laterally by the neoformation adhering to the deep planes of the parapharyngeal space. The facial nerve was then gently dissected from the deep lobe and the tumour was completely removed together with the parotid deep lobe from the parapharyngeal space. Histological examination revealed a pleomorphic adenoma of the parotid gland.
After a few days, the patient was discharged with a light and temporary deficit of the marginalis nerve.
Case 2
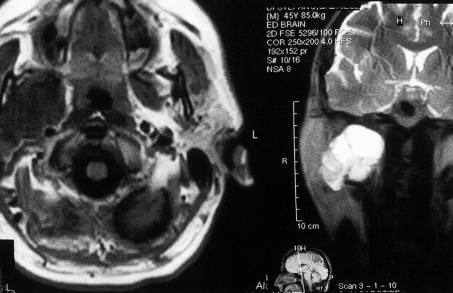
A 42-year-old male, with no previous clinical history of importance, was referred to our Clinic on account of an asymptomatic mass which had been increasing in size over the last 2 months in the region of the right mandibular angle. On examination, a tumour, 3 cm in diameter, of solid consistency, non-mobile, and not painful when palpated, was found in the right parotid region. The patient underwent MRI which showed a large growth in the deep parotid lobe, extending medially to the parapharyngeal space, provoking medial displacement of the muscles. It showed a low-density in T1 and a high-density in T2, evoking a solid formation (Fig. 2). FNAC, performed trans-cutaneously, was consistent with pleomorphic adenoma. The patient underwent surgery and excision of the lesion was performed via the cervical-transparotid approach; following the facial nerve, the superficial lobe was dissected to reach the deep lobe and parapharyngeal space; a blunt dissection of the deep lobe with the tumour was performed with complete extirpation. The histological exam confirmed the diagnosis of pleomorphic adenoma. The patient was discharged, after 7 days, with no signs of facial palsy.
Fig. 2.
T1 and T2 MRI scans showing tumour in continuity with deep right parotid lobe causing swelling in parotid region.
Case 3
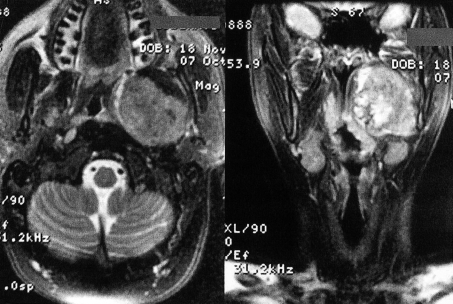
A 38-year-old female, with no previous clinical history of note, came to our Clinic complaining of pharyngodynia and the sensation of a foreign body in the pharynx which had been present for ~ 5 months. Physical examination showed a swelling on the left side of the soft palate; it was hard-woody with a normal overlying mucosa. No latero-cervical adenopathies were clinically appreciable. MRI showed a large expansive oval formation measuring ~ 58 x 55 mm with regular edges, localized in the left parapharyngeal space. The adipose cleavage plane appeared medially displaced by the mass, which dislocated the pterygoid muscle, and was attached to the parotid deep lobe and in contact with the neck long muscle posteriorly. The vascular-nervous bundle appeared dislocated posteriorly, without signs of infiltration. This mass presented a dishomogeneous enhancement following contrast injection, as necrotic irregular areas in the middle and peripheral areas (Fig. 3). FNAC, performed transorally, revealed a cytological picture of pleomorphic adenoma with some atypical neoplastic cells.
Fig. 3.
T2 fat suppression MRI scans showing large tumour in left parapharyngeal space arising in oral cavity and reducing pharyngeal air column.
After obtaining the patient’s informed consent, surgical exeresis was performed, of the parotid gland and of the parapharyngeal mass, by a cervical-transparotid approach combined with mandibular osteotomy, in order to achieve radical excision of the mass. The parotid superficial lobe and part of the deep lobe were removed by a cervical incision, respecting facial nerve integrity. The remnant of the deep parotid lobe together with the tumour were removed by para-median mandibulotomy: the procedure was continued along the oral floor and the lateral portion of the palatine pillar as far as the left parapharyngeal space. Complete resection of the large neoformation which licked the homolateral parotid area was then performed. Histological examination revealed a nucleus of carcinoma ex-pleomorphic adenoma inside the large pleomorphic adenoma, corresponding to the area with a higher contrast enhancement upon MRI. The patient was discharged after 7 days with no facial nerve deficit and was submitted to radiotherapy.
Discussion
Pleomorphic adenoma is the most frequent parotid gland tumour, presenting a high rate of recurrence even if it resembles a benign neoplasm. Due to the few symptoms complained of by the patient and the possibility of extention into a hidden site, such as the parapharyngeal space, they can grow for a long time before being diagnosed, and the potential risk of malignant transformation increases over the years with an incidence of 1-7% 4.
They are generally discovered, during routine physical examination, as an asymptomatic mass. Usually, they appear as a cervical swelling, as in our first two cases, or as an intra-oral mass, as in the third patient. Indeed, they remain silent for a long time and the slow growth does not lead to symptoms even if the tumour is in contact, or displaces, vital structures located in the parapharyngeal space, such as vessels or nerves.
Diagnostic imaging, such as computed tomography (CT) or MRI, are mandatory: MRI is preferred, on account of its better definition of soft tissue, and provides precise information concerning tumour margins as well as the relationship with the surrounding structures.
Much controversy exists regarding the use of FNAC in the diagnostic procedures due to localization of these lesions and their relationship with the vascular and nervous structures, that can be damaged by this kind of examination. In our opinion, FNAC is a reliable procedure that can guide the surgeon and be useful in choosing the right surgical approach 5 6, even though it would not be the first choice diagnostic tool, but it should be performed following diagnostic imaging in order to exclude a vascular lesion. Depending upon the location of the lesion, it can be performed intra-orally or percutaneously: some Authors report that the former is more sensitive and prefer the external approach, guided by imaging to avoid vital structures 7. In the cases described in the present report, reliable results were obtained also performing FNAC intra-orally. Open neck or trans-oral biopsies should be avoided, since opening the tumour capsule increases the risk of recurrence.
The elective treatment of para-pharyngeal space tumours is surgery. Many different approaches have been described in the literature 2 8–13. All Authors agree on the need to perform surgery requiring adequate exposure to identify and protect vital structures and ensure complete removal.
Approaches involving lateral neck dissection are indicated for large tumours involving the para-pharyngeal space without reaching the deep parotid lobe, but full surgical exposure is impeded by the presence of the mandible. The most frequent is the cervical-trans-parotid approach, that allows exeresis of the benign lesion with good control on the vascular and nervous structures following dissection of the superficial parotid lobe. In our first two cases, this kind of surgical technique was used, given the characteristics of the lesion; in fact, the dimensions and position in the deep parotid lobe allowed a trans-parotid approach to be performed. Various techniques involving osteotomy of the ramus 14 15, the angle 16 17 or the body of the mandible 18 19 and some modified techniques 20 have been described. We adopted a trans-mandibular approach in the third case due to the deep location of the tumour which created ballooning of the soft palate, and to the FNAC results, which indicated a possible malignant transformation. Median mandibulotomy increases surgical exposure, preserves mandibular nerve function and provides adequate control both of the neoplasm and of the cervical vessels. Some Authors 9 12 disagree with this approach as aesthetics are compromised by the labiotomy incision, and it also requires entering the oral cavity and involves salivary contamination of the wound. In our opinion, a well-trained surgeon, paying attention to the suture, can achieve good aesthetical results without infection of the wound.
A trans-palatal approach is reported 21 22 but, in spite of the aesthetic benefit, it does not offer good control of the vascular and nervous structures on account of its small working area and it does not provide adequate exposure for removal of the tumour which is often extirpated fragmented, increasing the rate of recurrence. Therefore, this technique should be indicated only for small benign lesions (< 3 cm) which occupy the anterior parapharyngeal deep planes.
The incidence of malignant transformation increases with time elapsing prior to surgery. Carcinoma ex-pleomorphic adenoma is usually an aggressive tumour. Almost one-half of the patients develop recurrences, and approximately one-third of the patients with parotid tumours develops metastases. The target gene in adenomas with rearrangements of genotype is the high mobility group protein gene (HMGIC) 23. This gene is also rearranged in a variety of mesenchymal tumours. HMGIC encodes an architectural transcription factor that promotes activation of gene expression by modulating the conformation of DNA. Detailed analysis of cells revealed that HMGIC and MDM2 (murine double minute 2) were deleted and that they were strongly positive for both genes. Southern blot analysis confirmed that both HMGIC and MDM2 were amplified and that no gross rearrangements of the genes had occurred. Immunostaining revealed that the HMGIC protein was highly overexpressed particularly in the large polymorphic cells within the carcinomatous part of the tumour. These findings suggest that amplification and overexpression of HMGIC and possibly MDM2 might be important genetic events possibly contributing to malignant transformation of benign pleomorphic adenoma. The malignant transformation of such benign neoplasms into carcinoma ex-pleomorphic adenoma, requires additional treatment in order to reduce any eventual recurrence. Our third patient, according to Chen’s series 24, underwent post-operative radiotherapy: indeed, surgery, followed by post-operative radiotherapy should be considered standard care for patients with carcinoma ex pleomorphic adenoma.
In summary, an exhaustive pre-operative diagnostic algorithm is required before approaching this lesion: MRI provides important information about the location and margins and can guide the surgeon in planning the right approach. FNAC, in our opinion, is mandatory to avoid any histological surprise. The surgical approach should provide excellent visibility with wide surgical exposure to secure local neurovascular structures: in our experience, we approached the tumour by means of transparotid surgery when the lesion was located higher and laterally; in the other case, when the tumour had a lower and more medial location, a combined transparotid and transmandibular approach was performed.
References
- 1.Batsakis JG, Sneige N. Parapharyngeal and retropharyngeal space diseases. Ann Otol Rhinol Laryngol 1989;98:320-1. [DOI] [PubMed] [Google Scholar]
- 2.Eveson JW, Cawson RA. Salivary gland tumours. A review of 2410 cases with particular reference to histological types, site, age and sex distribution. J Pathol 1985;146:51-8. [DOI] [PubMed] [Google Scholar]
- 3.Morita N, Miyata K, Sakamoto T, Wada T. Pleomorphic adenoma in the parapharyngeal space: report of three cases. J Oral Maxillofac Surg 1995;53:605-10. [DOI] [PubMed] [Google Scholar]
- 4.Izzo L, Frati R, Cianfrone F, Sassayannis PG, Costi U, Galati G, et al. Parotid gland cancer: a case report of a primitive adenocarcinoma arising from a multirecurrent pleomorphic adenoma. J Exp Clin Cancer Res 2004;23:153-6. [PubMed] [Google Scholar]
- 5.Contucci AM, Corina L, Sergi B, Fadda G, Paludetti G. Correlation between fine needle aspiration biopsy and histologic findings in parotid masses. Personal experience. Acta Otorhinolaryngol Ital 2003;23:314-8. [PubMed] [Google Scholar]
- 6.Sergi B, Contucci AM, Corina L, Paludetti G. Value of fine-needle aspiration cytology of parotid gland masses. Laryngoscope 2004;114:789. [DOI] [PubMed] [Google Scholar]
- 7.Yousem DM, Sack MJ, Scanlan KA. Biopsy of parapharyngeal space lesions. Radiology 1994;193:619-22. [DOI] [PubMed] [Google Scholar]
- 8.Olsen KD. Tumors and surgery of the parapharyngeal space. Laryngoscope 1994;104(Suppl.63):1-28. [DOI] [PubMed] [Google Scholar]
- 9.Bozzetti A, Biglioli F, Gianni AB, Brusati R. Mandibulotomy for access to benign deep lobe parotid tumors with parapharyngeal extension: report of four cases. J Oral Maxillofac Surg 1998;56:272-6. [DOI] [PubMed] [Google Scholar]
- 10.Guinto G, Abello J, Molin A, Gallegos F, Oviedo A, Nettel B, et al. Zygomatic-transmandibular approach for giant tumors of the infratemporal fossa and parapharyngeal space. Neurosurgery 1999;45:1385-98. [DOI] [PubMed] [Google Scholar]
- 11.Panoussopoulos D, Yotakis J, Pararas B, Theodoropoulos G, Papadimitriou K. Giant pleomorphic adenoma of the parotid gland involving the parapharyngeal space treated by a totally extraoral transparotid approach. J Surg Oncol 2002;81:155-7. [DOI] [PubMed] [Google Scholar]
- 12.Smith GI, Brennan PA, Webb AA, Ilankovan V. Vertical ramus osteotomy combined with a parasymphyseal mandibulotomy for improved access to the parapharyngeal space. Head Neck 2003;25:1000-3. [DOI] [PubMed] [Google Scholar]
- 13.Rodriguez-Ciurana J, Rodado C, Saez M, Bassas C. Giant parotid pleomorphic adenoma involving the parapharyngeal space: report of a case. J Oral Maxillofac Surg 2000;58:1184-7. [DOI] [PubMed] [Google Scholar]
- 14.Bass RM. Approaches to the diagnosis and treatment of tumors of the parapharyngeal space. Head Neck Surg 1982;4:281-9. [DOI] [PubMed] [Google Scholar]
- 15.Pogrel MA, Kaplan MJ. Surgical approach to the pterygomaxillary region. J Oral Maxillofac Surg 1986;44:183-7. [DOI] [PubMed] [Google Scholar]
- 16.Berdal P, Hall JG. Parapharyngeal growth of parotid tumours. Acta Otolaryngol Suppl 1969;263:164-6. [DOI] [PubMed] [Google Scholar]
- 17.Carr RJ, Bowerman JE. A review of tumours of the deep lobe of the parotid salivary gland. Br J Oral Maxillofac Surg 1986;24:155-68. [DOI] [PubMed] [Google Scholar]
- 18.Spiro RH, Gerold FP, Shah JP, Sessions RB, Strong EW. Mandibulotomy approach to oropharyngeal tumors. Am J Surg 1985;150:466-9. [DOI] [PubMed] [Google Scholar]
- 19.Attia EL, Bentley KC, Head T, Mulder D. A new external approach to the pterygomaxillary fossa and parapharyngeal space. Head Neck Surg 1984;6:884-91. [DOI] [PubMed] [Google Scholar]
- 20.Flood TR, Hislop WS. A modified surgical approach for parapharyngeal space tumours: use of the inverted ‘L’ osteotomy. Br J Oral Maxillofac Surg 1991;29:82-6. [DOI] [PubMed] [Google Scholar]
- 21.Myatt HM, Remedios D. A transpalatal approach to the parapharyngeal space. J Laryngol Otol 1997;111:159-62. [DOI] [PubMed] [Google Scholar]
- 22.Ruiz-Laza L, Infante-Cossio P, Garcia-Perla A, Hernandez-Guisado JM, Gutierrez-Perez JL. Giant pleomorphic adenoma in the parapharyngeal space: report of 2 cases. J Oral Maxillofac Surg 2006;64:519-23. [DOI] [PubMed] [Google Scholar]
- 23.Roijer E, Nordkvist A, Strom AK, Ryd W, Behrendt M, Bullerdiek J, et al. Translocation, deletion/amplification, and expression of HMGIC and MDM2 in a carcinoma ex pleomorphic adenoma. Am J Pathol 2002;160:433-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Chen AM, Garcia J, Bucci MK, Quivey JM, Eisele DW. Recurrent pleomorphic adenoma of the parotid gland: long-term outcome of patients treated with radiation therapy. Int J Radiat Oncol Biol Phys 2006;66:1031-5. [DOI] [PubMed] [Google Scholar]